“In the complex labyrinth of modern life, cervical spondylosis sometimes reveals itself as a silent shadow, a painful reminder that the health of our cervical spine is a precious boundary between well-being and discomfort. »
Synonym: Cervical spinal deforming osteoarthritis, Cervical deforming osteoarthritis, Cervical osteoarthritis, Cervical osteophytosis, Cervical spondyloarthrosis , Cervical Barré-Lieou syndrome
Introduction
Cervical spondylosis, also known as cervical spondylosis, is a degenerative condition of the spine that affects the cervical vertebrae, the neck part. Characterized by wear and tear of the intervertebral discs and joints, this condition often results from the natural aging process, although other factors such as trauma, repetitive movements, and structural abnormalities can also contribute to its development. Symptoms, ranging from neck pain to stiffness and neurological disorders, can have a significant impact on quality of life. With this in mind, it is essential to understand the importance of posture in the prevention of cervical spondylosis, as healthy postural habits can play a key role in the prevention and management of this debilitating condition.
Causes
- Aging: Natural aging is the main cause of cervical spondylosis. Over time, the intervertebral discs can lose elasticity, become thinner, and undergo degeneration, which can lead to degenerative changes in the cervical spine.
- Wear of the intervertebral discs: The intervertebral discs between the cervical vertebrae act as shock absorbers. Over time, these discs can wear out due to daily mechanical stress, pressure exerted during certain activities, and the natural aging process.
- Dehydration of the discs: Dehydration of the intervertebral discs, which occurs with age, can lead to a loss of flexibility and height, contributing to cervical spondylosis.
- Heredity: Some individuals may be genetically predisposed to developing degenerative changes in the spine, including cervical spondylosis.
- Previous injuries: Previous injuries to the neck, such as car accidents or falls, can accelerate the process of degeneration of cervical discs and joints.
- Poor posture and lifestyle habits: Poor posture, sedentary lifestyle habits, and activities that put excessive strain on the neck can contribute to the development of cervical spondylosis.
- Mechanical factors: Certain mechanical factors, such as being overweight, can increase the pressure placed on the cervical spine, thereby promoting degeneration of discs and joints.
- Underlying medical conditions: Certain medical conditions, such as rheumatoid arthritis, can increase the risk of cervical spondylosis by causing chronic inflammation of the joints.
Symptoms
- Neck Pain: Pain is one of the most common symptoms of cervical spondylosis. It can be felt in the neck and sometimes radiates to the shoulders and arms.
- Neck stiffness: People with cervical spondylosis may experience stiffness in the neck, which can make head movements difficult.
- Headaches: Headaches, especially in the back of the head, may accompany cervical spondylosis.
- Tingling sensations or numbness: Some individuals may experience tingling sensations or numbness in the arms and hands, resulting from irritation of the cervical nerves.
- Muscle weakness: Cervical spondylosis can lead to muscle weakness in the arms and hands, especially if the nerves are compressed.
- Balance and coordination problems: In some advanced cases, compression of the cervical structures can affect balance and coordination of movements.
- Crepitations or joint sounds: Crepitations may be felt during neck movements due to degenerative changes in the cervical joints.
- Decreased range of motion: People with cervical spondylosis may experience a decreased range of motion in the neck due to stiffness and discomfort.
Pathophysiology
Here is a step-by-step explanation of the pathophysiology of cervical spondylosis:
- Aging: The main cause of cervical spondylosis is natural aging. Over time, the structures of the spine undergo degenerative changes.
- Wear of the intervertebral discs: The intervertebral discs between the cervical vertebrae undergo a process of dehydration and wear. These discs, which act as shock absorbers between the vertebrae, lose their elasticity and height.
- Osteophyte Formation: In response to wear and instability of the intervertebral discs, the body can develop osteophytes, also called parrot beaks. These bony growths form along the edges of the vertebrae.
- Thickening of Ligaments: The ligaments that support the spine can thicken due to increasing instability and degenerative changes. This can lead to loss of mobility and contribute to cervical spondylosis.
- Reduction in intervertebral space: Degenerative changes cause a reduction in the height of the intervertebral discs, thereby reducing the space between the vertebrae.
- Compression of nerves: Osteophytes and other degenerative changes can compress the nerve roots that emerge from the spinal cord. This can lead to symptoms such as cervical radiculopathy, with pain, numbness or weakness in the arms and hands.
- Spinal cord compression: In some cases, disc degeneration and osteophyte formation can lead to compression of the spinal cord itself, causing cervical myelopathy. This can manifest as balance problems, impaired coordination, and difficulty walking.
The Impact of Cervical Spondylosis on Quality of Life
- Pain and Discomfort:
- Neck pain is one of the most common symptoms of cervical spondylosis. This pain may be persistent and may radiate to the shoulders, arms and head.
