Introduction
Plantar fasciitis, often accompanied by heel spurs, is a foot condition that can cause a variety of painful symptoms. Plantar fasciitis is characterized by inflammation of the plantar fascia, a thin, extensive ligament that connects the heel bone to the toes, providing crucial support to the arch of the foot. This condition may be associated with an abnormal bone growth on the heel bone, known as a heel spur or Lenoir spur.
The plantar fascia plays a vital role in shock absorption during walking, helping to mitigate the impacts experienced by the foot on a daily basis. However, various factors, such as excessive pressure on the plantar fascia, can lead to tears at its attachment point to the heel, triggering an inflammatory process. Pain and stiffness in the heel are characteristic symptoms of plantar fasciitis.
A heel spur, also called a Lenoir spur, is an abnormal bone growth that can form in response to excessive traction exerted by the plantar fascia on the heel bone. These two elements are often linked, contributing to the complexity of the symptoms experienced by those suffering from this painful condition.
Location of Metatarsalgia and Plantar Fasciitis
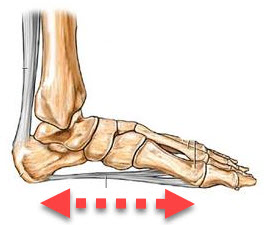
Metatarsalgia and plantar fasciitis are two common foot conditions that can cause significant pain and discomfort when walking or running. Metatarsalgia is characterized by localized pain in the heads of the metatarsals, the long bones located at the base of the toes, while plantar fasciitis manifests as pain in the heel, often centered under the heel or slightly toward the Before.
Metatarsalgia can affect one or more of the five metatarsal heads, but is most commonly felt under the second, third, and fourth metatarsal heads. This location corresponds to the area of maximum pressure during walking, where the weight of the body is transferred from the heel to the front of the foot. People with metatarsalgia may feel stabbing, burning, or shooting pain in these metatarsal heads, especially when standing, walking, or wearing uncomfortable shoes.
On the other hand, plantar fasciitis generally manifests itself as pain in the heel, more precisely at the point of attachment of the plantar fascia to the heel bone (calcaneus). This pain is often described as a sharp or stabbing pain, which may be more intense in the morning upon waking or after long periods of rest. Plantar fasciitis can also cause stiffness in the heel, which can make it difficult to walk or weight-bear the foot after a period of inactivity.
In terms of anatomy, metatarsalgia is often associated with excessive pressure on the metatarsal heads, sometimes resulting from muscular imbalances, biomechanical changes or excessive wear from shoes. On the other hand, plantar fasciitis is often caused by inflammation or overstretching of the plantar fascia, which can result from strenuous physical activity, wearing unsupportive shoes, or abnormal foot biomechanics.
Metatarsalgia
- Location of Pain: Metatarsalgia is characterized by pain in the metatarsal heads, which are the long bones located in the front of the foot, just before the toes.
- Associated Symptoms: Patients with metatarsalgia may feel a burning, tingling, or pressure sensation in the metatarsal heads. The pain may worsen with prolonged walking or standing.
Plantar Fasciitis
- Location of Pain: Plantar fasciitis generally causes pain in the heel, more specifically at the base of the heel where the plantar fascia attaches. This can also radiate to the arch of the foot.
- Associated Symptoms: The pain is often more intense in the morning, during the first steps after waking up. It may subside as the foot warms up, but may return after periods of activity.
Heel spur
- Relationship with Plantar Fasciitis: A heel spur is often associated with plantar fasciitis. It is formed by calcium deposits where the plantar fascia attaches to the calcaneus (heel bone).
- Location of Pain: Pain is generally localized in the heel, particularly on the lower part. The sensation may be similar to a sting or stab.
These conditions are often interconnected, as the plantar fascia is a fibrous band that runs from the heel to the toes, supporting the arch of the foot. Excessive activities, overuse, or biomechanical issues can lead to irritation, inflammation, and eventually metatarsalgia, plantar fasciitis, or a heel spur. If you experience persistent foot pain, it is advisable to consult a healthcare professional for an accurate diagnosis and appropriate treatment advice.
Causes of heel spur
Heel spur, also known as plantar fasciitis, is a painful condition that affects the arch of the foot, particularly in the heel area. Several factors can contribute to the development of this condition.
First, activities that put excessive stress on the foot, such as running, jumping, or walking on hard surfaces, can lead to repetitive strain injuries to the plantar fascia, causing inflammation and heel pain.
