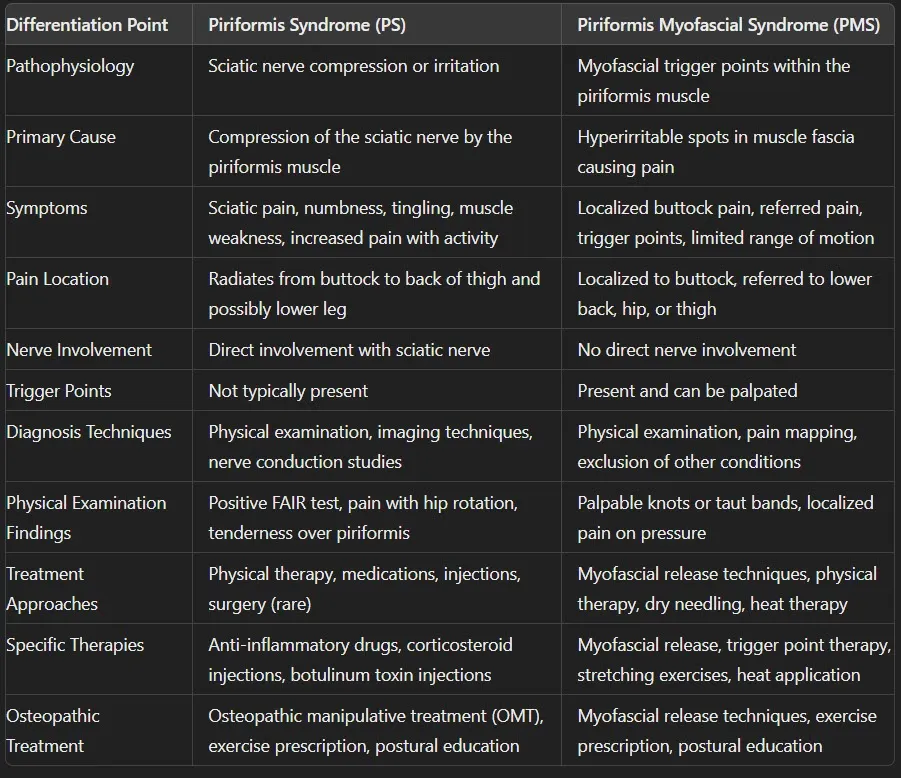
Introduction
Piriformis Syndrome (PS) and Piriformis Myofascial Syndrome (PMS) are two medical conditions that involve the piriformis muscle, located deep in the buttock region. Although these conditions share some overlapping symptoms, they are fundamentally different in their underlying mechanisms, clinical presentations, and treatment approaches.
Overview of Piriformis Syndrome (PS)
Piriformis Syndrome is primarily a neuromuscular disorder where the piriformis muscle irritates or compresses the sciatic nerve. This condition often leads to sciatic pain, which can radiate from the buttock down the back of the thigh and even into the lower leg. The compression of the sciatic nerve may result from various factors, including anatomical variations, acute trauma, repetitive stress injuries, or inflammation of the piriformis muscle. Patients with PS typically experience symptoms that worsen with activities like sitting, climbing stairs, or performing deep squats.
Overview of Piriformis Myofascial Syndrome (PMS)
Piriformis Myofascial Syndrome, on the other hand, is a condition characterized by the presence of myofascial trigger points within the piriformis muscle. These trigger points are hyperirritable spots that cause localized pain and can refer pain to other areas, such as the lower back, hip, or thigh. Unlike PS, PMS is not associated with sciatic nerve compression but rather with muscular dysfunction and tightness. Symptoms of PMS are generally more focused on the buttock area and can include a deep, aching pain that is exacerbated by pressure on the trigger points.
Importance of Differentiating Between the Two Conditions
Differentiating between Piriformis Syndrome and Piriformis Myofascial Syndrome is crucial for several reasons. First, the underlying causes of these conditions are different, necessitating distinct diagnostic approaches. Accurate diagnosis ensures that patients receive appropriate and effective treatments tailored to their specific condition. For instance, treatments targeting nerve compression in PS might not be effective for PMS, where the focus should be on relieving muscle trigger points and improving muscle function.
