Introduction
The hip joint is a complex and vital structure within the human body, essential for weight-bearing, movement, and overall stability. At the heart of this joint’s functionality are two primary angles of orientation: anteversion and retroversion. These terms describe the degree to which the femoral neck is rotated forward (anteversion) or backward (retroversion) relative to the frontal plane of the body. Understanding these variations is critical in diagnosing and treating a range of musculoskeletal issues.
The concept of femoral anteversion and retroversion has been a focus of study in both anatomical and clinical fields for decades. These angles are not static; they vary significantly among individuals due to genetic predisposition, developmental factors, and lifestyle influences. While some degree of variation is normal, extreme deviations can result in biomechanical inefficiencies, pain, and an increased risk of injury.
This article will explore the fundamental differences between hip anteversion and retroversion, their clinical significance, and their impact on movement patterns and joint health. By the end, readers will have a comprehensive understanding of how these angles influence biomechanics, as well as practical approaches for diagnosis and treatment within the field of osteopathy.
Anatomical Basis
The hip joint is a ball-and-socket joint formed by the articulation of the femoral head with the acetabulum of the pelvis. Its design provides a remarkable combination of stability and mobility, enabling activities such as walking, running, and jumping. However, the orientation of the femoral neck plays a pivotal role in determining the functional alignment of the hip.
Femoral Anteversion and Retroversion Defined
The term “anteversion” refers to the forward rotation of the femoral neck relative to the femoral condyles. A typical femoral neck anteversion angle ranges from 10° to 20° in adults. Conversely, “retroversion” describes a backward orientation of the femoral neck, where the angle is less than 10° or negative.
These angles are determined during skeletal development and are influenced by factors such as genetic predisposition, fetal positioning, and childhood activity levels. They play a critical role in joint congruency, influencing how the femoral head fits into the acetabulum.
Biomechanical Impact
The alignment of the femoral neck affects the loading patterns across the hip joint. Excessive anteversion can lead to an internal rotation of the femur, altering gait mechanics and increasing stress on the knee joint. Conversely, retroversion often results in external rotation, affecting hip range of motion and stability.
Understanding the anatomical basis of anteversion and retroversion is essential for recognizing their impact on movement patterns and overall musculoskeletal health. Deviations in these angles can lead to significant functional impairments, highlighting the importance of early identification and appropriate intervention.
Anteversion of the Hip
Femoral anteversion, characterized by a forward rotation of the femoral neck, is a natural anatomical feature with a range of normal variations. This angle typically measures between 10° and 20° in adults, though it is often higher during infancy and gradually decreases as a child grows. While some degree of anteversion is necessary for optimal hip function, excessive anteversion can lead to notable biomechanical and clinical challenges.
Causes and Risk Factors
Several factors contribute to the development of femoral anteversion. Genetics play a significant role, as family history can predispose individuals to higher angles of anteversion. Additionally, certain prenatal and postnatal conditions, such as abnormal fetal positioning or developmental dysplasia of the hip (DDH), can influence the orientation of the femoral neck. Childhood activities, particularly those that emphasize internal rotation of the hip, can also exacerbate this condition.
Functional Implications
Excessive femoral anteversion alters the biomechanics of the lower limb, leading to compensatory changes in posture and movement. One common manifestation is an inward rotation of the knees and feet during gait, commonly referred to as “in-toeing.” This adaptation occurs as the body attempts to maintain a stable base of support despite the altered hip alignment.
Increased anteversion can also affect the efficiency of the hip abductors and external rotators, which are crucial for maintaining pelvic stability during walking and running. Over time, this imbalance may contribute to overuse injuries, such as iliotibial band syndrome or patellofemoral pain syndrome.
Clinical Presentation
Patients with excessive femoral anteversion often report discomfort in the hips, knees, or lower back due to altered joint loading patterns. In severe cases, the condition can limit external rotation of the hip, restricting activities that require a wide range of motion, such as certain sports or yoga poses. Clinicians should be alert to signs of anteversion during physical examinations, particularly in individuals with a history of gait abnormalities or recurrent lower limb injuries.
By understanding the causes, functional implications, and clinical presentation of femoral anteversion, healthcare providers can tailor interventions to address both the symptoms and underlying biomechanical issues.
Retroversion of the Hip
Femoral retroversion, the backward orientation of the femoral neck relative to the frontal plane, is a less common variation compared to anteversion. Retroversion alters the alignment and biomechanics of the hip joint, often leading to functional limitations and discomfort if left unaddressed.