- Constant discomfort can make it difficult to do everyday activities, like working, driving, or even simple tasks like turning your head.
- Reduced mobility :
- Cervical spondylosis can cause loss of mobility in the neck. Rotation and tilt movements of the head may be limited, affecting the ability to perform normal activities.
- Sufferers may have difficulty participating in physical and recreational activities, which can lead to a decreased overall quality of life.
- Sleeping troubles :
- The pain and discomfort associated with cervical spondylosis can disrupt sleep, leading to chronic fatigue.
- Disrupted sleep can impact mental health, daily energy and the ability to cope with stress.
- Impact on Work:
- People with cervical spondylosis may find it difficult to sit for long periods of time, which can affect their performance at work.
- Symptoms can also lead to missed work, changes to job duties, or even an inability to work in some severe cases.
- Social and Emotional Repercussions:
- Constant pain can lead to mood changes, irritability, and even depressive symptoms.
- Physical limitations can also lead to social withdrawal, as people may avoid social activities due to pain or embarrassment.
Prevention of Cervical Spondylosis
- Maintaining Good Posture:
- Adopting correct posture when sitting, standing and walking is crucial to preventing cervical spondylosis. Avoid excessively bending your neck while looking down for long periods of time.
- Ergonomics at Work:
- Adjust your workstation to maintain an ergonomic posture. Use lumbar support, properly position the computer screen at eye level, and take regular breaks to stretch.
- Muscle Strengthening Exercises:
- Strengthen your neck, shoulder and back muscles with specific exercises recommended by a healthcare professional. This can help stabilize the cervical spine and prevent degeneration.
- Regular Stretching:
- Practice neck, shoulder, and back stretches to maintain flexibility and prevent stiffness. Gentle rotating and tilting movements can help relax muscles and prevent compression of the cervical vertebrae.
- Weight Management:
- Maintain a healthy body weight to reduce pressure on the spine. Excess weight can contribute to premature wear of intervertebral discs.
- Adequate Hydration:
- Drink enough water to maintain the flexibility of the intervertebral discs. Good hydration helps prevent premature degeneration of cartilage.
- Avoiding Bad Postural Habits:
- Avoid holding the phone between your shoulder and ear and limit prolonged use of tablets and smartphones by looking down.
- Use of Ergonomic Cushions:
- Use pillows and cushions that properly support the head and neck while sleeping. Adopt a sleeping position that keeps the spine in a neutral position.
- Stress management :
- Stress can contribute to muscle tension. Practice stress management techniques such as meditation, deep breathing, and yoga to relax your neck and shoulder muscles.
- Early Medical Consultation:
- If you experience symptoms of cervical spondylosis, see a healthcare professional as soon as possible. Early diagnosis can allow for effective management and interventions to prevent the condition from worsening.
The Importance of Posture in the Prevention of Cervical Spondylosis
- Sitting :
- Make sure your feet touch the floor or use a footrest to keep your knees at a 90-degree angle.
- Keep your back straight and well supported against the back of the chair.
- Avoid crossing your legs for long periods of time.
- Ergonomics at Work:
- Adjust the height of your chair and desk to keep the arms at a 90-degree angle when typing.
- Position the computer screen at eye level to avoid constantly lowering your head.
- Standing position :
- Distribute the weight evenly on both feet.
- Keep your feet shoulder-width apart.
- Avoid locking your knees and keep them slightly bent.
- Use of Mobile Devices:
- Avoid constantly lowering your head to look at your phone or tablet.
- Hold the device at eye level as much as possible.
- Car driving :
- Adjust the seat so that your feet can reach the pedals comfortably.
- Use a lumbar cushion to support the natural curvature of the spine.
- Pillow and Sleeping Position:
- Choose a pillow that keeps your head and neck in a neutral position.
- Avoid sleeping on your stomach, as this can lead to excessive neck twisting.
- Stress management :
- Stress can lead to muscle tension, affecting posture. Practice stress management techniques, such as meditation or deep breathing.
- Break and Stretch:
- Take regular breaks if you work seated for long periods of time.
- Perform neck, shoulder and back stretches to prevent stiffness.
- Muscle Strengthening Exercises:
- Strengthen your neck, shoulder and back muscles with specific exercises recommended by a healthcare professional.
- Posture Monitoring:
- Be aware of your posture throughout the day. Use visual reminders or apps to remind yourself to maintain good posture.
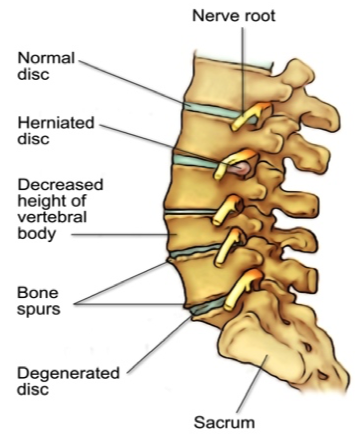
Disc degeneration and bone spur formation
With the natural process of aging, spinal discs undergo changes that can have implications for the stability and function of the spine. These discs, made primarily of water in their youth, experience degenerative changes over time.
