Introduction
Understanding the Crucial Role of Vastus Medialis Obliquus (VMO) Strength in Knee Health
The human knee, a complex joint crucial for mobility and stability, is supported by a network of muscles, tendons, and ligaments. Among these, the Vastus Medialis Obliquus (VMO) stands out as a key player in maintaining knee function and overall lower limb biomechanics.
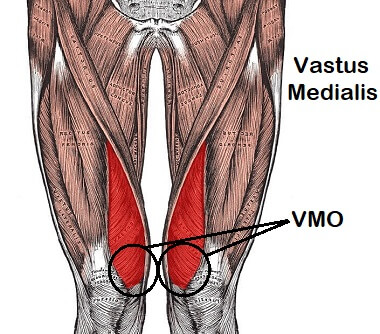
The VMO, a part of the quadriceps muscle group located on the inner side of the thigh, plays a pivotal role in knee stability and patellar tracking. Its unique oblique orientation enables it to exert a stabilizing force on the patella (kneecap), preventing lateral deviation and ensuring proper alignment during movement.
The importance of VMO strength in knee health cannot be overstated. A strong and well-functioning VMO contributes to optimal patellar tracking, reducing the risk of patellofemoral dysfunction and associated knee pain. Conversely, weakness or imbalance in the VMO can lead to various knee issues, including patellar malalignment, instability, and increased susceptibility to injury.
Understanding the significance of VMO strength goes beyond mere muscle function; it directly impacts an individual’s quality of life and ability to engage in physical activities. Whether it’s walking, running, jumping, or performing sports-specific movements, the integrity of the VMO influences knee stability, range of motion, and overall performance.
In this blog post, we delve deeper into the anatomy of the VMO, explore the factors contributing to its weakness, discuss the symptoms and effects of VMO dysfunction, and provide insights into diagnosis, treatment, and prevention strategies. By shedding light on the importance of VMO strength and addressing common misconceptions, we aim to empower individuals to take proactive steps towards maintaining optimal knee health and function.
Anatomy of the Vastus Medialis Obliquus (VMO)
The Vastus Medialis Obliquus (VMO) is a crucial component of the quadriceps muscle group, located on the inner aspect of the thigh. Its anatomy and function are intricately linked to knee stability and proper patellar tracking.
Description and Location:
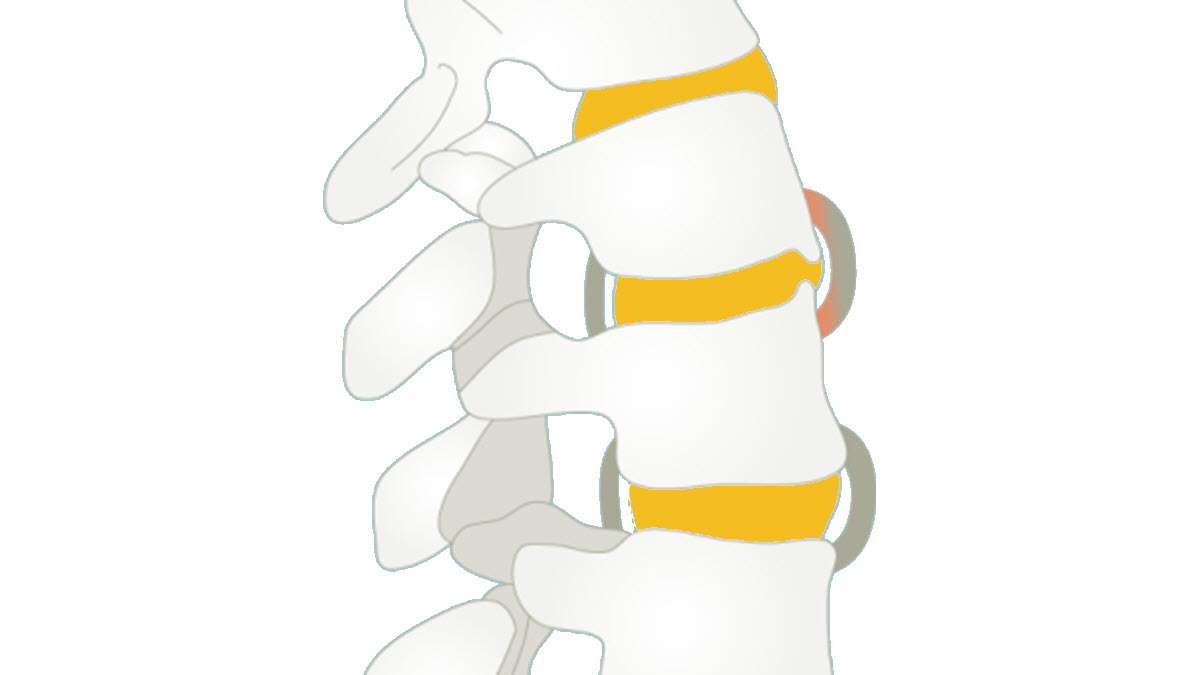
The VMO is one of four muscles that make up the quadriceps femoris muscle group. It originates from the femur’s lower portion, specifically the medial side of the femoral shaft, and extends downward to form the quadriceps tendon. This tendon then attaches to the patella (kneecap) and continues as the patellar ligament, which inserts into the tibial tuberosity.
The VMO has a distinct oblique orientation compared to the other quadriceps muscles, with fibers running at an angle from the inner thigh to the outer knee. This unique alignment allows the VMO to exert a stabilizing force on the patella, aiding in its proper alignment and preventing lateral displacement.