Moreover, misdiagnosis can lead to prolonged pain and disability, affecting a patient’s quality of life. Understanding the differences between PS and PMS can help healthcare providers develop better treatment plans, which may include physical therapy, medications, manual therapy techniques, and lifestyle modifications. Ultimately, recognizing and addressing the unique aspects of each condition can lead to more successful management and improved patient outcomes.
Understanding Piriformis Syndrome (PS)

In Piriformis Syndrome (PS), the sciatic nerve becomes compressed or irritated by the piriformis muscle, often due to anatomical variations, trauma, or inflammation. This nerve compression can cause radiating pain along the back of the leg, tingling, numbness, and weakness in the affected limb. The image shows the proximity of the sciatic nerve to the piriformis muscle, highlighting how structural issues can contribute to PS.
In Piriformis Myofascial Syndrome (PMS), the focus is on the piriformis muscle itself. Trigger points within the muscle cause localized pain in the buttock region, which may refer to the lower back, hip, or thigh. Unlike PS, PMS does not involve direct sciatic nerve compression but results from muscular dysfunction and tension.
This visual guide emphasizes the importance of understanding the unique mechanisms of PS and PMS to aid in accurate diagnosis and effective treatment.
Pathophysiology
Piriformis Syndrome (PS) involves irritation or compression of the sciatic nerve by the piriformis muscle, located deep within the buttock region. This compression can occur due to various factors, including anatomical variations where the sciatic nerve passes through or under the piriformis muscle, causing pressure and irritation.
Causes and Contributing Factors
Several factors contribute to the development of Piriformis Syndrome:
- Anatomical Variations: Abnormalities in the course of the sciatic nerve or piriformis muscle.
- Trauma: Injury to the buttock area from falls, accidents, or direct impact.
- Overuse: Repetitive activities that engage the piriformis muscle, such as running or cycling.
- Muscle Tightness or Spasm: Tightness or spasm of the piriformis muscle due to poor posture, prolonged sitting, or inadequate stretching.
- Inflammation: Conditions causing inflammation around the piriformis muscle or sciatic nerve.
Symptoms
Patients with Piriformis Syndrome may experience:
- Sciatic Pain: Sharp or dull pain that radiates from the buttock down the back of the thigh. Pain may extend into the lower leg and foot along the path of the sciatic nerve.
- Numbness and Tingling: Sensations of numbness, tingling, or pins and needles along the sciatic nerve distribution.
- Muscle Weakness: Weakness in the affected leg, particularly noticeable when walking, climbing stairs, or standing from a seated position.
- Increased Pain with Activity: Symptoms worsen with activities that engage the piriformis muscle, such as prolonged sitting, climbing stairs, or running.
Diagnosis
Diagnosing Piriformis Syndrome typically involves:
- Physical Examination: Assessment of range of motion, muscle strength, and tenderness in the buttock region. Special tests like the FAIR (Flexion, Adduction, Internal Rotation) test may reproduce symptoms.
- Imaging Techniques: MRI or ultrasound may be used to visualize the piriformis muscle and rule out other structural causes of buttock pain.
- Nerve Conduction Studies: Electromyography (EMG) or nerve conduction studies can assess the function and response of the sciatic nerve.
Treatment (Osteopathy)
Osteopathic treatment for Piriformis Syndrome focuses on:
- Manual Therapy: Hands-on techniques to release tension in the piriformis muscle and surrounding tissues, improving muscle flexibility and reducing nerve compression.
- Soft Tissue Techniques: Myofascial release, trigger point therapy, and deep tissue massage to alleviate muscle tightness and pain.
- Joint Mobilization: Gentle movements to restore normal joint function and alleviate secondary muscle tightness.
- Exercise Prescription: Tailored stretching and strengthening exercises to improve piriformis muscle flexibility and overall hip stability.
