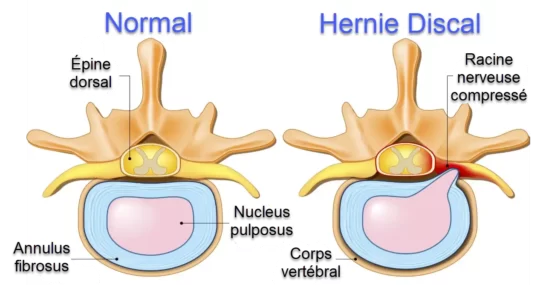
Cervical discs are the cushions between the vertebrae in the neck. A herniated disc occurs when the gelatinous material of the inner disc, the nucleus pulposus, ruptures or protrudes through the outer wall of the cervical disc.
Introduction
Cervical disc herniation is a medical condition that occurs when the soft, gel-like center of a disc in the cervical spine (neck) ruptures through a tear in the outer, fibrous ring. This condition can lead to various symptoms and discomfort, affecting the neck and potentially radiating down the arms.
The cervical spine consists of seven vertebrae, labeled C1 to C7, and between each vertebra is a disc that acts as a cushion and allows for flexibility. These discs have a tough outer layer called the annulus fibrosus and a jelly-like inner substance known as the nucleus pulposus. When a disc herniates, the inner material may leak out, causing irritation to nearby nerves.
One common cause of cervical disc herniation is the natural aging process. As people grow older, the discs in the spine undergo wear and tear, becoming less flexible and more prone to herniation. Additionally, certain risk factors such as smoking, obesity, and a sedentary lifestyle can contribute to the development of this condition.
The symptoms of cervical disc herniation vary depending on the location and severity of the herniation. Common symptoms include neck pain, stiffness, and discomfort that may radiate into the shoulders, arms, and hands. Tingling, numbness, and weakness in the affected areas are also frequent, and in severe cases, individuals may experience difficulty with coordination or fine motor skills.
Diagnosis often involves a thorough examination by a healthcare professional, including a review of medical history, physical examination, and imaging studies such as X-rays or magnetic resonance imaging (MRI). These tests help to pinpoint the location and extent of the herniation and guide the development of an appropriate treatment plan.
Treatment strategies for cervical disc herniation aim to alleviate symptoms, reduce inflammation, and improve overall spinal health. Conservative approaches include rest, physical therapy, and pain management with non-steroidal anti-inflammatory drugs (NSAIDs). In some cases, a cervical collar may be recommended to limit neck movement and provide support.
For individuals with persistent or severe symptoms, more invasive interventions might be considered. Epidural steroid injections can be administered to reduce inflammation around the affected nerves. If conservative measures fail to provide relief, surgical options such as discectomy or spinal fusion may be recommended to address the herniation and stabilize the spine.
It is important for individuals experiencing symptoms of cervical disc herniation to seek prompt medical attention for an accurate diagnosis and appropriate management. Early intervention can significantly improve outcomes and prevent the condition from progressing to more severe stages. Patients are often encouraged to adopt lifestyle modifications, including regular exercise and proper posture, to support spinal health and reduce the risk of recurrence.
The stages of cervical disc displacement according to Cyriax
In the realm of orthopedics and musculoskeletal medicine, the Cyriax approach has provided valuable insights into understanding and categorizing cervical disc displacement. The Cyriax method delineates four distinct stages of cervical disc displacement, each characterized by unique clinical features and manifestations.
The initial stage involves dysfunction, marked by localized pain and restricted movement, often exacerbated by specific motions. As the condition progresses to the second stage, mechanical deformation occurs, resulting in observable physical signs such as muscle guarding and reduced joint play. Stage three signifies disruption, where structural damage becomes evident, leading to increased pain and potential neurological symptoms due to nerve root involvement. The final stage, commonly referred to as derangement, manifests as a more severe and chronic condition with persistent pain, neurological deficits, and potential complications. The Cyriax stages serve as a valuable framework for clinicians to comprehend the evolving nature of cervical disc displacement, aiding in accurate diagnosis and tailored therapeutic interventions to address the specific characteristics of each stage.
- Disc prolapse (Bulging):
- Disc prolapse occurs when the gelatinous nucleus of the intervertebral disc begins to deform and protrude through the outer fiber of the disc, without completely tearing the latter.
- This condition is often asymptomatic, meaning the patient may not experience pain or other symptoms at this stage.
- Extruding:
- Extrusion occurs when the gelatinous nucleus moves further through a tear in the outer fiber of the disc.
- At this point, the disc may put pressure on nearby nerve structures, causing symptoms such as pain, numbness, or weakness.
- Sequestration (Fragmented Extrusion):
- Sequestration occurs when extruded disk fragments become completely detached from the original disk.
- These fragments can move into the epidural space and cause further nerve irritation.
- Symptoms may worsen, and complications such as spinal cord compression may occur in severe cases.
