Introduction
The human body is an intricate network of structural and functional systems, and nowhere is this complexity more evident than in the female anatomy. With adaptations that have evolved over millennia, the female body has developed unique features that serve specific reproductive and biomechanical purposes. These adaptations influence not only the function of the reproductive system but also have a ripple effect throughout the entire musculoskeletal system, impacting the way females move, stabilize, and interact with their environment. The connection between anatomical structure and functionality is so intertwined that even small differences can have far-reaching consequences on joint stability, posture, and overall biomechanics.
One of the most obvious anatomical differences between males and females is the structure of the pelvis. The female pelvis is wider, with a broader pelvic inlet and a more circular pelvic brim. This change is an evolutionary adaptation to facilitate childbirth, allowing more space for the passage of a baby. However, the broader pelvis doesn’t just affect reproductive capacity; it also influences the alignment of the lower limbs. The arms naturally angle outward when hanging at the sides, following the curve of the wider pelvis. This positioning may require greater flexibility at the elbows, contributing to a general pattern of hypermobility in the female body. In this case, the elbow joint’s function follows the structure of the pelvis, showcasing how anatomical adaptations for reproduction influence the upper limbs.
Another example of how structure influences function can be seen in the lumbar spine. Females generally have a more pronounced lumbar lordosis, or inward curve of the lower back, compared to males. This increased curvature is linked to an anterior pelvic tilt, which helps balance the weight of a growing fetus during pregnancy. The structural adaptation allows women to maintain balance and stability as their center of gravity shifts forward. However, this increased curvature has biomechanical consequences: the forward shift in weight distribution places more stress on the knees, potentially contributing to forward knee instability. Additionally, muscle imbalances often develop as a result, with tight hip flexors and overactive quadriceps putting further strain on the knee joint. Here, we see how a structural feature meant to support pregnancy can also increase the risk of lower body injuries.
The wider pelvis in females also affects the Q-angle, which is the angle formed between the quadriceps muscle and the patellar tendon. A greater Q-angle is observed in females due to the pelvis’s increased width. While this adaptation helps distribute weight more evenly through the lower body, it also affects knee mechanics. The greater angle can make women more susceptible to knee injuries, such as patellofemoral pain syndrome and anterior cruciate ligament (ACL) tears. The structure of the pelvis, therefore, has a direct impact on the stability and function of the knee, influencing how women perform various movements, from running to squatting.
Hip joint mobility is another area where structural differences between males and females are apparent. The female acetabulum, or hip socket, is shallower and more laterally oriented, allowing for a wider range of motion. This increased hip mobility is beneficial for activities like childbirth but can also lead to greater hip instability. Women are more prone to conditions such as hip impingement and labral tears, highlighting the trade-off between flexibility and stability. These anatomical differences in the hips also influence the mechanics of movements like squats, lunges, and hip rotations, requiring women to adopt different strategies for stabilization compared to men.
Beyond the lower body, differences in the thoracic cage also affect upper body function. Females typically have a narrower thoracic cage with more flexible ribs, allowing for greater chest expansion. This flexibility can influence breathing patterns and upper body biomechanics, affecting how women perform activities that require upper body strength or endurance. The thoracic cage’s structure impacts shoulder positioning and arm swing, demonstrating yet another way that structural differences affect function.
Additionally, foot and ankle alignment can be influenced by the wider female pelvis. The pelvis’s shape can lead to differences in lower limb mechanics, such as greater pronation of the foot. This tendency can affect balance, gait, and even increase the risk of foot and ankle injuries. Women may require different footwear or training techniques to accommodate these structural differences.
Finally, hormonal influences, such as estrogen, play a significant role in ligament laxity. These hormones make the connective tissue more elastic, which is essential for childbirth but can lead to generalized joint hypermobility throughout the body. This laxity is beneficial in terms of flexibility but comes with the cost of increased risk for joint injuries. Hormones like estrogen and relaxin have a systemic effect, showcasing how reproductive needs shape overall musculoskeletal function.
The female body’s unique anatomy highlights the intricate connection between structure and function, where evolutionary adaptations for reproduction and childbirth influence biomechanics, stability, and flexibility across the entire body.
Wider Female Pelvis and Its Implications
The female pelvis is one of the most distinct anatomical differences between males and females, designed to fulfill reproductive functions like carrying and delivering a baby. Over time, evolution has shaped the female pelvis to be wider and more rounded, with a broader pelvic inlet, shallower depth, and a larger subpubic angle. These structural adaptations have ripple effects throughout the body, influencing alignment, joint positioning, and overall biomechanics. What’s remarkable is how the design of the pelvis impacts areas seemingly unrelated to reproduction, such as the positioning of the arms and the mobility of the elbow joints.
How a Wider Pelvis Affects Body Alignment
The most immediate and apparent consequence of having a wider pelvis is its effect on body alignment. The broader pelvic bones cause the lower limbs to angle inward slightly to maintain proper balance and load distribution. This angling of the legs results in what’s known as a greater Q-angle, which is the angle formed between the femur and the tibia. The Q-angle is significantly wider in females compared to males, which influences the way the lower body absorbs shock and distributes weight during activities like walking, running, or standing. The inward angling of the femur puts additional stress on the knee joints, making them more susceptible to injury, but it is an unavoidable consequence of the pelvis’s wider structure.
The wider pelvis also tilts slightly forward, which changes the body’s center of gravity. This forward tilt, combined with a more pronounced lumbar lordosis, helps balance the weight distribution during pregnancy. However, even outside of pregnancy, this alignment impacts posture and the way forces are transmitted through the spine and hips. For instance, the anterior pelvic tilt associated with a wider pelvis can lead to muscle imbalances, such as tight hip flexors and weak gluteal muscles. These imbalances often require compensation from other muscle groups, which can affect overall movement patterns and even contribute to lower back pain.
The Impact on Arm Positioning and Elbow Hypermobility
What’s fascinating about the human body is the intricate ways in which one structural adaptation can influence multiple parts of the body. The wider pelvis in females, designed primarily to facilitate childbirth, has far-reaching impacts on biomechanics, extending all the way up to the positioning and movement of the arms. When the arms hang naturally at the sides, they don’t fall perfectly straight down as they might in a narrower-hipped frame; instead, they angle slightly outward. This outward angle serves a practical purpose, allowing the arms to avoid constant contact or rubbing against the sides of the pelvis. Such positioning supports a more fluid range of arm movements, especially in tasks requiring the arms to swing freely without obstruction.
This outward angling of the arms also necessitates adjustments in the flexibility and mobility of the elbow joint. To accommodate the natural width of the female pelvis, the elbow joint in women often exhibits a greater carrying angle—an angle between the long axes of the arm and forearm that allows the arms to angle away from the body. This increased carrying angle in females has been documented in multiple studies and is thought to be an adaptation that helps the arm avoid contact with the hips during movement (Van Roy et al., 2005), (Bari et al., 2015).
The increased carrying angle is not merely a coincidental trait but likely evolved as a biomechanical adaptation to complement pelvic width, which itself is a critical component of the female skeletal structure designed to support reproductive functions. A study by Golden et al. (2007) confirms that the carrying angle is generally larger in females than in males, facilitating a wider arm swing that avoids the hips and allows smoother movement (Golden et al., 2007).
The elbow joint’s increased carrying angle and flexibility provide a greater range of motion, enabling the arm to follow the outward angle necessitated by the wider pelvis. However, this adaptation is not without its drawbacks. A greater carrying angle has been associated with increased risks of musculoskeletal issues, including ulnar neuropathy and lateral epicondylitis due to the added stress on certain arm muscles and tendons (Chang et al., 2008). This highlights the biomechanical trade-offs in the human body: while the increased carrying angle is beneficial for unrestricted arm movement, it can also make the joint more susceptible to overuse injuries.
Additionally, this adaptation is a perfect illustration of a fundamental principle in biomechanics: structure drives function. The wider female pelvis, while essential for reproductive purposes, affects the alignment and movement of other body parts, including the arms and elbows. The requirement for a broader pelvic outlet influences how the entire musculoskeletal system organizes itself to maintain balance and functional efficiency. In this case, the need for a wider pelvis to facilitate childbirth cascades through the body, affecting the alignment and mobility of upper limbs. Consequently, the elbow joint’s greater carrying angle is not an isolated characteristic but rather an adaptation in response to a larger structural requirement. This connection underscores how the body’s design is a system of interrelated parts, each adapting to support one another in a coordinated, holistic manner.
For instance, in everyday activities like lifting, reaching, or even walking, the interaction between a wider pelvis and increased elbow carrying angle allows for a smooth, natural flow in arm movement. Such adaptability is critical for the efficiency of daily tasks and the broader physical agility that humans exhibit. However, the increased flexibility also highlights the body’s inherent compromises, balancing between mobility and stability. Understanding this dynamic relationship between the pelvis and upper limb biomechanics not only deepens our appreciation of the female musculoskeletal system but also sheds light on the origins of certain joint vulnerabilities common in women.
