Introduction to Fascia
Fascia, a complex and pervasive network of connective tissue, serves as a critical yet often overlooked component of the human body. Understanding fascia involves delving into both its structural composition and its historical journey through scientific inquiry.
What is Fascia?
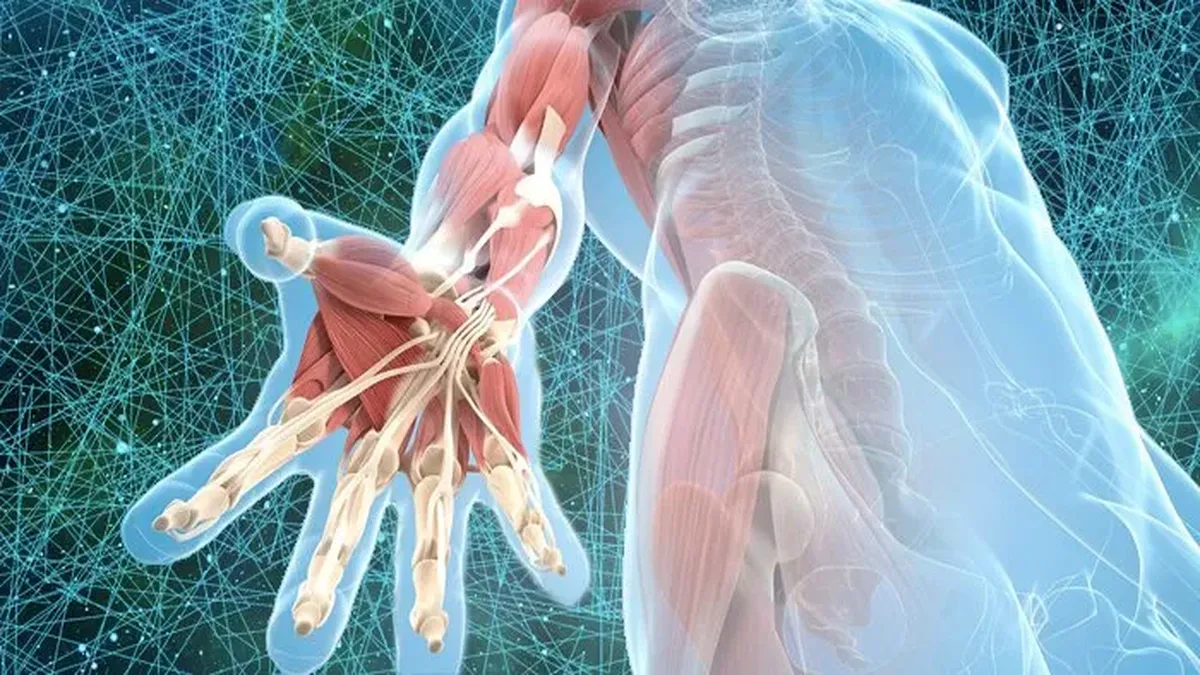
Fascia refers to the dense, fibrous connective tissue that surrounds and interconnects muscles, bones, nerves, and organs throughout the body. This intricate web not only provides structural support but also plays a crucial role in maintaining the body’s shape and function. Composed primarily of collagen, fascia exists in various forms—ranging from superficial layers just beneath the skin to deep layers surrounding muscles and organs.

The image above shows the fascia, a dense, fibrous connective tissue that envelops, supports, and connects muscles, bones, nerves, and organs throughout the body. Composed primarily of collagen, the fascia forms a continuous network that plays a fundamental role in anatomical structure and movement.
There are different types of fascia:
Superficial fascia: Located beneath the skin, it helps protect internal structures.
Deep fascia: Surrounds and separates muscles, nerves, and blood vessels.
Visceral fascia: Supports internal organs, keeping them in place.
The fascia is often compared to a three-dimensional spider web, as seen in the image, due to its interwoven fibers. This unique organization allows it to transmit mechanical forces throughout the body, facilitating mobility and postural balance.
However, the fascia can become rigid or adherent due to stress, trauma, or sedentary behavior, leading to pain and movement restrictions. Management includes techniques such as myofascial release or stretching exercises to restore its mobility and flexibility.
Thus, the fascia plays a key role in musculoskeletal health and overall well-being.
Beyond its structural role, fascia is increasingly recognized for its dynamic properties. It is involved in transmitting mechanical forces, regulating tension, and influencing movement patterns. This makes fascia integral to understanding biomechanics and the interconnectedness of bodily systems.
Historical Perspectives on Fascial Research
Ancient Beginnings: A Neglected Tissue
In early anatomical studies, fascia was largely disregarded as anatomists prioritized understanding more apparent structures like muscles, bones, nerves, and blood vessels. During dissections, fascia—this web-like connective tissue that surrounds and integrates every part of the body—was often removed to provide a clearer view of the underlying structures. This dismissal stemmed from a lack of understanding of its functional role and the tools available at the time, which limited the ability to study fascia’s finer details.
Ancient anatomists, such as Galen of Pergamon (2nd century AD), were among the first to provide detailed descriptions of the human body based on dissection and observation. However, their primary focus was on the musculoskeletal system, nerves, and vascular pathways, which were perceived as the most critical to the body’s function and health. Fascia, which enveloped these structures, was viewed merely as an inert “packing material” that provided mechanical support but lacked intrinsic importance. Galen’s anatomical theories, which dominated medical thought for centuries, described the body in terms of organs and systems but did not recognize the connective tissue’s role in integrating and supporting these systems.
This oversight was not entirely the fault of ancient anatomists but a reflection of the tools and methods available. Dissection techniques of the era were crude compared to modern standards, and the intricate, fibrous nature of fascia was difficult to preserve or study. As a result, fascia was often stripped away during dissections to expose muscles and organs, unintentionally perpetuating the idea that it was functionally insignificant.