Function in Knee Stability
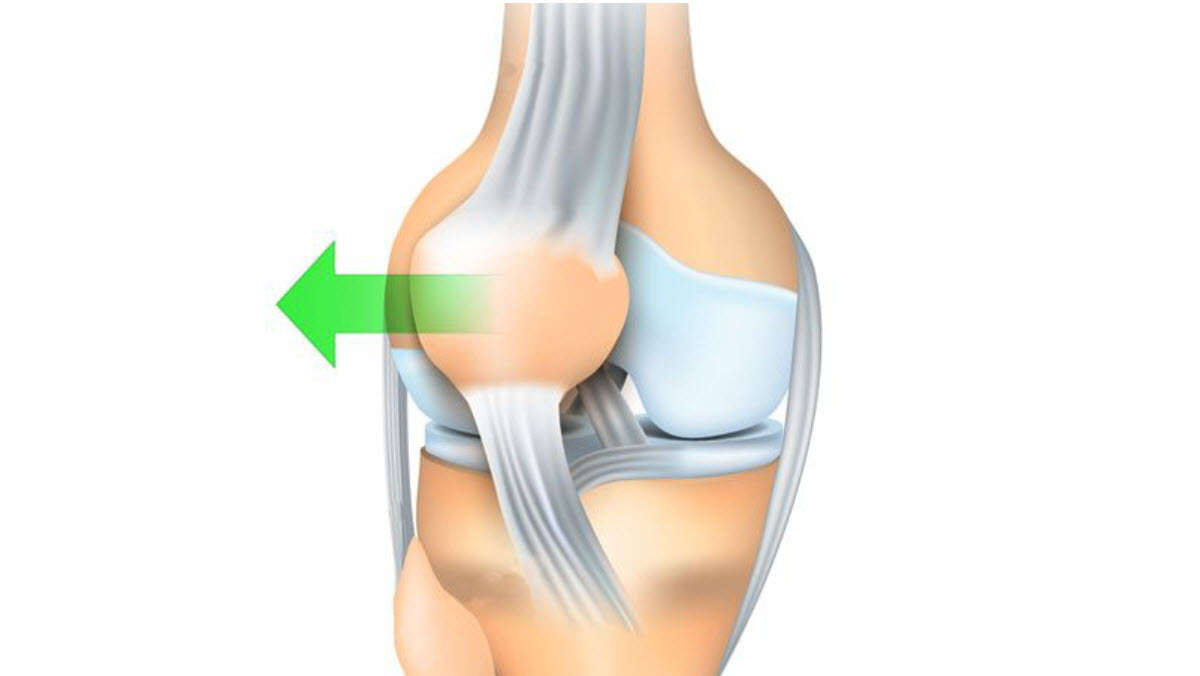
One of the primary functions of the VMO is to provide dynamic stability to the knee joint. During activities such as walking, running, or squatting, the VMO contracts to stabilize the patella within the trochlear groove of the femur. This stabilizing action helps maintain optimal patellofemoral alignment, reducing the risk of patellar maltracking and instability.
Additionally, the VMO plays a crucial role in controlling knee extension and flexion movements. It works in concert with the other quadriceps muscles to generate force during knee extension while also providing fine-tuned control to ensure smooth and stable movement patterns.
Role in Patellar Tracking
Proper patellar tracking refers to the smooth, vertical movement of the patella within the femoral groove during knee flexion and extension. The VMO contributes significantly to this process by exerting a medial pull on the patella, counteracting the lateral pull of the vastus lateralis muscle.
By maintaining an optimal balance between the medial and lateral forces acting on the patella, the VMO helps prevent patellar tilt and displacement. This balanced tracking is essential for distributing joint forces evenly, minimizing stress on the patellar cartilage, and reducing the risk of patellofemoral pain and dysfunction.
Why VMO has the tendency to be weak in some people
The vastus medialis obliquus (VMO) is prone to weakness due to several factors, including:
- Anatomical Variation: The VMO is part of the quadriceps muscle group, located on the inner side of the thigh. However, its attachment to the patella and its specific role in stabilizing the patella during knee movements can vary among individuals. Some people may have a smaller or less developed VMO compared to others, predisposing them to weakness.
- Muscle Imbalance: The VMO works in coordination with the other quadriceps muscles (vastus lateralis, vastus intermedius, and rectus femoris) to extend the knee joint. However, if there’s an imbalance in strength or activation between these muscles, the VMO may become relatively weaker. This imbalance can occur due to factors such as sedentary lifestyle, improper training techniques, or compensatory movements following injuries.
- Poor Neuromuscular Control: Effective muscle activation relies on proper neuromuscular control, which involves the communication between the nervous system and the muscle fibers. Some individuals may have difficulty activating the VMO efficiently during functional movements due to neuromuscular dysfunction or inadequate motor learning. This can lead to weakness and poor stabilization of the patella during dynamic activities.
- Muscle Atrophy: Prolonged disuse, immobilization, or inactivity of the knee joint can lead to muscle atrophy, including the VMO. When the muscle is not regularly engaged through physical activity, it can lose mass and strength over time. This is particularly common in individuals recovering from knee injuries or surgeries who may experience muscle wasting due to restricted movement.
- Injury or Trauma: Direct trauma, overuse injuries, or repetitive stress on the knee joint can damage the VMO muscle fibers, leading to weakness and dysfunction. Injuries such as patellar dislocation, ligament sprains, or muscle strains can impair the VMO’s ability to stabilize the patella and contribute to muscle weakness during rehabilitation.