Here are some references that discuss the increased elbow carrying angle and its association with wider pelvis or sexual dimorphism in females:
- Van Roy, P., Baeyens, J., Fauvart, D., Lanssiers, R., & Clarijs, J. (2005). Arthro-kinematics of the elbow: study of the carrying angle. Ergonomics, 48(12), 1645-1656. This study shows that females generally have a greater carrying angle than males, which allows the arm to swing freely, avoiding contact with the wider pelvis in females. Link to paper.
- Bari, W., Alam, M., & Omar, S. (2015). Goniometry of elbow carrying angle: a comparative clinical study on sexual dimorphism in young males and females. International Journal of Research in Medical Sciences, 3(12), 3482-3484. This study confirms that the carrying angle is generally greater in females, likely due to sexual dimorphism, which facilitates a broader arm swing without hitting the hips. Link to paper.
- Golden, D., Jhee, J. T., Gilpin, S. P., & Sawyer, J. (2007). Elbow range of motion and clinical carrying angle in a healthy pediatric population. Journal of Pediatric Orthopaedics B, 16(2), 144-149. This study highlights that the carrying angle increases with age and is typically larger in females, contributing to an outward angle that facilitates arm movement around the wider pelvic structure. Link to paper.
- Chang, C.-W., Wang, Y.-C., & Chu, C.-H. (2008). Increased Carrying Angle is a Risk Factor for Nontraumatic Ulnar Neuropathy at the Elbow. Clinical Orthopaedics and Related Research, 466(10), 2190-2195. This paper discusses the physiological implications of a greater carrying angle, noting it as a common feature in females that may contribute to musculoskeletal adaptations in response to broader pelvic structure. Link to paper.
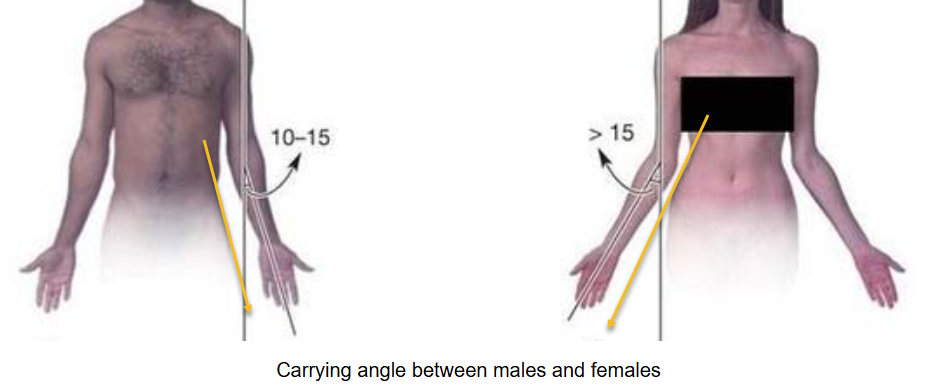
This adaptation, while biomechanically advantageous, comes with certain challenges. For instance, the enhanced elbow flexibility or hypermobility that allows the arms to maintain this angle can lead to increased susceptibility to joint instability and related injuries, such as dislocations or ligament strains. In contrast, males typically have a narrower pelvis and a smaller carrying angle (10-15 degrees), resulting in less demand for hypermobility in the elbows.
Overall, the image and accompanying explanation highlight a clear example of how structural differences between genders influence musculoskeletal function. The coordination between pelvic width and elbow joint flexibility exemplifies how the human body adapts to maintain efficiency and balance in movement.
Like our GPT? Try our full AI-powered search engine and academic features for free at
Function Following Structure: A Biomechanical Perspective
From a biomechanical standpoint, the idea that “function follows structure” is a central theme in understanding how the female body operates. The wider pelvis influences not only the lower body but also the alignment and movement patterns of the upper body. The arm’s outward angling and the requirement for greater elbow mobility highlight how different parts of the musculoskeletal system adapt to maintain overall balance and fluidity in movement. This interconnection is essential for activities that involve coordinated, full-body motion, such as running, carrying, or lifting.
The principle of function following structure is also evident in how the body compensates for the wider pelvis’s impact on stability. The lower back, for example, develops a more pronounced lumbar lordosis to balance the forward tilt of the pelvis. This curvature helps maintain an upright posture, but it can also increase the risk of lower back pain and other spinal issues. Similarly, the knees have to deal with the altered load distribution caused by the inward angle of the femur. The greater Q-angle predisposes women to knee injuries, such as patellofemoral pain syndrome or ACL tears, but it also ensures that the body remains stable and efficient during walking and running.
In addition, the wider pelvis affects gait patterns. Women often exhibit a different walking style compared to men, characterized by a wider stance and more hip movement. This difference in gait is necessary to accommodate the pelvic structure and maintain balance, especially when shifting weight from one leg to the other. The pelvis’s design also influences the activation of muscles in the lower body, with a greater emphasis on hip abductors and stabilizers to prevent the knees from caving inward during movement. This interconnectedness illustrates how every anatomical feature is optimized for specific functions, even if it means creating vulnerabilities in other areas.
The structural features of the female pelvis and their far-reaching effects underscore the complexity of human anatomy. What may seem like isolated traits—like elbow hypermobility or lower back curvature—are actually part of a finely tuned system where every component works together to accommodate the demands of pregnancy, childbirth, and daily life. This holistic approach to understanding the body helps explain why certain injury patterns and movement tendencies are more common in females, providing insights into both preventative care and the evolution of human biomechanics.
From a biomechanical perspective, a wider pelvis in females has several consequences. Firstly, it affects lower body alignment and load distribution. The increased pelvic width creates a larger Q-angle, the angle at which the femur meets the pelvis. This alteration predisposes women to certain knee injuries, such as patellofemoral pain syndrome and anterior cruciate ligament (ACL) tears, because the inward angle places more stress on the knee joint.
Additionally, the wider pelvis impacts gait mechanics. Women often exhibit a different walking style, with more lateral hip movement to maintain balance and stability. This difference requires greater activation of the hip abductors and stabilizer muscles, which helps to prevent the knees from collapsing inward during movement. However, it can also contribute to muscle fatigue and imbalances over time.
Overall, these structural differences underscore how the pelvis influences posture, stability, and risk of injury, demonstrating the concept that anatomical structure directly affects biomechanical function.
Increased Lumbar Lordosis and Knee Instability
Lumbar lordosis, the inward curve of the lower spine, is naturally more pronounced in females due to the structural demands of the pelvis and reproductive system. This anatomical feature is not simply a passive adaptation but plays a significant role in maintaining balance and stability, especially when considering the potential weight and postural changes associated with pregnancy. However, the effects of increased lumbar lordosis extend far beyond the lower back, influencing the alignment and stability of other joints, including the knees. This interrelationship between the spine, pelvis, and lower extremities showcases the complex biomechanical chain that connects different regions of the body.
The Relationship Between Lumbar Lordosis and Anterior Pelvic Tilt
Lumbar lordosis is intricately tied to the position of the pelvis. In females, the pelvis is naturally tilted more anteriorly (forward) to accommodate the wider pelvic inlet and facilitate childbirth. This anterior pelvic tilt accentuates the curve of the lower back, resulting in a more pronounced lumbar lordosis. The curvature is not just a structural necessity but also a way for the body to maintain an upright posture. As the pelvis tilts forward, the lower spine compensates by curving inward to keep the upper body balanced over the hips. This alignment is essential for distributing weight evenly through the spine and lower body.
Muscle imbalances play a critical role in this posture. The iliopsoas and rectus femoris muscles, located at the front of the hip, tend to become tight and overactive due to the pelvic tilt. This tightness pulls the pelvis downward and forward, exacerbating the curve in the lower spine. Meanwhile, the erector spinae muscles in the lower back work harder to maintain an upright posture, adding more stress to the lumbar region.
These adaptations, while necessary for stability and balance, can lead to biomechanical challenges. Chronic anterior pelvic tilt and increased lordosis often result in lower back pain, hip discomfort, and an increased risk of injury. Addressing these issues typically involves strengthening the core and gluteal muscles while stretching the hip flexors to restore a more neutral pelvic alignment.
However, the anterior pelvic tilt associated with increased lumbar lordosis shifts the body’s center of gravity forward. This forward shift places additional stress on the lower back and hips, and it also affects the mechanics of the lower extremities. To compensate for this altered center of gravity, the knees may be forced into a hyperextended or unstable position. The forward tilt of the pelvis can also increase the load on the quadriceps and reduce the efficiency of the gluteal and hamstring muscles, leading to an imbalance in the forces acting on the knees.
How Lumbar Curvature Affects Knee Stability and Alignment
The forward tilt of the pelvis and increased lumbar lordosis influence knee alignment and stability in several significant ways. As the pelvis tilts forward, the femur tends to rotate inward, which can cause the knees to angle slightly inward as well, a condition known as “knee valgus” or “knock-knees.”
The anterior tilt of the pelvis, common in females due to the demands of balancing a wider pelvic structure, further influences the alignment of the femur and knee joint. This inward rotation of the femur increases the stress placed on the medial side of the knee and can affect the knee’s stability. Consequently, females are more susceptible to knee-related injuries such as patellofemoral pain syndrome, ACL tears, and overuse injuries.