- Patient Education: Guidance on posture correction, ergonomic adjustments, and home exercises to manage symptoms and prevent recurrence.
Effective management of Piriformis Syndrome through osteopathic care aims to reduce pain, improve mobility, and enhance overall quality of life for patients experiencing sciatic nerve-related symptoms.
Piriformis Myofascial Syndrome (PMS)
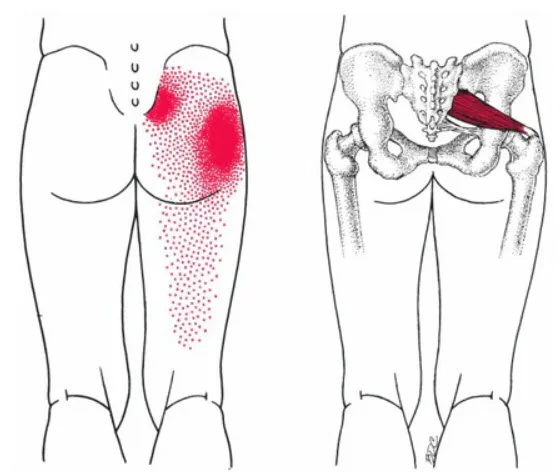
On the left, the red shaded area represents the pain referral pattern commonly associated with Piriformis Myofascial Syndrome (PMS). Trigger points in the piriformis muscle lead to localized pain in the buttock and referred pain extending to the hip, lower back, or thigh. The dotted distribution emphasizes that PMS is primarily a muscular issue, without direct sciatic nerve involvement.
On the right, the anatomical depiction of the piriformis muscle shows its relationship to the sciatic nerve, crucial for understanding Piriformis Syndrome (PS). In PS, the sciatic nerve is compressed or irritated by the piriformis muscle, causing radiating pain along the back of the thigh, often reaching the lower leg. Unlike PMS, PS involves neurological symptoms such as tingling, numbness, and weakness.
This visual comparison underscores the need for accurate diagnosis to address the distinct mechanisms and presentations of these conditions effectively.
4o
Pathophysiology
Piriformis Myofascial Syndrome (PMS) is characterized by the presence of myofascial trigger points within the piriformis muscle. These trigger points are hyperirritable spots in the fascia surrounding muscle tissue, causing local and referred pain patterns. Unlike Piriformis Syndrome, which involves sciatic nerve compression, PMS is primarily a muscular disorder focused on the dysfunction of the piriformis muscle itself.
Causes and Contributing Factors
Several factors can contribute to the development of Piriformis Myofascial Syndrome:
- Muscle Overuse: Repetitive activities, such as running or cycling, that strain the piriformis muscle.
- Poor Posture: Prolonged sitting, improper ergonomics, or imbalanced muscle use can lead to chronic muscle tension and the formation of trigger points.
- Injury: Acute trauma or microtrauma to the buttock area can initiate the formation of myofascial trigger points.
- Muscle Imbalances: Weakness in surrounding muscles or tightness in opposing muscle groups can increase the strain on the piriformis muscle.
- Stress: Emotional and physical stress can contribute to muscle tension and the development of trigger points.
Symptoms
Patients with Piriformis Myofascial Syndrome typically experience:
- Localized Buttock Pain: Deep, aching pain localized in the buttock region, often exacerbated by sitting or direct pressure.
- Referred Pain: Pain that radiates from the buttock to other areas, such as the lower back, hip, or thigh, following specific referral patterns from the trigger points.
- Trigger Points: Palpable knots or taut bands within the piriformis muscle that elicit pain when pressed.
- Limited Range of Motion: Stiffness and decreased flexibility in the hip and buttock area, affecting movement and activities.
Diagnosis
Diagnosing Piriformis Myofascial Syndrome involves:
- Physical Examination: Assessment of the buttock area to identify trigger points and evaluate muscle tension. Manual palpation of the piriformis muscle to locate hyperirritable spots.
- Pain Mapping: Identifying pain referral patterns from the trigger points to differentiate from other causes of buttock pain.
