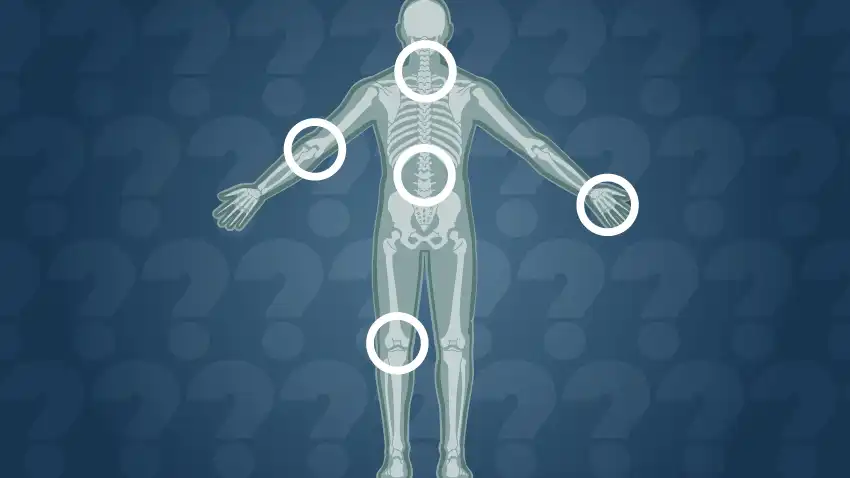
Osteoarthritis, a degenerative joint condition, can have a significant impact on quality of life. Understanding the general factors that influence its progression is essential to implementing effective prevention strategies. In this article, we will explore the multiple aspects that can contribute to the progression of osteoarthritis and ways to address them.
Introduction to Osteoarthritis
Osteoarthritis is a common joint disease that affects millions of people worldwide. It is characterized by the progressive degradation of cartilage, this elastic and cushioning tissue which covers the ends of the bones within the joints. This breakdown of cartilage can lead to joint inflammation, pain and stiffness, as well as reduced mobility and quality of life.
Although osteoarthritis is often associated with aging, it can also occur in younger people due to a variety of factors. These factors may include previous joint injuries, genetic predispositions, inflammatory diseases such as rheumatoid arthritis, a sedentary lifestyle, obesity and unhealthy eating habits.
Understanding these factors is crucial to implementing effective osteoarthritis prevention and management strategies. By identifying specific risk factors in an individual, it is possible to take proactive steps to reduce the risk of developing this debilitating disease or to slow its progression in those who already have it.
In this series of articles, we will explore in detail the different aspects of osteoarthritis, including its causes, symptoms, diagnostic methods, treatment options, and prevention strategies. By providing comprehensive, up-to-date information about this complex joint disease, our goal is to help individuals better understand osteoarthritis and make informed decisions regarding their joint health. Stay tuned to learn more about this important topic.
Causes
Osteoarthritis, a common form of arthritis, is a complex condition with multifactorial causes. At the heart of its development is a combination of genetic, environmental and mechanical factors. Genes play an essential role in the predisposition to osteoarthritis. Studies have identified several genetic variants associated with an increased risk of developing this disease. These variants can influence the structure and function of cartilage, as well as the body’s inflammatory response. However, the expression of these genes is often modulated by environmental factors.
Environmental factors, such as age, body weight, previous joint injuries and physical activity, play a crucial role in the development of osteoarthritis. Aging is one of the main risk factors, as it leads to a decrease in the ability of cartilage to regenerate and repair itself. In addition, overweight and obesity place additional pressure on the joints, thus accelerating the wear and tear of the cartilage. Previous joint injuries, whether sports, accidental or work-related, can damage cartilage and increase the risk of developing osteoarthritis in the long term. Likewise, intense or repetitive physical activity can cause excessive wear and tear on the joints, thus promoting the development of the disease.
Mechanical imbalances in joints can also contribute to osteoarthritis. Poor posture, congenital joint defects, and lower limb alignment disorders, such as hip or knee osteoarthritis, can lead to uneven distribution of load on the joints, which can accelerate wear and tear. cartilage and cause damage.