This biomechanical setup requires the surrounding muscles, like the hip abductors and external rotators, to work harder to maintain knee stability. However, when these muscles are weak or imbalanced, the risk of injury increases, emphasizing the importance of targeted strength and conditioning to mitigate these structural vulnerabilities.
This inward angling places extra stress on the medial (inner) side of the knee joint and the supporting ligaments, making the knees more prone to instability. Over time, this misalignment can contribute to conditions such as patellofemoral pain syndrome, where the kneecap doesn’t track properly, or even more severe injuries like ACL tears.
Additionally, the altered biomechanics affect the way forces are transmitted through the knee joint during activities such as walking, running, or jumping. The knee is designed to act as a shock absorber, efficiently dissipating the forces generated by movement. However, when the alignment is off due to pelvic and spinal imbalances, the knee joint becomes less effective at absorbing these forces. This can lead to an increased risk of joint degeneration and overuse injuries, especially in high-impact activities. Women are particularly vulnerable to knee instability, partly because of the anatomical relationship between the pelvis, lumbar spine, and lower extremities.
Muscle Imbalances Resulting From Postural Changes
One of the significant consequences of increased lumbar lordosis and anterior pelvic tilt is the development of muscle imbalances. These imbalances occur because certain muscle groups become overactive or shortened, while others become underactive or lengthened. For instance, the hip flexors, which include muscles like the iliopsoas and rectus femoris, are often tightened due to the forward tilt of the pelvis. These muscles pull the pelvis downward and forward, exacerbating the anterior pelvic tilt and reinforcing the increased curvature of the lower back.
On the opposite side, the gluteal muscles and the hamstrings tend to become weakened or underactive. The gluteal muscles are crucial for stabilizing the pelvis and supporting the lower back, while the hamstrings help control hip and knee movement. When these muscles are not functioning optimally, the burden of stabilization shifts to other muscle groups, like the quadriceps and lower back extensors. This compensatory pattern can lead to overuse injuries and chronic pain, particularly in the lower back and knees.
The quadriceps, in particular, become overactive in this scenario, which has a direct impact on knee stability. When the quadriceps dominate the mechanics of the lower body, they exert excessive force on the patella (kneecap), increasing the risk of knee pain and instability. The imbalance between the quadriceps and the weaker hamstrings disrupts the natural function of the knee joint, making it more susceptible to injury. Additionally, weak gluteal muscles fail to provide adequate support for the pelvis, causing further strain on the lower spine and exacerbating the anterior pelvic tilt.
The effects of these muscle imbalances are compounded during dynamic activities. For example, when running or jumping, the knees are subjected to increased forces, and the lack of proper muscular support can cause the knee joint to become unstable. Athletes and physically active individuals who exhibit these postural imbalances are often at a higher risk of knee injuries. Corrective exercises that target the gluteal muscles and hamstrings, while stretching the hip flexors, are often recommended to restore balance and reduce the risk of injury.
Q-Angle and Knee Vulnerability
One of the most significant structural differences between males and females that impacts lower body mechanics is the Q-angle. The Q-angle, or quadriceps angle, is the angle formed between the line of the quadriceps muscle and the patellar tendon. It describes how the femur (thigh bone) angles inward from the hip to the knee. In general, females have a greater Q-angle compared to males, primarily because of the wider structure of the female pelvis. This difference is crucial to understanding why women are more prone to certain knee injuries and how the biomechanics of the lower body are adapted to accommodate these structural realities.
Understanding the Greater Q-Angle in Females
The greater Q-angle in females is a direct consequence of the pelvic width required for childbearing. The female pelvis is designed to be wider to allow for the passage of a baby during childbirth, and this broader pelvic structure influences the alignment of the femur. As the femur extends downward from a wider pelvis, it angles inward more sharply to meet the knee, creating a larger Q-angle. While the average Q-angle in males is around 10 to 15 degrees, it can be 15 to 20 degrees or even higher in females.
This increase in the Q-angle has several biomechanical implications. A larger Q-angle alters the way forces are transmitted through the knee joint and how the quadriceps muscles pull on the patella (kneecap). The inward angle can create a lateral pull on the patella, making it more likely to be displaced or misaligned. This lateral force can increase the risk of patellofemoral pain syndrome, where the cartilage under the kneecap becomes irritated, leading to pain and discomfort during activities like running, squatting, or climbing stairs.
The Q-angle is also linked to the positioning and loading of the knee joint. Because the knee joint is more prone to inward angulation, there is a greater tendency for valgus collapse, a condition where the knees cave inward, especially during activities that involve jumping or sudden direction changes. This inward collapse puts extra stress on the medial (inner) structures of the knee, such as the meniscus and ligaments, making them more susceptible to injury.
How It Influences Knee Mechanics and Risk of Injury
The mechanics of the knee joint are significantly influenced by the alignment created by the Q-angle, an angle formed between the quadriceps muscles and the patellar tendon. This angle plays a crucial role in determining the biomechanical behavior of the knee joint, particularly affecting the distribution of forces during weight-bearing activities. When the Q-angle is greater, as often observed in females, the natural biomechanics of the knee can be disrupted. This disruption may lead to uneven force distribution, increased pressure on specific areas within the joint, and a heightened risk of various injuries.
One notable injury associated with an increased Q-angle is the anterior cruciate ligament (ACL) tear. Research indicates that women are two to eight times more likely than men to suffer an ACL injury, with the Q-angle being a key contributing factor to this elevated risk (Imhoff et al., 2020). The greater Q-angle leads to an inward angling of the femur and knee valgus positioning, which significantly strains the ACL, particularly during high-impact activities or sudden changes in direction. When the knee collapses inward, the stress on the ACL increases, often resulting in a tear. This type of injury is prevalent in sports like soccer, basketball, and volleyball, which involve frequent pivoting and sudden directional shifts (Kent et al., 2018).
Patellar tracking disorders are also commonly linked to a greater Q-angle. The increased lateral pull on the patella caused by the inward angling of the femur can lead to patellar instability or even dislocation. Studies show that individuals with a high Q-angle experience lateral patellar displacement and increased patellofemoral contact pressures, which can contribute to discomfort and pain around the kneecap, especially during activities requiring repetitive knee flexion or substantial knee loads (Mizuno et al., 2001). Over time, this misalignment can cause wear and tear on the cartilage, potentially leading to conditions such as osteoarthritis, as excessive lateral pressure accelerates joint degeneration (Tsakoniti et al., 2008).
Additionally, the greater Q-angle impacts muscle activation patterns around the knee. This altered alignment can affect the quadriceps, hamstrings, and gluteal muscles’ ability to coordinate effectively in stabilizing the knee joint. For instance, an increased Q-angle often leads to overactivation of the quadriceps while reducing the engagement of the hamstrings and gluteal muscles, which are essential for knee stability. This imbalance places further strain on the knee, making it more susceptible to injuries during activities that require explosive power or quick deceleration. Research suggests that such muscle imbalances can increase knee instability, which is a significant factor in injuries among athletes (Saç, 2018).
In conclusion, the Q-angle is an essential parameter in understanding knee joint biomechanics, especially in relation to injury risks like ACL tears and patellar tracking issues. A larger Q-angle, which is more common in females, disrupts the knee’s natural alignment, increasing the likelihood of injury due to uneven force distribution and muscle imbalances. Addressing these risks through targeted strengthening exercises, particularly for the hamstrings and gluteal muscles, may help in reducing knee instability and mitigating injury risk associated with a high Q-angle.
- Imhoff, F., Cotic, M., Dyrna, F., Cote, M., Diermeier, T., Achtnich, A., & Beitzel, K. (2020). Dynamic Q-angle is increased in patients with chronic patellofemoral instability and correlates positively with femoral torsion. Knee Surgery, Sports Traumatology, Arthroscopy, 29, 1224-1231. Link to paper.
- Kent, R. N., Amirtharaj, M. J., Hardy, B., Pearle, A., Wickiewicz, T., & Imhauser, C. (2018). Anterior laxity, lateral tibial slope, and in situ ACL force differentiate knees exhibiting distinct patterns of motion during a pivoting event: A human cadaveric study. Journal of biomechanics, 74, 9-15. Link to paper.
- Mizuno, Y., Kumagai, M., Mattessich, S., Elias, J., Ramrattan, N., Cosgarea, A., & Chao, E. (2001). Q‐angle influences tibiofemoral and patellofemoral kinematics. Journal of Orthopaedic Research, 19, 131-136. Link to paper.
- Tsakoniti, A. E., Stoupis, C., & Athanasopoulos, S. (2008). Quadriceps cross-sectional area changes in young healthy men with different magnitudes of Q angle. Journal of Applied Physiology, 105(3), 800-804. Link to paper.
- Saç, A. (2018). Correlation between the Q angle and isokinetic knee strength and muscle activity. Turkish Journal of Physical Medicine and Rehabilitation, 64(4), 308-313. Link to paper.
Adaptations for Lower Body Movement
Despite the challenges posed by a greater Q-angle, the female body has adapted to allow for efficient movement and stability. These adaptations often involve changes in muscle recruitment patterns and strategies to reduce the risk of knee injuries. One key adaptation is the emphasis on strengthening the muscles that stabilize the pelvis and knee joint, such as the gluteus medius, which plays a critical role in controlling hip movement and preventing knee valgus.