The limited understanding of fascia in early anatomical studies significantly delayed the recognition of its true role. Only centuries later, with advances in imaging, histology, and biomechanics, has fascia been appreciated as a dynamic and integral tissue vital to force transmission, movement, and systemic health. Ancient anatomists like Galen may have unknowingly documented fascia’s presence, but its functional importance remained hidden until much later in medical history.
The Renaissance: Leonardo da Vinci’s Observations
Leonardo da Vinci (1452–1519), though primarily celebrated as an artist, was also a pioneering anatomist whose detailed dissections and drawings laid the groundwork for modern anatomy. While he did not specifically identify or name fascia as it is understood today, his meticulous studies of the human body often depicted the interconnected tissues that we now recognize as fascia.
- Observations of Interconnectedness: Leonardo’s anatomical work demonstrated a keen awareness of how muscles, tendons, and connective tissues worked together to form a unified structure. His dissections revealed the fibrous layers that surrounded and connected muscles, organs, and bones, elements that align closely with our current understanding of fascia.
- Detailed Illustrations: Some of Leonardo’s sketches, particularly those of musculature and joint systems, include depictions of the fibrous, web-like structures that correspond to fascia. Although fascia was not a defined concept during his time, his drawings hint at its role in supporting and integrating the body’s structures.
- Holistic Perspective: Leonardo viewed the body as a functional, interconnected system. This perspective aligns with the modern understanding of fascia as a continuous network that links all parts of the body, transmitting force and facilitating movement.
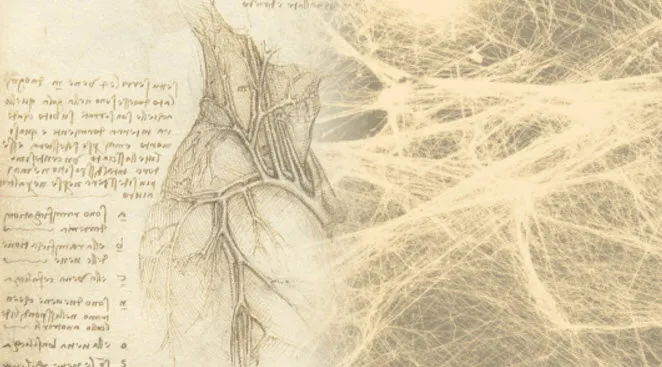
In his detailed dissections and anatomical sketches, Leonardo documented the relationships between muscles, tendons, and bones with unparalleled precision. While he did not explicitly identify fascia as we understand it today, his work often hinted at the fibrous, web-like tissues surrounding and supporting the body’s structures. The left side of this image reflects one of Leonardo’s anatomical drawings, while the modern depiction of fascia on the right visually parallels his findings, showing the intricate web of connective tissue.
Leonardo’s ability to capture the continuity and complexity of human anatomy was far ahead of his time. Today, researchers recognize fascia’s role in biomechanics, posture, and force transmission throughout the body. By bridging historical anatomical art with modern fascia research, this image pays homage to Leonardo’s pioneering spirit, demonstrating that his work remains profoundly relevant in uncovering the body’s hidden connections.
Leonardo da Vinci’s anatomical work, though centuries ahead of its time, provided a foundation for the exploration of fascia. Modern fascia research, which recognizes its dynamic role in biomechanics, postural stability, and health, echoes Leonardo’s vision of the body’s interconnected complexity. His studies remain a timeless reference, bridging the past and present in understanding human anatomy.
17th–18th Century: Early Mentions
During the 17th and 18th centuries, anatomical studies began to explore fascia with greater detail and recognition, yet its importance as a functional tissue remained overlooked. Anatomists like William Hunter and Jean-Baptiste de Sénac were among the first to describe fascia explicitly in their writings and dissections. Despite their contributions, the prevailing medical view of fascia during this period was still that of a passive structure, serving merely as a sheath or envelope for muscles, organs, and other key anatomical components.
William Hunter, a renowned 18th-century anatomist and physician, focused extensively on the layers of tissues within the human body. His dissections and lectures began to document fascia as part of the body’s structural architecture. Hunter noted the presence of thin, fibrous sheets surrounding muscles and organs, but his descriptions lacked an understanding of fascia’s dynamic properties, such as its role in movement and force transmission. Instead, he described fascia in terms of support and separation, framing it as a tissue that kept muscles and organs in their respective positions.
Similarly, Jean-Baptiste de Sénac, a French physician and anatomist, included fascia in his anatomical work, particularly in relation to the cardiovascular and musculoskeletal systems. De Sénac recognized the perivascular fascia (connective tissue surrounding blood vessels) and its importance in protecting these critical structures. However, like Hunter, his work focused on fascia’s protective and structural roles, not its active participation in biomechanical processes or its potential contribution to health and disease.
During this era, anatomical studies were heavily influenced by the priorities of the time, which focused on the muscles, nerves, and blood vessels as the key drivers of human physiology. As a result, fascia was not viewed as an integral system but rather as a passive bystander, overshadowed by the study of organs and other seemingly more dynamic tissues. While Hunter and de Sénac made strides in recognizing fascia’s existence, their work reflected the limited tools and conceptual frameworks of their time.
19th Century: A Functional Role Emerges
The 19th century marked a significant turning point in the understanding of fascia, as anatomists and surgeons began to recognize it as more than just a passive tissue. Researchers like Julius Wolff and Guillaume Dupuytren advanced the study of fascia by exploring its functional role in biomechanics and clinical significance, particularly its involvement in force transmission, structural support, and pathological conditions.
Julius Wolff, a German anatomist and surgeon, is best known for his work on Wolff’s Law, which describes how bone remodels in response to mechanical stress. In his studies, Wolff acknowledged the role of fascia in transmitting forces throughout the musculoskeletal system. He observed that fascia, through its tension and structural continuity, helps distribute mechanical loads efficiently across bones, muscles, and joints, maintaining the body’s structural integrity. This insight contributed to the growing understanding of fascia as an active participant in biomechanical processes rather than a mere “packing material.”