- Biomechanical Factors: Anatomical variations, such as patellar dysplasia or abnormal lower limb alignment, can affect the biomechanics of the knee joint and alter the distribution of forces across the quadriceps muscles, including the VMO. These biomechanical factors can predispose individuals to VMO weakness and contribute to patellofemoral dysfunction.
- Age-related Changes: With aging, there is a natural decline in muscle mass, strength, and flexibility throughout the body, including the VMO. Age-related changes such as sarcopenia (loss of muscle mass) and decreased muscle fiber recruitment can contribute to VMO weakness and functional limitations, particularly in older adults.
Causes of VMO Weakness
Weakness in the vastus medialis oblique (VMO) muscle, a part of the quadriceps muscle group, can stem from various causes, leading to functional limitations and potentially contributing to knee instability and pain.
One primary cause of VMO weakness is disuse atrophy, often resulting from prolonged periods of inactivity or immobilization following injury or surgery. When the knee joint remains inactive, muscle fibers begin to weaken and lose their strength and mass, including the VMO. Additionally, poor biomechanics and movement patterns during physical activities, such as squatting or lunging, can place excessive stress on other muscles within the quadriceps while neglecting the activation of the VMO, leading to its underdevelopment and weakness over time. Furthermore, muscle imbalances, where certain muscles overpower others, can occur due to factors like repetitive movements or improper training techniques, thereby inhibiting the optimal functioning of the VMO. Inadequate rehabilitation following knee injuries, particularly those involving the patella or anterior cruciate ligament (ACL), can also contribute to VMO weakness, as the muscle may not receive sufficient attention or targeted exercises to regain its strength and stability. Moreover, anatomical factors such as patellar malalignment or structural abnormalities in the knee joint can predispose individuals to VMO weakness by altering the biomechanics of the joint and placing uneven stress on the surrounding muscles. Additionally, neuromuscular conditions or nerve damage affecting the femoral nerve, which innervates the quadriceps muscles including the VMO, can result in diminished muscle activation and control, leading to weakness and functional deficits. Furthermore, age-related changes in muscle mass and strength, commonly referred to as sarcopenia, can affect the VMO along with other muscles in the body, potentially exacerbating weakness and impairing knee function in older individuals. Finally, factors such as poor posture, inadequate warm-up or cool-down routines, and excessive sitting can contribute to muscle stiffness and tightness, limiting the range of motion around the knee joint and compromising the ability of the VMO to function effectively.
List of causes
- Disuse Atrophy: When the VMO is not regularly engaged through physical activity or is immobilized due to injury or surgery, the muscle fibers weaken and lose mass over time, resulting in VMO weakness.
- Poor Biomechanics: Incorrect movement patterns during exercises or daily activities can lead to disproportionate stress on other quadriceps muscles, neglecting proper activation of the VMO and causing it to weaken over time.
- Muscle Imbalances: Repetitive movements or inadequate training techniques may lead to imbalances among the quadriceps muscles, where certain muscles become overdeveloped while others, like the VMO, are underdeveloped and weakened.
- Inadequate Rehabilitation: Following knee injuries, particularly those involving the patella or ACL, if the rehabilitation program does not include specific exercises targeting the VMO, the muscle may not regain its strength and stability, leading to weakness.
- Anatomical Factors: Structural issues such as patellar malalignment or abnormalities in the knee joint can alter the biomechanics of the joint, resulting in uneven stress distribution among the quadriceps muscles, including the VMO, and potentially causing weakness.
- Neuromuscular Conditions: Conditions affecting the nerves responsible for innervating the quadriceps muscles, such as femoral nerve damage, can impair the proper activation and control of the VMO, leading to weakness and functional deficits.
- Age-Related Muscle Changes (Sarcopenia): As individuals age, they may experience a natural decline in muscle mass and strength, including the VMO, which can exacerbate weakness and impair knee function.
- Poor Posture: Incorrect posture can lead to muscle stiffness and tension, affecting the range of motion around the knee joint and compromising the ability of the VMO to function effectively, ultimately resulting in weakness.
- Insufficient Warm-Up or Cool-Down: Skipping warm-up or cool-down routines before and after physical activity can increase the risk of muscle stiffness and limited joint mobility, which can contribute to VMO weakness over time.
- Excessive Sitting: Prolonged periods of sitting can lead to tightness and weakness in the hip flexors and quadriceps muscles, including the VMO, due to reduced activation and blood flow, further contributing to VMO weakness.
- Overtraining: Excessive or repetitive training without adequate rest can lead to fatigue and breakdown of muscle tissue, potentially weakening the VMO over time.
- Nutritional Deficiencies: Inadequate intake of essential nutrients like protein, vitamins, and minerals can impair muscle repair and growth, contributing to VMO weakness.
- Genetic Factors: Some individuals may have genetic predispositions that affect muscle development and function, potentially leading to VMO weakness.
- Hormonal Imbalances: Hormonal fluctuations or imbalances, such as those occurring during puberty, pregnancy, or menopause, can affect muscle strength and function, including the VMO.
- Chronic Illness or Medical Conditions: Certain medical conditions like arthritis, muscular dystrophy, or metabolic disorders can impact muscle health and contribute to VMO weakness.
- Medication Side Effects: Some medications may have side effects that affect muscle function or metabolism, potentially leading to weakness in muscles, including the VMO.
- Poor Foot Mechanics: Issues such as overpronation or flat feet can alter lower limb biomechanics, affecting muscle activation patterns and potentially leading to VMO weakness.