Furthermore, inflammation plays an important role in the pathogenesis of osteoarthritis. Although osteoarthritis is traditionally considered a non-inflammatory disease, recent studies suggest that inflammation plays an active role in disease progression. Factors such as obesity, joint injuries and metabolic diseases can trigger an inflammatory response in the joints, causing accelerated cartilage breakdown.
Finally, other factors such as hormonal imbalances, metabolic disorders and autoimmune diseases can also contribute to the development of osteoarthritis. For example, hormonal fluctuations in postmenopausal women can affect joint health, while autoimmune diseases such as rheumatoid arthritis can increase the risk of secondary osteoarthritis.
Here are the main factors that can contribute:
List of factors contributing to the development of this joint disease:
- Aging : Age is one of the main risk factors for osteoarthritis. Over time, articular cartilage can experience natural breakdown from daily wear and tear, which can lead to progressive joint deterioration.
- Genetic factors : Studies have shown that certain genetic variants can predispose individuals to developing osteoarthritis. Genes play a role in the structure and composition of cartilage, as well as the body’s inflammatory response, which can influence the risk of developing this disease.
- Previous joint injuries : Joint injuries, whether sports, traumatic, or accident-related, can damage cartilage and increase the risk of developing osteoarthritis later in life. Joint fractures, severe sprains and dislocations can disrupt the normal structure of the joint and accelerate cartilage wear.
- Inflammatory joint diseases : Certain inflammatory diseases, such as rheumatoid arthritis, lupus, and ankylosing spondylitis, can damage joints and lead to chronic inflammation, which can contribute to the development of osteoarthritis.
- Obesity : Being overweight and obese puts additional pressure on the joints, especially those that support the body’s weight such as the knees, hips and lumbar vertebrae. This increased pressure can accelerate cartilage wear and increase the risk of osteoarthritis.
- Lifestyle : Factors such as a sedentary lifestyle, unhealthy eating habits, and smoking can also contribute to the development of osteoarthritis by increasing inflammation in the body and impairing joint health.
- Strenuous physical activity : Although regular exercise is beneficial for joint health, strenuous physical activity, especially high-impact activities or sports involving repetitive movements, can increase the risk of joint injuries and osteoarthritis, especially if not practiced appropriately and progressively.
- Joint abnormalities : Anatomical abnormalities or congenital malformations of the joints, such as bone malpositions or joint dysplasia, can lead to abnormal distribution of forces on the cartilage, which can promote early wear and development of osteoarthritis.
- Muscle deficits : Muscle imbalance or muscle weaknesses around joints can lead to joint instability and overload of joint structures, which can contribute to cartilage wear and the development of osteoarthritis.
- Medical Treatments : Certain medical treatments, such as corticosteroids given by injection to treat joint inflammation, may have long-term side effects on joint health and increase the risk of osteoarthritis.
- Environmental factors : Environmental factors such as exposure to toxic chemical agents, repetitive trauma related to work or certain occupational activities, as well as working conditions that involve prolonged standing or repetitive movements, can also contribute to the development osteoarthritis.
- Joint instability : Injuries or conditions that lead to joint instability, such as ligamentous laxity or meniscal damage, can contribute to cartilage wear and promote the development of osteoarthritis.
- Hormones : Hormonal changes, such as those seen during menopause in women, can influence joint health and play a role in the development of osteoarthritis.
- Metabolic factors : Metabolic disorders, such as diabetes and high cholesterol, have been linked to an increased risk of osteoarthritis, although the exact mechanisms of this association are not yet completely understood.
- Repetitive trauma : Activities or occupations that cause repeated trauma to joints, such as manual labor or high-impact sports, can contribute to premature wear of cartilage and the development of osteoarthritis.
- Psychosocial factors : Psychological stress, depression, and other psychosocial factors can influence pain perception and the body’s inflammatory response, which can impact joint health and the development of osteoarthritis.
- Joint Formation Defects : Some individuals may have birth defects or joint formation defects that may increase their predisposition to developing osteoarthritis.
- Neurological disorders : Neurological conditions such as Parkinson’s disease or spinal cord injury can alter the way joints are used and stabilized, which can contribute to cartilage wear and the development of osteoarthritis.
- Previous joint infections : Previous joint infections, such as sepsis or infectious arthritis, can damage cartilage and joint tissue, which can increase the risk of developing osteoarthritis later.
