Introduction
Breastfeeding is a crucial stage in an infant’s development, providing a multitude of benefits for both physical and mental health. However, it is essential to pay close attention to certain key nutrients to avoid possible deficiencies in mother and baby.
One nutrient of particular concern is vitamin D. Although breast milk is a valuable source of nutrients, it does not provide enough vitamin D to meet infants’ needs. Recommendations from the American Academy of Pediatrics emphasize the need for a daily supplement of 400 IU of vitamin D for breastfed infants, beginning in the first days of life. This is intended to prevent the risk of rickets, a potentially serious condition.
Another major concern is iron, a vital element for hemoglobin production and neurological development. Breast milk is relatively low in iron, especially after the first months of life. Thus, exclusively breastfed infants are generally encouraged to take an iron supplement starting at 4 months of age to support their growth. Parents should consult their healthcare professional to determine the appropriate dose based on the child’s body weight.
Vitamin B12 is also worth considering, especially for mothers following a strict vegetarian or vegan diet. Although vitamin B12 is usually transferred through breast milk, deficiencies can occur if the mother does not consume enough animal sources. In such cases, supplements may be necessary to avoid potential complications in the infant.
Vitamin K, essential for blood clotting, deserves special attention. Breast milk is naturally low in vitamin K, and the American Academy of Pediatrics recommends an intramuscular injection of vitamin K1 soon after birth to prevent the risk of bleeding. This injection is crucial for newborns, whether they are breastfed or bottle fed.
Finally, iodine is a crucial mineral for the neurological development of infants. Breastfeeding women should ensure adequate iodine intake, as a deficiency can lead to cognitive impairment in the baby. Food sources rich in iodine, such as dairy products and iodized salt, may be essential in meeting nutritional needs.
Iodine
Iodine deficiency during breastfeeding can have significant implications for maternal and infant health. Iodine is an essential element in the production of the thyroid hormones thyroxine (T4) and triiodothyronine (T3), playing a crucial role in infant neurodevelopment and fetal growth during pregnancy.
Breastfeeding women, especially those with certain risk factors, may be more prone to iodine deficiency. Recommendations from the American Thyroid Association and the American Academy of Pediatrics emphasize the importance of all women of childbearing age consuming 150 micrograms of iodine per day, either through their diet or a vitamin supplement. .
Groups at risk for iodine deficiency during breastfeeding include women who do not consume dairy products, those who smoke, those who do not use iodized salt, and those who consume foods rich in goitrogens, such as Brussels sprouts, kale, cauliflower, radishes and broccoli. These foods can interfere with the production of thyroid hormones, increasing the risk of iodine deficiency.
Although breast milk naturally contains iodine, the concentration can vary depending on maternal iodine levels. If a pregnant or breastfeeding woman is deficient in iodine, the infant may be exposed to a risk of deficiency, which can lead to cognitive and psychomotor disorders.
The Recommended Dietary Allowance (RDA) recommendations for iodine during breastfeeding are 290 micrograms per day, emphasizing the importance of adequate intake to support optimal growth and development of the infant.
To address potential deficiencies, the American Thyroid Association and the American Academy of Pediatrics recommend that pregnant or breastfeeding women take a daily multivitamin or prenatal supplement containing 150 micrograms of iodine. It is important to note that not all supplements necessarily contain this amount, and women should check the nutrition label or consult their healthcare professional to ensure sufficient intake.
Who is at risk of iodine deficiency while breastfeeding?
Several groups of women may be at risk of iodine deficiency while breastfeeding. The main risk factors include:
- Women who do not consume dairy products: Dairy products, such as milk, yogurt and cheese, are important sources of iodine. Women who avoid these foods may have reduced iodine intake.
- Women who smoke cigarettes: Smoking may increase the risk of iodine deficiency because cigarette smoke may contain substances that interfere with iodine absorption.
- Women who do not use iodized salt: Iodized salt is a common source of iodine in the diet. If a woman does not use iodized salt in her cooking, she may have insufficient iodine intake.