The consequences of aging on spinal discs include a progressive loss of their water content, leading them to dry out and become structurally weakened. This phenomenon contributes to the reduction of intervertebral disc spaces, causing a decrease in the height between the vertebrae and, therefore, leading to a loss of spinal stability.
Simultaneously, the facet joints, which play a crucial role in spinal mobility and stability, experience increased pressure due to these degenerative changes. This excessive pressure can lead to degeneration of the joints, giving rise to a form of arthritis.
Articular cartilage, once smooth and protective, gradually wears away over time, exposing the bony surfaces of the joints. This process can lead to a loss of stability in the affected spinal segment. If the cartilage wears away completely, adjacent bones can come into contact, causing bone friction.
Faced with degeneration and loss of cartilage, the body may attempt to compensate by growing new bone within the facet joints. These bony growths, known as bone spurs, are the body’s response to stabilize the affected area by supporting the vertebrae.
However, over time, these bone spurs can contribute to stenosis, a narrowing of the space for nerves and the spinal cord to pass through. This bone overgrowth can lead to symptoms such as nerve compression, radiculopathy, and in some cases, mobility problems.
In summary, spinal disc aging is a complex process that can lead to structural alterations, impacting the stability and mobility of the spine and contributing to conditions such as spondylosis and spinal stenosis.
Classification of cervical spondylosis
Cervical spondylosis is a non-specific term which covers a wide range of conditions but which, for reasons of precision, can be divided into three clinical syndromes: type I syndrome (cervical radiculopathy); type II syndrome (cervical myelopathy); and type III syndrome (axial joint pain).
- Type I Syndrome (Cervical Radiculopathy): Cervical radiculopathy occurs when the nerve roots of the spinal cord in the neck are compressed or irritated. This can lead to symptoms such as pain, numbness, tingling, or weakness in the arms and hands.
- Type II Syndrome (Cervical Myelopathy): Cervical myelopathy occurs when the spinal cord itself is compressed or damaged in the neck. Symptoms may include impaired coordination, limb weakness, balance problems, and difficulty walking.
- Type III Syndrome (Axial Joint Pain): Axial joint pain in the context of cervical spondylosis refers to pain centered on the joints of the cervical spine. It can be the result of wear of the discs and facet joints in the cervical region.
Exercises and Stretches for Cervical Spondylosis
Muscle Strengthening Exercises
- Isometric Cervical Flexion:
- Sit or stand with your back straight.
- Place your hands on your forehead and apply light forward pressure while resisting with your neck.
- Hold the position for 5 to 10 seconds and repeat 10 times.
- Isometric Cervical Extension:
- Sit or stand with your back straight.
- Place your hands on the back of your head and apply gentle backward pressure while resisting with your neck.
- Hold the position for 5 to 10 seconds and repeat 10 times.
- Isometric Cervical Rotation:
- Sit or stand with your back straight.
- Slowly turn your head to the right, resisting with your neck muscles.
- Hold for 5 to 10 seconds and repeat on each side 10 times.
- Shoulder Raise:
- Sit or stand with your shoulders relaxed.
- Gently lift your shoulders toward your ears, then lower back down.
- Perform 15 repetitions.
Stretches for Flexibility
- Lateral Neck Tilt:
- Sit or stand with your back straight.
- Slowly tilt your head to one side, trying to bring your ear toward your shoulder.
- Hold the position for 15 to 30 seconds on each side.
- Neck Rotation:
- Sit or stand with your back straight.
- Slowly turn your head to one side, looking over your shoulder.
- Hold the position for 15 to 30 seconds on each side.
- Neck Extension:
- Sit or stand with your back straight.
- Gently tilt your head back, looking toward the ceiling.
- Hold the position for 15 to 30 seconds.
- Neck Flexion:
- Sit or stand with your back straight.
- Gently lower your chin toward your chest, stretching the back of your neck.
- Hold the position for 15 to 30 seconds.
- Trapeze Stretch:
- Sit or stand with your back straight.
- Tilt your head to one side, while gently pulling on the side of your neck with the opposite hand.
- Hold the position for 15 to 30 seconds on each side.
Important Tips:
- Perform these exercises and stretches slowly, without forcing.
- Make each movement in a controlled manner.
- If you experience significant pain or discomfort, stop immediately and consult a healthcare professional.
- Perform these exercises regularly, but do not overload the cervical region.
It is crucial to personalize these exercises according to your physical condition and to consult a health professional for appropriate guidance.