Around the same time, Guillaume Dupuytren, a French surgeon, brought fascia into the spotlight with his work on Dupuytren’s contracture, a condition characterized by the thickening and shortening of the palmar fascia in the hand. His detailed observations revealed that pathological changes in fascia could lead to severe functional impairments. Dupuytren’s work demonstrated that fascia was not just a structural element but also played a critical role in movement and mobility. His research on palmar fascia provided the first significant clinical evidence of fascia’s importance in both health and disease.

Additionally, 19th-century advances in surgical techniques and histological staining allowed anatomists to study fascia with greater precision. Surgeons observed how fascial planes could be used as natural pathways during dissections, minimizing damage to surrounding tissues. This practical knowledge reinforced the importance of fascia in maintaining structural organization and functional harmony within the body.
By the end of the 19th century, fascia was increasingly recognized as a dynamic tissue involved in force transmission, structural support, and disease processes. The pioneering work of Wolff, Dupuytren, and others laid the foundation for modern research into fascia’s role in biomechanics, movement, and health, paving the way for its growing importance in clinical practice and anatomical studies in the 20th century.
21st Century: A Fascia Renaissance
The 21st century has seen an explosion of interest and advancements in fascia research, marking what many refer to as a “fascia renaissance.” Spearheading this movement was the establishment of the Fascia Research Congress in 2007, which brought together anatomists, clinicians, and researchers to deepen our understanding of fascia as an integral and dynamic tissue. Alongside this collaboration, technological advancements in imaging techniques like ultrasound and MRI have allowed scientists to study fascia in unprecedented detail, revealing its complex structure and functional significance.

Key Discoveries
One of the most groundbreaking revelations is fascia’s role in force transmission and movement coordination. Research has shown that fascia forms a continuous, interconnected network throughout the body, enabling mechanical forces to be distributed efficiently across muscles, bones, and joints. This insight has redefined the way we understand movement, showing that fascia is not a passive layer but an active participant in biomechanics and functional movement patterns.
Another pivotal discovery is fascia’s contribution to pain perception. Studies have revealed that fascia contains a dense network of sensory nerves, including mechanoreceptors and nociceptors, making it highly sensitive to mechanical stress, inflammation, and injury. This has led to a better understanding of chronic pain syndromes, such as myofascial pain syndrome, where fascial dysfunction plays a key role in generating and perpetuating pain.
Fascia’s involvement in clinical conditions has also been extensively documented. Disorders such as fasciitis, chronic pain syndromes, and mobility restrictions often stem from or exacerbate fascial dysfunction. Conditions like plantar fasciitis, Dupuytren’s contracture, and frozen shoulder highlight how fascial abnormalities can impair mobility, cause discomfort, and significantly impact quality of life. Researchers have identified fascial adhesions and stiffness as primary contributors to these conditions, emphasizing the importance of maintaining fascial health.
Fascia’s New Role in Medicine
Today, fascia is recognized as a tissue with sensory, structural, and regulatory roles. Therapies like myofascial release, foam rolling, and targeted exercises have emerged to address fascial dysfunction. The understanding of fascia has transformed approaches to physical therapy, sports medicine, and chronic pain management, providing new tools for enhancing movement and alleviating pain.
The fascia renaissance of the 21st century has redefined anatomy, biomechanics, and therapeutic practice, cementing fascia as a cornerstone of human health and performance. This ongoing exploration continues to reshape our understanding of the body’s interconnected systems.
The Anatomy of Fascia: Structural Components and Variability
Fascia, often described as the body’s connective tissue matrix, is a complex and integral part of human anatomy, exhibiting both structural consistency and remarkable variability across different regions of the body.
Structural Components of Fascia
Fascia is primarily composed of collagen fibers, elastin, and a gel-like substance called ground substance. These components combine to form a resilient yet flexible network that surrounds and supports muscles, organs, blood vessels, and nerves throughout the body.
- Collagen Fibers: Predominantly type I collagen, these fibers provide tensile strength and structural integrity to fascial tissues. They are arranged in a parallel fashion in some areas to resist tension and are more loosely organized in others to allow for flexibility and movement.
- Elastin: Found alongside collagen, elastin fibers impart elasticity to fascia, enabling it to recoil after stretching and maintaining tissue shape and function.
- Ground Substance: This viscous gel-like substance fills the spaces between collagen and elastin fibers, providing lubrication and facilitating nutrient exchange and waste removal within the fascial matrix.
Variability in Fascial Architecture Across the Body
Despite its universal presence, fascia exhibits significant variability in its architectural organization and functional roles depending on its location within the body:
Superficial vs. Deep Fascia: Fascia can be categorized into superficial and deep layers. Superficial fascia lies just beneath the skin and often contains adipose tissue, while deep fascia surrounds muscles, bones, and joints, providing structural support and compartmentalization.
