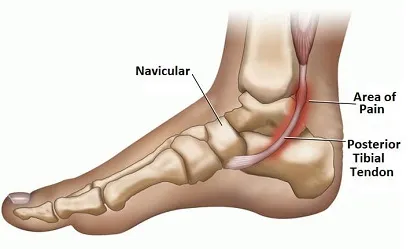
Posterior tibial tendon dysfunction is an inflammation (tendinitis) that degenerates (tendinosis) to lead to microtears of the posterior tibial tendon. The function of the tibialis posterior is to support the plantar arch. An insufficiency of this will cause the foot to flatten (pronation).
Introduction
The tibialis posterior plays a vital role by acting as the primary dynamic stabilizer of the medial longitudinal arch and serving as a major inverter of the medial foot. This crucial function helps maintain the integrity of the medial longitudinal arch, ensuring stability and rigidity of the medial foot structure. At the same time, contraction of the tibialis posterior elevates the medial longitudinal arch, creating a solid platform and promoting the efficiency of the gastrocnemius during the gait cycle.
It is important to emphasize that degradation of the posterior tibial tendon does not necessarily require total rupture to result in foot collapse. Even minor damage can compromise its support capacity. Due to its short length, the tendon is particularly vulnerable to damage, and minor alterations can already disrupt its effectiveness.
The predominant cause of this deterioration is often tendinosis, resulting from repeated microtrauma. Over time, these microtraumas lead to degeneration of the tendon, gradually replacing functional tissue with ineffective fibrous tissue. This degradation can occur in an area of hypovascularization, typically in the region of the medial malleolus.
When the posterior tibial tendon loses its functional capacity, the medial longitudinal arch of the foot collapses. This phenomenon induces a relative internal rotation of the tibia and talus, accompanied by an eversion of the subtalar joint. As a result, the heel aligns in valgus, while abduction occurs at the Talonavicular joint.
Varus misalignment of the heel results in lateral displacement of the normal axis of the Achilles tendon. Over time, this shift can lead to contracture of the Achilles tendon. As the deformity progresses, the distal fibula comes into contact with the lateral calcaneus, generating lateral rearfoot pain.
The consequences of these anatomical alterations go beyond simple deformation of the foot. The impact is felt through the lower extremity, affecting the alignment of the tibia, talus and subtalar joint. This series of changes can lead to biomechanical imbalances, joint pain, and stability issues when walking.
Early diagnosis of posterior tibial tendon tendinosis is essential for effective management. Treatment options may include osteopathy to strengthen the muscles of the foot and ankle, orthotics to support the medial arch, and in some cases, surgical procedures to repair the damaged tendon.
Causes of posterior tibial tendon dysfunction
| Inflammatory | Inflammatory rheumatoid arthritis |
| Mechanical | Impairment of tendinopathy Functional impairment Anomaly of the talocrural joint Soft tissue tension/traction Pre-existing flat foot Excessive functional pronation |
| Metabolic | Increased cholesterol Menopause |
| Others | Infection Vieillissement |
| Non-specific causes | Pregnancy Microvascular damage Macrovascular deficiency |
| Non-specific factors increasing the risk of developing chronic pathology | Increased body mass index Smoker Localized steroid exposure Long-term medication use Diabetes Hypertension Anterior hindfoot trauma/surgery |
From: Yao et al, 1999; Kirby, 2000; Bowring and
Chockalingam, 2009
Arch Fall: Stages and Implications
Arch drop, also known as “flat foot” or “medial arch sag,” can occur gradually over time. The stages of arch droop can vary from person to person, and the severity of the condition depends on various factors, including genetics, physical activities, and pre-existing medical conditions. Here is a general description of the possible stages of arch loss:
- Foot with Normal Arch: Initially, the foot has a normal arch, with a slightly elevated curvature at the inner part of the foot, known as the medial arch. This structure ensures balanced distribution of body weight while walking.
- Soft flat foot (early stage): In the early stages, the person may develop what is called “soft flat foot”. The medial arch may sag temporarily during weight-bearing, but it usually returns to its normal shape in a non-weight-bearing position.
