Lumbar radiculopathy is a very common cause of lower back and leg pain, resulting in acute or chronic disability. It is defined as a focal neurological impairment in a specific myotomal and/or dermatological distribution due to nerve root compression or irritation. Common patient complaints include low back pain with pain radiating to the lower extremity, lower extremity weakness, and/or sensory changes such as numbness or tingling. Men are more frequently affected than women. Men are usually affected after the age of 40, while women are affected between the ages of 50 and 60.
Synonym for radiculopathy: Radicular Avulsion (Neuropathy), Nerve Root Compression, Radicular Compression, Radiculitis, Radiculoneuritis, Radicular Disorder
What causes lumbar radiculopathy?
- Herniated disc, when a disc surfaces, compressing the sciatic nerve root
- Degenerative disc disease
- Bone spur
- Tumors of the spine
- Osteoarthritis
- Spinal canal stenosis
- Compression fractures
- Spondylolisthesis, when a vertebra moves and rests on the lower vertebra
- Scoliosis
- Diabetes, caused by an alteration of the blood circulation of the nerves
- Cauda equina syndrome is an uncommon but serious condition where nerve root compression affects the pelvic organs and lower extremities.
What are the symptoms of lumbar radiculopathy?
- Radiculopathy causes pain:
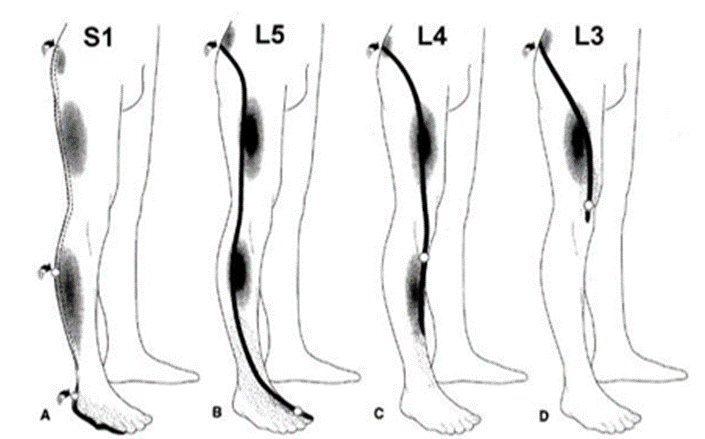
- S1: Posterior part of the thigh and calf
- L5: buttock and anterolateral leg
- L4, douleur dans la partie antérieure de la cuisse, dans la partie antérieure ou médiale du genou et dans la partie médiale de la jambe.
- L3: Groin
- Pain in the area around the affected nerve.
- Tingling and numbness (parasthesia)
- Muscle weakness.
What are the differential diagnoses of lumbar radiculopathy?
- Trochanteric bursitis
- Anterosuperior bursitis
- Hamstring sprain
- Lumbosacral plexopathy
- Diabetic muscular dystrophy
- Peripheral neuropathy: sciatic, tibial, peroneal, femoral
- Avascular necrosis of the hip
- Osteoarthritis of the hip
- Shin splints
- Lateral femoral cutaneous neuropathy (meralgia
- paresthesia)
- Spinal stenosis
- Cauda equina syndrome
- Demyelinating disorder
- Lumbar facet syndrome
- Piriformis syndrome
What are the osteopathic approaches for the treatment of lumbar radiculopathy?
Mobilization of the spine with leg movement
Synonyme : Mobilisation vertébrale avec mouvement des jambes
Indication: Leg pain and other symptoms that extend below the knee induced by the SLR test.
Technique:
- This technique requires a therapist and an assistant.
- The patient is in a side-lying position with the affected leg on top near the edge of the treatment table. The affected leg is extended with a slight abduction at the hip and held by the assistant. The therapist applies and maintains a transverse glide from the spinous process to the floor of the cranial vertebra at the affected segment.
- The patient actively moves the leg in SLR with the help of the assistant.
- This position is maintained for 30 seconds
- The treating therapist releases the pressure on the spinous process and the patient lowers the supported leg onto the treatment table.
- Three rehearsals during the first visit.
- However, when the patient has improved during subsequent visits, the therapist should apply overpressure to the supported leg while the assistant performs the SLR.
- This pressure was also maintained for 30 seconds, after which the leg must be lowered onto the treatment table. This procedure was repeated six times on subsequent visits.
- At the end of a session, always reassess the SLR in the supine position.
Progressive inhibition of neuromuscular structures (PNMS)
Definition: A form of inhibition technique developed by Dennis Dowling, DO. The practitioner locates two related points and sequentially applies pressure along a series of related points:
Technique:
- Two connected points, called primary and end points, must be found. These points are the most and least sensitive areas, respectively, along a neuromuscular structure.
- When an area of reduced tenderness (end point) was found, moderate ischemic compression was applied with the index finger of one hand without releasing the pressure until the treatment was completed.
- When an area of greater sensitivity was found (primary point), moderate ischemic compression was also applied with the index finger of the other hand for 30 s, after which another sensitive point was identified with the middle finger of the same hand in the vicinity of the final point without releasing the index finger pressure.
- When the middle finger pressure was judged to be more sensitive than the index finger, pressure, the index finger, pressure was released and the middle finger pressure was held without releasing the end point pressure. This was maintained for 30 s before the third point was identified. Similar patterns for all identified tender points were followed continuously along the neuromuscular continuum until the last point, approximately 2 cm from the end point, was found. Pressure was held for 30 seconds simultaneously on both points (the last and the end point) and then released.