- Exclusion of Other Conditions: Ruling out other potential causes of buttock and leg pain, such as lumbar spine disorders, hip joint pathologies, or neurological conditions.
Treatment
Effective treatment for Piriformis Myofascial Syndrome focuses on relieving muscle tension and addressing the underlying causes:
- Myofascial Release Techniques: Manual therapy, including myofascial release, trigger point therapy, and deep tissue massage, to alleviate tension in the piriformis muscle and reduce pain.
- Physical Therapy: Customized stretching and strengthening exercises to improve muscle flexibility, correct imbalances, and enhance overall hip stability. Techniques such as active release therapy (ART) may also be utilized.
- Dry Needling: Insertion of fine needles into trigger points to release muscle tension and improve blood flow to the affected area, facilitating healing.
- Heat Therapy: Application of heat to the buttock region to relax the piriformis muscle, reduce pain, and improve flexibility. This can include hot packs, warm baths, or infrared therapy.
Combining these treatment approaches can effectively manage and alleviate the symptoms of Piriformis Myofascial Syndrome, improving function and quality of life for patients. Accurate diagnosis and a tailored treatment plan are essential for addressing the unique aspects of this condition.
Comparative Analysis: PS vs. PMS
Key Differences in Pathophysiology
Piriformis Syndrome (PS)
- Sciatic Nerve Compression: PS is primarily a neuromuscular disorder where the piriformis muscle irritates or compresses the sciatic nerve.
- Nerve Involvement: The condition directly affects the sciatic nerve, leading to neurological symptoms such as pain, numbness, and tingling along the nerve’s pathway.
Piriformis Myofascial Syndrome (PMS)
- Myofascial Trigger Points: PMS is characterized by the presence of myofascial trigger points within the piriformis muscle.
- Muscular Dysfunction: The primary issue is muscle tension and trigger points, not nerve compression. The pain is due to hyperirritable spots within the muscle fascia.
Distinct Symptom Profiles
Piriformis Syndrome (PS)
- Sciatic Pain: Sharp or dull pain radiating from the buttock down the back of the thigh, and possibly into the lower leg and foot.
- Numbness and Tingling: Sensations of numbness or tingling in the buttock, thigh, or leg.
- Muscle Weakness: Weakness in the affected leg, particularly noticeable when performing certain movements like walking or climbing stairs.
- Increased Pain with Activity: Symptoms worsen with activities that engage the piriformis muscle, such as prolonged sitting or climbing stairs.
Piriformis Myofascial Syndrome (PMS)
- Localized Buttock Pain: Deep, aching pain localized in the buttock region, often worsened by prolonged sitting or direct pressure.
- Referred Pain: Pain that radiates from the buttock to other areas, such as the lower back, hip, or thigh, following specific referral patterns from the trigger points.
- Trigger Points: Palpable knots or taut bands within the piriformis muscle that elicit pain when pressed.
- Limited Range of Motion: Stiffness and decreased flexibility in the hip and buttock area, affecting movement and activities.
Diagnostic Approaches
Piriformis Syndrome (PS)
- Physical Examination: Includes tests like the FAIR (Flexion, Adduction, Internal Rotation) test to reproduce symptoms.
- Imaging Techniques: MRI or ultrasound may be used to visualize the piriformis muscle and rule out other structural causes of buttock pain.
- Nerve Conduction Studies: Electromyography (EMG) or nerve conduction studies can assess the function and response of the sciatic nerve.
Piriformis Myofascial Syndrome (PMS)
- Physical Examination: Identification of trigger points in the piriformis muscle. Pain response to pressure on these points confirms the diagnosis.
- Pain Mapping: Understanding the referred pain patterns from the trigger points.
- Exclusion of Other Conditions: Rule out other causes of buttock pain, such as lumbar radiculopathy or hip joint disorders.
Treatment Strategies
Piriformis Syndrome (PS):
- Physical Therapy: Stretching and strengthening exercises for the piriformis muscle.
- Medications: Anti-inflammatory drugs and muscle relaxants.
- Injections: Corticosteroid or botulinum toxin injections to reduce inflammation and muscle spasm.