Additionally, certain anatomical factors may predispose to heel spurs. For example, poor foot posture, such as excessive pronation or supination, can cause body weight to be distributed unevenly across the foot, putting increased pressure on the plantar fascia and heel.
Inappropriate footwear can also play a role in the development of heel spurs. Shoes that fit poorly, are too worn, or don’t provide adequate arch support can put more stress on the plantar fascia and worsen symptoms.
Factors such as age and being overweight can also increase the risk of developing a heel spur. As we age, the body’s tissues, including the plantar fascia, tend to lose their elasticity and ability to absorb shock, making them more vulnerable to injury and inflammation. Likewise, excess weight puts additional pressure on the structures of the foot, which can worsen heel spur symptoms.
Finally, underlying medical conditions such as arthritis, diabetes, or a gait abnormality can also contribute to the development of heel spurs. These conditions can affect the health of the body’s connective tissues, including the plantar fascia, and increase the risk of injury and inflammation.
The specific causes of heel spurs are not always clear, but several factors can contribute to the development of this condition. Common causes include:
- Repetitive strain on the plantar fascia: One of the main causes of heel spurs is repetitive strain on the plantar fascia. This can result from certain physical activities, especially those that involve repetitive movements of the foot, such as running, prolonged walking, or activities that put excessive strain on the feet.
- Overuse or Changes in Activity: A sudden or excessive increase in physical activity, especially one that puts increased strain on the feet, can contribute to the development of plantar fasciitis.
- Poor arch support: Wearing shoes that do not provide adequate arch support or that are worn out can increase your risk of developing heel spurs.
- Foot Anatomy: Certain anatomical features of the foot, such as flat feet or an abnormally high arch, can increase tension on the plantar fascia and contribute to plantar fasciitis.
- Age: Heel spurs are more common in middle-aged people, although they can also occur in younger people.
- Biomechanical Factors: Biomechanical issues, such as abnormal gait, can cause uneven pressure on the plantar fascia, increasing the risk of developing plantar fasciitis.
- Obesity: Excess weight can put additional pressure on the plantar fascia, increasing the risk of developing problems such as heel spurs.
Symptoms of heel spur
Heel spur, also known as plantar fasciitis, is a painful foot condition characterized by heel pain, primarily in the lower, central part of the heel, where the plantar fascia attaches to the bone of the heel (calcaneus). Heel spur symptoms can vary in intensity and duration, but they are often described as following a common pattern.
Heel pain is the main symptom of heel spurs. This pain is generally felt during the first steps in the morning, after a prolonged period of rest, or after an intense activity that puts strain on the foot, such as running or prolonged walking. The pain may be sharp, stabbing, or burning, and tends to subside as the foot warms and the tissues stretch, but it may persist throughout the day in some people.
In addition to pain, heel spurs can also be associated with stiffness in the heel, particularly in the morning upon waking. This stiffness can make it difficult to weight-bear the foot and initially walk, and it may gradually improve with activity and stretching.
In some cases, heel spur pain may radiate to other parts of the foot, such as the arch or even the toes. This radiation of pain may be due to biomechanical compensation or overuse of other parts of the foot to avoid putting weight on the painful heel.
Additionally, heel spurs may be associated with local sensitivity to touch in the heel, particularly where the plantar fascia attaches to the heel bone. This sensitivity can be exacerbated by direct pressure on the heel, such as when pressing on it or wearing ill-fitting shoes.
Common symptoms of heel spur include:
- Heel pain: Pain is usually felt at the heel, often near the center or slightly on the inner side. The pain may be throbbing or stabbing and may vary in intensity.
- Increased pain in the morning: Many people with heel spurs experience increased heel pain in the morning, right after getting out of bed. This is often due to stiffness during the night and reactivation of pain when taking the first steps.
- Pain after rest: Pain may also be more severe after periods of rest or inactivity, since the plantar fascia tends to contract during these periods.
- Pain when walking or running: Pain may worsen during physical activity, especially when walking, running, or climbing stairs.
- Redness and swelling: There may be slight redness and swelling around the affected area.
- Sensitivity to touch: The area around the heel spur may be sensitive to touch.
- Limited mobility: Some individuals may experience limited mobility of the foot due to pain.
- Rest.
- Decreasing or even stopping activities that make pain worse is the first step to reducing pain.