Strengthening the glutes and hip abductors can help mitigate the inward collapse of the knees and provide better alignment during movement. Physical therapy and strength training programs for women often focus on developing these muscle groups to compensate for the structural disadvantages created by the Q-angle. Core stability is another crucial component, as a strong core can help maintain proper pelvic alignment and reduce the stress placed on the knees.
Biomechanical training, such as teaching proper landing techniques and jump mechanics, can also be effective in reducing knee injury risk. For example, teaching athletes to land with their knees aligned over their toes, rather than allowing them to collapse inward, can help distribute forces more evenly and protect the ACL. Wearing supportive footwear and using orthotics to control foot pronation can also play a role in improving lower body alignment and reducing stress on the knee joint.
Additionally, many women benefit from flexibility training that targets the hip flexors and quadriceps. These muscles can become tight due to the alignment of the pelvis and femur, exacerbating knee issues. Stretching and mobility exercises can help maintain a healthy range of motion and prevent compensatory movement patterns.
Overall, while the greater Q-angle in females presents biomechanical challenges, understanding these vulnerabilities and implementing targeted adaptations can significantly reduce the risk of injury. It’s a complex interplay of structure and function, highlighting the importance of tailored training and injury prevention strategies for women.
Hip Joint Mobility and Functional Benefits
The hip joint, as a central component of the musculoskeletal system, plays a crucial role in enabling a wide range of movements, from walking and running to squatting and rotating. In females, the structural design of the hip joint differs significantly from that of males, and these differences are closely related to reproductive functions. The female hip joint is designed to provide greater mobility, which is essential for pregnancy and childbirth. However, while this increased range of motion offers several functional advantages, it also comes with certain biomechanical drawbacks, including a higher risk of hip instability and injury.
Structural Differences in the Female Hip Joint
The primary structural differences in the female hip joint stem from the broader pelvis required to accommodate childbirth. The female pelvis is wider and more rounded, with a larger pelvic inlet and a greater subpubic angle. These characteristics influence the orientation and depth of the hip socket, or acetabulum. In females, the acetabulum is often more shallow and oriented slightly forward and laterally compared to the deeper and more laterally positioned acetabulum in males. This shallow and forward-facing socket provides greater hip mobility, allowing for a wider range of motion in multiple planes, such as flexion, extension, abduction, and rotation.
The femoral head, which fits into the acetabulum, also reflects these differences. The angle of inclination of the femur and the femoral neck’s angle relative to the shaft of the femur are slightly different in females. These variations contribute to a greater range of motion in the hips but can also predispose females to specific hip-related issues. Additionally, the connective tissues and ligaments surrounding the hip joint tend to be more elastic in females, further enhancing mobility but often at the cost of joint stability.
Advantages and Disadvantages of Greater Hip Mobility
One of the primary advantages of greater hip mobility in females is the body’s ability to accommodate the physical demands of pregnancy and childbirth. During pregnancy, the hormone relaxin is released, causing the ligaments and connective tissues to become even more elastic. This hormonal adaptation allows the pelvis to expand and provides the flexibility needed to support the weight of the growing fetus and the eventual process of labor and delivery. Without this mobility, childbirth would be significantly more difficult and dangerous.
Beyond reproductive benefits, greater hip mobility also provides functional advantages in daily activities and athletic performance. A wide range of hip motion is beneficial for movements that require flexibility and adaptability, such as squatting, lunging, dancing, and performing yoga. In sports, increased hip mobility allows for more fluid transitions, better agility, and the ability to perform complex movements like lateral shuffles, pivots, and rotations. For dancers, gymnasts, and athletes in sports like soccer and basketball, this flexibility can be a competitive advantage, enhancing performance and allowing for a broader repertoire of movements.
However, the advantages of hip mobility come with a trade-off. The shallow and forward-facing acetabulum, combined with more elastic ligaments, increases the risk of hip instability. The hip joint, while highly mobile, is less inherently stable than in males, who have deeper hip sockets and tighter connective tissues. This predisposes females to conditions like hip dysplasia, where the femoral head does not sit properly in the acetabulum, and hip impingement, which can cause pain and limit movement.
Risk of Hip Instability and Common Injuries
Hip instability is a significant concern for females, especially those who engage in sports or activities that involve repetitive hip movements or sudden changes in direction. The shallow acetabulum makes it easier for the femoral head to move out of place, leading to partial or complete dislocations. In addition, activities that place high stress on the hip joint, such as running, jumping, or weightlifting, can exacerbate this instability and lead to chronic pain or acute injuries.
Labral tears are a common injury associated with hip instability. The labrum is a ring of cartilage that surrounds the acetabulum, providing a seal and adding stability to the hip joint. In females with increased hip mobility, the labrum is more susceptible to injury, especially during movements that involve excessive rotation or deep hip flexion. A labral tear can cause symptoms such as hip pain, clicking, or a feeling of the hip joint catching or locking, and it often requires medical intervention.
Hip impingement, or femoroacetabular impingement (FAI), is another condition that can occur due to the structural differences in the female hip joint. In FAI, abnormal contact between the femoral head and the acetabulum can cause joint damage, particularly in individuals who repeatedly move their hips into extreme positions, such as deep squats or high kicks. This condition can lead to chronic pain and limit the hip’s range of motion, and it may eventually contribute to the development of osteoarthritis in the hip joint.
Tendinopathies and bursitis are also more prevalent in females due to the increased stress placed on the tendons and bursae surrounding the hip. The iliotibial (IT) band, hip flexor tendons, and gluteal tendons can become overused or irritated, causing pain and inflammation. These issues are often exacerbated by muscle imbalances, where the stabilizing muscles of the hip, such as the gluteus medius and gluteus minimus, are not strong enough to support the joint properly. This imbalance can cause excessive strain on the hip joint and surrounding structures, leading to chronic conditions.
Preventative measures and targeted training can help mitigate some of these risks. Strengthening the muscles that support the hip joint, such as the glutes, hamstrings, and core muscles, can improve stability and reduce the likelihood of injury. Additionally, flexibility training that focuses on maintaining a healthy range of motion while avoiding hypermobility can be beneficial. Physical therapists and trainers often emphasize proper movement mechanics and joint stabilization exercises to help women maintain hip health and prevent injuries.
Thoracic Cage Structure and Shoulder Mechanics
The thoracic cage, or ribcage, serves as a protective shield for vital organs, like the heart and lungs, and also plays a pivotal role in upper body mechanics and respiration. In females, the thoracic cage is uniquely shaped, with structural differences that influence both breathing patterns and the mechanics of the shoulder complex. Understanding these differences provides insights into why women may be more prone to certain postural tendencies, such as rounded shoulders, and how these anatomical characteristics impact movement and stability.
Additionally, the diaphragm, the primary muscle of respiration, is about 9% shorter in females than in males. This shorter diaphragm length also contributes to differences in breathing efficiency and lung capacity between the sexes. As a result, females may rely more on thoracic (chest) breathing rather than diaphragmatic (abdominal) breathing compared to males, who can utilize deeper and more efficient diaphragmatic breaths.
These anatomical differences in the rib cage and diaphragm reflect how the respiratory system has adapted in females, influencing not only lung function but also athletic performance and endurance. Understanding these variations is crucial in fields such as medicine, sports science, and ergonomics to tailor training and therapeutic approaches accordingly.
Differences in Thoracic Cage Shape
To expand on the discussion of structural differences between male and female ribcages, recent studies highlight several anatomical variations and their biomechanical implications. One of the most prominent distinctions is the overall size and shape of the ribcage. Females tend to have a narrower and more rounded ribcage, with ribs sloping more downward compared to the broader and more rectangular ribcage observed in males. This narrower ribcage in females has evolved, in part, to accommodate a larger pelvic region, essential for reproductive functions. This adaptation, however, influences not only the lower body but also affects upper body biomechanics, particularly in terms of shoulder and thoracic flexibility.
The narrower ribcage affects the positioning of the shoulder girdle, specifically the clavicles (collarbones) and scapulae (shoulder blades), which are positioned more laterally and often rotate slightly forward. This positioning impacts shoulder joint mechanics, particularly the glenohumeral joint, which relies on proper scapular movement for stability and a full range of motion. The lateral scapular positioning helps facilitate smoother arm movement, although it slightly limits the structural support, potentially contributing to increased susceptibility to shoulder injuries (García‐Martínez et al., 2019).
The ribcage’s flexibility, which is generally greater in females, also plays a crucial role in accommodating these structural requirements. This flexibility is influenced by hormonal factors, such as estrogen, which increases the elasticity of connective tissues and cartilage. Such flexibility is especially beneficial during pregnancy, allowing for greater thoracic expansion to support respiratory needs. However, it can reduce upper body stability, impacting how force is distributed across the thoracic cage during physical activities. This increased compliance in the female thorax has been shown to contribute to greater respiratory rib movement compared to males, which is an adaptation for accommodating increased oxygen needs in scenarios like pregnancy (Bellemare et al., 2003).