- Surgery: Rarely required, but may be considered in severe cases.
- Osteopathic Treatment: Manual therapy, soft tissue techniques, joint mobilization, exercise prescription, and patient education on posture and ergonomics.
Piriformis Myofascial Syndrome (PMS):
- Myofascial Release Techniques: Manual therapy, including myofascial release, trigger point therapy, and deep tissue massage, to alleviate tension in the piriformis muscle and reduce pain.
- Physical Therapy: Customized stretching and strengthening exercises to improve muscle flexibility, correct imbalances, and enhance overall hip stability.
- Dry Needling: Insertion of fine needles into trigger points to release muscle tension and improve blood flow to the affected area, facilitating healing.
- Heat Therapy: Application of heat to the buttock region to relax the piriformis muscle, reduce pain, and improve flexibility.
Comparative Analysis: Conclusion
Key Differences in Pathophysiology
Piriformis Syndrome (PS) and Piriformis Myofascial Syndrome (PMS) are two conditions that involve the piriformis muscle but differ fundamentally in their underlying mechanisms.
Piriformis Syndrome (PS):
PS is primarily a neuromuscular disorder caused by the compression or irritation of the sciatic nerve by the piriformis muscle. This compression often results from anatomical variations, such as the sciatic nerve passing through or underneath the piriformis muscle, or from external factors like trauma or inflammation. The hallmark of PS is sciatic nerve involvement, which leads to radiating pain along the nerve’s pathway. PS represents a direct interaction between muscle and nerve, with nerve compression being the primary issue.
Piriformis Myofascial Syndrome (PMS):
In contrast, PMS is a musculoskeletal condition characterized by the presence of myofascial trigger points within the piriformis muscle. These hyperirritable spots within the muscle fascia cause localized and referred pain without involving the sciatic nerve. PMS stems from muscle dysfunction rather than nerve compression. Contributing factors include muscle overuse, poor posture, stress, or trauma, leading to chronic tension and restricted blood flow in the muscle tissue.
Distinct Symptom Profiles
The symptomatology of PS and PMS differs due to their distinct pathophysiologies.
Piriformis Syndrome (PS):
- Sciatic Pain: Pain radiates from the buttock down the back of the thigh, often extending to the lower leg and foot.
- Neurological Symptoms: Numbness, tingling, or pins-and-needles sensations along the sciatic nerve pathway are common.
- Muscle Weakness: Weakness in the affected leg, particularly during activities like walking or climbing stairs, is often present.
- Activity-Dependent Pain: Symptoms worsen with activities that engage the piriformis muscle, such as sitting, climbing stairs, or deep squats.
Piriformis Myofascial Syndrome (PMS):
- Localized Buttock Pain: Deep, aching pain is confined to the buttock region and exacerbated by prolonged sitting or pressure on the area.
- Referred Pain: Pain may spread to the lower back, hip, or thigh, following specific trigger point referral patterns.
- Trigger Points: Palpable knots or taut bands within the piriformis muscle that elicit pain when pressed.
- Limited Range of Motion: Stiffness and reduced flexibility in the hip and buttock area, affecting movement and daily activities.
Diagnostic Approaches
Accurate diagnosis is crucial to differentiate between PS and PMS, as misdiagnosis can lead to ineffective treatments.
Piriformis Syndrome (PS):
- Physical Examination: Tests like the FAIR (Flexion, Adduction, Internal Rotation) test are performed to reproduce symptoms. Tenderness in the buttock along with sciatic nerve pain supports the diagnosis.
- Imaging Techniques: MRI or ultrasound is often used to visualize the piriformis muscle and rule out other causes of sciatic pain, such as herniated discs or lumbar radiculopathy.
- Nerve Conduction Studies: Electromyography (EMG) or nerve conduction studies can assess sciatic nerve function and confirm nerve involvement.
Piriformis Myofascial Syndrome (PMS):
- Manual Palpation: Identification of myofascial trigger points in the piriformis muscle through palpation. Pain referral patterns and sensitivity to pressure are key diagnostic criteria.