- Joint Hypermobility: Excessive joint laxity or hypermobility can destabilize the knee joint, placing increased stress on the surrounding muscles, including the VMO, and contributing to weakness.
- Psychological Factors: Mental health issues like stress, anxiety, or depression can affect motivation levels and adherence to exercise programs, potentially leading to VMO weakness due to reduced physical activity.
- Environmental Factors: Environmental factors such as temperature extremes, altitude, or pollution can impact exercise performance and recovery, potentially influencing VMO strength and function.
Symptoms and Effects of VMO Weakness
Weakness in the vastus medialis oblique (VMO) muscle can lead to various symptoms and effects, impacting both daily activities and athletic performance. The VMO is a crucial stabilizer of the knee joint and plays a significant role in proper knee alignment and function. When this muscle is weak or dysfunctional, it can result in several noticeable manifestations.
One primary symptom of VMO weakness is knee instability. The VMO helps maintain the patella (kneecap) in its proper position within the femoral groove during movement. When the VMO is weak, the patella may not track correctly, leading to malalignment and instability. This instability can manifest as feelings of the knee giving way or buckling, particularly during weight-bearing activities like walking, climbing stairs, or squatting.
Another common effect of VMO weakness is patellofemoral pain syndrome (PFPS). PFPS is characterized by pain around or behind the patella, often exacerbated by activities that involve bending the knee, such as running, jumping, or sitting for prolonged periods. Weakness in the VMO can contribute to PFPS by altering patellar tracking and increasing stress on the surrounding structures, leading to inflammation and pain.
In addition to knee instability and PFPS, individuals with VMO weakness may experience decreased quadriceps strength. The VMO is one of the four muscles that make up the quadriceps group, and its weakness can result in overall quadriceps imbalances. This imbalance may further exacerbate knee joint dysfunction and compromise functional movements, such as rising from a seated position or performing activities that require knee extension against resistance.
Furthermore, VMO weakness can impact athletic performance, particularly in activities that require lower limb stability and power. Athletes involved in sports like running, jumping, or cutting maneuvers rely heavily on the integrity of the knee joint for optimal performance. Weakness in the VMO can impair knee joint stability, affecting agility, balance, and overall athletic efficiency. Additionally, athletes may be at increased risk of knee injuries, such as patellar dislocation or ligament sprains, due to compromised joint stability.
Addressing VMO weakness typically involves targeted strengthening exercises and rehabilitation protocols. Physiotherapy interventions often focus on activating and strengthening the VMO through specific exercises, such as terminal knee extensions, leg presses, and clamshells. Additionally, techniques like manual therapy, neuromuscular re-education, and proprioceptive training may be utilized to enhance muscle recruitment and improve knee joint stability.
Here are some of the symptoms and effects associated with VMO weakness:
List of symptoms
- Knee Pain: Weakness in the VMO can lead to altered patellar tracking and increased stress on the knee joint, resulting in pain, especially during activities that involve bending or straightening the knee.
- Patellofemoral Instability: The VMO plays a crucial role in stabilizing the patella (kneecap) within the femoral groove. Weakness in this muscle can contribute to patellar maltracking or instability, leading to sensations of the patella “slipping” or “giving way.”
- Decreased Knee Stability: A weakened VMO can compromise the stability of the knee joint, making it more susceptible to injuries such as ligament sprains or meniscal tears due to inadequate support during movements.
- Knee Swelling: Chronic VMO weakness may contribute to increased joint inflammation and fluid accumulation within the knee, leading to swelling, stiffness, and discomfort.
- Reduced Knee Range of Motion: Weakness in the VMO can restrict the normal range of motion of the knee joint, making it challenging to fully bend or straighten the knee, thereby limiting functional activities like walking, squatting, or climbing stairs.
- Altered Gait Mechanics: Compensation patterns may develop to compensate for VMO weakness, leading to abnormal gait mechanics such as limping or favoring one leg over the other, which can further exacerbate musculoskeletal imbalances and increase the risk of injuries.
- Decreased Athletic Performance: Athletes with VMO weakness may experience diminished performance in sports that require dynamic knee movements, such as running, jumping, or cutting, due to reduced power, agility, and control.
- Muscle Imbalances: VMO weakness can contribute to imbalances within the quadriceps muscle group, where other muscles become overactive or dominant, further exacerbating knee joint instability and dysfunction.
- Compromised Functional Activities: Activities that involve weight-bearing through the lower extremities, such as standing up from a seated position, kneeling, or squatting, may become challenging or painful due to VMO weakness.
- Increased Risk of Knee Injuries: Weakness in the VMO can predispose individuals to various knee injuries, including patellar tendonitis, iliotibial band syndrome, or anterior cruciate ligament (ACL) tears, due to altered joint mechanics and compromised stability.
- Knee Crepitus: Weakness in the VMO can contribute to abnormal patellar tracking, leading to crepitus or “crunching” sensations in the knee joint during movement.
- Reduced Endurance: Individuals with VMO weakness may experience fatigue and reduced endurance during activities that require sustained knee muscle contraction, such as prolonged standing or walking.
- Muscle Atrophy: Chronic VMO weakness can result in muscle atrophy or wasting of the quadriceps muscles, including the VMO, leading to visible loss of muscle mass and definition around the knee area.
- Poor Balance: Weakness in the VMO can affect proprioception and balance, making it more challenging to maintain stability during activities that require weight shifting or changes in direction.