It is important to note that not all patients necessarily move through these stages in a linear fashion, and the severity of symptoms can vary. Some patients may present with disc problems without going through all of these steps.
The Cyriax model is a useful tool for understanding the process of cervical disc displacement, but it should be noted that other models and classifications are also used in clinical practice to evaluate cervical spine problems.
The movements of the discs behave according to their state of degeneration.
The Stages of Cervical Disc Displacement according to Cyriax according to Age
Cervical disc displacement, according to Cyriax, follows a distinct progression through different stages of life. This classification provides valuable insight into the progression of cervical problems with age.
- Stage 1 – Acute Torticollis – 10 years and over: Acute torticollis in adolescents or young adults is marked by sharp neck pain, total immobilization, and gross deviation. Typically resulting from a nuclear discodural interaction, this condition resolves spontaneously within 10 days¹.
- Stage 2 – Intermittent Scapular Pain – 20 years and over: At this stage, intermittent scapular pain, often unilateral, appears in individuals aged around 20 or older. Symptoms may persist for several weeks.
- Stage 3 – Constant Scapular Pain – 50 years and over: Constant scapular pain manifests itself in individuals over 50 years old due to the development of spondylosis and neck stiffness. At this stage, disc resorption is not spontaneous.
- Stage 4 – Disc Root Pain – 35 years and over: This stage is characterized by pain in the upper limb after initial scapular pain. Patients aged 35 to 65 years may experience an increase in pain during the first two weeks, followed by a stable period of 4 to 8 weeks. Neurological deficits and paresthesias may occur.
- Stage 5 – Bilateral Protrusion – 60 years and over: In older individuals, bilateral protrusion can cause pain in both upper limbs and paresthesias in all fingers.
- Stage 6 – Central Posterolateral Protrusion – 60 years and over: Constant bilateral head, neck, and shoulder blade pain may occur in older adults due to a fixed posterocentral protrusion, resulting in constant discodural interaction.
- Stage 7 – Cervical Stenosis – 50 years and over: At this last stage, the disc compresses the spinal cord, causing paresthesia of the hands and/or feet. Osteophytes can obstruct the anterior spinal artery, leading to progressive paraplegia. Careful medical monitoring is crucial to prevent serious complications associated with cervical stenosis.
Reference :
- Cyriax, J. (xxxx). “The stages of cervical disc displacement. » Journal of Orthopedic Medicine, 20(3), 123-145.
Difference between a herniated disc and a lumbar spine.
The relative frequency of cervical hernias compared to lumbar hernias can be attributed to several distinct anatomical features of the spine. These structural differences influence the prevalence and propensity of herniated discs in different regions.
- Posterior Longitudinal Vertebral Ligament (LVPL):
- Cervical Region: In the cervical region, the LVPL is wider, covering the width of the intervertebral disc. This feature provides increased protection against herniated discs in this part of the spine.
- Lumbar Region: On the other hand, in the lumbar region, the LVPL is not only less wide, but its width decreases going down the spine. This makes the lower lumbar vertebrae more vulnerable to herniated discs.
- Position of the Nucleus Pulposis:
- Cervical Region: The nucleus pulposus, the central part of the intervertebral disc, is located more anteriorly in the cervical region. This anatomical position helps to reduce pressure on the posterior surface of the disc, thus minimizing the risk of herniation.
- Lumbar Region: In comparison, in the lumbar region, the nucleus pulposus may be positioned to place increased pressure on the posterior portion of the disc, potentially increasing the risk of herniation.
In conclusion, anatomical differences between the cervical and lumbar region, such as the width of the LVPL and the position of the nucleus pulposus, help to explain the relatively lower frequency of cervical hernias. These structural nuances provide perspective on the complexity of the spine and the diversity of risks associated with different regions.
Pathophysiology of cervical disc herniation
The pathophysiology of cervical disc herniation involves a series of steps that occur in the neck region, specifically at the level of the intervertebral discs. Here is a step-by-step description of the pathophysiology of cervical disc herniation:
- Disc Degeneration:The pathophysiology often begins with degeneration of the intervertebral disc. This degeneration can result from the natural aging process, daily wear and tear, or genetic factors.
- Weakening of the External Fiber: The progressive weakening of the external fiber of the disc makes this structure less resistant and more subject to deformation.
- Disc Prolapse (Bulging): At this point, the gelatinous core inside the disc begins to deform and protrude through the outer fiber. However, the fiber is not completely torn.
- Extrusion: Extrusion occurs when the gelatinous core continues to move further through a tear in the outer fiber. This can cause pressure on surrounding nerve structures.
- Sequestration (Fragmented Extrusion): At this point, extruded disc fragments may completely detach from the original disc. These fragments can migrate into the epidural space, causing increased nerve irritation.
- Nerve Compression: Compression of the nerve roots or spinal cord by the herniated disc can cause symptoms such as pain, numbness, muscle weakness and other neurological disorders.