- Stopping or reducing sports activities pound the feet on hard surfaces.
- Application of ice.
- Roll your foot on a bottle of cold water (or plastic bottle with water that has become ice cold) for 20 minutes (3 to 4 times a day).
- Footwear and orthotics.
- Shoes with thick soles and extra cushioning can reduce pain.
- When you walk and your heel hits the ground, significant tension is placed on the fascia, causing microtrauma (tiny tears in the tissue).
- A padded shoe or insert reduces this tension and the microtrauma that occurs with each step.
- Soft silicone heel cushions are inexpensive and work by elevating and cushioning your heel.
- Pre-made or custom orthotics (shoe inserts) are also helpful
- Heel support for heel spur
- A range of heel pieces are sold on the market with the aim of cushioning the impact shock of the heel when walking. These products are for the most part effective and allow you to be more functional.
Pathophysiology of the heel spur
Heel spur, also known as plantar fasciitis, is a medical condition characterized by heel pain, usually caused by inflammation of the plantar fascia, a band of tissue that connects the heel to the toes. Here is a step-by-step description of heel spur pathophysiology:
- Repetitive strain injuries: The most common cause of heel spurs is excessive tension on the plantar fascia. This may be due to repetitive strain injuries resulting from certain activities such as running, prolonged walking on hard surfaces, inappropriate footwear or biomechanical imbalances.
- Inflammation: Repetitive strain injuries can lead to inflammation of the plantar fascia. Inflammation is the body’s response to injury or irritation, and it often causes pain, redness, and swelling.
- Heel spur development: Over time, chronic inflammation can lead to the formation of a heel spur, a small bony growth on the heel. However, it is important to note that the presence of the heel spur does not always correlate with pain. Some individuals may have a heel spur without experiencing symptoms, while others may have significant pain without experiencing a spur.
- Microscopic rupture of the plantar fascia: Microtrauma can also cause microscopic ruptures in the plantar fascia. These small tears contribute to pain and can cause excessive scarring of the tissue, which can make the problem worse.
- Excessive heel traction: Excessive traction on the plantar fascia during walking or other activities can make symptoms worse. The first steps in the morning or after a prolonged period of rest are often the most painful due to the contraction of the fascia during rest.
- Risk Factors: Certain risk factors can contribute to the development of heel spurs, such as obesity, flat feet, abnormal gait, improper shoes, and certain medical conditions like arthritis.
Beneficial stretches for the heel spur
Heel spur, or plantar fasciitis, is a painful condition that affects the plantar fascia, a tissue that connects the heel to the toes. Stretching exercises can help relieve tension in this area. Here are some specific exercises that may benefit people with heel spurs:
- Plantar fascia stretching:
- Sitting on the floor or at the edge of a bed, extend the affected leg.
- Using your hand, gently pull the toes toward you until you feel a stretch along the ball of the foot and heel.
- Hold the position for 15 to 30 seconds.
- Repeat this exercise several times a day, especially in the morning before putting your foot on the ground.
- Calf stretch against the wall:
- Stand facing a wall with your hands pressed against it.
- Place the affected foot behind you, keeping the heel on the ground.
- Bend the knee of the front leg while keeping the back leg straight.
- You should feel the stretch in the calf of the back leg.
- Hold the position for 15 to 30 seconds.
- Repeat on the other side.
- Stretching with a frozen bottle:
- Place a frozen water bottle under the affected foot.
- Gently roll the bottle under the sole of your foot, applying light pressure.
- This can help reduce inflammation and relieve pain.
- Do this for a few minutes several times a day.
- Toe stretch with a towel:
- Sit on the floor with your legs extended in front of you.
- Place a towel around the sole of the affected foot.
- Gently pull on the towel to bring the toes toward you.
- Hold the position for 15 to 30 seconds.
- Stretching your toes with your fingers:
- Sit in a chair and cross the affected leg over the other knee.
- Use your fingers to gently pull the toes toward you.
- Hold the position for 15 to 30 seconds.
X-ray
Radiographic signs of heel spur (or plantar fasciitis) may include specific features that help healthcare professionals confirm the diagnosis. However, it is important to note that the presence of a heel spur on the x-ray does not always correspond to the severity of the symptoms experienced by the patient. Some individuals may have a heel spur without experiencing significant pain, while others may have severe pain without it necessarily being related to the presence of a heel spur. Here are some possible radiographic signs:
- Heel spur: X-ray may reveal the presence of a bone spur at the calcaneus (heel), which is often the classic feature of heel spur. However, not all patients with plantar fasciitis have a heel spur.