The narrower ribcage in females positions the shoulders at a slight outward angle, making the shoulder girdle more prone to forward rotation or “rounded shoulders.” This posture, often accentuated by lifestyle factors like prolonged sitting or certain occupational activities, can lead to postural imbalances and upper back strain. Rounded shoulders are associated with weakened upper back muscles and tight pectoral muscles, both of which contribute to upper body discomfort and decreased shoulder mobility. Understanding these structural differences highlights the importance of targeted exercises to strengthen the upper back and improve postural alignment in women, helping to mitigate the tendency for rounded shoulders.
Moreover, sexual dimorphism in the thoracic cage has functional implications beyond respiration. The differences in rib orientation and flexibility affect thoracic stability and shoulder mechanics. A study by García‐Martínez et al. (2016) revealed that females’ ribcages, which are more flexible and adapted for greater respiratory movement, tend to have a smaller thoracic volume, necessitating increased inspiratory muscle engagement. This additional engagement can lead to a more extensive use of accessory muscles during breathing, which may affect shoulder stability during high-impact activities (García‐Martínez et al., 2016).
These structural and functional adaptations demonstrate the intricate relationship between ribcage morphology and biomechanics. The ribcage not only supports respiratory function but also plays a pivotal role in shoulder stability and overall upper body mechanics. This connection between form and function underscores the broader principle in anatomy: structural adaptations in one area often lead to compensatory changes in other areas to maintain balance and functionality.
- García‐Martínez, D., Bastir, M., Torres-Tamayo, N., O’Higgins, P., Torres-Sánchez, I., García-Río, F., & Heuzé, Y. (2019). Three-dimensional analysis of sexual dimorphism in ribcage kinematics of modern humans. American Journal of Physical Anthropology, 169(2), 348-355. Link to paper.
- Bellemare, F., Jeanneret, A., & Couture, J. (2003). Sex differences in thoracic dimensions and configuration. American Journal of Respiratory and Critical Care Medicine, 168(3), 305-312. Link to paper.
- García‐Martínez, D., Torres-Tamayo, N., Torres-Sánchez, I., García-Río, F., & Bastir, M. (2016). Morphological and functional implications of sexual dimorphism in the human skeletal thorax. American Journal of Physical Anthropology, 161(3), 467-477. Link to paper.
How It Influences Upper Body Movement and Breathing Patterns
The shape and flexibility of the female thoracic cage have a direct impact on upper body movement and shoulder mechanics. The downward-sloping ribs and narrower ribcage can alter how the scapulae sit and move in relation to the ribcage. Because the shoulder blades are positioned more laterally, it can be challenging for women to achieve full scapular retraction, which is the movement where the shoulder blades are pulled back and together. This affects the function of stabilizing muscles like the rhomboids, trapezius, and serratus anterior, which are essential for maintaining proper shoulder alignment and supporting overhead movements.
In activities like weightlifting, swimming, or even daily tasks that involve lifting or reaching, this altered scapular positioning can make it harder to maintain optimal shoulder mechanics. Women may be more susceptible to developing shoulder impingements or muscle imbalances if the stabilizing muscles are not adequately engaged or strengthened. For example, if the upper trapezius becomes overactive while the lower trapezius and rhomboids are weak, it can lead to dysfunctional movement patterns and increased risk of injury.
Breathing patterns are also influenced by the thoracic cage’s shape. Females may be more prone to upper chest breathing rather than diaphragmatic breathing, partly due to the more rounded and flexible ribcage. This breathing style can engage accessory muscles, such as the scalenes and sternocleidomastoid, leading to tension in the neck and upper shoulders. Over time, this can contribute to postural issues and discomfort in the upper body.
Impact on Shoulder Posture: Rounded Shoulders
A key postural tendency associated with the shape of the female thoracic cage is the development of rounded shoulders. The downward slope and narrower shape of the ribcage predispose the shoulder girdle to a forward position. The clavicles and acromion process of the scapulae may naturally sit in a slightly more downward or forward orientation, making it easier for the shoulders to round forward, especially if there is muscle tightness in the chest or weakness in the upper back muscles.
This postural tendency is further exacerbated by modern habits, such as prolonged sitting, working at a computer, or using mobile devices, which encourage a forward head and rounded shoulder posture. When the shoulders are rounded, the muscles of the upper back, including the rhomboids, lower trapezius, and posterior deltoids, are often lengthened and weakened. Meanwhile, the chest muscles, such as the pectoralis major and minor, may become shortened and tight, pulling the shoulders even further forward.
The structural design of the ribcage makes it challenging to counteract this natural tendency without targeted strength and flexibility training. Exercises that focus on strengthening the upper back and retracting the scapulae are essential to improve posture and prevent dysfunction. Movements like scapular retractions, rows, and shoulder blade squeezes can help counterbalance the pull of tight chest muscles. At the same time, stretching and opening up the pectoral muscles are equally important to create more space in the front of the body.
Rounded shoulders can lead to several complications, such as impingement of the rotator cuff tendons, neck tension, and reduced range of motion in the shoulder joint. This postural imbalance can also affect athletic performance, making it harder to execute movements that require optimal shoulder stability and strength. In sports or activities that require repeated overhead movements, rounded shoulders can place excess strain on the rotator cuff, increasing the risk of injury.
Rounded Shoulders and Upper Back Musculature: How the Female Ribcage and Shoulder Mechanics Increase Susceptibility to Rounded Shoulders and Upper Back Strain
The unique structure of the female body, particularly in the upper torso, introduces specific anatomical characteristics that can predispose women to certain postural challenges. One common issue is rounded shoulders, often coupled with upper back strain and discomfort. This posture, characterized by forward-slumped shoulders and a rounding of the upper back, stems from a combination of anatomical factors—like the narrower, more rounded ribcage in females—as well as alignment and mechanics of the shoulder girdle. Recognizing these influences provides valuable insights into why women may be more prone to this posture and offers a foundation for developing strategies to address and prevent it.
Female Ribcage Structure and Shoulder Positioning
One of the most noticeable anatomical differences between male and female bodies is the shape and size of the ribcage. The female ribcage is generally narrower, more rounded, and smaller in volume compared to the broader, more rectangular ribcage typically seen in males. This narrower ribcage creates more space in the pelvic region for reproductive functions, but it also impacts the alignment and mechanics of the shoulder girdle.
Due to the narrower ribcage, the female shoulder blades (scapulae) are positioned more laterally and are often angled slightly forward. This setup helps create space for shoulder joint movement without constant contact with the ribcage, supporting fluid arm movement. However, this forward orientation of the scapulae also means that the shoulders naturally sit in a slightly forward position, creating a predisposition for them to round forward, particularly in individuals who engage in activities that encourage forward posture, such as working at a computer, driving, or prolonged phone use.
The rounded ribcage shape itself contributes to the forward positioning of the shoulders, making it easier for the upper back and shoulder muscles to fall into a slouched posture. Over time, this can lead to what is commonly known as “rounded shoulders,” a posture in which the shoulders rest forward of the ideal anatomical alignment, pulling the upper back muscles into a stretched and weakened position. When left unaddressed, this posture can lead to chronic upper back strain and neck discomfort.
Muscle Imbalances and Postural Strain
The rounded shoulder posture in females is further compounded by muscle imbalances that develop due to this alignment. When the shoulders are positioned forward, certain muscle groups become overactive and tight, while others become overstretched and weakened. The pectoral muscles (pectoralis major and minor) in the chest, for instance, tend to shorten and tighten in individuals with rounded shoulders. This tightness pulls the shoulders forward and down, reinforcing the rounded shoulder posture.
Conversely, the muscles of the upper back—including the rhomboids, trapezius, and rear deltoids—are overstretched and weakened in this posture. These muscles are essential for retracting (pulling back) the shoulder blades and stabilizing the upper back. When they are weakened and overstretched, they cannot counteract the forward pull from the chest muscles effectively, resulting in an imbalance that perpetuates the rounded posture. This imbalance places additional strain on the upper back and neck, often leading to discomfort and, over time, chronic pain.
Additionally, the trapezius muscle, particularly its upper fibers, may become overactive as it tries to compensate for the lack of stability in the shoulder girdle. This overactivity can lead to tension and pain in the upper shoulders and neck, further aggravating the postural strain. Women who experience chronic shoulder and neck tension may find that these issues stem from an underlying imbalance linked to the forward shoulder position and weak upper back musculature.
Lifestyle Factors Exacerbating Rounded Shoulders
Modern lifestyle factors further contribute to rounded shoulders and upper back strain. Many common activities and postures, especially in today’s increasingly sedentary lifestyle, encourage a forward-slumped position. Prolonged sitting, particularly with poor posture, accelerates the development of rounded shoulders. Hours spent at a computer, looking down at a phone, or driving lead to a slouched posture that reinforces the natural inclination of the female ribcage and shoulder alignment.
Sedentary behavior and limited physical activity also play a role. Without regular strength training or exercises that target the upper back and postural muscles, these areas become progressively weaker, making it challenging to maintain proper shoulder alignment. This creates a feedback loop where weak muscles grow even weaker, and tight muscles become tighter, reinforcing the rounded shoulder posture and increasing upper back strain.