- Psychological trauma : Traumatic or stressful life events, such as serious accidents, bereavements or emotional trauma, can impact joint health by influencing the body’s inflammatory response and ability to heal.
- Non-specific genetic factors : In addition to specific genetic variants associated with osteoarthritis, there are non-specific genetic factors that can influence a person’s susceptibility to developing joint disorders and degenerative diseases.
- Hormonal dysfunction : Hormonal imbalances, such as those associated with conditions such as hypothyroidism or hyperthyroidism, can affect joint health and contribute to the development of osteoarthritis.
- Occupational factors : Certain occupations involving repetitive movements, heavy lifting, or uncomfortable positions may increase the risk of developing osteoarthritis, particularly in the joints affected by these activities.
- Smoking : Smoking has been linked to an increased risk of developing osteoarthritis, due to its harmful effects on blood flow and connective tissue health, which can compromise joint health.
- Medications : Certain medications, such as long-term corticosteroids or immunosuppressive treatments, can have side effects on joint health and increase the risk of osteoarthritis.
- Education level : Studies have suggested that a lower education level may be associated with an increased risk of osteoarthritis, although the exact mechanisms of this association are not yet fully understood.
- Psychological factors : Psychological disorders such as anxiety, depression or chronic stress can impact the perception of pain and the body’s inflammatory response, which can influence the development and progression of osteoarthritis.
- Family medical history : A family history of osteoarthritis can increase an individual’s risk of developing this condition, suggesting a potential genetic link in some cases.
- Socio-economic level : Studies have shown that socio-economic factors such as economic status, access to health care and associated stress level can influence the risk of osteoarthritis.
- Psychological trauma : Traumatic events in childhood or adulthood, such as physical or emotional abuse, can impact long-term joint health due to their effects on stress and the inflammatory response.
- Religious or spiritual practices : Studies have suggested that regular religious or spiritual practice may be associated with a reduced risk of developing osteoarthritis, although the exact mechanisms of this association are not yet clear.
- Environmental conditions : Environmental factors such as air pollution or exposure to toxic agents can also contribute to the development of osteoarthritis by causing chronic inflammation and cellular damage.
- Infant Nutrition : Studies suggest that childhood nutrition, including breastfeeding and the introduction of solid foods, may impact joint development and the risk of osteoarthritis in adulthood.
- Exposure to heavy metals : Exposure to heavy metals such as lead, mercury, and cadmium can damage joint tissue and contribute to the development of osteoarthritis.
- Climatic factors : The climate in which a person lives can influence the risk of osteoarthritis. For example, changes in temperature and humidity can make symptoms worse in some people.
- Immune system dysfunctions : Immune system dysfunctions, such as those seen in autoimmune diseases, can contribute to joint inflammation and the development of osteoarthritis.
- Recreational activities : Certain recreational activities, such as intensive gardening or manual labor, can increase the risk of joint injuries and the development of osteoarthritis.
- Exposure to pesticides and chemicals : Occupational or environmental exposure to pesticides, industrial chemicals, and toxic products can damage joints and contribute to the development of osteoarthritis.
- Clotting disorders : Blood clotting disorders, such as thrombophilia, can affect blood flow to the joints and lead to damage to joint tissue.
- Long-term pain medications : Prolonged use of pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can have detrimental effects on joint health and increase the risk of osteoarthritis.
- Endocrine diseases : Endocrine diseases such as acromegaly, Cushing’s syndrome and hyperparathyroidism can affect bone metabolism and increase the risk of osteoarthritis.
- Early emotional trauma : Traumatic events during childhood or adolescence, such as abuse or neglect, can influence long-term joint health due to their impact on psychological and physiological development.
- Exposure to Ionizing Radiation : Prolonged exposure to ionizing radiation, such as from X-rays or medical radiation, can damage joint tissue and increase the risk of osteoarthritis.
- Physical activity level in childhood : Physical activity level during childhood and adolescence can impact long-term joint health. Regular physical activity while growing up can promote the development of healthy joints and reduce the risk of osteoarthritis later in life.
- Fluoride Exposure : Excessive exposure to fluoride, whether through fluoridated drinking water or other sources, can contribute to abnormalities in bone and joint development, potentially increasing the risk of osteoarthritis.