- Pain Mapping: Referral pain patterns originating from trigger points help differentiate PMS from other conditions like lumbar radiculopathy.
- Exclusion of Other Conditions: Ruling out structural or neurological causes of pain is essential for an accurate diagnosis.
Treatment Strategies
The treatment approaches for PS and PMS differ significantly due to their distinct underlying causes.
Piriformis Syndrome (PS):
- Physical Therapy: Focuses on stretching and strengthening the piriformis muscle to relieve nerve compression.
- Medications: Anti-inflammatory drugs and muscle relaxants are commonly prescribed to reduce inflammation and spasms.
- Injections: Corticosteroid or botulinum toxin injections may be used to reduce inflammation and muscle tension.
- Surgery: In rare, severe cases, surgical intervention may be required to release the sciatic nerve from compression.
- Osteopathic Treatment: Manual therapy, including joint mobilization, muscle energy techniques, and soft tissue release, is employed to alleviate nerve compression and restore mobility.
Piriformis Myofascial Syndrome (PMS):
- Myofascial Release Techniques: Manual therapy to release tension in the piriformis muscle and deactivate trigger points.
- Dry Needling: The insertion of fine needles into trigger points helps relieve tension and improve blood flow.
- Stretching and Strengthening Exercises: Customized exercise programs improve flexibility and correct muscle imbalances to reduce strain on the piriformis muscle.
- Heat Therapy: Heat application relaxes the piriformis muscle, reduces pain, and enhances blood flow.
- Stress Management: Addressing physical and emotional stress can help prevent recurrence of trigger points.
Conclusion
Piriformis Syndrome (PS) and Piriformis Myofascial Syndrome (PMS) are distinct conditions that share involvement of the piriformis muscle but differ significantly in their underlying mechanisms, symptomatology, and treatment approaches. Understanding these differences is vital for accurate diagnosis and effective management.
PS is primarily a neuromuscular disorder involving irritation or compression of the sciatic nerve by the piriformis muscle. This results in symptoms such as sciatic pain radiating from the buttock to the lower leg, numbness, tingling, and sometimes muscle weakness. PS is commonly triggered by anatomical variations, trauma, or overuse of the piriformis muscle. Diagnosis relies on physical examination, imaging, and nerve conduction studies. Treatments focus on alleviating nerve compression through physical therapy, medications, injections, and in severe cases, surgery. Osteopathic interventions emphasize manual therapy, muscle release techniques, and patient education to improve mobility and relieve nerve irritation.
In contrast, PMS is a musculoskeletal condition characterized by myofascial trigger points within the piriformis muscle. These trigger points cause localized pain, referred pain to areas like the lower back, hip, and thigh, and limited range of motion. PMS is typically associated with muscle overuse, poor posture, stress, or trauma. Unlike PS, PMS does not involve sciatic nerve compression but instead centers on muscular dysfunction. Diagnosis is based on identifying trigger points and pain referral patterns, often excluding other conditions. Treatment focuses on releasing muscle tension and addressing trigger points through techniques like myofascial release, dry needling, stretching, and heat therapy.
Accurate differentiation between PS and PMS is critical because their management requires distinct approaches. Misdiagnosis can result in ineffective treatments, prolonged discomfort, and decreased quality of life for patients. For example, interventions targeting nerve compression in PS may not address the underlying muscular dysfunction of PMS, and vice versa.
References
- Boyajian-O’Neill, L. A., McClain, R. L., Coleman, M. K., & Thomas, P. P. (2008). Piriformis Syndrome: Diagnosis and Treatment. Journal of the American Osteopathic Association, 108(11), 657-664.
- Hopayian, K., Song, F., Riera, R., & Sambandan, S. (2010). The Clinical Features of the Piriformis Syndrome: A Systematic Review. European Spine Journal, 19(12), 2095-2109.
- Filler, A. G., Haynes, J., Jordan, S. E., Prager, J., Villablanca, J. P., Farahani, K., & Tsuruda, J. S. (2005). Sciatica of Nerve Origin: MRI Imaging of Piriformis Muscle and the Sciatic Nerve. Neurosurgery, 56(6), 1014-1024.