- Moderate flatfoot (intermediate stage): As the condition progresses, sagging of the medial arch becomes more pronounced, even in a non-weight-bearing position. This may be associated with increased foot fatigue during walking or physical activities.
- Severe flatfoot (advanced stage): In advanced stages, flatfoot may become more evident, with a significant decrease in medial arch height. Foot stability may be compromised, leading to changes in gait and associated pain.
- Structural deformation (advanced stage): In some severe cases, the fall of the plantar arch may be accompanied by a structural deformation of the foot, such as internal rotation of the talus or excessive pronation.
- Posterior Tibial Tendon Dysfunction: Plantar arch drop can often be associated with posterior tibial tendon dysfunction. This tendon, responsible for supporting the medial arch, can weaken or deteriorate, contributing to foot deformity.
It is important to note that the progression of arch drop can be influenced by various factors such as age, physical activity, underlying medical conditions, and shoes worn. Early management, including muscle strengthening exercises, wearing orthotics and, in some cases, physical therapy, can help alleviate symptoms and slow the progression of the condition.
Symptoms of posterior tibial tendon dysfunction
Posterior tibial tendon dysfunction can manifest with a variety of symptoms, which can vary in intensity depending on the stage of the condition. Here are some symptoms commonly associated with posterior tibial tendon dysfunction:
List of symptoms
- Pain along the inner side of the foot and ankle: Pain is often felt along the inner side of the foot and ankle, particularly near the medial malleolus.
- Pain in the medial arch of the foot: Pain and tenderness may develop in the medial arch of the foot, especially when walking or weight-bearing.
- Medial Arch Sag: A decrease in the height of the medial arch of the foot may be observed visually, which may be a sign of posterior tibial tendon dysfunction.
- Foot Fatigue and Weakness: Patients may experience increased foot fatigue, especially during activities requiring significant support of the posterior tibial tendon.
- Swelling and redness: In more advanced cases, swelling and redness may develop along the posterior tibial tendon.
- Difficulty performing a tiptoe raise: Affected individuals may have difficulty performing a tiptoe raise due to tendon weakness.
- Pain when flexing or inverting the foot: Certain specific movements, such as flexing or inverting the foot, can trigger characteristic pain.
- Difficulty walking on uneven surfaces: Foot stability may be compromised, making it difficult to walk on uneven surfaces.
- Ankle Instability: Decreased function of the posterior tibial tendon can lead to ankle instability, increasing the risk of stability-related injuries.
- Valgus Heel Shift: With tendon breakdown, the heel can shift inward, causing valgus shift.
- Loss of foot alignment: The medial longitudinal arch of the foot can lose support, leading to loss of foot alignment during walking.
- Limitation of foot mobility: Some individuals may experience limitation of foot mobility, particularly when bending or inverting.
- Inflammation of the tendon (tendinitis): Inflammation of the posterior tibial tendon, called tendinitis, can cause increased pain and swelling in the affected area.
- Lameness: Due to pain and limitation of function, lameness may develop while walking.
- Biomechanical Alterations of the Lower Extremity: Changes in the structure of the foot can lead to biomechanical alterations of the lower extremity, affecting the way a person walks and moves.
- Radiating pain: Pain from posterior tibial tendon dysfunction can sometimes radiate to other parts of the foot, ankle, or even calf.
- Difficulty in daily activities: Symptoms of posterior tibial tendon dysfunction can make it difficult to perform daily activities such as prolonged walking, climbing stairs, or wearing inappropriate shoes.
- Progressive foot deformity: As the condition progresses, progressive foot deformity may manifest, affecting the physical appearance and function of the foot.
- Impact on quality of life: Constant pain and functional limitations can have a significant impact on overall quality of life, affecting the ability to participate in social and recreational activities.
- Postural Changes: Alterations in the biomechanics of the foot can lead to compensatory postural changes, which can affect other parts of the body, such as the knees, hips, and lower back.
- Psychological impacts: Chronic pain and physical limitations can lead to psychological impacts such as stress, anxiety and depression.
