“Explore the intriguing impacts of Joint Hypermobility Syndrome on our joints. An exciting journey to the heart of this little-known condition awaits you, revealing its implications on health and mobility. »
Introduction
Joint hypermobility syndrome, often overlooked, has significant effects on joint function, creating a delicate balance between excessive flexibility and increased vulnerability. This syndrome, characterized by extended joint range of motion beyond normal limits, can affect various parts of the body, ranging from peripheral joints to large axial joints.
The primary impact of joint hypermobility syndrome is the overstretching of the ligaments and connective tissues that stabilize joints. This overelasticity can lead to joint instability, increasing the risk of dislocations, subluxations, and other structural problems. Joints, instead of providing firm support, can become prone to excessive, uncontrolled movement.
The effects of joint hypermobility syndrome are particularly pronounced in large joints such as the shoulders, elbows and knees. People with this syndrome may experience a range of symptoms, including chronic joint pain, increased fatigue of surrounding muscles, and a propensity for joint injuries.
Additionally, joint hypermobility syndrome may influence muscle dynamics, as muscles may be required to compensate for structural joint weakness. This can lead to increased muscle tension, painful trigger points, and possibly posture problems.
Awareness of the effects of joint hypermobility syndrome is crucial for the management and prevention of associated complications. Therapeutic approaches such as osteopathy, targeted muscle strengthening and modification of physical activities can help stabilize joints, reduce pain and improve the quality of life of people with this syndrome. Raising awareness of these effects, both among health professionals and the individuals concerned, is essential to promote proactive and personalized management of this particular joint condition.
- Genetic Factors: HAS has a strong genetic component, meaning it can be inherited within families. Genetic mutations in certain genes, particularly those related to the production of collagen and other connective tissue proteins, are often associated with the development of HAS. People whose parents have joint hypermobility have an increased risk of developing this condition.
- Collagen Abnormalities: Collagen is an essential structural protein that provides strength and stability to connective tissues, including ligaments, tendons and joint cartilage. In AHS, abnormalities in collagen production or structure make tissues more elastic, leading to increased joint laxity. This laxity increases joint mobility beyond normal.
- Hormonal Factors: Certain hormonal factors can influence the expression of SHA. For example, hormonal fluctuations during puberty and pregnancy can make symptoms worse in some people. Sex hormones, particularly estrogen, play a role in regulating joint stability, and hormonal changes may contribute to joint hyperlaxity.
- Repetitive Trauma and Microtrauma: Joint trauma, particularly that occurring during growth, can be triggers for AHS. Repetitive strain injuries, such as excessive movement or strenuous sports activities, can also contribute to joint laxity and worsen symptoms in genetically predisposed individuals.
- Environmental Factors: In addition to genetic influences, environmental factors, such as infections and developmental disorders, may play a role in the development of HAS. Studies suggest that early infections or disruptions in the immune system may contribute to the manifestation of this condition.
- Central Nervous System Alterations: Alterations in the neurological control of posture and movement may also contribute to AHS. Some patients experience decreased proprioception, which can lead to excessive joint movements without adequate awareness of joint position.
- Joint Hypermobility:
- Abnormally high range of joint movement, often seen in multiple joints, including fingers, elbows, shoulders, knees, and hips.
- Ability to perform movements such as flexing the thumbs to touch the forearm or hyperextending the elbows and knees.
- Joint pain :
- Diffuse joint pain, often described as persistent, deep and sometimes shooting pain.
- Pain can be exacerbated by physical activity, stress or climate changes.
- Muscle fatigue :
- Frequent muscle fatigue, even after moderate effort.
- Feeling of muscle weakness, especially after prolonged periods of physical activity.
- Joint Instability:
- Feeling unstable or weak in the joints, increasing the risk of dislocations or sprains.
- Difficulty maintaining a stable posture, especially when walking or standing for prolonged periods.
- Coordination Problems:
- Difficulties in coordinating movements, which may affect walking, manipulating objects or performing fine tasks.
- Systemic Symptoms:
- Frequent headaches and migraines.
- Gastrointestinal problems such as gastroesophageal reflux, constipation or diarrhea.
- Urological problems, including increased bladder sensitivity.
- Sleeping troubles :
- Difficulty falling asleep or maintaining restful sleep.
- Frequent awakenings during the night due to pain or discomfort.
- Anxiety Symptoms:
- Some patients may experience anxiety, often related to managing chronic symptoms and fear of joint injury.