Causes and Risk Factors
Retroversion can arise from genetic predisposition or developmental factors during childhood. Conditions such as congenital hip deformities, trauma during growth, or reduced physical activity levels can all contribute to a decrease in the femoral neck angle. Unlike anteversion, which may decrease naturally with age, retroversion often becomes more pronounced over time if not addressed.
Functional Implications
Retroversion impacts the alignment of the entire lower limb, leading to compensatory adaptations in posture and movement. It often results in external rotation of the hip, causing the feet to point outward during gait—a condition known as “out-toeing.” This altered alignment can increase stress on the medial structures of the knee and exacerbate conditions such as medial knee osteoarthritis.
The limited internal rotation associated with retroversion can restrict movements requiring deep hip flexion or rotation, such as squatting or sitting cross-legged. Athletes may notice reduced performance in sports requiring multidirectional movements or explosive lower-limb actions.
Clinical Presentation
Symptoms of femoral retroversion often include hip or groin pain, stiffness, and reduced range of motion. Patients may also experience lower back discomfort due to compensatory pelvic tilt or lumbar lordosis. Retroversion can contribute to conditions like femoroacetabular impingement (FAI), where the altered hip alignment leads to abnormal contact between the femoral head and the acetabulum during movement.
Effective management of retroversion requires a thorough understanding of its anatomical and functional implications, along with individualized assessment and intervention.
Clinical Assessment
Accurate diagnosis of femoral anteversion and retroversion is critical for effective treatment. A combination of clinical evaluation and imaging studies is typically used to determine the degree of femoral neck rotation and its impact on hip function.
Physical Examination
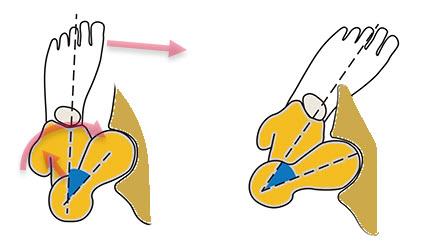
A comprehensive physical examination begins with an assessment of the patient’s gait. In-toeing may indicate excessive anteversion, while out-toeing suggests retroversion. Additional tests, such as the hip internal and external rotation range of motion, can provide further insights. Reduced external rotation is a hallmark of anteversion, while retroversion is associated with limited internal rotation.
The Craig’s Test, or Ryder Method, is a widely used clinical technique to estimate femoral anteversion. During this test, the patient lies prone, and the clinician palpates the greater trochanter while rotating the hip to determine the angle at which the trochanter is most prominent laterally. This angle approximates the degree of femoral anteversion.
Imaging Techniques
Radiographic imaging is essential for confirming the diagnosis. Plain X-rays, particularly axial and lateral views of the hip, can reveal the orientation of the femoral neck relative to the acetabulum. Computed tomography (CT) scans provide the most accurate measurements of femoral anteversion and retroversion, allowing for detailed three-dimensional analysis.
Functional Assessments
Functional assessments, such as observing squat mechanics or single-leg balance, help identify compensatory patterns caused by altered femoral neck angles. These evaluations are particularly valuable in athletes and active individuals who require optimal lower-limb biomechanics for performance and injury prevention.
By combining clinical examination, imaging, and functional assessments, practitioners can accurately diagnose and quantify femoral anteversion or retroversion, paving the way for effective treatment strategies.
Impact on Biomechanics and Movement
The orientation of the femoral neck significantly affects lower-limb biomechanics and overall movement patterns. Both femoral anteversion and retroversion alter the alignment of the hip, knee, and ankle, leading to compensatory changes that can influence gait, athletic performance, and the risk of injury.
Effects of Anteversion on Biomechanics
Excessive femoral anteversion causes internal rotation of the femur, which can manifest as an inward twisting of the knees and feet during walking or running. This inward alignment shifts the mechanical loading of the lower limb, increasing stress on the medial aspect of the knee and the patellofemoral joint. As a result, conditions such as patellofemoral pain syndrome or iliotibial band syndrome may develop over time.
In individuals with high anteversion, hip joint stability can be compromised, as the femoral head may not sit optimally within the acetabulum. This misalignment may lead to abnormal contact forces and wear on the articular cartilage, increasing the risk of early-onset osteoarthritis. Additionally, the restricted external rotation caused by anteversion can limit activities requiring lateral movements, such as certain sports or dance routines.
Effects of Retroversion on Biomechanics
Conversely, femoral retroversion results in an external rotation of the femur, causing the feet to point outward (out-toeing) during gait. This alignment shifts the load to the lateral structures of the knee and hip, which can lead to lateral hip pain or iliotibial band tightness. Retroversion may also decrease the ability to internally rotate the hip, limiting activities that require deep hip flexion or twisting motions, such as squatting or certain yoga poses.