- Poor posture : Poor posture, whether due to daily habits or musculoskeletal disorders, can put uneven pressure on joints and promote cartilage wear.
- Nutritional deficits : Deficiencies in certain essential nutrients, such as vitamin D, calcium, magnesium and omega-3 fatty acids, can compromise joint health and increase the risk of osteoarthritis.
- Chronic inflammation : Medical conditions characterized by chronic inflammation, such as metabolic syndrome, cardiovascular disease, or inflammatory bowel disease, may increase the risk of osteoarthritis due to the detrimental effect of inflammation on joint tissues.
- Intestinal dysbiosis : An imbalance in gut flora, known as gut dysbiosis, can lead to systemic inflammation and affect joint health, increasing the risk of osteoarthritis.
- Environmental Metal Exposure : Environmental exposure to heavy metals, such as lead, cadmium, and mercury, may contribute to the development of osteoarthritis by disrupting metabolic processes and damaging joint tissues.
- Sleep Disturbances : Sleep disorders, such as sleep apnea or chronic insomnia, can contribute to inflammation and oxidative stress, which are known risk factors for the development of osteoarthritis.
- Exposure to chemicals in the home environment : Exposure to chemicals found in cleaning products, plastics or floor coverings can contribute to inflammation and metabolic disorders, increasing the risk of osteoarthritis.
Symptoms
Osteoarthritis is a chronic joint disease characterized by progressive breakdown of cartilage and changes in surrounding joint tissues. The symptoms of osteoarthritis vary depending on the location of the affected joints, the severity of the disease and the individual factors of each patient. However, several common symptoms can be seen in people with osteoarthritis.
Joint pain is one of the most common symptoms of osteoarthritis. This pain may be described as a dull aching sensation, stiffness, or tenderness in or around the affected joint. It may be mild at the start of the disease, but gradually worsen over time, particularly after physical activity or a period of rest.
Joint stiffness is also a common symptom of osteoarthritis. People with osteoarthritis may experience joint stiffness, especially in the morning or after a prolonged period of inactivity. This stiffness can make moving the joint difficult and uncomfortable, but it tends to improve with movement and physical activity.
Decreased joint flexibility is often seen in people with osteoarthritis. Due to the breakdown of cartilage and the formation of bone spurs around the joint, normal movements may become limited and restricted. Affected joints may feel stiff and may not bend or twist as easily as before.
Loss of mobility is another symptom commonly associated with osteoarthritis. Due to pain, stiffness, and loss of flexibility, people with osteoarthritis may experience a decrease in their ability to move normally. This may affect their ability to perform daily activities such as walking, climbing stairs, bending and standing.
Joint crepitations are cracking or grinding noises or sensations that may be felt or heard during movement of the affected joints. This noise is caused by the friction of rough or damaged joint surfaces, resulting in the breakdown of cartilage and the formation of bone spurs.
Joint swelling can also occur in people with osteoarthritis, due to synovial fluid buildup or inflammation in the joint. The swelling can make the joint swollen, tender, and tender to the touch.
It is important to note that the symptoms of osteoarthritis can vary from person to person and can also change over time. Some patients may experience periods of remission where symptoms improve, while others may experience flare-ups of more severe symptoms. In all cases, it is essential to consult a healthcare professional to obtain an accurate diagnosis and an appropriate treatment plan if osteoarthritis is suspected.
Here is a more detailed description of these symptoms:
- Joint pain : Pain is one of the most common symptoms of osteoarthritis. It may be described as a feeling of dull pain or stiffness in or around the affected joint. The pain may be mild at first, but it may gradually get worse over time.
- Joint stiffness : People with osteoarthritis may experience joint stiffness, especially after a period of rest or inactivity. This stiffness can make moving the joint difficult and uncomfortable, but it usually tends to improve with movement.
- Loss of joint flexibility : Osteoarthritis can cause decreased flexibility in affected joints, which can make normal movements more difficult to perform. Joints may feel stiff and not bend or twist as easily as before.
- Decreased mobility : Due to pain, stiffness, and loss of flexibility, people with osteoarthritis may also experience a decrease in their ability to move normally. This may affect their ability to perform daily activities such as walking, climbing stairs, bending and standing.