- Increased risk of secondary injuries: Untreated posterior tibial tendon dysfunction can increase the risk of developing other foot problems, such as hallux valgus (bunion) or Achilles tendonitis.
- Difficulty maintaining regular physical activity: Symptoms can make it difficult to participate in regular physical activities, potentially contributing to a less active lifestyle.
- Development of calluses or corns: Changes in weight distribution and pressure on the foot can lead to the development of calluses or corns, especially in areas subject to increased friction.
- Changes in gait: Affected individuals may adopt an altered gait to compensate for the loss of stability, which can lead to overloading other parts of the foot or lower extremities.
- Discomfort or pain during prolonged standing: Prolonged standing can become uncomfortable and painful, affecting the ability to stand for long periods of time.
- Difficulties finding suitable shoes: Due to the anatomical changes of the foot, it can become difficult to find comfortable and suitable shoes.
- Reduction in physical activity: Symptoms can lead to a reduction in overall physical activity, which can contribute to other health problems related to a sedentary lifestyle.
- Balance Problems: Loss of stability due to posterior tibial tendon dysfunction can lead to balance problems, increasing the risk of falls.
- Impaired proprioception: Proprioception, the body’s ability to perceive its position in space, may be impaired, which can affect motor coordination.
- Frequent need for foot rest: Sufferers may feel the need to take frequent breaks or rest their foot to relieve pain.
- Adaptations in daily activities: Adaptations may be needed in daily activities, such as how to go up and down stairs or participate in sports activities.
- Impact on social and professional life: Functional limitations can have an impact on participation in social and professional activities, sometimes leading to lifestyle adjustments.
Associated Factors and Other Considerations
Posterior tibial tendon dysfunction (PTTD) is a complex condition influenced by various associated factors and other considerations that may affect its development, progression, and management. Understanding these factors and considerations is crucial for comprehensive evaluation and effective treatment of PTTD.
A major factor associated with DTTP is excessive foot pronation, often seen in people with flat feet or weakness in the stabilizing muscles of the arch. Excessive pronation causes overload of the posterior tibial tendon, increasing the risk of dysfunction and degeneration. Likewise, muscular imbalances in the foot and ankle complex, such as weakness of the intrinsic muscles of the foot or tightness of the calf muscles, may contribute to the occurrence of DTTP by disrupting the normal mechanics of the foot and ankle. ankle.
Biomechanical factors, such as abnormalities in lower limb or foot alignment, may also play a role in the development of DTTP. For example, hyperpronation or excessive internal rotation of the tibia can cause increased stress on the posterior tibial tendon and promote its dysfunction. Likewise, anatomical abnormalities of the foot, such as flat feet or pes cavus, can affect the distribution of loads on the foot and increase stress on the posterior tibial tendon.
Factors related to physical activity and lifestyle can also influence the occurrence of PTTD. High-impact activities, such as running or jumping sports, can place excessive stress on the posterior tibial tendon, promoting its inflammation and degeneration. Likewise, sudden changes in the intensity or duration of physical activities may increase the risk of posterior tibial tendon injury in unprepared or insufficiently conditioned individuals.
In addition to physical factors, systemic and medical factors may also be associated with DTTP. For example, certain medical conditions such as diabetes, obesity, inflammatory arthritis, or endocrine disorders may increase the risk of developing PTTD by impairing connective tissue health or disrupting blood flow to the posterior tibial tendon. Likewise, medications such as corticosteroids or fluoroquinolones may increase the risk of tendinopathy by weakening connective tissues and inhibiting tissue repair.
In addition to these associated factors, several other considerations must be taken into account when evaluating and managing DTTP. It is essential to carefully assess the patient’s clinical history, including injury history, previous symptoms, and physical activity habits. A thorough physical examination, including assessment of foot and ankle biomechanics, can help identify contributing factors and guide the treatment plan. Additionally, additional assessments such as diagnostic ultrasound imaging or magnetic resonance imaging (MRI) may be necessary to assess the extent of tissue damage and guide clinical decision-making.