- Dermatological manifestations:
- Velvety or soft-to-the-touch skin.
- Atrophic scars (scars that appear thinner than normal) and bruise easily.
- Collagen Abnormalities:
- Collagen is an essential structural protein found in connective tissues, including ligaments, tendons and cartilage.
- In AHS, genetic mutations or abnormalities in collagen production make these tissues more elastic and less resilient, leading to increased joint laxity.
- Joint Laxity:
- Joint laxity resulting from collagen abnormalities allows for an abnormally wide range of joint motion.
- This joint hypermobility can lead to instability, promoting dislocations, sprains and excessive joint movement.
- Muscle Alterations:
- In response to joint laxity, surrounding muscles may undergo adaptive changes.
- Some muscles may become overactive to compensate for joint weakness or instability, while others may weaken due to lack of use.
- Neuromuscular Dysfunction:
- Collagen alterations can also affect mechanoreceptors and proprioceptors in connective tissues and muscles.
- This can lead to neuromuscular dysfunction, disrupting sensory perception and coordination of movements.
- Inflammation and Pain:
- Joint instability, combined with repetitive strain injuries, can trigger chronic inflammation in the joints and surrounding tissues.
- This inflammation can cause persistent joint pain, contributing to AHS symptoms.
- Joint Function Deficits:
- Joint laxity and muscle alterations can lead to deficits in joint function, affecting the ability to maintain adequate stability during daily movements and activities.
- Systemic Implications:
- SHA may have implications beyond the musculoskeletal system. Systemic symptoms, such as headaches, gastrointestinal problems, and sleep disturbances, may result from alterations in collagen and the body’s adaptive responses.
Joint damage experienced by those with Joint Hypermobility Syndrome (HAS) is a central aspect of this medical condition. AHS is characterized by an abnormally high range of joint motion, which can lead to adverse consequences for joint health.
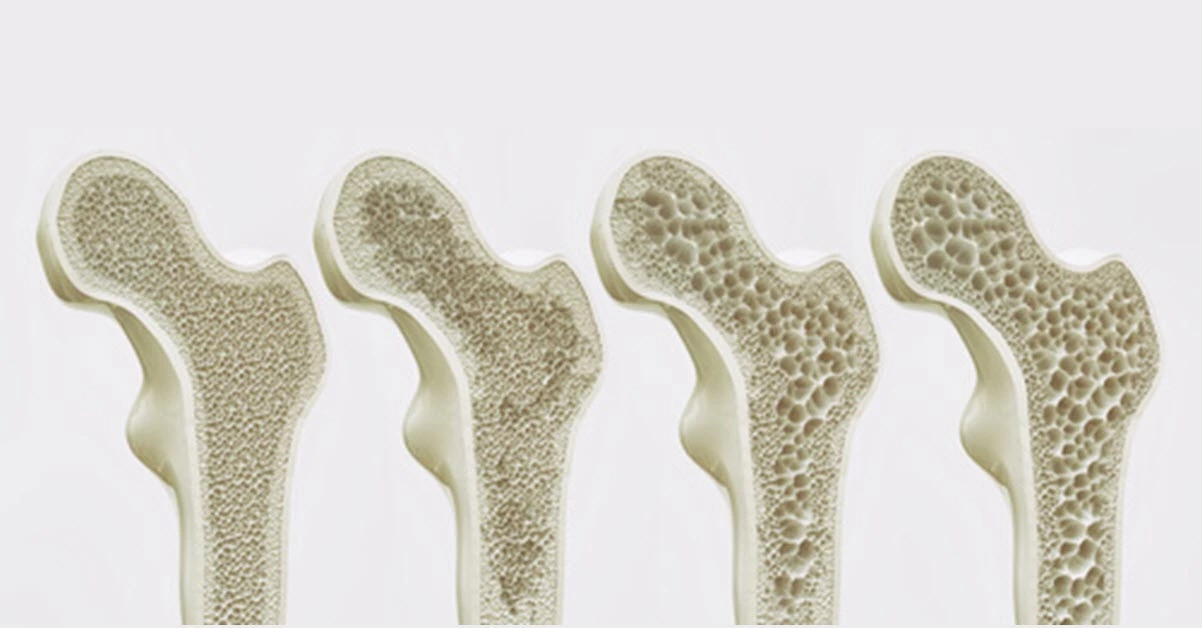
Frequent hyperextension of joints can lead to premature wear of cartilage, which normally acts as a shock absorber between bones. When cartilage becomes damaged, bones can rub directly against each other, causing painful inflammation and increasing the risk of developing osteoarthritis.