Retroversion is often associated with an increased risk of femoroacetabular impingement (FAI), where abnormal contact between the femoral neck and acetabulum occurs during hip movements. This impingement can lead to pain, reduced range of motion, and labral damage over time.
Compensatory Movement Patterns
To compensate for the altered alignment, individuals with anteversion or retroversion often develop compensatory movement patterns in the pelvis, spine, or lower limbs. For example, a person with excessive anteversion may exhibit increased lumbar lordosis to maintain balance, while someone with retroversion may adopt an exaggerated pelvic tilt to facilitate hip movement. These adaptations can contribute to secondary issues such as lower back pain or sacroiliac joint dysfunction.
Understanding the biomechanical impact of femoral neck orientation is crucial for identifying the root causes of movement impairments and developing targeted interventions. Clinicians and osteopaths must consider these factors when assessing patients with gait abnormalities or chronic lower-limb pain.
Associated Conditions
Variations in femoral anteversion and retroversion are associated with a range of musculoskeletal conditions that can affect hip joint function and overall quality of life. Early recognition and management of these conditions are essential for preventing long-term complications.
Hip Dysplasia
Developmental dysplasia of the hip (DDH) is a condition in which the hip joint does not develop properly, often leading to excessive anteversion. This misalignment compromises joint stability and increases the risk of subluxation or dislocation. If untreated, DDH can result in chronic pain, gait abnormalities, and early-onset osteoarthritis.
Femoroacetabular Impingement (FAI)
Femoral retroversion is a common contributor to femoroacetabular impingement (FAI). The backward orientation of the femoral neck increases the likelihood of abnormal contact between the femoral head and the acetabulum during hip movements. Over time, this repetitive impingement can damage the cartilage and labrum, causing pain, stiffness, and a progressive loss of hip mobility.
Osteoarthritis
Both excessive anteversion and retroversion are risk factors for hip osteoarthritis. Abnormal femoral neck angles alter the distribution of forces across the joint, accelerating cartilage wear and degeneration. Patients with extreme variations in hip orientation often present with joint stiffness, reduced range of motion, and chronic pain as osteoarthritis progresses.
Patellofemoral Pain Syndrome (PFPS)
In individuals with excessive anteversion, internal rotation of the femur can lead to malalignment of the patella within the femoral groove. This maltracking increases stress on the patellofemoral joint, contributing to anterior knee pain commonly seen in PFPS.
Lower Back Pain
Compensatory postural adjustments to accommodate femoral anteversion or retroversion often involve the lumbar spine and pelvis. Increased lumbar lordosis or pelvic tilt can strain the lower back, leading to chronic pain or discomfort. Addressing these compensatory patterns is crucial for long-term relief.
Treatment Approaches
Treatment for variations in femoral anteversion and retroversion depends on the severity of the condition, the symptoms, and their impact on the patient’s daily life. A combination of osteopathic interventions and, in some cases, surgical treatments is used to address the biomechanical and functional challenges.
Osteopathic Management
Osteopathy provides a holistic approach to managing the structural and functional issues associated with femoral anteversion and retroversion. Through manual techniques and patient-specific interventions, osteopaths aim to restore alignment, improve mobility, and alleviate pain.
- Manual Therapy
Osteopaths use techniques such as soft tissue manipulation, myofascial release, and joint mobilization to improve mobility and reduce discomfort. These interventions not only target the hip but also address compensatory areas such as the pelvis, spine, and knees. For anteversion, treatments often focus on enhancing external rotation, while for retroversion, they target improved internal rotation. - Muscle Energy Techniques (MET)
MET is a collaborative technique where the patient engages specific muscle groups against gentle resistance provided by the osteopath. This method helps realign the femoral neck, reduce muscle imbalances, and restore optimal joint mechanics. - Functional Exercise Prescription
Osteopaths provide individualized exercise plans to strengthen key muscle groups, including the hip abductors, rotators, and core stabilizers. These exercises focus on improving functional movement patterns and compensating for altered biomechanics caused by femoral anteversion or retroversion. - Postural Re-education
Postural assessment and correction are integral to osteopathic treatment. By addressing compensatory patterns such as excessive lumbar lordosis or pelvic tilt, osteopaths help reduce strain on the hip and surrounding joints. - Holistic Approaches
Osteopaths incorporate a whole-body perspective, recognizing that systemic factors such as stress, visceral restrictions, or cranial imbalances can influence musculoskeletal health. By addressing these factors, they aim to optimize overall well-being and support hip function.
Surgical Interventions
While osteopathy can effectively manage many cases of femoral anteversion and retroversion, surgical intervention may be necessary for severe cases or when conservative management fails to relieve symptoms.