Pathophysiology of posterior tibial tendon dysfunction
The pathophysiology of posterior tibial tendon (TTP) dysfunction involves a series of pathological processes that lead to functional alterations of the tendon. Here is a detailed explanation of the pathophysiology associated with this condition:
- Inflammation and Microtrauma:
- Posterior tibial tendon dysfunction often begins with repetitive strain injury or overuse of the tendon. These excessive stresses can cause inflammation in the tendon.
- Structural Degradation:
- Prolonged inflammation can lead to degradation of tendon structures, including degenerative changes in collagen fibers and extracellular matrix.
- Weakening of the Tendon:
- The breakdown of collagen fibers can weaken the tendon, compromising its ability to effectively support the loads exerted during walking and other activities.
- Vascular Alterations:
- Inflammation and degeneration of the tendon can affect local vascularity, reducing the blood supply necessary for tendon regeneration and healing.
- Anatomical Changes:
- Pathological processes can lead to anatomical changes in the tendon, including thickenings, adhesions, or surface irregularities.
- Tendon Instability:
- Structural weakening can lead to tendon instability, compromising the tendon’s ability to maintain normal foot and ankle position.
- Involvement of Surrounding Structures:
- Posterior tibial tendon dysfunction can affect other surrounding structures, such as ligaments and joints, contributing to the overall symptomatology.
- Body Defensive Response:
- In response to the injury, the body may initiate repair processes, but these may often be insufficient to fully restore normal tendon function.
- Cycle of Continuous Deterioration:
- A cycle of continued deterioration can be established, where chronic inflammation, progressive degeneration and structural weakening are perpetuated, leading to persistent tendon dysfunction.
Examinations and Diagnostic Evaluation
- Is there a valgus knee deformity (genu valgum) on the symptomatic side? (This can precipitate or exacerbate posterior tibial tendon dysfunction, especially if it is chronic.)
- Is there tenderness and swelling especially along the terminal course of the tendon, usually between the medial malleolus and the navicular insertion or, less commonly, in the posterior aspect of the medial malleolus?
- Is there tenderness in the insertion area of the tibialis anterior tendon
- Looking at the weight-bearing patient from behind, is there increased abduction or pronation of the forefoot, a sign of too many toes?
- Is the Achilles tendon tight?
Diagnosis of posterior tibial tendon dysfunction
Diagnosis of posterior tibial tendon dysfunction is essential for the appropriate management of this often debilitating condition. This condition, also known as posterior tibial tendon syndrome, is characterized by impaired function of the posterior tibial tendon, which can lead to pain and instability in the foot and ankle region. To arrive at an accurate diagnosis, several steps and examinations are necessary.
First, a detailed history is crucial. The practitioner must ask the patient about their medical history, current symptoms, duration of pain and possible previous trauma. Information on the patient’s physical activities, level of mobility and occupation may also be relevant to assess risk factors and stresses on the tendon.
Then, a thorough clinical examination is carried out. This usually involves an assessment of posture, gait, and palpation of the posterior tibial tendon area. The practitioner looks for signs of inflammation, swelling, deformation or pain on palpation. Specific functional tests, such as the posterior tibialis isometric strength test or plantar flexion and foot inversion tests, can be performed to assess tendon strength and stability.
Additional tests such as x-rays, ultrasounds and MRIs may be necessary to confirm the diagnosis and assess the extent of the tendon injury. X-rays can help rule out other conditions such as fractures or arthritis, while ultrasound and MRI provide detailed images of the soft tissues, including the posterior tibial tendon itself.
The severity of posterior tibial tendon dysfunction can be classified into several stages based on the results of these examinations. Stage I is characterized by inflammation and edema of the tendon without significant anatomical deformation. Stage II involves partial deformity of the tendon and may be associated with chronic pain and instability. Finally, stage III is characterized by complete deformity of the tendon, loss of function, and eventually collapse of the arch of the foot.
In addition to evaluating posterior tibial tendon dysfunction, it is also important to look for other abnormalities or associated conditions that could be contributing to the patient’s symptoms. This may include foot and ankle alignment disorders such as posterior valgus or flat foot, as well as underlying neurological or rheumatological conditions.