- Thickening of the plantar fascia: An x-ray may show thickening of the plantar fascia, indicating inflammation or excessive tension in the tissue.
- Enthesopathy: Enthesopathy is a condition characterized by inflammation at the enthesis, the area where the tendon or ligament attaches to the bone. In the case of heel spurs, the enthesis of the plantar fascia may show signs of inflammation.
It is essential to note that the diagnosis of plantar fasciitis does not rely solely on radiographic findings. The clinical picture, including the symptoms reported by the patient, the physical examination and sometimes additional tests such as ultrasound, can also be used to make an accurate diagnosis.
Conclusion
In conclusion, heel spur, also known as plantar fasciitis, is a painful foot condition characterized by heel pain, morning stiffness, and local tenderness to touch. These symptoms can cause significant discomfort when walking, running or even resting, thus affecting the quality of life of those affected. Prompt recognition and treatment of this condition is essential to prevent it from becoming chronic and to enable rapid and effective recovery. Treatment options may include stretching and strengthening exercises, wearing appropriate shoes, using orthotic insoles, physical therapy, and in some cases more advanced medical interventions. By working in collaboration with health professionals, it is possible to relieve pain, restore foot function and regain a better quality of life despite this sometimes debilitating condition.
References
- oexistence of plantar calcaneal spurs and plantar fascial thickening in individuals with plantar heel pain. Menz HB, Thomas MJ, Marshall M, et al. Rheumatology (Oxford) 2019;58:237–245. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. A study of calcaneal enthesophytes (spurs) in Indian population. Kullar JS, Randhawa GK, Kullar KK. Int J Appl Basic Med Res. 2014;4:0–6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. The plantar calcaneal spur: a review of anatomy, histology, etiology and key associations. Kirkpatrick J, Yassaie O, Mirjalili SA. J Anat. 2017;230:743–751. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. History and mechanical control of heel spur pain. Bergmann JN. https://europepmc.org/article/med/2189536 . Clin Podiatr Med Surg. 1990;7:243–259. [ PubMed ] [ Google Scholar ]
- 5. Biomechanics of longitudinal arch support mechanisms in foot orthoses and their effect on plantar aponeurosis strain. Kogler GF, Solomonidis SE, Paul JP. Clin Biomech Bristol Avon. 1996;11:243–252. [ PubMed ] [ Google Scholar ]
- 6. Obesity and pronated foot type may increase the risk of chronic plantar heel pain: a matched case-control study. Irving DB, Cook JL, Young MA, Menz HB. BMC Musculoskelet Disord. 2007;8:41. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. Lemont H, Ammirati KM, Usen N. J Am Podiatr Med Assoc. 2003;93:234–237. [ PubMed ] [ Google Scholar ]
- 8. The age dependent change in the incidence of calcaneal spur. Beytemür O, Öncü M. Acta Orthop Traumatol Turc. 2018;52:367–371. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Plantar calcaneal spurs in older people: longitudinal traction or vertical compression? Menz HB, Zammit GV, Landorf KB, Munteanu SE. J Foot Ankle Res. 2008;1:7. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. The relationship between the thickness and elasticity of the heel pad and heel pain. Ozdemir H, Urgüden M, Ozgörgen M, Gür S. https://dergipark.org.tr/en/pub/aott/issue/18086/190575 . Acta Orthop Traumatol Turkish. 2002;36:423–428. [ PubMed ] [ Google Scholar ]
- 11. The incidence, age dependence and sex distribution of the calcaneal spur. An analysis of its x-ray morphology in 1027 patients of the central European population. Riepert T, Drechsler T, Urban R, Schild H, Mattern R. Rofo. 1995;162:502–505. [ PubMed ] [ Google Scholar ]
- 12. Calcaneal spurs in a black African population. Banadda BM, Gona O, Vaz R, Ndlovu DM. Foot Ankle. 1992;13:352–354. [ PubMed ] [ Google Scholar ]
- 13. Incidence of calcaneal spurs in osteoarthrosis and rheumatoid arthritis, and in control patients. Bassiouni M. Ann Rheum Dis. 1965;24:490–493. [ PMC free article ] [ PubMed ] [ Google Scholar ]