- Women who eat foods containing goitrogens: Goitrogens are substances found in certain foods that can interfere with the production of thyroid hormones. Cruciferous vegetables such as Brussels sprouts, kale, cauliflower, radishes, and broccoli are examples of foods high in goitrogens.
- Women living in iodine-deficient regions: Geographic regions can influence the iodine content of soils and, therefore, the iodine content of foods produced in those regions. Women living in areas with low iodine soil may be at increased risk of deficiency
Do infants get enough iodine from breast milk?
Usually. The Recommended Dietary Allowance (RDA) (the average amount of a vitamin or mineral that meets the daily nutritional needs of almost all healthy people) of iodine is higher for pregnant or breastfeeding women so to support healthy fetal or infant growth and neurological development. Although breast milk contains iodine, concentrations can vary depending on maternal iodine levels. If a pregnant or breastfeeding woman is deficient in iodine, the fetus or infant may be at risk of deficiency and have cognitive and psychomotor disorders.
The Institute of Medicine has set the RDA for iodine:
Period Iodine RDA
Before pregnancy 150 mcg per day
During pregnancy 220 mcg per day
Breastfeeding 290 mcg per day
Because a pregnant or breastfeeding woman’s diet may not contain enough iodine to meet the RDA, the American Thyroid AssociationExternal and the American Academy of PediatricsExternal recommend that pregnant or breastfeeding women take a daily daily multivitamin or prenatal supplement containing 150 mcg of iodine.
Not all multivitamin and prenatal supplements contain 150 mcg of iodine; Therefore, all women should check the nutrition label or talk to their healthcare provider if their multivitamin supplement or prenatal vitamin contains enough iodine.
Vitamin D
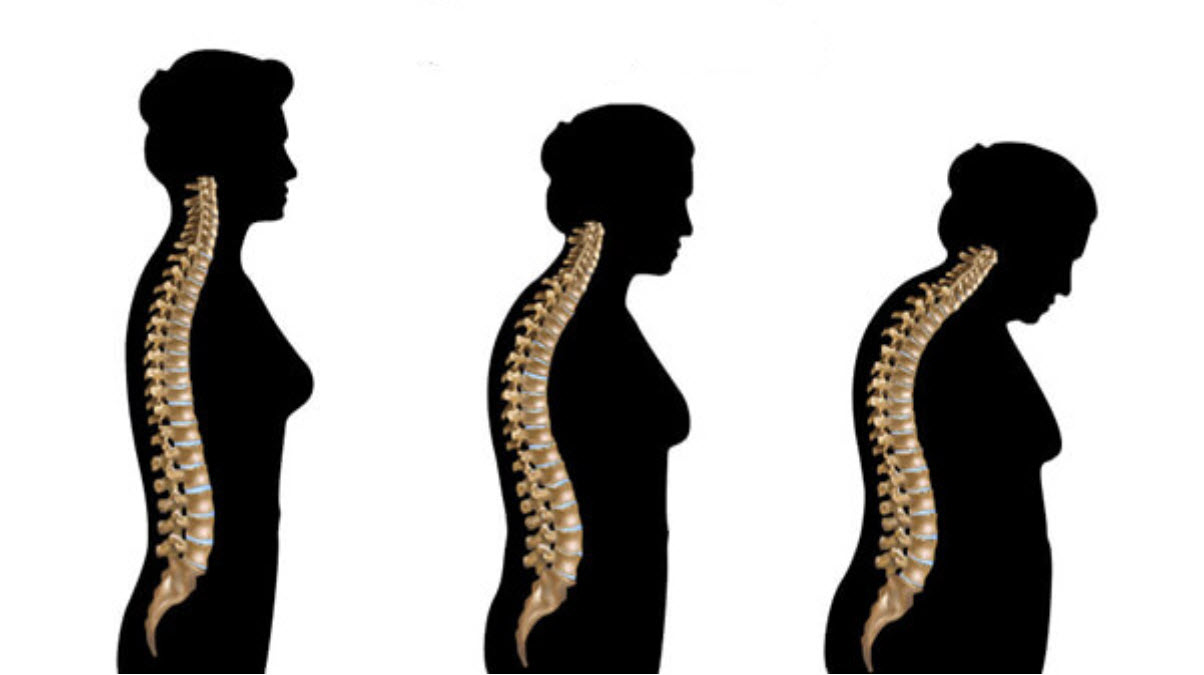
Vitamin D deficiency during breastfeeding can have important implications for maternal and infant health. Vitamin D plays a crucial role in bone development, immune health and prevention of rickets in infants. Although breast milk is a valuable source of many nutrients, it does not provide enough vitamin D to meet the needs of infants, especially beyond the first few months of life.