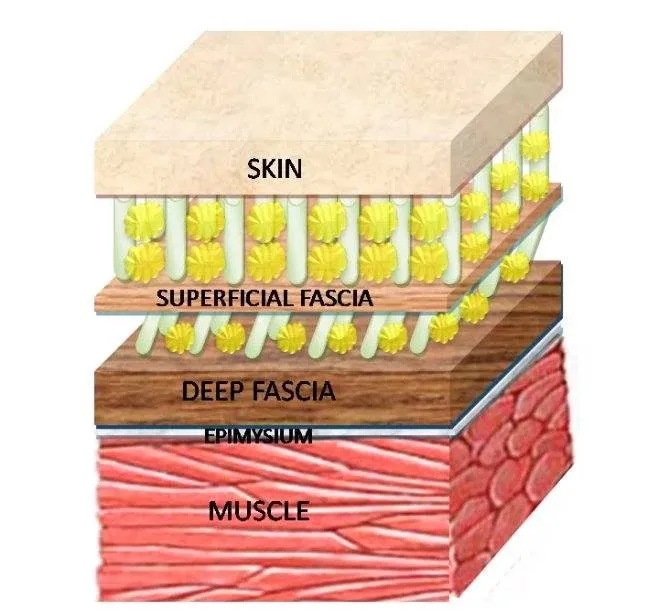
This image highlights the layers of fascia and its relationship with the skin, muscles, and other tissues in the human body. Fascia is a continuous connective tissue network that surrounds, supports, and separates structures like muscles, nerves, and blood vessels. It plays a crucial role in maintaining structural integrity, facilitating movement, and transmitting mechanical forces throughout the body.
Superficial fascia: Located just below the skin, this layer contains adipose (fat) tissue, blood vessels, and nerves. It provides cushioning, insulation, and allows for the movement of skin over deeper tissues.
Deep fascia: Found beneath the superficial fascia, this dense, fibrous layer surrounds and separates individual muscles, bones, and organs. It contributes to muscular coordination by reducing friction and transmitting force.
Epimysium: This fascial layer specifically envelops individual muscles, providing protection and structural support. It works in harmony with deeper fascia to facilitate contraction and force distribution.
Fascia is no longer seen as inert “packing material”; it is now recognized as a dynamic and responsive tissue vital for posture, movement, and stability. Dysfunction within fascia—whether from trauma, overuse, or inactivity—can result in stiffness, pain, and reduced mobility. Understanding its structure emphasizes the importance of maintaining fascial health through stretching, movement, and myofascial release techniques. This image clearly illustrates fascia’s interconnectedness within the body, showcasing its essential role in human anatomy.
Regional Variations: Fascial architecture varies greatly across different regions of the body. For example, in the limbs, fascia forms thick, fibrous structures such as the iliotibial tract and plantar fascia, which stabilize joints and facilitate movement. In contrast, facial fascia in the head and neck is thinner and more intricate, contributing to facial expression and cranial support.
Visceral Fascia: Fascia also envelops organs and viscera, forming layers that support organ position, provide cushioning, and allow for organ mobility during physiological processes such as digestion and respiration.
Functional Implications
Understanding the structural components and variability of fascial architecture is crucial for various fields, including medicine, physical therapy, and athletic training. It informs treatment approaches for conditions involving fascial dysfunction, such as myofascial pain syndrome, and guides rehabilitative strategies aimed at optimizing movement patterns and reducing injury risk.
Functions of Fascia: Support, Protection, and Biomechanical Influence
Fascia, a connective tissue network that pervades the entire body, serves essential functions in providing structural support, protecting organs and muscles, and facilitating biomechanical efficiency crucial for movement and overall health.
Support and Protection of Organs and Muscles
One of the primary functions of fascia is to provide structural support and maintain the integrity of bodily structures:
- Organ Support: Fascia forms a three-dimensional matrix that surrounds and supports internal organs, such as the kidneys, liver, and intestines. This supportive role helps maintain organ position and stability within the abdominal and thoracic cavities.
- Muscle Envelopes: Fascia surrounds individual muscles and groups of muscles, forming strong sheaths that provide protection against external trauma and facilitate smooth muscle contractions. For example, the thoracolumbar fascia in the lower back supports the spine and helps stabilize the trunk during movements.
- Joint Stability: Deep fascial layers contribute to joint stability by providing reinforcement around joints and enhancing proprioceptive feedback, which helps maintain balance and coordination.
Role in Biomechanics and Movement
Fascia plays a crucial role in optimizing biomechanical efficiency and enhancing movement dynamics throughout the body:
- Transmission of Force: Fascia acts as a transmission system for muscular forces, enabling efficient transfer of mechanical energy from one muscle group to another. This interconnected network allows coordinated movements and optimal muscle function during activities ranging from walking to complex athletic maneuvers.
- Tensegrity Principle: According to the tensegrity model, fascia maintains tensional integrity within the body. It balances tension and compression forces, optimizing posture and distributing mechanical stress evenly across tissues. This principle underlines fascia’s role in maintaining structural stability while allowing flexibility and adaptability to various movement patterns.
- Fascial Slings and Chains: Fascia forms interconnected slings and chains that span multiple joints and muscle groups. These myofascial chains facilitate kinetic energy transfer and coordinate movement patterns across the body. For example, the superficial back line connects the plantar fascia on the foot to the muscles along the back of the leg and spine, contributing to efficient running and walking mechanics.
Clinical Relevance
Understanding the multifaceted functions of fascia is crucial in clinical settings, such as physical therapy and sports medicine:
- Rehabilitation: Rehabilitation programs often incorporate fascial release techniques and exercises to improve tissue flexibility, reduce pain, and restore functional movement patterns.
- Injury Prevention: Maintaining healthy fascial integrity through proper movement mechanics and targeted exercises can help prevent overuse injuries and enhance athletic performance.
Fascia and Physiology: Relationship with the Nervous System, Circulation, and Fluid Dynamics
Fascia, a dynamic and interconnected network of connective tissue, plays integral roles in physiology beyond its structural functions. Understanding its interactions with the nervous system and its contributions to circulation and fluid dynamics provides insights into its profound influence on overall health and function.
Relationship with the Nervous System
Fascia is intricately linked with the nervous system, forming a complex network of sensory receptors and proprioceptive feedback mechanisms:
- Sensory Receptors: Fascia contains a variety of sensory receptors, including mechanoreceptors, nociceptors, and proprioceptors. These receptors respond to mechanical stimuli such as pressure, stretch, and tension, providing feedback to the brain about body position, movement, and the state of muscular and fascial tissues.