Occupational habits contribute as well. Many jobs require extended periods of seated or forward-leaning work, which can accelerate postural issues. Similarly, household chores, childcare, and other common daily activities that involve bending forward can make it challenging to counterbalance the natural forward pull on the shoulders.
Structural Consequences of Rounded Shoulders
Rounded shoulders are not only a postural issue but also contribute to physical strain and structural imbalances throughout the body. This posture compresses the chest and restricts respiratory efficiency, leading to shallow breathing that can further strain the neck and upper back muscles. As the shoulders round forward, the thoracic spine also tends to curve excessively, leading to an exaggerated kyphotic (rounded) upper back posture. This exaggerated curvature places additional stress on the lower cervical spine and the upper thoracic region, increasing the likelihood of neck pain and shoulder impingements.
Furthermore, when the scapulae are positioned forward, they lose their natural stabilization, which can lead to shoulder joint instability. Instability in the shoulder joint makes movements like lifting and reaching less efficient and can result in overuse injuries. Over time, individuals with rounded shoulders may experience reduced shoulder mobility and an increased risk of conditions like rotator cuff tendinitis and shoulder impingement syndrome due to the compromised joint positioning.
Corrective Strategies for Rounded Shoulders and Upper Back Strain
Addressing rounded shoulders requires a combination of strengthening exercises, flexibility work, and lifestyle adjustments. Corrective strategies focus on realigning the shoulders, reducing strain on the upper back, and building balanced musculature.
Strengthening the Upper Back Muscles: Exercises that target the rhomboids, lower trapezius, and rear deltoids are essential for improving shoulder alignment. Movements like rows, reverse flies, and scapular retractions help activate and strengthen the muscles responsible for retracting the shoulder blades. Building strength in these muscles helps counterbalance the forward pull from tight chest muscles, restoring a more neutral shoulder position.
Stretching the Chest Muscles: Stretching the pectoral muscles is crucial to allow the shoulders to return to a more neutral position. Chest stretches, doorway stretches, and foam rolling are effective methods for releasing tension in the pectorals, reducing the forward pull on the shoulders, and allowing for better posture.
Improving Postural Awareness and Ergonomics: Developing postural awareness can significantly impact shoulder alignment throughout the day. Setting up an ergonomic workstation, avoiding prolonged slouching, and taking regular breaks from seated positions can help prevent rounded shoulders. Additionally, practicing good posture while standing and walking, with shoulders relaxed and positioned back, supports overall shoulder health and prevents unnecessary strain.
Incorporating Functional Movements: Functional training that incorporates exercises like pull-apart bands, scapular wall slides, and prone Y raises can build strength in the stabilizing muscles around the scapulae. These movements emphasize shoulder blade mobility and stability, promoting better shoulder mechanics in daily activities.
Foot Arch and Ankle Alignment
The alignment of the lower limbs, including the feet and ankles, is heavily influenced by the structure of the pelvis. In females, the wider pelvis, which has evolved to accommodate reproductive functions, significantly affects the biomechanics of the lower body. This structural difference impacts how forces are distributed through the legs, feet, and ankles, leading to variations in gait, balance, and susceptibility to certain musculoskeletal issues. Understanding these implications can help in developing strategies to prevent injuries and improve overall movement efficiency.
Effects of a Wider Pelvis on Lower Limb Alignment
The wider pelvis in females creates a distinct alignment pattern in the lower limbs compared to males. This difference is most apparent in the angle at which the femur (thigh bone) meets the knee, known as the Q-angle. A greater Q-angle causes the femur to angle inward more significantly, which, in turn, affects the positioning of the knees, ankles, and feet. As the femur angles inward, it places more stress on the inside of the knee and can cause the lower leg to rotate slightly outward. This rotation affects how weight is distributed through the foot, impacting the arches and overall stability of the ankle.
One of the primary effects of this alignment is the increased tendency for the foot to pronate, or roll inward, during weight-bearing activities like walking, running, or standing. Pronation is a natural part of the foot’s shock absorption mechanism, but when it becomes excessive, it can lead to biomechanical inefficiencies and strain on the structures of the foot and ankle. The inward rolling of the foot caused by pronation places additional stress on the medial arch and the stabilizing muscles and ligaments of the ankle.
The wider pelvis also impacts the position of the ankle joint. Because the knees are more likely to angle inward, the ankle has to compensate to maintain balance and proper gait mechanics. This compensation can lead to altered loading patterns on the foot and ankle, contributing to issues such as ankle instability, overuse injuries, and even problems higher up the kinetic chain, like hip and lower back pain. The interplay between pelvic structure and foot alignment underscores the complexity of the musculoskeletal system and how changes in one area can affect multiple others.
Implications for Gait and Balance
Gait, or the manner in which a person walks, is directly influenced by the alignment of the lower limbs. In females, the combination of a wider pelvis and greater Q-angle changes the biomechanics of walking and running. The inward angling of the femur and the tendency for the foot to pronate can affect the efficiency and stability of each step. During gait, the body must maintain balance while transitioning weight from one leg to the other. If the alignment of the feet and ankles is not optimal, this process can become less efficient and more prone to instability.
One common adaptation seen in females is a wider stance or a gait pattern that involves more lateral hip movement. This adaptation helps accommodate the structural alignment of the pelvis but can place additional stress on the muscles and joints of the lower body. The hips and glutes must work harder to stabilize the pelvis, and the muscles of the feet and ankles are tasked with absorbing and distributing the forces generated by movement. When this system becomes overworked or imbalanced, it can lead to fatigue, pain, and injury.
Balance is another area affected by the alignment of the foot and ankle. The foot’s arch plays a critical role in maintaining balance and distributing forces evenly across the foot. In females with a wider pelvis and increased pronation, the arch may become less effective at providing support. This can lead to instability in the ankle joint, making it easier to roll an ankle or experience balance-related issues. Activities that require quick direction changes, like sports, or those that involve uneven surfaces, like hiking, can be particularly challenging and increase the risk of injury.
Common Issues Like Pronation and Ankle Instability
Pronation, when excessive, is one of the most common issues seen in females due to the wider pelvis and altered lower limb alignment. While a certain degree of pronation is necessary for shock absorption, overpronation can lead to a cascade of problems. The arch of the foot may collapse more than it should, putting strain on the plantar fascia, the thick band of tissue that runs along the bottom of the foot. Over time, this can lead to conditions like plantar fasciitis, a painful inflammation of the plantar fascia that is common in runners and those who spend a lot of time on their feet.
As the thigh rotates inward, this motion continues down to the knee and lower leg, leading to internal rotation of the tibia (shin bone) and causing the knee to move inward, a condition often referred to as knee valgus. This chain of movement ultimately reaches the foot, promoting overpronation. Pronation is the natural inward roll of the foot while walking or running, but excessive pronation, influenced by this chain, can lead to stability and alignment issues.
The image visually captures how each part of the lower body is interconnected, emphasizing how structural characteristics, like a wider pelvis, can influence alignment and movement patterns down to the feet, potentially increasing the risk of musculoskeletal problems over time.
Ankle instability is another frequent issue linked to the biomechanics of the female lower limb. The inward angling of the knee and the tendency to overpronate can make the ankle joint more prone to rolling or spraining. Chronic ankle instability, where the ankle frequently gives way, can develop as a result of repeated sprains or insufficient strength in the muscles and ligaments that support the joint. This instability not only affects performance in sports and physical activities but can also increase the risk of long-term joint damage, including arthritis.
Furthermore, the altered alignment caused by a wider pelvis can lead to compensatory patterns in the muscles and tendons around the ankle. For example, the posterior tibialis muscle, which supports the arch and helps control pronation, can become overworked and develop tendinitis. Achilles tendinitis is also more common in women who overpronate, as the excessive inward rolling of the foot places added strain on the Achilles tendon.
The challenges of excessive pronation and ankle instability often require targeted interventions, such as strengthening the muscles of the foot and lower leg, wearing supportive footwear, or using custom orthotics to help control foot mechanics. Physical therapy exercises that focus on improving ankle stability, such as balance training and proprioceptive exercises, can be beneficial. Additionally, exercises that strengthen the gluteal muscles can help stabilize the pelvis and reduce the compensatory strain placed on the feet and ankles.
Hormonal Influence on Ligament Laxity
The musculoskeletal system is profoundly affected by hormones, which influence everything from bone density to ligament flexibility. In females, hormones such as estrogen and relaxin play a particularly significant role in determining the laxity of ligaments and the overall stability of joints. These hormonal effects are essential for reproductive purposes, but they come with trade-offs that impact joint health and injury risk throughout a woman’s life. Understanding the influence of these hormones can shed light on why women are more prone to certain musculoskeletal conditions and how to address these challenges effectively.
Role of Hormones Such as Estrogen and Relaxin
Estrogen and relaxin are two key hormones that impact ligament laxity in females. Estrogen is a hormone produced mainly by the ovaries, and its levels fluctuate throughout a woman’s menstrual cycle. It is known for its effects on reproductive tissues, but it also has a significant impact on collagen, the protein that provides strength and structure to ligaments and other connective tissues. Estrogen tends to soften collagen fibers, making ligaments more elastic. This increased elasticity is beneficial in some contexts, such as childbirth, where the body needs to accommodate the growing fetus and prepare for delivery.