Diagnosis of posterior tibial tendon dysfunction is usually made by a healthcare professional, such as an orthopedist, podiatrist, or doctor who specializes in feet and ankles. The diagnostic process may involve several steps, including:
- History and physical examination: The healthcare professional will take a detailed medical history, paying particular attention to the symptoms experienced. A physical exam will also be performed to assess arch stability, ankle mobility, and posterior tibial tendon strength.
- Imaging tests: Imaging tests, such as X-rays, ultrasounds, or MRIs, may be performed to view the tendon, assess its condition, and rule out other potential problems.
- Gait Analysis: Gait analysis can be performed to assess how a person walks and whether this is contributing to the symptoms of posterior tibial tendon dysfunction.
- Functional tests: Certain functional tests, such as the posterior tibial tendon strength test or specific tests to assess ankle stability, may be performed.
- Pain assessment: The healthcare professional can discuss in detail the nature of the pain, its location and its intensity with the patient.
Treatment Approaches and Management
Posterior tibial tendon (TTP) dysfunction is a condition in which the posterior tibial tendon, located at the back of the ankle, becomes weakened, inflamed, or damaged. This condition can lead to arch instability and flat foot problems.
The treatment approach to posterior tibial tendon dysfunction may vary depending on the severity of symptoms and disease progression. Here are some treatment options that may be considered:
- Rest and reduced activity: Rest is often recommended to allow the tendon to heal. Reducing activities that worsen symptoms, such as prolonged walking or running, can help prevent excessive strain on the tendon.
- Orthotics and adapted shoes: Custom orthotics may be prescribed to support the arch of the foot and relieve pressure on the posterior tibial tendon. Appropriate shoes with good arch support may also be recommended.
- Physical therapy: Muscle strengthening and stretching exercises may be prescribed by a physical therapist to strengthen the muscles of the foot and ankle, improve stability, and promote tendon healing.
- Ankle orthoses: Rigid ankle orthoses can be used to stabilize the ankle and reduce stress on the posterior tibial tendon.
- Anti-inflammatory medications: Nonsteroidal anti-inflammatory medications (NSAIDs) may be prescribed to reduce inflammation and relieve pain.
- Corticosteroid injection: In some cases, a corticosteroid injection may be recommended to reduce inflammation around the tendon.
- Surgery: If posterior tibial tendon dysfunction is severe and does not respond to conservative treatments, surgery may be considered. Surgery may involve tendon repair, release of adhesions, or other procedures depending on the specific nature of the dysfunction.
It is important to consult a healthcare professional, such as an orthopedist or podiatrist, to obtain an accurate diagnosis and an appropriate treatment plan based on the severity of the posterior tibial tendon dysfunction. Each case may be unique, and treatment can be tailored accordingly.
References and Useful Resources
- Ross MH, Smith MD, Mellor R, Vicenzino B. Exercise for posterior tibial tendon dysfunction: a systematic review of randomised clinical trials and clinical guidelines. BMJ Open Sport Exerc Med. 2018;4(1):e000430. [PMC free article] [PubMed]2.
- Holmes GB, Mann RA. Possible epidemiological factors associated with rupture of the posterior tibial tendon. Foot Ankle. 1992 Feb;13(2):70-9. [PubMed]3.
- Manske MC, McKeon KE, Johnson JE, McCormick JJ, Klein SE. Arterial anatomy of the tibialis posterior tendon. Foot Ankle Int. 2015 Apr;36(4):436-43. [PubMed]4.
- Uchiyama E, Kitaoka HB, Fujii T, Luo ZP, Momose T, Berglund LJ, An KN. Gliding resistance of the posterior tibial tendon. Foot Ankle Int. 2006 Sep;27(9):723-7. [PubMed]5.
- Jahss MH. Spontaneous rupture of the tibialis posterior tendon: clinical findings, tenographic studies, and a new technique of repair. Foot Ankle. 1982 Nov-Dec;3(3):158-66. [PubMed]6.