Frequently asked questions
- What is cervical spondylosis?
- Cervical spondylosis, also called cervical spondylosis, is a degenerative spinal condition that affects the cervical (neck) vertebrae. It is characterized by wear of the intervertebral discs and the joints between the vertebrae.
- What are the causes of cervical spondylosis?
- Cervical spondylosis is mainly caused by the natural aging of the body, involving the degeneration of intervertebral discs and joints. However, factors such as increased wear and tear from repetitive motion, trauma, or structural abnormalities can also contribute.
- What are the symptoms of cervical spondylosis?
- Symptoms may include neck pain, stiffness, headache, tingling or numbness in the arms, and sometimes difficulty making neck movements.
- How is cervical spondylosis diagnosed?
- Diagnosing cervical spondylosis usually involves a thorough medical evaluation, medical history, imaging tests such as X-rays or MRI, and neurological tests to assess nerve function.
- What treatments are available for cervical spondylosis?
- Treatments may include medications to relieve pain, physical therapy to strengthen the neck muscles, lifestyle changes, and in some cases, surgeries to relieve nerve compression.
- Can cervical spondylosis be prevented?
- Although it is not possible to completely prevent cervical spondylosis due to the natural aging process, maintaining good posture, adopting healthy lifestyle habits, and practicing specific exercises can help prevent or alleviate symptoms.
- Is osteopathy beneficial for cervical spondylosis?
- Osteopathy can be beneficial in the treatment of cervical spondylosis by using manual techniques to improve mobility, reduce muscle tension, and promote better blood circulation. However, its effectiveness may vary from person to person.
- What are the risk factors for cervical spondylosis?
- Major risk factors include aging, repetitive neck movements, previous trauma, smoking, genetics, and certain underlying medical conditions.
Radiographic signs
Radiographic signs of cervical spondylosis can be seen through imaging tests such as cervical x-rays. Cervical spondylosis is characterized by degenerative changes in the cervical spine. Here are some of the radiographic signs commonly associated with cervical spondylosis:
- Osteophytes (parrot beaks): Bony growths, called osteophytes or parrot beaks, can form around the edges of the vertebrae. These growths may be visible on x-rays and are the result of bone growth in response to aging and degeneration of the intervertebral discs.
- Narrow space between the intervertebral discs: Cervical spondylosis can cause a narrowing of the space between the intervertebral discs due to wear and degeneration of the discs.
- Thickening of ligaments: The ligaments surrounding the spine can thicken in response to stress and degeneration, which can be seen on x-rays.
- Reduced disc height: Degeneration of the intervertebral discs can cause a reduction in disc height, which may be visible on x-rays.
- Abnormal alignment: Changes in the normal alignment of the cervical vertebrae can occur due to degeneration of the discs and facet joints.
- Synovial cyst formation: Synovial cysts can develop in the joints between vertebrae, and these cysts may be visible on x-rays.
Dysphagia can be caused by hypertrophic anterior cervical osteophytes, 1 and approximately 100 such cases have been reported in the literature. It affects up to 10% of patients over 65 years old (Resnick D & Robins, 1975)
A retrospective study of 376 patients over 60 years of age who were evaluated for dysphagia demonstrated that 10% of cases were determined to be secondary to protrusion of cervical osteophytes. (Granville et al, 1998). Generally levels from C3 to 6 are most often involved. Therefore, cervical osteophytes should be suspected as a cause of swallowing difficulties when other explainable causes are absent (Lee et al, 2008)
Conclusion
In conclusion, cervical spondylosis represents a health challenge that requires a proactive approach, and the adoption of good postural habits is crucial in this process. Maintaining correct posture during daily activities, at work, while driving, or even while sleeping, can help reduce pressure on the cervical spine. These simple lifestyle adjustments can help prevent the development or worsening of cervical spondylosis. However, it is always recommended to consult a healthcare professional for advice tailored to each individual situation and to put in place an effective prevention and management plan for this degenerative condition. By cultivating ongoing awareness of our posture and incorporating practices that promote cervical spine health, we can help maintain our physical well-being and preserve optimal quality of life.
Reference
Granville LJ, Musson N, Altman R, et al. Anterior cervical osteophytes as a cause of pharyngeal stage of dysphagia. J Am Geriatr Soc 1998;46:1003-1007.
Lee, Seung Ah, MD; Kim, Kyung Eun, MD; Paik, Nam-Jong, MD, PhD : Dysphagia Caused by Multilevel Cervical Osteophytes : American Journal of Physical Medicine & Rehabilitation: July 2008 – Volume 87 – Issue 7 – p 607
Resnick D, Shaul SR, Robins JM: Diffuse idiopathic skeletal hyperostosis (DISH): Forestier’s disease with extraspinal manifestations. Radiology 1975;115:513–24