- Joint crepitus : In some cases, cracking or grinding sounds may be felt or heard when moving the affected joints. This noise, called crepitation, is caused by friction of rough or damaged joint surfaces.
- Joint swelling : Osteoarthritis can sometimes cause swelling in the joints, due to synovial fluid buildup or inflammation. The swelling can make the joint swollen, tender, and tender to the touch.
It is important to note that the symptoms of osteoarthritis can vary from person to person and may also change over time. Some patients may experience periods of remission where symptoms improve, while others may experience flare-ups of more severe symptoms. In all cases, it is essential to consult a healthcare professional to obtain an accurate diagnosis and an appropriate treatment plan if osteoarthritis is suspected.
How to diagnose osteoarthritis
The diagnosis of osteoarthritis is based on a combination of medical history, physical examination and imaging tests. Although there is no specific test to definitively diagnose osteoarthritis, doctors use several methods to assess symptoms and identify joint changes characteristic of the disease.
The diagnostic process often begins with an in-depth patient interview to gather a detailed medical history, including symptoms, duration, and severity. The doctor may ask questions about the patient’s daily activities, movements that aggravate pain, and factors that relieve symptoms. Family medical history of osteoarthritis or other joint conditions may also be considered.
The physical examination is an important step in the process of diagnosing osteoarthritis. The doctor will examine the affected joints, assessing pain, stiffness, joint mobility, and the presence of bone spurs or signs of inflammation. Specific tests may be performed to determine joint stability and function, as well as to identify possible abnormalities in joint alignment or structure.
Imaging tests, such as x-rays, are often used to confirm the diagnosis of osteoarthritis and assess the extent of joint damage. X-rays can reveal characteristic signs of osteoarthritis, such as decreased joint space, formation of bone spurs, and changes in the surrounding bone structure. In some cases, other imaging tests, such as MRI or ultrasound, may be used to more accurately assess the condition of the cartilage and surrounding soft tissues.
Sometimes lab tests may be done to rule out other medical conditions that may have symptoms similar to osteoarthritis, such as rheumatoid arthritis or gout. Blood tests can be used to look for inflammatory markers or rheumatoid factors, although these tests are generally not specific to osteoarthritis.
Finally, the doctor can also use standardized diagnostic criteria, such as the ACR (American College of Rheumatology) criteria for hand osteoarthritis, to help confirm the diagnosis and assess the severity of the disease.
Genetic and Hereditary Factors
Osteoarthritis is a degenerative joint disease that can lead to chronic pain, stiffness and loss of joint function. Although osteoarthritis is often associated with aging and environmental factors such as obesity and joint injuries, there is growing evidence that genetic factors also play a significant role in its development and progression.
Extensive studies have identified several genetic variants that are associated with increased risk of osteoarthritis. For example, research has shown that variations in genes responsible for the formation and repair of articular cartilage may influence susceptibility to developing this disease. Additionally, mutations in genes involved in bone and joint metabolism, such as extracellular matrix genes and inflammation genes, have also been linked to an increased risk of osteoarthritis.
Heredity also plays an important role in osteoarthritis. Individuals with a family history of osteoarthritis have a higher risk of developing the disease, suggesting that there are genetic components passed down from generation to generation that predispose to this condition. This observation is supported by family studies and twin studies, which have shown a significant correlation between the presence of osteoarthritis in family members and increased risk of osteoarthritis in individuals.
It is important to note that genetic factors do not necessarily determine a person’s fate when it comes to osteoarthritis. Although certain genetic variants can increase the risk of developing the disease, other factors, such as lifestyle, environment and health choices, can also play a crucial role in its onset and progression. For example, obesity, which puts additional strain on joints, is a well-established risk factor for osteoarthritis. Likewise, joint injuries, dietary habits and physical activity can all influence joint health and modulate the risk of osteoarthritis.
Understanding the genetic and hereditary factors of osteoarthritis may have important implications for the prevention, diagnosis and treatment of the disease. By identifying individuals at high risk due to their genetic profile, it is possible to implement early prevention strategies, such as interventions to reduce body weight and tailored exercise programs to strengthen the muscles around the joints. and improve their stability.