Ligaments and tendons, which usually stabilize joints, may also be affected in people with AHS. Increased joint laxity makes these structures more vulnerable to sprains and overstretching. Repetitive microtrauma, often associated with joint instability, can lead to chronic damage and contribute to progressive tissue deterioration.
The effects of SHA are not limited to peripheral joints. The joints of the spine can also be affected, leading to posture problems and lower back pain. The consequences of joint damage can have a significant impact on quality of life, leading to functional limitations, decreased mobility and increased pain over time.
Preventing joint damage in people with AHS is a critical aspect of managing this condition. Treatment approaches often aim to strengthen surrounding muscles to provide additional support to the joints. Specific exercises, focused on stabilization and strengthening, can help minimize the risk of injury and prevent damage from progressing.
Regular follow-up with healthcare professionals, such as rheumatologists, physiotherapists or osteopaths, is recommended to assess joint health, monitor the progression of the condition and adjust therapeutic interventions as needed.
In conclusion, joint damage is a major concern for those with Joint Hypermobility Syndrome. A comprehensive management approach, combining prevention strategies, specific exercises and regular medical monitoring, is essential to mitigate the adverse effects on joint health and improve the quality of life of people affected by this condition.
Diagnosis of hypermobility syndrome is often based on a combination of medical history, physical examination, and sometimes specific tests. Although there is no definitive single test for hypermobility syndrome, healthcare professionals can use the following approaches:
- Beighton score:
- The Beighton score is a simple clinical assessment that measures joint hypermobility. It involves checking the flexibility of different joints, such as the fingers, elbows and knees. A higher Beighton score may indicate increased joint hypermobility.
- Physical examination:
- Healthcare professionals will perform a thorough physical exam, assessing joint mobility, flexibility, and any associated symptoms, such as pain or instability.
- Family and medical history:
- Gathering information about personal and family medical history helps to understand whether hypermobility is a family characteristic or whether there are other related health conditions.
- Blood tests:
- In some cases, blood tests may be done to rule out other conditions associated with joint hypermobility, such as rheumatoid arthritis or autoimmune disorders.
- Genetic testing:
- In exceptional cases, genetic testing may be considered, especially if there is suspicion of a specific hereditary connective tissue disorder, such as Ehlers-Danlos syndrome.
- Imaging studies:
- X-rays or other imaging studies may be ordered to assess joint health, identify possible structural abnormalities, and rule out conditions such as arthritis.
It is important to note that hypermobility itself is not always pathological, and a diagnosis of hypermobility syndrome is usually made when joint hypermobility is associated with symptoms such as pain, fatigue, and instability. articular. Consult a rheumatologist, sp
As we conclude this exploration of the effects of Joint Hypermobility Syndrome, it becomes evident that in-depth knowledge of this condition is essential to guide management and treatment approaches. The complexity of its repercussions on mobility and joint health highlights the importance of individualized care. By continuing to deepen our knowledge, both on physiological aspects and on therapeutic solutions, we are opening the way to more effective and better adapted approaches. This will not only improve the quality of life of those affected, but also lay the foundation for a more complete understanding of the interactions between the human body and the challenges it may encounter. Thus, by combining our efforts in research and care, we are shaping a future where understanding of Joint Hypermobility Syndrome guides more precise interventions and significantly improves the well-being of those affected.
- Grahame R, Bird HA, Child A. The revised (Brighton 1998) criteria for the diagnosis of benign joint hypermobility syndrome (BJHS). J Rheumatol. 2000;27(7):1777-1779.
- Tinkle BT, Bird HA, Grahame R, Lavallee M, Levy HP, Sillence D. The lack of clinical distinction between the hypermobility type of Ehlers-Danlos syndrome and the joint hypermobility syndrome (aka hypermobility syndrome). Am J Med Genet A. 2009;149A(11):2368-2370.
- Castori M, Tinkle B, Levy H, Grahame R, Malfait F, Hakim A. A framework for the classification of joint hypermobility and related conditions. Am J Med Genet C Semin Med Genet. 2017;175(1):148-157.
- Hakim AJ, Grahame R. Joint hypermobility. Best Pract Res Clin Rheumatol. 2003;17(6):989-1004.
- Sinibaldi L, Ursini T, Turchetti G. Joint hypermobility syndrome: a common clinical disorder in rheumatology. Eur Rev Med Pharmacol Sci. 2015;19(24):4857-4861.