Recommendations from the American Academy of Pediatrics emphasize the importance of a daily supplement of 400 IU of vitamin D for breastfed infants, beginning in the first days of life. This supplementation is essential to prevent rickets, a condition characterized by weak or misshapen bones, which can lead to serious complications.
Breastfed infants are particularly at risk for vitamin D deficiency because they rely on their diet, and breast milk alone does not provide an adequate amount of this vitamin. The need for vitamin D supplementation persists until the infant consumes sufficient vitamin D-fortified formula or is adequately exposed to sunlight.
Vitamin D deficiency can also affect breastfeeding mothers, especially if they have limited sun exposure or a diet lacking natural sources of vitamin D, such as oily fish, eggs and mushrooms. Women who follow strict vegan diets may also be at risk for vitamin D deficiency, as most dietary sources of this vitamin come from animal sources.
It is essential that breastfeeding mothers and their infants receive adequate amounts of vitamin D to support their bone, immune and overall health. In addition to supplementation, moderate sun exposure is a natural source of vitamin D. However, it is important to take precautions to avoid risks associated with excessive sun exposure, such as sunburn.
Do infants get enough vitamin D from breast milk?
No. Breast milk alone does not provide infants with an adequate amount of vitamin D, even if mothers take vitamins containing vitamin D. Soon after birth, most infants will need an additional source of vitamin D. .
To avoid developing a vitamin D deficiency, the American Academy of Pediatrics recommends that breastfed and partially breastfed infants get a supplement of 400 IU per day of vitamin D starting in the first days of life. Vitamin D supplementation should be continued unless the infant is weaned off at least 1 liter per day (approximately 1 liter per day) of vitamin D-fortified formula. Any infant who receives <1 liter or 1 liter of formula per day day needs another way to get 400 IU/day of vitamin D, for example through vitamin D supplementation.
Why are infants at risk for vitamin D deficiency?
The risk of vitamin D deficiency increases when sun exposure is limited or when an infant does not consume an adequate amount of vitamin D. Although reducing sun exposure is important for preventing cancer, it decreases also how much vitamin D a person can make from sunlight.
The iron
Iron deficiency during breastfeeding can have significant implications for maternal and infant health. Iron is a crucial element for the production of hemoglobin, carrying oxygen to all parts of the body. Additionally, it supports appropriate neurodevelopment during early childhood.
Breast milk naturally contains little iron, and although most newborns have adequate iron stores for the first few months of life, these stores can begin to become depleted. This is why the American Academy of Pediatrics recommends that exclusively breastfed infants begin receiving an iron supplement starting at 4 months of age. The recommended dose is 1 milligram of iron for every kilogram of the child’s body weight.
It is essential to note that when infants receive both breast milk and formula, their supplemental iron needs depend on the amount of each type of milk consumed. A discussion with the child’s healthcare provider can help determine if an infant is getting enough iron from their diet.
During breastfeeding, mothers may also be at risk of iron deficiency, particularly if they lost a lot of blood during childbirth. Pregnant and lactating women have increased iron requirements to support fetal growth and breast milk production. Food sources rich in iron include red meat, poultry, fish, legumes, fortified cereals and green leafy vegetables.
Maternal iron deficiency can lead to persistent fatigue, weakness, and decreased ability to meet the energy demands of breastfeeding. This highlights the importance for breastfeeding women to maintain a balanced diet and, if necessary, take iron supplements under the supervision of a healthcare professional.