- Femoral Derotational Osteotomy
This procedure surgically realigns the femoral neck to correct excessive anteversion or retroversion, improving joint congruency and biomechanics. - Hip Arthroscopy
Hip arthroscopy is used to address complications such as femoroacetabular impingement (FAI) or labral tears associated with abnormal femoral neck angles. - Total Hip Replacement
In cases of advanced osteoarthritis or joint degeneration, total hip replacement may be required to restore mobility and reduce pain.
Prevention and Lifestyle Considerations
Preventing complications related to femoral anteversion and retroversion requires a proactive approach to maintaining hip health, addressing biomechanical risks, and supporting overall well-being. Osteopathy plays a significant role in helping patients adopt lifestyle changes and preventive strategies tailored to their individual needs.
Exercise for Strength and Stability
- Targeted Strengthening
Building strength in the hip stabilizers, such as the gluteus medius and external rotators, is essential. Osteopaths provide patients with customized exercise programs that align with their hip orientation. For anteversion, exercises that enhance external rotation are prioritized, while retroversion focuses on internal rotation capacity. - Dynamic Movements
Incorporating dynamic exercises, such as lateral lunges or single-leg balancing drills, improves coordination and balance, reducing the risk of injury.
Stretching and Mobility Work
- Hip Flexibility
Stretching tight muscle groups, such as the iliopsoas and hamstrings, promotes a balanced range of motion in the hip joint. Osteopaths often guide patients through gentle, targeted stretches to improve flexibility. - Joint Mobility Exercises
Simple movements like hip circles or controlled internal and external rotation exercises maintain joint mobility and reduce stiffness.
Ergonomics and Posture Awareness
- Postural Education
Poor posture exacerbates the strain on the hip joint. Osteopaths educate patients on maintaining proper posture during activities such as sitting, standing, and walking. - Ergonomic Adjustments
Ensuring an ergonomic setup at workstations, including supportive chairs and proper desk height, helps minimize unnecessary stress on the hips and spine.
Lifestyle Modifications
- Activity Moderation
Osteopaths guide patients on how to modify activities to avoid excessive stress on the hips. For example, limiting repetitive internal or external rotation movements during sports can prevent overuse injuries. - Rest and Recovery
Adequate rest and recovery are essential for maintaining joint health, especially for active individuals. Osteopaths emphasize the importance of balancing activity with recovery periods.
Nutrition and Bone Health
- Dietary Support
A nutrient-rich diet that includes calcium, vitamin D, and magnesium supports bone and joint health. Osteopaths may provide general dietary advice to complement treatment plans. - Hydration
Staying well-hydrated improves tissue elasticity and joint lubrication, promoting overall mobility.
Conclusion
Femoral anteversion and retroversion are complex anatomical variations that significantly impact biomechanics, movement patterns, and overall joint health. Left unmanaged, these conditions can lead to compensatory adaptations, chronic pain, and an increased risk of musculoskeletal injuries. However, with a comprehensive osteopathic approach, individuals can achieve improved alignment, mobility, and quality of life.
Osteopathy offers a unique, holistic perspective on managing these conditions. By addressing both the structural and functional aspects of femoral neck orientation, osteopaths help patients restore balance and optimize movement. Techniques such as manual therapy, muscle energy techniques, and patient-specific exercises play a central role in achieving these goals. Furthermore, osteopaths emphasize prevention and patient education, empowering individuals to maintain hip health and prevent future complications.
Collaboration with other healthcare professionals, when necessary, ensures that patients receive the most effective and well-rounded care. Whether through conservative management or as part of a multidisciplinary approach, osteopathy is a vital resource for addressing the challenges of femoral anteversion and retroversion.
As awareness of these conditions grows, continued research and case study documentation will further enhance the understanding and treatment of femoral anteversion and retroversion. Osteopaths remain at the forefront of providing patient-centered, evidence-based care, helping individuals live healthier, more active lives.
References
- Clohisy, J. C., et al. (2009). “The Diagnosis and Treatment of Femoroacetabular Impingement.” The Journal of the American Academy of Orthopaedic Surgeons.
- Hefti, F., et al. (1995). “Development of the Femoral Neck: Biomechanical Implications of Orientation Changes in Childhood.” Clinical Orthopaedics and Related Research.
- Kendall, F. P., et al. (2005). Muscles: Testing and Function with Posture and Pain. 5th Edition.
- Oatis, C. A. (2004). Kinesiology: The Mechanics and Pathomechanics of Human Movement.
- Osteopathy Australia (2020). “The Role of Osteopathy in Managing Hip Dysplasia.”