- Limited Functional Mobility: Difficulty performing functional movements such as rising from a chair, squatting to pick up objects, or transitioning between sitting and standing positions due to compromised knee stability and strength.
- Impaired Performance in Sports: Athletes with VMO weakness may experience decreased performance in sports requiring rapid changes in direction, jumping, or landing, due to reduced knee stability and power generation.
- Increased Risk of Falls: Weakness in the VMO can contribute to impaired balance and coordination, increasing the risk of falls, particularly in older adults or individuals with existing musculoskeletal issues.
- Joint Degeneration: Chronic VMO weakness may contribute to accelerated wear and tear of the knee joint cartilage, leading to degenerative changes such as osteoarthritis over time.
- Difficulty Descending Stairs: Weakness in the VMO can make descending stairs or inclines challenging, as the muscle is essential for controlling knee flexion and maintaining stability during weight-bearing activities.
- Altered Movement Patterns: Compensation patterns may develop to compensate for VMO weakness, leading to altered movement mechanics and increased stress on other joints and muscles, potentially resulting in secondary musculoskeletal issues.
Diagnosis of VMO Weakness
Here’s an overview of the diagnostic process for VMO weakness:
- Medical History: The healthcare provider will begin by taking a detailed medical history, including any past injuries, surgeries, or medical conditions that may affect the knee or quadriceps muscles.
- Physical Examination: A thorough physical examination will be conducted to assess knee function, range of motion, muscle strength, and stability. Specific tests may be performed to evaluate VMO strength and activation, such as the “quad set” test or manual muscle testing.
- Palpation: The healthcare provider may palpate (feel) the quadriceps muscles, including the VMO, to assess for muscle tone, tenderness, or signs of atrophy.
- Functional Assessment: Functional movement assessments, such as squatting, lunging, or single-leg balance tests, may be performed to evaluate how VMO weakness affects overall knee function and stability during dynamic activities.
- Electromyography (EMG): Electromyography may be used to measure the electrical activity of the quadriceps muscles, including the VMO, during different movements or exercises. This can provide objective data on muscle activation patterns and potential weakness.
- Diagnostic Imaging: In some cases, diagnostic imaging studies such as ultrasound, magnetic resonance imaging (MRI), or X-rays may be ordered to assess for structural abnormalities, patellar malalignment, or other underlying issues contributing to VMO weakness.
- Functional Testing: Functional testing, such as hop tests or agility drills, may be used to assess knee stability and performance during sport-specific movements, especially in athletes or individuals with active lifestyles.
- Comparison with Contralateral Side: Comparing the strength, size, and function of the affected knee and quadriceps muscles with the contralateral (unaffected) side can help identify asymmetries and determine the extent of VMO weakness.
- Clinical Observation: Observing the patient’s gait, movement patterns, and biomechanics during various activities can provide valuable insights into how VMO weakness may be impacting their overall function and mobility.
- Collaboration with Other Specialists: In complex cases or when underlying medical conditions are suspected, collaboration with other healthcare professionals such as orthopedic surgeons, physical therapists, or sports medicine specialists may be necessary to confirm the diagnosis and develop an appropriate treatment plan.
Prevention of VMO Weakness
Preventing VMO weakness involves a combination of lifestyle modifications, proper training techniques, and targeted exercises aimed at maintaining muscle strength and function. Here are some strategies for preventing VMO weakness:
List
- Regular Exercise: Engage in regular physical activity that includes strength training exercises targeting the quadriceps muscles, including the VMO. Exercises such as squats, lunges, leg presses, and step-ups can help maintain muscle strength and prevent weakness.
- Proper Technique: Ensure proper technique and form during exercises to effectively activate the VMO and avoid overloading other quadriceps muscles. Focus on maintaining alignment of the knee and hip joints and avoid excessive forward knee movement during lower body exercises.
- Gradual Progression: Gradually increase the intensity, duration, and resistance of exercise sessions to avoid overloading the muscles and reduce the risk of injury. Incorporate progressive overload principles into your training program to continually challenge the muscles and promote strength gains.
- Balance Training: Include balance and stability exercises in your workout routine to improve proprioception and joint stability, which can help prevent VMO weakness and reduce the risk of falls or injuries.
- Functional Movement Patterns: Incorporate functional movement patterns into your workouts that mimic activities of daily living and sports-specific movements. This can help improve overall muscle coordination and enhance VMO activation during dynamic activities.
- Stretching and Mobility Work: Perform regular stretching and mobility exercises to maintain flexibility in the quadriceps muscles and surrounding tissues. Focus on stretches that target the VMO, such as the seated VMO stretch or quad stretch against a wall.
- Proper Warm-Up and Cool-Down: Always warm up before engaging in exercise to prepare the muscles and joints for activity and reduce the risk of injury. Similarly, cool down after exercise to aid in muscle recovery and flexibility maintenance.
- Cross-Training: Incorporate a variety of exercises and activities into your fitness routine to prevent overuse injuries and ensure balanced muscle development. Include activities such as cycling, swimming, or yoga to complement your strength training program.
- Nutrition and Hydration: Maintain a balanced diet rich in nutrients essential for muscle health, including protein, carbohydrates, vitamins, and minerals. Stay hydrated before, during, and after exercise to support optimal muscle function and recovery.
- Rest and Recovery: Allow adequate time for rest and recovery between exercise sessions to prevent overtraining and promote muscle repair and growth. Listen to your body and adjust your training intensity and volume as needed to avoid burnout or injury.
- Posture Awareness: Maintain good posture throughout the day, especially during prolonged periods of sitting or standing, to reduce unnecessary strain on the knee joint and surrounding muscles, including the VMO.