- Proprioception: Proprioceptive signals from fascia contribute to kinesthetic awareness and coordination. They help regulate muscle tone and joint stability, enabling smooth and efficient movement patterns. Dysfunction in fascial proprioception can lead to altered movement mechanics and increased injury risk.
- Neurofascial Interactions: Recent research highlights the role of neurofascial interactions, where fascia communicates bidirectionally with the nervous system. This interaction influences pain perception, motor control, and even emotional states, emphasizing fascia’s role beyond mechanical support.
Fascia’s Role in Circulation and Fluid Dynamics
Beyond its structural framework, fascia contributes significantly to circulation and fluid dynamics within the body:
- Interstitial Fluid Movement: Fascial layers act as pathways for interstitial fluid movement. This fluid supports cell nutrition, waste removal, and immune surveillance, crucial for tissue health and function.
- Lymphatic Drainage: Fascial planes guide lymphatic vessels that remove excess fluid and metabolic waste from tissues. Efficient lymphatic drainage facilitated by fascial pathways supports immune function and reduces inflammation.
- Blood Flow Regulation: Fascial tensions and adhesions can affect blood vessel permeability and blood flow dynamics. Restrictions in fascial planes may contribute to localized ischemia or impaired tissue perfusion, influencing healing processes and tissue viability.
Clinical Implications
Understanding fascia’s physiological interactions informs clinical practices across various disciplines:
- Manual Therapy: Techniques such as myofascial release aim to restore fascial mobility and optimize fluid dynamics, promoting tissue healing and pain relief.
- Rehabilitation: Integrating exercises that target fascial mobility and proprioception enhances functional recovery and movement rehabilitation post-injury or surgery.
- Holistic Health Approaches: Recognizing fascia’s role in nervous system regulation and fluid dynamics supports holistic health approaches that integrate physical, mental, and emotional well-being.
Fascia and Healing: Response to Injury and Role in Tissue Repair and Regeneration
Fascia, an intricate network of connective tissue, plays a pivotal role in the body’s response to injury and its processes of tissue repair and regeneration. Understanding how fascia responds to injury and inflammation, as well as its role in these healing processes, is crucial for advancing therapeutic interventions and promoting optimal recovery.
How Fascia Responds to Injury and Inflammation
When fascia is injured, it undergoes a series of complex responses aimed at mitigating damage and initiating repair:
- Inflammatory Response: Upon injury, the body triggers an inflammatory response, characterized by the release of cytokines and growth factors. These signaling molecules attract immune cells to the injury site, which helps to clear debris and prevent infection. However, excessive or prolonged inflammation can lead to fibrosis, where fascia becomes thickened and less flexible.
- Fibroblast Activation: Fascia contains fibroblasts, specialized cells responsible for producing collagen and other extracellular matrix components. Following an injury, fibroblasts become activated and migrate to the damaged area, where they synthesize new collagen fibers to replace those that were damaged.
- Myofibroblast Formation: Fibroblasts can differentiate into myofibroblasts, which have contractile properties similar to smooth muscle cells. Myofibroblasts help to contract and close the wound, promoting tissue approximation and reducing the size of the injury.
- Matrix Remodeling: The initial collagen laid down by fibroblasts is typically disorganized and forms a scar tissue matrix. Over time, this matrix undergoes remodeling, where collagen fibers are realigned and organized to restore the tissue’s tensile strength and functional integrity.
Fascia’s Role in Tissue Repair and Regeneration
Fascia is not merely a passive bystander but an active participant in the healing process:
- Scaffold for Tissue Repair: Fascia provides a structural scaffold that supports the regeneration of damaged tissues. This scaffold facilitates cell migration, nutrient delivery, and waste removal, all of which are essential for effective tissue repair.
- Mechanical Environment: The mechanical properties of fascia influence the healing process. Proper fascial tension and mobility can create an optimal mechanical environment that supports tissue regeneration. Conversely, fascial restrictions can impede healing and lead to chronic pain and dysfunction.
- Stem Cell Niche: Fascia serves as a niche for mesenchymal stem cells (MSCs), which have the potential to differentiate into various cell types, including fibroblasts, osteoblasts, and chondrocytes. These stem cells contribute to tissue regeneration and repair by replenishing damaged cells and promoting the formation of new tissue.
- Electrical Signaling: Emerging research suggests that fascia may play a role in bioelectric signaling, which influences cell behavior and tissue healing. Electrical fields within the fascia can guide cell migration and proliferation, contributing to the coordinated repair of injured tissues.
Clinical Implications
Understanding fascia’s role in healing has significant implications for clinical practice:
- Manual Therapies: Techniques such as myofascial release and fascial manipulation aim to enhance fascial mobility, reduce adhesions, and promote optimal healing environments. These therapies can alleviate pain and improve functional outcomes in patients with fascial injuries.
- Rehabilitative Strategies: Incorporating exercises that promote fascial flexibility and strength can aid in the recovery process. Such strategies help to restore normal tissue architecture and prevent the formation of restrictive scar tissue.
- Integrative Approaches: Combining conventional medical treatments with fascial-focused therapies can lead to more comprehensive and effective healing outcomes. This integrative approach acknowledges the multifaceted role of fascia in tissue repair and regeneration.
Clinical Implications of Fascia: Relevance to Medical Disciplines and Applications in Osteopathy and Physical Therapy
The understanding of fascia’s intricate roles in the body has profound clinical implications, influencing various medical disciplines and enhancing therapeutic approaches in osteopathy and physical therapy. Recognizing fascia’s relevance and leveraging this knowledge can improve patient outcomes and advance holistic healthcare practices.
Fascia’s Relevance to Various Medical Disciplines
Fascia’s complex structure and functions make it relevant to a wide array of medical fields:
- Sports Medicine: In sports medicine, fascia’s role in movement, force transmission, and injury recovery is crucial. Injuries often involve fascial structures, and treatments focusing on fascia can aid in quicker and more effective recovery for athletes.