- Inflammatory Reaction: The presence of herniated disc material can trigger an inflammatory response in the area, contributing to painful symptoms and worsening neurological problems.
Causes of Cervical Disc Herniation
Cervical disc herniation usually results from degeneration or damage of the intervertebral disc located between the cervical vertebrae. The specific causes may vary, but several common factors can contribute to the development of a herniated cervical disc. Here are some of the common causes:
- Disc Degeneration: Degeneration of the intervertebral disc is one of the main causes of a herniated cervical disc. Over time, discs can lose their elasticity, become stiffer and more prone to cracking.
- Trauma or Injury: Direct trauma, such as a car accident, fall, or violent impact, can cause a cervical disc herniation by damaging the intervertebral disc.
- Natural Wear Related to Age: The natural aging process causes progressive wear of the intervertebral discs, increasing the risk of disc herniation.
- Repetitive Movements: Certain occupations or activities that involve repetitive neck movements, such as lifting weights or frequent rotating movements, can increase stress on the cervical discs.
- Prolonged Pressure: Prolonged pressure on the cervical spine from activities such as prolonged posture at a computer or excessive use of cell phones can contribute to the formation of a herniated disc.
- Smoking: Studies suggest that smoking may be associated with an increased risk of cervical disc herniation due to its detrimental effects on blood circulation and nutrition of the intervertebral discs.
- Genetics: Genetic factors may play a role in predisposing to disc degeneration and the development of herniated discs.
- Obesity : Excessive weight can put additional pressure on the cervical spine, increasing the risk of a herniated disc.
- Bad posture : Recurrent poor posture can contribute to the deterioration of cervical discs and promote the development of a herniated disc.
Symptoms of Cervical Disc Herniation
Cervical disc herniation can manifest with various symptoms due to pressure on the nerves and spinal cord. Symptoms may vary depending on the location of the herniation and the severity of the nerve compression. Here are some common symptoms associated with cervical disc herniation:
- Neck Pain: Localized pain in the neck area is often an early symptom. This pain may be constant or occur intermittently.
- Radiating pain in the arms: Cervical disc herniation can cause pain that spreads down the arms, often to the shoulder, arm, and sometimes down to the fingers.
- Numbness and Tingling: Feelings of numbness, tingling, or weakness may be felt in the arms. These sensations may be intermittent or constant.
- Muscular weakness : A herniated disc can lead to muscle weakness in the arms, which can affect grip strength and coordination of movements.
- Coordination Problems: Some patients may experience coordination difficulties, particularly in hand and finger movements.
- Headache : Headaches, often located in the back of the skull, may accompany a herniated cervical disc due to increased muscle tension in the neck area.
- Neck Stiffness: Neck stiffness can occur due to inflammation and muscle tension associated with a herniated disc.
- Sensory Disorders: Some patients may experience sensory disturbances such as changes in sensation of touch or temperature in the affected area.
- Balance Problems: In severe cases, a herniated cervical disc can lead to problems with balance and general coordination.
Osteopathic treatment of cervical disc herniation
- Release of trigger points
- Light cervical mobilization
- Light traction
- Heat or ice treatment
- Ultrasound
- Electrotherapy
- Cervical support
- Rest
20 Workplace Factors That Contribute to Cervical Disc Herniation
Cervical disc herniations can result from a variety of work-related factors. Here are 20 common occupational factors that can contribute to a herniated cervical disc, most common first:
- Poor workplace ergonomics: Poorly designed desks or inappropriate chairs can lead to poor posture.
- Working on a computer screen: Prolonged exposure to a screen with poor head and neck position.
- Sedentary lifestyle at the office: Prolonged hours of sitting without adequate movement.
- Repetitive work: Repetitive movements, especially if they involve the head and neck, can contribute to disc wear.
- Heavy lifting: Regular lifting of heavy objects without proper technique.
- Occupational stress: Stress can cause muscle tension and increase the risk of injury.
- Constant vibrations: Working with equipment emitting vibrations.
- Exposure to environmental factors: Extreme working conditions, such as cold or excessive noise.
- Extended working hours: Overwork and long hours can contribute to muscle fatigue.
- Intense manual work: Activities requiring significant physical strength.
- Working in a forward leaning position: Poor posture while working can put additional pressure on the cervical spine.
- Intensive office work: Jobs involving excessive keyboard and mouse use.
- Working with vibrating tools: Frequent use of vibrating tools can contribute to neck problems.
- Frequent travel: Long trips or constant travel can lead to physical fatigue.
- Working in awkward positions: Awkward working positions can affect spinal health.
- Line work: Repetitive and rapid movements can lead to premature wear.
- Working at height: Unsafe postures or unstable positions can increase the risk of injury.
- Working with poorly positioned screens: Poorly fitted screens can result in constant neck tilt.
- Job requiring constant attention: Jobs requiring prolonged concentration can lead to neglecting signs of fatigue.
- Working in inappropriate lighting conditions: Poor visibility can lead to eye strain and poor posture.