- Footwear Selection: Choose appropriate footwear with good arch support and cushioning to help maintain proper lower limb alignment and reduce the risk of biomechanical issues that can contribute to VMO weakness.
- Orthotics: Consider using orthotic inserts or shoe modifications if you have foot abnormalities or gait issues that may affect lower limb alignment and contribute to VMO weakness.
- Avoid Overtraining: Avoid excessive training volume or intensity, which can lead to fatigue, overuse injuries, and muscle imbalances that may predispose you to VMO weakness.
- Periodization: Incorporate periodization into your training program by alternating between periods of high-intensity training and recovery to optimize performance, reduce the risk of overtraining, and prevent muscle weakness.
- Injury Prevention Programs: Participate in injury prevention programs tailored to your specific sport or activity, focusing on strengthening the muscles around the knee, including the VMO, and improving movement mechanics to reduce the risk of injuries that can lead to weakness.
- Biomechanical Analysis: Seek guidance from a qualified professional, such as a physical therapist or biomechanics specialist, to assess your movement patterns and identify any biomechanical abnormalities or imbalances that may predispose you to VMO weakness.
- Active Lifestyle: Maintain an active lifestyle that includes a variety of physical activities and movements to promote overall muscle health and prevent muscle weakness associated with sedentary behavior.
- Regular Monitoring: Monitor your progress and adjust your training program as needed based on changes in strength, flexibility, and overall function to prevent stagnation and ensure continued improvement in VMO strength and function.
- Listen to Your Body: Pay attention to any signs of discomfort, pain, or fatigue during exercise, and modify your activities accordingly to avoid exacerbating existing weaknesses or developing new injuries.
Treating VMO weakness
Taping Techniques
Taping techniques are commonly used in sports medicine and rehabilitation to provide support, stability, and pain relief to injured joints and muscles. When it comes to addressing issues related to the vastus medialis obliquus (VMO) and patellar tracking, taping can be a valuable adjunct to therapy. Here are several taping techniques that can be utilized:
- McConnell Taping: This technique aims to correct patellar alignment by applying tape in a specific pattern to facilitate medial patellar glide. The tape is applied from the outer aspect of the knee, across the patella, and towards the inner aspect of the thigh, encouraging the patella to track more centrally within the femoral groove.
- Kinesiology Taping: Kinesiology tape is flexible and elastic, allowing for a range of motion while providing support to the muscles and joints. In the case of VMO weakness, kinesiology tape can be applied in a manner that stimulates and supports the muscle during movement, helping to improve muscle activation and function.
- Patellar Taping: This technique involves applying tape directly over the patella to provide stability and support. By stabilizing the patella, patellar taping can help alleviate pain associated with conditions such as patellofemoral pain syndrome (PFPS) and chondromalacia patella.
- Proximal Stabilization: Taping can also be applied proximally to the knee joint to provide stability and support to the entire lower extremity. Techniques such as the “X” tape or “basket-weave” taping can help improve overall alignment and proprioception, reducing the risk of injury and enhancing performance during activities.
- Dynamic Taping: Dynamic taping involves applying tape in a manner that allows for movement while providing support and stability. This technique is particularly useful for athletes or individuals returning to activity after injury, as it allows for functional movement while still offering support to the muscles and joints.
- Combined Techniques: Depending on the specific needs of the individual and the underlying pathology, a combination of taping techniques may be employed to address VMO weakness and patellar tracking issues comprehensively. This could involve a combination of McConnell taping, kinesiology taping, and patellar taping to target different aspects of the problem.
Stretching and Flexibility Exercises
- Seated VMO Stretch:
- Sit on the floor with your legs extended in front of you.
- Bend your right knee and bring the sole of your right foot to the inside of your left thigh.
- Place your hands behind you for support and gently press your right knee towards the floor.
- Lean forward slightly to deepen the stretch in the VMO.
- Hold for 20-30 seconds and then switch sides.
- Quad Stretch Against Wall:
- Stand facing a wall and place your right hand against the wall for support.
- Bend your left knee and grab your left ankle with your left hand.
- Gently pull your left heel towards your buttocks until you feel a stretch in the front of your thigh, including the VMO.
- Keep your knees close together and your pelvis neutral.
- Hold for 20-30 seconds and then switch sides.
- Lying VMO Stretch:
- Lie on your back with your legs extended.
- Bend your right knee and bring it towards your chest.
- Use your hands to gently pull your right knee towards your opposite shoulder until you feel a stretch in the VMO.
- Keep your hips and lower back flat on the ground.
- Hold for 20-30 seconds and then switch sides.
- Half Kneeling Hip Flexor Stretch:
- Kneel on your right knee with your left foot in front, forming a 90-degree angle at both knees.
- Engage your core and shift your weight forward slightly, feeling a stretch in the front of your right hip and thigh.
- Maintain an upright posture and avoid arching your lower back.
- Hold for 20-30 seconds and then switch sides.
- Standing Hamstring Stretch with Strap:
- Stand with your feet hip-width apart and place a strap or belt around your left foot.
- Extend your left leg in front of you and flex your left foot.
- Keeping your back straight, hinge forward at the hips until you feel a stretch in the back of your left thigh and knee.
- Hold onto the strap with both hands and gently pull towards you to deepen the stretch.
- Hold for 20-30 seconds and then switch sides.
Strength Training
- Terminal Knee Extension (TKE):
- Attach a resistance band to a stable anchor point behind you.