Relaxin, another hormone produced by the ovaries and the placenta during pregnancy, has a more specialized role. As the name suggests, relaxin’s primary function is to “relax” the ligaments and connective tissues, particularly in the pelvic area, to facilitate childbirth. Relaxin loosens the pubic symphysis and softens the cervix, making labor and delivery possible. However, relaxin doesn’t act in isolation; it also affects ligaments throughout the body, increasing overall joint laxity and reducing joint stability. The effects of relaxin can be felt well beyond the pelvis, influencing how other joints behave under load or during movement.
The impact of these hormones isn’t limited to pregnancy. Throughout the menstrual cycle, estrogen levels vary, and these fluctuations can lead to changes in ligament laxity. For instance, during the luteal phase of the menstrual cycle, when estrogen levels are elevated, women may experience greater joint flexibility and, consequently, reduced joint stability. This hormonal influence means that ligament laxity is not constant but varies depending on where a woman is in her hormonal cycle, which can have implications for athletic performance and injury risk.
How Hormonal Changes Affect Joint Stability and Flexibility
The increased ligament laxity caused by estrogen and relaxin has both advantages and disadvantages. On the positive side, greater flexibility can be beneficial for activities that require a wide range of motion, such as dance, gymnastics, and yoga. It can also be an asset in sports that demand fluid and adaptable joint mechanics, allowing for more dynamic movements. However, the downside of increased flexibility is a significant reduction in joint stability. Ligaments that are too lax are less effective at holding joints securely in place, making the joints more susceptible to instability and injury.
For example, the knee joint, one of the most complex and frequently injured joints in the body, is particularly vulnerable. The anterior cruciate ligament (ACL), which helps stabilize the knee, can be compromised by increased ligament laxity. Women are two to eight times more likely to suffer ACL injuries compared to men, and this is partly attributed to hormonal influences on ligament strength and elasticity. During high-impact activities or movements that involve sudden stops or changes in direction, the knee is less able to withstand these forces, leading to a higher risk of tears and sprains.
The shoulder joint is another area affected by hormonal changes. The shoulder is already one of the most mobile joints in the body, but the added ligament laxity can make it prone to instability and dislocations. Women who engage in sports that require repetitive shoulder movements, such as swimming or tennis, may experience increased wear and tear on the joint, leading to chronic instability and pain. The effects of estrogen and relaxin on ligament laxity extend to the ankle joint as well, increasing the likelihood of ankle sprains, especially during activities that involve jumping or rapid directional changes.
Hormonal changes also affect the spine, particularly the lumbar and sacroiliac joints. The increased flexibility in these areas can contribute to lower back pain, especially during pregnancy, when relaxin levels are at their peak. The spine’s ability to provide a stable base for movement is compromised when the ligaments are too lax, leading to discomfort and an increased risk of injury. Women who experience chronic lower back pain may need to pay extra attention to core stabilization exercises to counteract the effects of ligament laxity.
The Trade-Offs Between Flexibility and Injury Risk
While increased flexibility can be advantageous in certain contexts, it comes at a significant cost. The primary trade-off is the elevated risk of injury. Ligaments are essential for stabilizing joints and preventing excessive or abnormal movement. When these ligaments become too elastic, they can’t provide the necessary support, leaving joints vulnerable to dislocations, sprains, and chronic instability. This is particularly problematic in sports and high-impact activities, where the joints are subjected to sudden and forceful movements.
When ligaments become loose or lax, surrounding muscles may respond by tightening to compensate for the lack of stability. This compensatory mechanism, while providing additional support, often places undue strain on the muscles involved. Over time, this additional tension can lead to muscle fatigue and, under repetitive or high-stress conditions, increase the risk of muscle tears. A study by Krivickas and Feinberg (1996) provides evidence linking ligament laxity to an increase in muscle tightness, especially in athletes. Their study found that in college athletes, lower ligament stability corresponded with tighter surrounding muscles, raising the incidence of injuries in athletes with high ligament laxity scores (Krivickas & Feinberg, 1996).
An example of this phenomenon is frequently observed in athletes who experience anterior cruciate ligament (ACL) injuries. In individuals with ACL tears, compensatory muscle activity, particularly from the hamstrings, is often heightened to stabilize the knee joint in the absence of a fully functioning ligament. This increased reliance on the hamstrings can lead to excessive muscle strain, often resulting in additional injuries or muscle tears if not managed properly. A study by Snyder-Mackler et al. (1994) highlights this relationship, showing that the quadriceps muscles in patients with ACL injuries often experience reflex inhibition while hamstrings tighten to provide stability, placing these muscles at higher risk for strain and tear (Snyder-Mackler et al., 1994).
The risk of injury is further complicated by the fact that ligament laxity is not static but changes with hormonal fluctuations. Women may be more susceptible to injuries at certain times of their menstrual cycle, depending on hormone levels. For athletes, this means that training and competition schedules might need to be adjusted to account for periods of increased vulnerability. Injury prevention strategies, such as targeted strength training, proprioceptive exercises, and neuromuscular conditioning, are crucial for mitigating these risks. Strengthening the muscles around a joint can help compensate for the reduced support from the ligaments, enhancing overall joint stability.
Pregnancy presents another set of challenges. While the body needs to become more flexible to prepare for childbirth, this increased laxity can lead to musculoskeletal issues that persist postpartum. Women may experience chronic joint pain or instability long after pregnancy, highlighting the long-term impact of hormonal changes on the body. Rehabilitation and strengthening programs are often necessary to restore joint stability and function.
- Krivickas, L., & Feinberg, J. (1996). Lower extremity injuries in college athletes: relation between ligamentous laxity and lower extremity muscle tightness. Archives of Physical Medicine and Rehabilitation, 77(11), 1139-1143. Link to paper
- Snyder-Mackler, L., De Luca, P., Williams, P. R., Eastlack, M., & Bartolozzi, A. (1994). Reflex inhibition of the quadriceps femoris muscle after injury or reconstruction of the anterior cruciate ligament. The Journal of Bone and Joint Surgery. American Volume, 76(4), 555-560. Link to paper
The Evolutionary Roots and Implications of Female Hypermobility
Hypermobility, or an increased range of motion in the joints, is a fascinating trait with deep evolutionary roots. In females, this trait is particularly pronounced and is widely believed to have evolved in response to specific reproductive demands, primarily the physical requirements of pregnancy and childbirth. While the ability to adapt to these demands has had clear advantages for reproductive success, it also brings with it a set of vulnerabilities. Understanding the evolutionary purpose of hypermobility in females offers valuable insights into the complex interplay between adaptability, survival, and musculoskeletal health.
Hypermobility and Its Role in Pregnancy and Childbirth
The human body is a product of evolutionary adaptations, finely tuned to maximize survival and reproductive success. For females, hypermobility evolved as a way to support the intense physical requirements of pregnancy and childbirth. The female pelvis, hips, and other musculoskeletal structures are distinctively shaped to accommodate a growing fetus and facilitate childbirth. Unlike the male pelvis, the female pelvis is broader and has a larger, more circular pelvic inlet and outlet, designed to allow safe passage of a baby during delivery.
During pregnancy, the body undergoes dramatic physiological changes, with increased joint flexibility being a crucial adaptation. This flexibility is enhanced by the hormone relaxin, which softens ligaments and connective tissues throughout the body, especially in the pelvis. Relaxin prepares the body for labor by loosening the pelvic ligaments, enabling the pelvis to expand as needed. However, relaxin’s effects are not limited to the pelvis; it has a systemic influence, making ligaments throughout the body more pliable. This increased joint laxity helps accommodate the growing fetus and manage the altered weight distribution as the center of gravity shifts forward.
The lumbar spine in females also shows adaptations linked to reproductive needs. With a more pronounced curve, or lordosis, the spine helps balance the extra weight of pregnancy, preventing the body from tipping forward. This adaptation in the spine supports the mother’s stability and mobility during pregnancy, though it also increases the risk of lower back pain and musculoskeletal strain.
Hormonal Influences and Joint Laxity
The hormonal underpinnings of hypermobility extend beyond pregnancy. Relaxin, which plays a central role in loosening ligaments during pregnancy, is accompanied by estrogen, another hormone that contributes to ligament laxity. Estrogen affects collagen, the protein that provides structure to ligaments, making them more elastic. This hormonal influence helps maintain flexibility, especially during the reproductive years, but also predisposes women to joint-related issues.
Women experience cyclical fluctuations in estrogen levels throughout their menstrual cycle, with peaks causing temporary increases in joint flexibility. This heightened laxity can lead to joint instability at certain times of the month, which has implications for female athletes and those engaged in physical activities. Menopause introduces a new phase, with declining estrogen levels reducing flexibility but potentially increasing the risk of joint degeneration, such as osteoarthritis.
Evolutionary Trade-Offs: Adaptability vs. Vulnerability
While hypermobility provides essential benefits for childbirth, it is also a classic example of an evolutionary trade-off. Greater joint flexibility, though advantageous for reproductive success, comes with increased vulnerability to musculoskeletal issues. Hypermobile joints tend to be less stable, making individuals more susceptible to injuries such as sprains, dislocations, and chronic pain. This instability is especially common in joints that bear significant weight, like the knees and ankles, and in the shoulders, where hypermobility increases the risk of overextension or ligament strain.