It should be noted that some women, due to factors such as gastrointestinal issues, may have difficulty absorbing iron from foods or supplements. In such cases, personalized adjustments and regular medical monitoring may be necessary to address the iron deficiency.
Do infants get enough iron from breast milk?
Most newborns have enough iron stored in their body for at least the first 4 months of life. Breast milk contains very little iron; therefore, the American Academy of PediatricsExternal recommends that infants who receive only breast milk (exclusively breastfed) will need an iron supplement each day at a dose of 1 milligram of iron for each kilogram of body weight; this iron supplement should start at 4 months of age.
When infants receive both breast milk and formula, their need for additional iron will depend on the amount of breast milk and the amount of formula they consume. Parents should ask their child’s healthcare provider if their child is getting enough iron.
If an infant is only receiving iron-fortified infant formula (during the period before complementary foods are given), additional iron supplementation is not necessary.
At approximately 6 months of age, an infant’s iron needs can be met by introducing iron-rich foods, iron-fortified cereals, or iron supplement drops.
Vitamin B12
Vitamin B12 deficiency during breastfeeding can have significant consequences on the health of the mother and infant. Vitamin B12 is essential for brain development and the production of healthy red blood cells in infants. Untreated deficiencies can lead to permanent brain damage in infants, highlighting the importance of special vigilance during breastfeeding.
Infants depend on vitamin B12 for their growth and neurological development. Breast milk is a natural source of vitamin B12, transferred from the placenta to the fetus during pregnancy and continuing to be supplied by breast milk after birth. However, the concentration of vitamin B12 in breast milk largely depends on the mother’s diet.
Women who follow a strict vegan diet, excluding animal products, may be particularly at risk of vitamin B12 deficiency. This vitamin is mainly found in meat, fish, dairy products and eggs. Breastfeeding mothers maintaining a vegan diet should be aware of their vitamin B12 intake and may require supplementation under the supervision of a healthcare professional.
Infants who only receive breast milk from mothers who are deficient in vitamin B12 may also be at risk of deficiency. In such cases, it is crucial for nursing mothers to consult their health care provider to determine if they need a vitamin B12 supplement and how much is appropriate.
Women who have had a poorly absorbent bariatric procedure, have pernicious anemia (low red blood cell count due to vitamin B12 deficiency), or have certain gastrointestinal disorders may also be at risk for vitamin B12 deficiency. Health care providers should monitor these women for nutrient deficiencies, including vitamin B12.
Vitamin B12 deficiency in the mother can lead to symptoms such as fatigue, weakness and neurological disorders. These symptoms can impact the mother’s ability to meet the energy needs of breastfeeding and highlight the importance of regular medical monitoring.
Do infants get enough B12 from breast milk?
Usually. Vitamin B12 is transferred through the placenta to the fetus during pregnancy and through breast milk after birth. Infants who drink breast milk from a mother who consumes sufficient amounts of vitamin B12, or infants who drink infant formula, will receive sufficient vitamin B12. However, if a breastfeeding mother is deficient in vitamin B12, her child may also become deficient.
Vitamin B12 is most commonly found in foods of animal origin; Therefore, infants who only receive breast milk from mothers who do not consume animal products are at greater risk of developing vitamin B12 deficiency soon after birth. Breastfeeding mothers following a strict vegetarian or vegan diet should consult their health care provider about taking a supplement containing the appropriate amount of vitamin B12. Mothers can learn more about the importance of vitamin B12, how much is needed, and foods rich in vitamin B12.
Breastfeeding mothers who have had a poorly absorbent bariatric procedure (such as gastric bypass), who have pernicious anemia (low red blood cell count due to vitamin B12 deficiency), or who have certain gastrointestinal disorders, may not being able to absorb various vitamins and minerals, such as vitamin B12, folic acid (vitamin B9), iron and calcium. Health care providers should monitor these mothers for nutrient deficiencies, including vitamin B12 deficiency.