- Pain Management: Chronic pain conditions, such as myofascial pain syndrome and fibromyalgia, are often linked to fascial dysfunction. Understanding fascia’s involvement in pain pathways can lead to better diagnostic and therapeutic strategies, including targeted manual therapies and interventions to alleviate pain.
- Rheumatology: Rheumatic conditions like rheumatoid arthritis and systemic sclerosis affect connective tissues, including fascia. Addressing fascial health can improve mobility and reduce pain in patients with these chronic inflammatory diseases.
- Surgery: Surgeons need to consider fascial planes and structures during procedures to minimize damage and promote optimal healing. Post-surgical recovery can be enhanced by therapies that maintain or restore fascial integrity.
- Neurology: The fascial system’s interaction with the nervous system influences conditions such as neuropathic pain and carpal tunnel syndrome. Understanding these connections aids in developing comprehensive treatment plans that address both neural and fascial components.
Applications in Osteopathic and Physical Therapy Practices
Osteopathy and physical therapy have long recognized the importance of fascia, integrating this knowledge into various therapeutic approaches:
- Osteopathic Manipulative Treatment (OMT): Osteopaths use techniques like myofascial release, fascial unwinding, and craniosacral therapy to address fascial restrictions and improve bodily function. These techniques aim to restore fascial mobility, enhance circulation, and support the body’s natural healing processes.
- Fascial Release Techniques: Physical therapists often employ fascial release techniques to treat musculoskeletal pain and dysfunction. Methods such as foam rolling, manual fascial release, and instrument-assisted soft tissue mobilization help reduce fascial adhesions and improve tissue flexibility and mobility.
- Functional Movement Rehabilitation: Both osteopaths and physical therapists incorporate functional movement exercises that focus on restoring fascial integrity and promoting efficient movement patterns. These exercises help prevent injury, enhance performance, and facilitate recovery.
- Postural Alignment and Correction: Fascia plays a critical role in maintaining posture and alignment. Therapies that target fascial imbalances can correct postural deviations, reduce strain on the musculoskeletal system, and alleviate associated pain.
- Scar Tissue Management: After surgery or injury, scar tissue can lead to fascial restrictions. Techniques to mobilize scar tissue and restore fascial glide are essential components of rehabilitation protocols, aiding in the restoration of normal movement and function.
Integrative Approaches
Integrating fascial knowledge across medical disciplines promotes a holistic approach to patient care:
- Collaborative Care: Collaboration between different healthcare providers, including osteopaths, physical therapists, and medical doctors, can lead to comprehensive treatment plans that address both the structural and functional aspects of fascial health.
- Patient Education: Educating patients about the importance of fascia and self-care techniques, such as stretching and foam rolling, empowers them to take an active role in their recovery and long-term health.
- Research and Innovation: Ongoing research into fascia’s roles and therapeutic potential continues to inform clinical practice. Innovations in diagnostic tools and treatment modalities are likely to emerge as our understanding of fascia deepens.
Fascia in Pathology and Pain: Fascia-Related Disorders and Chronic Pain Syndromes
Fascia, the connective tissue network that supports and envelops various structures in the body, plays a significant role in pathology and pain. Fascia-related disorders and conditions often contribute to chronic pain syndromes, highlighting the importance of understanding fascia’s involvement in these complex issues.
Fascia-Related Disorders and Conditions
Several disorders and conditions specifically involve fascia, leading to pain and dysfunction:
Disorders and conditions
- Myofascial Pain Syndrome: Characterized by the presence of trigger points within the fascial and muscular tissues, myofascial pain syndrome causes localized and referred pain. Trigger points are hyperirritable spots within a taut band of muscle or fascia, leading to significant discomfort and restricted movement.
- Plantar Fasciitis: This condition involves inflammation of the plantar fascia, a thick band of tissue running along the bottom of the foot. It causes sharp heel pain, particularly with the first steps in the morning or after prolonged periods of standing.
- Dupuytren’s Contracture: A condition where the fascia of the palm thickens and tightens, leading to the bending of fingers towards the palm. This progressive disorder can severely impair hand function.
- Adhesive Capsulitis (Frozen Shoulder): In this condition, the fascia and capsule surrounding the shoulder joint become inflamed and stiff, resulting in pain and severely limited range of motion.
- Fascial Adhesions: These are bands of scar tissue that form between fascial layers after injury, surgery, or inflammation. Adhesions restrict tissue mobility and can cause pain and functional limitations.
- Ehlers-Danlos Syndrome (EDS): EDS is a group of connective tissue disorders characterized by hypermobile joints, skin hyperextensibility, and tissue fragility. The collagen abnormalities in EDS affect the structural integrity of fascia, leading to various complications. Individuals with EDS often experience chronic pain, joint dislocations, and subluxations due to the laxity of fascial tissues. Fascial dysfunction in EDS can also lead to gastrointestinal issues and cardiovascular problems.
- Chronic Fatigue Syndrome (CFS): CFS, also known as myalgic encephalomyelitis (ME), is a complex disorder characterized by extreme fatigue that doesn’t improve with rest and is worsened by physical or mental activity. Fascial restrictions and adhesions may contribute to the musculoskeletal pain and stiffness commonly reported in CFS patients. Dysfunctional fascia can also impair lymphatic and vascular circulation, potentially exacerbating fatigue and systemic symptoms.
- Scleroderma: Scleroderma is an autoimmune disease that involves hardening and tightening of the skin and connective tissues, including fascia. The excessive collagen deposition in scleroderma can lead to significant fascial thickening and fibrosis, resulting in reduced skin elasticity, joint mobility, and organ function.
- Polymyalgia Rheumatica (PMR): PMR is an inflammatory disorder causing muscle pain and stiffness, particularly in the shoulders and hips. Fascia inflammation in PMR leads to pain and restricted movement. The condition often requires anti-inflammatory treatment to manage symptoms and improve function.