Evolutionary biology often involves such trade-offs, where a trait that is beneficial in one context introduces risks in another. For early human females, the reproductive benefits of hypermobility far outweighed the potential disadvantages of joint instability. The ability to safely carry a pregnancy to term and deliver a baby was crucial to the survival of both mother and offspring. Thus, while joint instability posed some biomechanical risks, it was a minor disadvantage relative to the reproductive advantage provided by increased joint flexibility.
Gender Differences in Hypermobility: An Evolutionary Perspective
Studies indicate that hypermobility is more prevalent in females than in males, underscoring the role of evolutionary pressures related to reproduction. Female bodies have evolved to prioritize flexibility over rigidity, a trait that is reinforced by hormonal influences. In contrast, male bodies typically emphasize stability and strength, reflecting roles that were historically associated with hunting and protective activities. These evolutionary roles suggest that hypermobility in females developed as an adaptation to the unique physical demands of pregnancy and childbirth, while males’ joint structures evolved for stability and resilience in physically strenuous activities.
This gender difference highlights how evolutionary pressures have shaped anatomy and function in line with different reproductive and social roles. While men’s physical activities historically required joint stability for tasks like running, lifting, and throwing, women’s bodies adapted to support flexibility and adaptability, especially in the context of reproduction and caregiving.
The Modern Implications of Hypermobility
In contemporary society, hypermobility remains both an advantage and a challenge. In sports and activities that require a high degree of flexibility, such as gymnastics, yoga, and dance, hypermobility is often a valuable asset. However, modern lifestyles that involve prolonged sitting and repetitive movements can exacerbate the downsides of hypermobility, leading to chronic joint pain, instability, and injuries.
The persistence of hypermobility into modern times illustrates the complex interplay between evolution and lifestyle. While hypermobility evolved for specific reproductive purposes, it poses new challenges in a modern environment that does not align with the lifestyle and physical demands of early humans. Increased awareness of hypermobility-related disorders, such as hypermobility spectrum disorders (HSD) and hypermobile Ehlers-Danlos syndrome (hEDS), has drawn attention to the health issues associated with extreme joint flexibility. These conditions, involving chronic pain and joint instability, demonstrate how a trait that was once advantageous can now be a health concern due to the differences between ancestral and modern environments.
Conclusion
The human body’s design is a remarkable testament to the intricate connection between structure and function, with the female body providing a vivid example of how evolutionary pressures shape anatomy and biomechanics. From the shape of the pelvis to the flexibility of the ligaments, each feature is carefully tailored to support reproductive functions, such as pregnancy and childbirth, while maintaining overall mobility and adaptability. Yet, these evolutionary adaptations come with trade-offs that have significant implications for how women experience movement, balance, and injury risk in the modern world.
One of the most striking examples of this structure-function relationship is the wider female pelvis. While essential for childbirth, the broader pelvis alters lower limb alignment, affecting the knees, ankles, and feet. It contributes to a greater Q-angle, which influences knee mechanics and increases the likelihood of conditions like ACL injuries and patellofemoral pain. Similarly, the shallow hip sockets that provide greater range of motion also result in a higher risk of hip instability and labral tears. These adaptations underscore how evolution has prioritized reproductive success, even if it means introducing vulnerabilities elsewhere in the body.
Ligament laxity, influenced by hormones like estrogen and relaxin, further demonstrates the balance between flexibility and stability. Greater ligament flexibility is crucial during pregnancy, allowing the pelvis to expand and adapt to the growing fetus. However, this increased laxity reduces joint stability, making women more prone to sprains, dislocations, and chronic joint pain. The hormonal shifts that drive these changes are a double-edged sword: they enable crucial reproductive functions but complicate the management of joint health and stability throughout a woman’s life.
The shape of the thoracic cage and its influence on shoulder mechanics also highlight this delicate balance. A narrower, more rounded ribcage affects the positioning of the scapulae and predisposes women to postural challenges like rounded shoulders. This can lead to muscle imbalances, shoulder impingement, and chronic neck and upper back tension. Similarly, the evolutionary adaptation of a more flexible lumbar spine helps maintain balance during pregnancy but also contributes to lower back pain and spinal instability.
In the modern world, these evolutionary features can pose challenges as women engage in activities and sports that place new demands on their bodies. The prevalence of joint injuries in female athletes, for example, highlights the need for tailored training and injury prevention strategies that address the unique biomechanics of the female body. Strength training, core stabilization, and proprioceptive exercises are essential components of a comprehensive approach to maintaining joint health and reducing the risk of injury.
Supporting female biomechanics requires a holistic understanding of how structure and function are intertwined. It’s about acknowledging that the same traits that offer flexibility and adaptability also necessitate extra care to ensure long-term musculoskeletal health. This means focusing on prevention and management strategies that strengthen stabilizing muscles, promote balanced movement patterns, and account for hormonal influences on joint stability. Education and awareness are critical, empowering women to make informed choices about their bodies and health.
Ultimately, the female body is a complex system optimized for the demands of reproduction, yet it must also function in a world filled with physical challenges that evolution never anticipated. The balance between evolutionary adaptations and modern implications serves as a reminder of the incredible resilience and adaptability of the human body. By understanding these unique biomechanics and tailoring interventions accordingly, we can support women in living active, healthy lives, honoring both their evolutionary heritage and their modern aspirations.
References
- “Female Pelvis Bones Diagram & Function” – This article offers an overview of the female pelvic anatomy, highlighting differences between male and female pelvises. Healthline
- “Hypermobility, Hormones, and the Menstrual Cycle” – This resource discusses how hormonal fluctuations during the menstrual cycle can influence joint laxity, particularly in women with hypermobility disorders. Mayo Clinic Connect
- “Effect of Estrogen on Musculoskeletal Performance and Injury Risk” – This study examines the impact of estrogen on ligament structure and joint stability, providing insights into injury risks associated with hormonal changes. Frontiers
- “The Pelvis” – An anatomical guide detailing the structure and function of the pelvis, including its role in supporting the body’s weight and facilitating movement. Teach Me Anatomy
- “Female Pelvis Diagram: Anatomy, Function of Bones, Muscles, Ligaments” – This article provides a comprehensive look at the bones, muscles, and ligaments of the female pelvis, explaining their functions and common conditions affecting them. Healthline
- “Anatomy of Female Pelvic Area” – A detailed overview of the female pelvic anatomy, including descriptions of the reproductive organs and their functions. Johns Hopkins Medicine
- “The Effect of Sex Hormones on Ligament Structure, Joint Laxity, and Injury Risk” – This chapter explores how sex hormones influence ligament structure and joint laxity, contributing to differences in injury risk between sexes. Springer Link
- “Female Pelvis Organs & Inner Muscles Diagram & Function” – An interactive resource illustrating the organs and inner muscles of the female pelvis, along with their functions. Healthline
- “Hormonal Influence on the Neuromusculoskeletal System in Pregnancy” – This chapter discusses the role of hormones like relaxin and progesterone in modulating the neuromusculoskeletal system during pregnancy. Springer Link
- “Female Anatomy: Organs and Reproductive System Diagrams” – This article provides diagrams and explanations of the female reproductive system, detailing the structure and function of various organs. Verywell Health
- “Female Reproductive System: Structure & Function” – This article from the Cleveland Clinic offers an in-depth overview of the female reproductive system, including anatomical structures and their functions. Cleveland Clinic
- “Anatomy and Physiology of the Female Reproductive System” – This resource provides comprehensive information on the anatomy and physiology of the female reproductive system, including hormonal regulation and reproductive cycles. Lumen Learning
- “Female Reproductive Organs: Anatomy and Functions” – Kenhub offers detailed anatomical descriptions and functions of female reproductive organs, accompanied by high-quality illustrations. Kenhub
- “Overview of the Female Reproductive System” – The Merck Manual provides a thorough overview of the female reproductive system, discussing anatomy, hormonal regulation, and common health issues. Merck Manual
- “A Guide to Female Reproductive Hormones” – This article explores the roles of various hormones in the female reproductive system, including estrogen, progesterone, and others. Medicine.com
- “Female Anatomy: Organs and Reproductive System Diagrams” – Verywell Health provides diagrams and explanations of the female reproductive system, detailing the structure and function of various organs. Verywell Health
- “Female Anatomy: Body Parts, Their Functions, and Diagram” – Medical News Today offers a comprehensive guide to female anatomy, including external and internal structures and their functions. Medical News Today
- “Interactive Guide to Female Reproductive Anatomy” – Innerbody provides an interactive resource illustrating the organs and inner muscles of the female pelvis, along with their functions. Innerbody
- “Human Reproductive System – Female Anatomy, Hormones, Reproduction” – Encyclopaedia Britannica offers detailed information on the female reproductive system, including anatomy, hormonal regulation, and reproductive processes. Britannica
- “Complete Guide to Female Anatomy: Organs, Hormones, and Differences” – Everyday Health provides a comprehensive guide to female anatomy, discussing organs, hormonal influences, and differences between male and female anatomy. Everyday Health