- Cohen, S. P., & Raja, S. N. (2007). Pathogenesis, Diagnosis, and Management of Piriformis Syndrome. Anesthesiology, 107(6), 114-129.
- Stecco, C., Macchi, V., Porzionato, A., Duparc, F., De Caro, R., & Delmas, V. (2010). Anatomical Basis of Piriformis Syndrome: A Review. Surgical and Radiologic Anatomy, 32(4), 335-340.
- Simons, D. G., Travell, J. G., & Simons, L. S. (1999). Myofascial Pain and Dysfunction: The Trigger Point Manual. Vol. 1. Williams & Wilkins.
- Borg-Stein, J., & Simons, D. G. (2002). Focused Review: Myofascial Pain. Archives of Physical Medicine and Rehabilitation, 83(3), S40-S47.
- Fernández-de-Las-Peñas, C., & Dommerholt, J. (2018). Myofascial Trigger Points: Peripheral and Central Mechanisms. Journal of Manual & Manipulative Therapy, 26(1), 10-18.
- Bron, C., Franssen, J., Wensing, M., & Oostendorp, R. A. B. (2007). Interrater Reliability of Palpation of Myofascial Trigger Points in Three Shoulder Muscles. Journal of Manual & Manipulative Therapy, 15(4), 203-215.
- Shah, J. P., Thaker, N., Heimur, J., Aredo, J. V., Sikdar, S., & Gerber, L. (2015). Myofascial Trigger Points Then and Now: A Historical and Scientific Perspective. PM&R, 7(7), 746-761.
- Fishman, L. M., & Dombi, G. W. (2002). Piriformis Syndrome: Diagnosis, Treatment, and a New Theory About Pathogenesis. Archives of Physical Medicine and Rehabilitation, 83(3), 295-301.
- Probst, D., Stout, A., Hunt, D., & Schnapp, D. (2019). Piriformis Syndrome: A Narrative Review of the Anatomy, Diagnosis, and Treatment. Orthopedic Clinics of North America, 50(4), 487-493.
- Papadopoulos, E. C., & Khan, S. N. (2004). Piriformis Syndrome and Low Back Pain: A New Classification and Review of the Literature. Orthopedic Clinics of North America, 35(1), 65-71.
- Nabhan, A., Ahlhelm, F., Kelm, J., Pape, D., & Rickert, M. (2007). The Value of MR Imaging in Diagnosing Extraspinal Sciatica of the Piriformis Syndrome: A Case Report and Review of the Literature. The Spine Journal, 7(5), 552-555.
- Miller, T. A., White, K. P., Ross, D. C., & Cosio-Lima, L. M. (2012). Management of Chronic Piriformis Syndrome with Ultrasound-Guided Botulinum Toxin Type A Injection: A Case Series. American Journal of Physical Medicine & Rehabilitation, 91(12), 1140-1145.
- Phillips, S. A., & Anloague, P. A. (2014). Differentiating Piriformis Syndrome from Other Causes of Posterior Hip Pain. Current Sports Medicine Reports, 13(5), 354-358.
- Rodrigues, L. M. R., & Takeda, F. R. (2019). Piriformis Syndrome in Athletes: Diagnostic Criteria and Management. International Journal of Sports Physical Therapy, 14(4), 501-510.
- Hopayian, K., Song, F., Riera, R., & Sambandan, S. (2010). The Clinical Features of the Piriformis Syndrome: A Systematic Review. European Spine Journal, 19(12), 2095-2109.
- Ferrell, W. R., & Donnelly, R. (2013). Myofascial Pain: The Fibromyalgia Syndrome. British Medical Bulletin, 69(1), 123-136.
- Gerwin, R. D. (2014). Myofascial Pain Syndrome and Fibromyalgia: Trigger Points and Tender Points. Current Pain and Headache Reports, 14(5), 468-475