- Compartment Syndrome .Compartment syndrome occurs when increased pressure within a fascial compartment (a group of muscles, nerves, and blood vessels covered by fascia) impairs blood flow and nerve function. This condition can result from trauma, repetitive activity, or tight casts/bandages. Acute compartment syndrome is a medical emergency requiring prompt surgical intervention to prevent permanent damage.
- Lymphedema: Lymphedema is the swelling of body parts, usually the limbs, due to lymphatic system blockages. Fascial restrictions can impair lymphatic flow, contributing to fluid accumulation and swelling. Manual lymphatic drainage and fascial release techniques can help manage lymphedema by improving lymphatic circulation.
- Plantar Fibromatosis (Ledderhose Disease): Plantar fibromatosis is a condition characterized by the development of benign, slow-growing nodules in the plantar fascia of the foot. These nodules can cause pain and discomfort, especially when walking or standing. Treatment options include physical therapy, orthotics, and in some cases, surgical intervention.
- Tension-Type Headaches: Tension-type headaches are the most common form of headaches, often caused by muscle tension and stress.
- Fascial tightness and trigger points in the neck and scalp muscles can contribute to the development of tension headaches. Techniques like myofascial release and massage therapy can help alleviate these headaches by addressing fascial and muscular tension.
Role of Fascia in Chronic Pain Syndromes
Fascia plays a critical role in the development and maintenance of chronic pain syndromes:
- Tension and Stress Transmission: Fascia transmits mechanical stress and tension throughout the body. Chronic tension or stress within fascial tissues can lead to pain and dysfunction, contributing to conditions such as tension headaches and temporomandibular joint disorders (TMJ).
- Neurofascial Interactions: Fascia is rich in sensory nerve endings and can generate and perpetuate pain signals. Chronic irritation or inflammation of fascial tissues can lead to persistent pain and hypersensitivity, as seen in conditions like fibromyalgia.
- Central Sensitization: Chronic pain syndromes often involve central sensitization, where the central nervous system becomes hypersensitive to pain signals. Fascial dysfunction can contribute to this process by continuously sending pain signals, even in the absence of ongoing injury or inflammation.
- Restricted Movement and Compensatory Patterns: Fascial restrictions can alter movement patterns, leading to compensatory mechanisms that place additional stress on other tissues and joints. Over time, these compensatory patterns can cause widespread pain and dysfunction.
Clinical Implications and Treatment Approaches
Understanding the role of fascia in pathology and pain informs various treatment approaches:
- Myofascial Release Therapy: Manual techniques aimed at releasing fascial restrictions and trigger points can help alleviate pain and restore normal tissue function. Techniques include hands-on manipulation, foam rolling, and instrument-assisted soft tissue mobilization.
- Stretching and Mobility Exercises: Regular stretching and mobility exercises can help maintain fascial flexibility and prevent adhesions. Yoga, pilates, and specific fascial stretching routines are effective in promoting fascial health.
- Postural and Movement Re-education: Addressing poor posture and dysfunctional movement patterns can reduce fascial stress and prevent the development of chronic pain syndromes. Physical therapists often use movement re-education techniques to optimize functional movement.
- Integrative Therapies: Combining manual therapies with other modalities such as acupuncture, dry needling, and electrotherapy can enhance the effectiveness of fascial treatment and pain management.
- Patient Education and Self-Care: Educating patients about the importance of fascia and self-care techniques empowers them to manage and prevent pain. Techniques such as foam rolling, gentle stretching, and mindful movement can be incorporated into daily routines.
Fascia in Sports and Performance
Fascia, the connective tissue that encases and supports muscles, bones, and organs, plays a crucial role in athletic performance. Its influence extends beyond structural support, affecting movement efficiency, injury prevention, and overall athletic capability. Understanding the impact of fascia on performance and adopting strategies to optimize fascial health can enhance athletic outcomes.
Impact of Fascia on Athletic Performance
1. Force Transmission and Efficiency:
- Role in Force Transmission: Fascia connects and transmits forces between muscles, enhancing the efficiency of movement. Efficient force transmission allows for more powerful and coordinated movements.
- Energy Storage and Release: Fascia acts as an elastic storage system, storing energy during muscle lengthening and releasing it during muscle shortening, much like a spring. This contributes to the rebound effect seen in running and jumping.
2. Movement Coordination and Stability:
- Integrated Movement: Fascia integrates various body parts, enabling coordinated and smooth movements. Proper fascial function ensures that movements are efficient and fluid, reducing energy expenditure.
- Stability and Proprioception: Fascia is rich in proprioceptors, which provide feedback about body position and movement. This enhances stability and balance, crucial for athletic performance.
3. Injury Prevention:
- Load Distribution: Fascia distributes mechanical stress across muscles and joints, reducing the risk of overloading specific areas. This helps prevent injuries caused by repetitive stress or acute overload.
- Shock Absorption: The elastic properties of fascia allow it to absorb and dissipate impact forces, protecting muscles and joints from injury.
4. Recovery and Adaptation:
- Tissue Repair: Fascia plays a role in tissue repair and regeneration following injury. Healthy fascia promotes quicker recovery and adaptation to training loads.
- Inflammation and Healing: Fascia can influence inflammatory responses and tissue healing processes, impacting recovery times and the effectiveness of rehabilitation.
Strategies for Optimizing Fascial Health in Athletes
1. Dynamic Stretching and Mobility Exercises:
- Functional Flexibility: Incorporate dynamic stretching routines that mimic athletic movements. This helps maintain fascial flexibility and ensures tissues are prepared for the demands of sports.
- Mobility Drills: Perform mobility drills to enhance joint range of motion and fascial pliability. Exercises such as leg swings, arm circles, and hip openers are effective.