Additionally, understanding the underlying genetic mechanisms of OA may lead to the development of targeted therapies that specifically target the biological pathways involved in the pathogenesis of the disease. For example, drugs that target joint inflammation processes or stimulate cartilage regeneration could represent promising approaches for the treatment of osteoarthritis in patients with particular genetic predispositions.
Finally, a better understanding of the genetic and hereditary factors of osteoarthritis may also help provide a more personalized perspective on disease management. By taking into account each patient’s unique genetic profile, doctors can tailor treatment strategies to meet each individual’s specific needs, which could lead to better clinical outcomes and improved quality of life for patients with Alzheimer’s disease. osteoarthritis.
Impact of Lifestyle and Diet
Lifestyle and diet play a crucial role in the development and progression of osteoarthritis. Obesity, in particular, is a major risk factor, as extra weight puts extra pressure on joints, which can accelerate cartilage wear and worsen osteoarthritis symptoms.
A sedentary lifestyle, associated with low physical activity, is often correlated with obesity and also increases the risk of osteoarthritis. Regular exercise, on the other hand, can help strengthen the muscles around the joints, improve their stability and reduce pressure on the cartilage. Activities such as walking, swimming and cycling are particularly beneficial because they are both gentle on the joints and effective in maintaining overall health.
When it comes to diet, adopting a balanced, nutrient-rich approach can play an important role in the prevention and management of osteoarthritis. An anti-inflammatory diet, which emphasizes foods rich in antioxidants, omega-3 fatty acids and other anti-inflammatory nutrients, can help reduce inflammation in the joints and alleviate symptoms of inflammation. osteoarthritis.
Foods such as fruits and vegetables, fatty fish, nuts, seeds and legumes are essential components of an anti-inflammatory diet. On the other hand, processed foods, high in added sugars, saturated fats and additives, can promote inflammation and worsen osteoarthritis symptoms. Reducing the consumption of these foods and favoring healthier options can therefore have a positive impact on joint health.
Additionally, maintaining a healthy body weight through a balanced diet and regular physical activity is essential to reduce pressure on joints and prevent osteoarthritis from getting worse. Weight loss in overweight or obese people can also help relieve osteoarthritis symptoms by reducing the load on affected joints.
Trauma and Joint Injuries
Previous joint injuries, whether they occur during sporting activities or accidents, can have a significant impact on long-term joint health. These injuries can damage the cartilage and surrounding structures, which can lead to premature wear and tear on joints and significantly increase the risk of developing osteoarthritis later in life.
Sports injuries, in particular, are common among young athletes and can have serious consequences for long-term joint health. High-impact sports, such as football, basketball and rugby, are often associated with an increased risk of joint injuries, including sprains, ligament tears and joint fractures. Such injuries can irreversibly damage joint tissue and increase the risk of developing osteoarthritis in the future.
Likewise, accidental joint injuries, such as falls or car accidents, can also increase the risk of osteoarthritis. Joint fractures or dislocations can disrupt the normal structure of the joint and cause early deterioration of cartilage, which can lead to osteoarthritis later in life.
Prevention of joint injuries, especially in young people, is therefore crucial for the long-term preservation of joint health. This involves measures such as appropriate training, use of adequate protective equipment, implementation of safe playing techniques and monitoring of joint health throughout sporting life.
A focus on joint injury prevention can help reduce the long-term burden of osteoarthritis by preserving joint health and minimizing the risk of developing this debilitating disease. By investing in the prevention of joint injuries in youth, it is possible to promote better quality of life and optimal joint health in adulthood and beyond.
Inflammation and Related Diseases
Absolutely, André. Certain inflammatory diseases, such as rheumatoid arthritis (RA), can actually accelerate the process of osteoarthritis. RA is an autoimmune disease characterized by inflammation of the joints, which can lead to progressive destruction of cartilage and bone, ultimately leading to osteoarthritis.
Understanding and managing these related conditions is essential to minimizing the risks associated with osteoarthritis in RA patients. A multidisciplinary approach is often necessary, involving close collaboration between rheumatologists, pain management specialists, and sometimes other healthcare professionals such as osteopaths and nutritionists.
Rheumatologists play a central role in the diagnosis and treatment of RA, as well as the management of joint complications such as osteoarthritis. They may prescribe anti-inflammatory medications and disease-modifying agents to control inflammation and slow disease progression. Additionally, they can closely monitor the condition of the joints and recommend appropriate interventions to prevent or alleviate osteoarthritis.