- Anderson JG, Harrington R, Ching RP, Tencer A, Sangeorzan BJ. Alterations in talar morphology associated with adult flatfoot. Foot Ankle Int. 1997 Nov;18(11):705-9. [PubMed]7.
- Mosier SM, Lucas DR, Pomeroy G, Manoli A. Pathology of the posterior tibial tendon in posterior tibial tendon insufficiency. Foot Ankle Int. 1998 Aug;19(8):520-4. [PubMed]8.
- Mann RA, Thompson FM. Rupture of the posterior tibial tendon causing flat foot. Surgical treatment. J Bone Joint Surg Am. 1985 Apr;67(4):556-61. [PubMed]9.
- Deland JT, Page A, Sung IH, O’Malley MJ, Inda D, Choung S. Posterior tibial tendon insufficiency results at different stages. HSS J. 2006 Sep;2(2):157-60. [PMC free article] [PubMed]10.
- Ellis SJ, Deyer T, Williams BR, Yu JC, Lehto S, Maderazo A, Pavlov H, Deland JT. Assessment of lateral hindfoot pain in acquired flatfoot deformity using weightbearing multiplanar imaging. Foot Ankle Int. 2010 May;31(5):361-71. [PubMed]11.
- Younger AS, Sawatzky B, Dryden P. Radiographic assessment of adult flatfoot. Foot Ankle Int. 2005 Oct;26(10):820-5. [PubMed]12.
- Nielsen MD, Dodson EE, Shadrick DL, Catanzariti AR, Mendicino RW, Malay DS. Nonoperative care for the treatment of adult-acquired flatfoot deformity. J Foot Ankle Surg. 2011 May-Jun;50(3):311-4. [PubMed]13.
- Imhauser CW, Abidi NA, Frankel DZ, Gavin K, Siegler S. Biomechanical evaluation of the efficacy of external stabilizers in the conservative treatment of acquired flatfoot deformity. Foot Ankle Int. 2002 Aug;23(8):727-37. [PubMed]14.
- Myerson MS, Badekas A, Schon LC. Treatment of stage II posterior tibial tendon deficiency with flexor digitorum longus tendon transfer and calcaneal osteotomy. Foot Ankle Int. 2004 Jul;25(7):445-50. [PubMed]15.
- Kadakia AR, Haddad SL. Hindfoot arthrodesis for the adult acquired flat foot. Foot Ankle Clin. 2003 Sep;8(3):569-94, x. [ PubMed ]16.
- Pellegrini MJ, Schiff AP, Adams SB, DeOrio JK, Easley ME, Nunley JA. Outcomes of Tibiotalocalcaneal Arthrodesis Through a Posterior Achilles Tendon-Splitting Approach. Foot Ankle Int. 2016 Mar;37(3):312-9. [PubMed]17.
- Smith JT, Bluman EM. Update on stage IV acquired adult flatfoot disorder: when the deltoid ligament becomes dysfunctional. Foot Ankle Clin. 2012 Jun;17(2):351-60. [PubMed]18.
- Pomeroy GC, Pike RH, Beals TC, Manoli A. Acquired flatfoot in adults due to dysfunction of the posterior tibial tendon. J Bone Joint Surg Am. 1999 Aug;81(8):1173-82. [PubMed]19.
- Iossi M, Johnson JE, McCormick JJ, Klein SE. Short-term radiographic analysis of operative correction of adult acquired flatfoot deformity. Foot Ankle Int. 2013 Jun;34(6):781-91. [PubMed]20.
- Alvarez RG, Marini A, Schmitt C, Saltzman CL. Stage I and II posterior tibial tendon dysfunction treated by a structured nonoperative management protocol: an orthosis and exercise program. Foot Ankle Int. 2006 Jan;27(1):2-8. [PubMed]21.
- Pinney SJ, Lin SS. Current concept review: acquired adult flatfoot deformity. Foot Ankle Int. 2006 Jan;27(1):66-75. [PubMed]22.
- Coetzee JC, Hansen ST. Surgical management of severe deformity resulting from posterior tibial tendon dysfunction. Foot Ankle Int. 2001 Dec;22(12):944-9. [PubMed]