2. Myofascial Release Techniques:
- Foam Rolling: Regular use of foam rollers can help release fascial tension and adhesions. Focus on major muscle groups and areas prone to tightness, such as the calves, quads, and back.
- Manual Therapy: Techniques such as myofascial release, massage, and trigger point therapy can be performed by trained therapists to address deeper fascial restrictions.
3. Strength and Conditioning:
- Functional Strength Training: Engage in strength training exercises that promote functional movement patterns. Compound movements like squats, deadlifts, and lunges enhance fascial integration and strength.
- Core Stability: Strengthen the core muscles to support fascial structures and improve overall stability and power.
4. Hydration and Nutrition:
- Hydration: Maintain proper hydration to keep fascial tissues supple and pliable. Dehydrated fascia is more prone to stiffness and injury.
- Nutrient-Rich Diet: Consume a balanced diet rich in nutrients that support connective tissue health, such as collagen, vitamins C and E, and omega-3 fatty acids.
5. Recovery and Rest:
- Active Recovery: Incorporate active recovery sessions, such as light jogging, swimming, or yoga, to promote blood flow and fascial health without adding stress to the body.
- Rest and Sleep: Ensure adequate rest and sleep to allow fascia and other tissues to repair and regenerate.
6. Neuromuscular Training:
- Proprioceptive Training: Engage in exercises that enhance proprioception and body awareness, such as balance drills and agility training. This helps improve coordination and reduces the risk of injury.
- Plyometrics: Incorporate plyometric exercises to train the elastic properties of fascia. Movements like jump squats, box jumps, and bounding exercises are effective.
7. Mind-Body Practices:
- Yoga and Pilates: Practices like yoga and Pilates can improve fascial flexibility, strength, and awareness. These disciplines emphasize controlled movements and mindful stretching.
- Breathwork and Relaxation: Techniques such as deep breathing and relaxation exercises can reduce stress and tension in fascial tissues, promoting overall health.
Conclusion
Fascia, the intricate connective tissue webbing throughout our bodies, is a fundamental yet often overlooked component in both athletic performance and holistic health. Its roles extend far beyond mere structural support, influencing movement efficiency, injury prevention, and overall functional capacity. Understanding fascia provides a deeper insight into the mechanics of our bodies and the interconnected nature of our physiological systems.
Key Takeaways About Fascia
Fascia’s primary function is to support and protect our organs, muscles, and bones. It facilitates efficient force transmission, allowing for powerful and coordinated movements essential in athletic performance. Additionally, fascia plays a crucial role in movement coordination and stability, thanks to its integration of various body parts and its rich supply of proprioceptors, which enhance balance and body awareness.
Fascia’s involvement in chronic pain syndromes cannot be understated. Dysfunctional fascia can lead to a range of conditions such as myofascial pain syndrome, plantar fasciitis, and fascial adhesions, contributing significantly to chronic pain and restricted movement. Understanding these conditions helps in developing effective treatments that target the underlying fascial issues.
Optimizing fascial health involves a multifaceted approach, including dynamic stretching, myofascial release, functional strength training, proper hydration, and balanced nutrition. Recovery practices such as active recovery, adequate rest, and mind-body techniques like yoga further support fascial flexibility and overall well-being.
The Importance of Understanding Fascia in Holistic Health Practices Like Osteopathy
In holistic health practices such as osteopathy, a comprehensive understanding of fascia is indispensable. This knowledge allows practitioners to adopt a holistic perspective, considering the interconnectedness of the body’s systems in their treatments. By recognizing fascial patterns and dysfunctions, osteopaths can provide personalized assessments and interventions tailored to the unique needs of each patient.
Understanding fascia also enhances therapeutic outcomes. Techniques like myofascial release and manual therapy can be employed more effectively, addressing the root causes of pain and dysfunction rather than just the symptoms. Furthermore, educating patients about the role of fascia empowers them to engage actively in their care, adopting self-care practices that promote long-term health.
The broad applicability of fascia knowledge allows practitioners to address a wide range of conditions, from sports injuries and chronic pain to stress-related tension and postural imbalances. This understanding fosters collaboration across health disciplines, creating a more integrated and effective healthcare system.
References
- Lesondak, D. (2022). Fascia: What it is and Why it Matters (Second Edition). Handspring Publishing.
- Schleip, R., Findley, T. W., Chaitow, L., & Huijing, P. A. (2012). Fascia: The Tensional Network of the Human Body: The Science and Clinical Applications in Manual and Movement Therapy. Elsevier Health Sciences.
- Stecco, C., & Stecco, A. (2014). Functional Atlas of the Human Fascial System. Elsevier Health Sciences.
- Langevin, H. M., & Sherman, K. J. (2007). Pathophysiological model for chronic low back pain integrating connective tissue and nervous system mechanisms. Medical Hypotheses, 68(1), 74-80.
- Wilke, J., Krause, F., Vogt, L., & Banzer, W. (2016). What is evidence-based about myofascial chains: A systematic review. Archives of Physical Medicine and Rehabilitation, 97(3), 454-461.
- Findley, T. W., & Schleip, R. (2007). Fascia research: Implications for massage therapy. Journal of Bodywork and Movement Therapies, 11(1), 50-52.
- Pischinger, A. (2007). Matrix and Matrix Regulation: Basis for a Holistic Theory in Medicine. Medicina Biologica.
- Bordoni, B., & Lintonbon, D. (2019). The fascial system and exercise intolerance in chronic fatigue syndrome. Cureus, 11(6), e4856.
- Langevin, H. M. (2014). Connective tissue: A body-wide signaling network? Medical Hypotheses, 82(1), 75-80.
- Myers, T. W. (2020). Anatomy Trains: Myofascial Meridians for Manual and Movement Therapists (Fourth Edition). Elsevier Health Sciences.
4o