Vitamin K
Vitamin K deficiency during breastfeeding can have crucial implications for infant health, as this vitamin is essential for blood clotting and preventing excessive bleeding. Babies are born with small stores of vitamin K, and breast milk, although rich in many nutrients, generally does not provide sufficient amounts of vitamin K to meet the child’s needs.
Vitamin K is essential for the synthesis of clotting factors in the liver, and a deficiency can lead to excessive bleeding, endangering the infant’s health. To prevent this, the American Academy of Pediatrics recommends that all newborns, whether breastfed or bottlefed, receive a single intramuscular injection of vitamin K shortly after birth.
Breast milk, even that from mothers who take vitamin K supplements, is naturally low in vitamin K. This highlights the importance of administering vitamin K directly to infants to ensure adequate levels and prevent serious complications related to it. to a deficiency.
Administration of vitamin K is usually performed shortly after birth, often while the mother and newborn are hospitalized. Although an intramuscular injection is the recommended method, an oral dose can be administered after the first breastfeed, but no later than 6 hours after birth. Oral administration alone is not routinely recommended, because vitamin K ingested orally is not as efficiently absorbed as that administered by injection.
Vitamin K is particularly crucial during the infant’s first weeks of life, when the infant’s own production mechanisms are not yet fully developed. Parents should be careful to follow medical recommendations regarding the administration of vitamin K to ensure optimal protection against bleeding in newborns.
It is important to note that adherence to vitamin K supplementation guidelines should not be neglected, even if some alternative practices are suggested or discussed. Infant safety should remain the priority, and parents are encouraged to discuss any wishes or concerns regarding vitamin K with their health care providers.
Do infants get enough vitamin K from breast milk?
No. Breast milk is low in vitamin K. Breast milk from mothers who take vitamin K supplements is also low in vitamin K.
The American Academy of Pediatrics recommends that all newborns, whether breastfed or formula-fed, receive a single intramuscular injection of vitamin K1 (phytonadione) at a dose of 0.5 to 1.0 milligrams a little. time after birth (this is usually given during birth hospitalization).
A vitamin K injection can be given after the first breastfeed, but no later than 6 hours. An oral dose of vitamin K is not recommended. Oral vitamin K is not systematically absorbed from the stomach and intestines, and it does not provide adequate amounts for the breastfed infant. Infants who receive the vitamin K vaccine do not need additional supplementation.
A vitamin K injection given at birth is the best way to prevent low amounts of vitamin K and VKDB in infants.
Are there any others?
Besides iodine, vitamin D, iron, vitamin B12 and vitamin K, other nutrients can also be considered when breastfeeding. It is important to ensure a balanced diet to meet the nutritional needs of the mother and infant. Here are some other things that can be considered:
- Calcium: Necessary for the development of bones and teeth, as well as blood clotting. Food sources rich in calcium include dairy products, leafy green vegetables, nuts and seeds.
- Omega-3 fatty acids: Essential for brain and vision development. Oily fish, nuts and flax seeds are good sources of omega-3 fatty acids.
- Protein: Crucial for growth and development. Sources of protein include meat, fish, eggs, dairy, legumes, and nuts.
- Vitamin A: Important for vision, cell growth, and the immune system. Carrots, sweet potatoes, spinach and apricots are rich in vitamin A.
- Vitamin C: Promotes healthy skin, strengthens the immune system. Citrus fruits, strawberries, kiwis and peppers are good sources of vitamin C.
- Zinc: Contributes to normal growth and development. Meats, seafood, dairy products and legumes are sources of zinc.
- Fiber: Essential for digestive health. Whole grains, fruits, vegetables and legumes are rich in fiber.
- Vitamin E: Antioxidant important for cellular health. Nuts, seeds, vegetable oils and green leafy vegetables are sources of vitamin E.
It is recommended to maintain a varied and balanced diet to ensure adequate nutrient intake during breastfeeding. If you have specific concerns, it is always a good idea to consult a healthcare professional or nutritionist for personalized advice.