- Loop the other end of the band around your affected knee (the one with VMO weakness).
- Stand facing the anchor point with your feet hip-width apart.
- Slowly extend your knee against the resistance of the band, focusing on engaging the VMO at the end of the movement.
- Control the movement as you return to the starting position.
- Perform 2-3 sets of 10-15 repetitions.
- Mini Squats:
- Stand with your feet hip-width apart and your toes pointed slightly outward.
- Keep your chest lifted and your core engaged.
- Bend your knees and hips to lower your body into a squatting position, keeping your weight in your heels.
- Focus on pushing through your heels as you return to the starting position, squeezing your glutes and engaging the VMO at the top of the movement.
- Perform 2-3 sets of 10-15 repetitions.
- Single-Leg Press:
- Sit on a leg press machine with your back against the pad and your feet shoulder-width apart.
- Place one foot on the platform and extend your leg, keeping the other foot off the platform.
- Press the platform away from you by straightening your leg, focusing on engaging the VMO.
- Slowly bend your knee to return to the starting position.
- Perform 2-3 sets of 10-12 repetitions on each leg.
- Step-Ups:
- Stand facing a step or platform with your feet hip-width apart.
- Place one foot on the step and press through your heel to lift your body up onto the step.
- Lower yourself back down with control, focusing on engaging the VMO of the stepping leg.
- Perform 2-3 sets of 10-12 repetitions on each leg.
- Bulgarian Split Squats:
- Stand facing away from a bench or step with one foot elevated behind you.
- Lower your body into a lunge position by bending your front knee, keeping your chest upright.
- Push through your front heel to return to the starting position, engaging the VMO of the front leg.
- Perform 2-3 sets of 10-12 repetitions on each leg.
- Wall Sits:
- Stand with your back against a wall and slide down until your thighs are parallel to the floor, creating a seated position.
- Hold this position, focusing on engaging your quadriceps, including the VMO, for 30-60 seconds.
- Gradually increase the duration of the hold as you build strength.
Neuromuscular Training
Neuromuscular training for the VMO involves exercises and techniques aimed at improving the coordination, activation, and control of the quadriceps muscles, with a specific focus on the VMO. Here are some effective neuromuscular training exercises for the VMO:
- Isometric VMO Contractions:
- Sit or lie down with your legs extended.
- Place your fingers or hand on the inside of your knee to feel the VMO.
- Contract the VMO by pressing the inside of your knee towards the surface you’re sitting or lying on.
- Hold the contraction for 5-10 seconds, focusing on engaging the VMO.
- Relax and repeat for 10-15 repetitions.
- VMO Activation with Biofeedback:
- Use a mirror or place your hand on the VMO to provide visual or tactile feedback during exercises.
- Perform exercises such as mini squats, terminal knee extensions, or step-ups while focusing on activating and engaging the VMO.
- Use feedback from the mirror or your hand to ensure proper VMO activation throughout the movement.
- Proprioceptive Neuromuscular Facilitation (PNF):
- Perform PNF patterns such as rhythmic stabilization or contract-relax techniques to improve neuromuscular control and coordination of the quadriceps muscles, including the VMO.
- Incorporate PNF techniques into exercises like leg presses, lunges, or squats to enhance VMO activation and stability.
- Balance and Stability Exercises:
- Stand on one leg or use balance equipment such as a wobble board or balance disc.
- Focus on maintaining stability and control while engaging the VMO to stabilize the knee joint.
- Progressively challenge balance by incorporating dynamic movements or changing surfaces.
- Plyometric Training:
- Perform plyometric exercises such as jump squats, box jumps, or lateral hops to improve power and coordination of the quadriceps muscles, including the VMO.
- Focus on landing softly and absorbing shock with proper knee alignment and VMO activation.
- Functional Movement Patterns:
- Incorporate functional movements such as squatting, lunging, or stepping up and down onto a platform.
- Focus on proper alignment, control, and activation of the VMO throughout each movement to enhance neuromuscular coordination and stability.
- Manual Resistance Training:
- Work with a physical therapist or training partner to provide manual resistance against knee extension movements.
- Focus on resisting the resistance while engaging the VMO to strengthen the muscle and improve neuromuscular control.
- Mirror Therapy:
- Use a mirror to provide visual feedback during exercises, focusing on proper knee alignment and VMO activation.
- Perform movements such as squats or lunges while observing and adjusting knee position and VMO activation based on the mirror reflection.
Conclusion
In conclusion, Vastus Medialis Oblique (VMO) weakness poses a significant challenge to knee stability and function, impacting individuals’ daily lives and athletic endeavors. Understanding the multifactorial nature of VMO weakness, including its causes, symptoms, and effects, is essential for effective management and prevention strategies. Through a comprehensive approach encompassing proper diagnosis, targeted exercises, neuromuscular training, and preventive measures, individuals can address VMO weakness, improve knee stability, and enhance overall musculoskeletal health. By prioritizing regular exercise, proper technique, balanced training, and injury prevention strategies, individuals can mitigate the risk of VMO weakness, optimize knee function, and achieve long-term well-being. With dedication and guidance from healthcare professionals, individuals can overcome VMO weakness, reclaim their mobility, and pursue their desired activities with confidence and vitality.