Pain management specialists can help patients manage painful symptoms associated with osteoarthritis and improve their quality of life. They can offer a variety of treatments, including pain-relieving medications, physical therapies, and stress management techniques, to help patients cope with pain and maintain joint function.
Additionally, a multidisciplinary approach may also include interventions to promote long-term joint health, such as tailored exercise programs, nutrition counseling, and weight management strategies. By addressing all of patients’ needs, it is possible to minimize the risks of osteoarthritis and improve their quality of life despite the presence of inflammatory conditions such as RA.
Daily Prevention Strategie
Prevention of osteoarthritis relies largely on healthy lifestyle choices that aim to maintain joint health and reduce the risk factors associated with this degenerative disease. Here are some key elements of osteoarthritis prevention:
- Regular exercise : Exercise is essential for strengthening the muscles around joints, improving their stability and maintaining their functionality. Low-impact activities, such as swimming, cycling and walking, are particularly beneficial because they stress the joints while minimizing the risk of injury. Regular exercise can also help maintain a healthy body weight, which is crucial for reducing pressure on joints and preventing osteoarthritis.
- Maintaining a healthy weight : Obesity is a major risk factor for osteoarthritis, because excess weight puts additional pressure on the joints, thus accelerating the wear and tear of the cartilage. Maintaining a healthy body weight through a balanced diet and regular physical activity is therefore essential to reduce this risk.
- Adopting an anti-inflammatory diet : A diet rich in fruits, vegetables, oily fish, nuts, seeds and legumes can help reduce inflammation in the joints and alleviate the symptoms of osteoarthritis. Avoiding processed foods, high in added sugars and saturated fat, can also help prevent inflammation and protect joint health.
- Stress management : Chronic stress can contribute to inflammation in the body, which can worsen osteoarthritis symptoms. Practicing stress management techniques such as meditation, yoga, and deep breathing can help reduce stress and ease inflammation, which may benefit long-term joint health.
Testimonials and Success Stories
- Marie, 55 years old : “After years of suffering from joint pain and stiffness due to osteoarthritis, I decided to take matters into my own hands. In collaboration with my doctor and an osteopath, I began a specific exercise program to strengthen my muscles and improve the mobility of my joints. I also changed my diet by adopting an anti-inflammatory diet, rich in fruits, vegetables and fatty fish. These changes have made a huge difference in my daily life. I am now able to do activities I thought I would never be able to do again, and my joint pain has improved significantly. »
- Pierre, 62 years old : “After being diagnosed with osteoarthritis in my knee, I felt a deep sense of despair. But thanks to a proactive approach and close collaboration with my medical team, including an osteopath, I managed to slow the progression of the disease. In addition to following an exercise program supervised by an osteopath, I also benefited from hyaluronic acid injections to relieve joint pain. At the same time, I learned stress management techniques and adopted a positive attitude towards my condition. Today, although I still have to deal with osteoarthritis, I live an active and fulfilled life. »
- Sophie, 45 years old : “I was unexpectedly confronted with osteoarthritis after an injury to my knee during a sports accident. This experience was a real turning point in my life. With the support of my rheumatologist and an osteopath, I completely overhauled my lifestyle. I lost weight thanks to a healthy diet and a proper exercise program. Additionally, I learned to manage my pain through relaxation and meditation techniques. Although osteoarthritis is still present, I feel stronger than ever and am determined to continue living life to the fullest. »
Conclusion
By understanding the multiple factors that influence the progression of osteoarthritis, it becomes possible to take proactive steps to prevent and manage it effectively. Whether through healthy lifestyle choices, appropriate medical treatments, or surgery when necessary, the key lies in a holistic approach to joint health. Taking action today can make a significant difference in future quality of life.
References
- Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010;
- Felson DT, Zhang Y. An update on the epidemiology of knee and osteo hiparthritis with a view to prevention. Arthritis Rheum. 1998;
- Blagojevic M, Jinks C, Jeffery A, Jordan KP. Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2010;
- Conaghan PG. Osteoarthritis in 2012: Parallel evolution of OA phenotypes and therapies. Nat Rev Rheumatol. 2013;
- Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014.