References
- Myer GD, Ford KR, Barber Foss KD, Goodman A, Ceasar A, Rauh MJ, Divine JG, Hewett TE. The incidence and potential pathomechanics of patellofemoral pain in female athletes. Clin Biomech (Bristol, Avon) 2010;25:700–7. doi: 10.1016/j.clinbiomech.2010.04.001. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Engelina S, Antonios T, Robertson CJ, Killingback A, Adds PJ. Ultrasound investigation of vastus medialis oblique muscle architecture: an in vivo study. Clin Anat. 2014;27:1076–84. doi: 10.1002/ca.22413. [PubMed] [CrossRef] [Google Scholar]
- Arazpour M, Bahramian F, Abutorabi A, Nourbakhsh ST, Alidousti A, Aslani H. The effect of patellofemoral pain syndrome on gait parameters: a literature review. Arch Bone Jt Surg. 2016;4:298–306. [PMC free article] [PubMed] [Google Scholar]
- Arazpour M, Notarki TT, Salimi A, Bani MA, Nabavi H, Hutchins SW. The effect of patellofemoral bracing on walking in individuals with patellofemoral pain syndrome. Prosthet Orthot Int. 2013;37:465–70. doi: 10.1177/0309364613476535. [PubMed] [CrossRef] [Google Scholar]
- Johnston LB, Gross MT. Effects of foot orthoses on quality of life for individuals with patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2004;34:440–8. doi: 10.2519/jospt.2004.34.8.440. [PubMed] [CrossRef] [Google Scholar]
- Dixit S, DiFiori JP, Burton M, Mines B. Management of patellofemoral pain syndrome. Am Fam Physician. 2007;75:194–202. [PubMed] [Google Scholar]
- Murphy AC, Muldoon SF, Baker D, Lastowka A, Bennett B, Yang M, Bassett DS. Structure, function, and control of the human musculoskeletal network. PLoS Biol. 2018;16:e2002811. doi: 10.1371/journal.pbio.2002811. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Hortobágyi T, Garry J, Holbert D, Devita P. Aberrations in the control of quadriceps muscle force in patients with knee osteoarthritis. Arthritis Rheum. 2004;51:562–9. doi: 10.1002/art.20545. [PubMed] [CrossRef] [Google Scholar]
- Lefebvre R, Leroux A, Poumarat G, Galtier B, Guillot M, Vanneuville G, Boucher JP. Vastus medialis: anatomical and functional considerations and implications based upon human and cadaveric studies. J Manipulative Physiol Ther. 2006;29:139–44. doi: 10.1016/j.jmpt.2005.12.006. [PubMed] [CrossRef] [Google Scholar]
- Sattler M, Dannhauer T, Ring-Dimitriou S, Sänger AM, Wirth W, Hudelmaier M, Eckstein F. Relative distribution of quadriceps head anatomical cross-sectional areas and volumes–sensitivity to pain and to training intervention. Ann Anat. 2014;196:464–70. doi: 10.1016/j.aanat.2014.07.005. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Castanov V, Hassan SA, Shakeri S, Vienneau M, Zabjek K, Richardson D, McKee NH, Agur AMR. Muscle architecture of vastus medialis obliquus and longus and its functional implications: a three-dimensional investigation. Clin Anat. 2019;32:515–23. doi: 10.1002/ca.23344. [PubMed] [CrossRef] [Google Scholar]
- Sattler M, Dannhauer T, Hudelmaier M, Wirth W, Sänger AM, Kwoh CK, Hunter DJ, Eckstein F. Side differences of thigh muscle cross-sectional areas and maximal isometric muscle force in bilateral knees with the same radiographic disease stage, but unilateral frequent pain- data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2012;20:532–40. doi: 10.1016/j.joca.2012.02.635. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Glass NA, Torner JC, Frey Law LA, Wang K, Yang T, Nevitt MC, Felson DT, Lewis CE, Segal NA. The relationship between quadriceps muscle weakness and worsening of knee pain in the MOST cohort: a 5-year longitudinal study. Osteoarthritis Cartilage. 2013;21:1154–9. doi: 10.1016/j.joca.2013.05.016. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Villafañe JH, Bissolotti L, La Touche R, Pedersini P, Negrini S. Effect of muscle strengthening on perceived pain and static knee angles in young subjects with patellofemoral pain syndrome. J Exerc Rehabil. 2019;15:454–9. doi: 10.12965/jer.1938224.112. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Abe T, Loenneke JP, Thiebaud RS. Morphological and functional relationships with ultrasound measured muscle thickness of the lower extremity: a brief review. Ultrasound. 2015;23:166–73. doi: 10.1177/1742271X15587599. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Parry SM, El-Ansary D, Cartwright MS, Sarwal A, Berney S, Koopman R, Annoni R, Puthucheary Z, Gordon IR, Morris PE, Denehy L. Ultrasonography in the intensive care setting can be used to detect changes in the quality and quantity of muscle and is related to muscle strength and function. J Crit Care. 2015;30:1151.e9–14. doi: 10.1016/j.jcrc.2015.05.024. [PubMed] [CrossRef] [Google Scholar]
- Grob K, Manestar M, Filgueira L, Ackland T, Gilbey H, Kuster MS. New insight in the architecture of the quadriceps tendon. J Exp Orthop. 2016;3:32. doi: 10.1186/s40634-016-0068-y. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Ayala-Mejias JD, Garcia-Gonzalez B, Alcocer-Perez-España L, Villafañe JH, Berjano P. Relationship between widening and position of the tunnels and clinical results of anterior cruciate ligament reconstruction to knee osteoarthritis: 30 patients at a minimum follow-up of 10 years. J Knee Surg. 2017;30:501–8. doi: 10.1055/s-0036-1593367. [PubMed] [CrossRef] [Google Scholar]