A throbbing sensation envelops my skull, each pulse of pain seeming to synchronize with the beating of my heart. Headaches, like waves of pressure, create a veil obscuring my state of well-being, giving way to a persistent discomfort that resonates like an acrobat in every corner of my head.
Understanding Tension Headaches and Their Triggers
Tension headaches are the most common type of primary headache, affecting millions of people worldwide. Unlike migraines, which often present with throbbing pain, nausea, and sensitivity to light or sound, tension headaches typically produce a dull, steady ache or a sensation of tightness that encircles the head like a band. This discomfort is often bilateral—affecting both sides of the head—and may radiate toward the neck and shoulders.
The pain is generally described as mild to moderate in intensity and does not usually worsen with physical activity. However, its persistence and frequency can significantly affect daily functioning and quality of life. Tension headaches can be episodic, occurring less than 15 days per month, or chronic, persisting more than 15 days a month for at least three months.
The exact mechanisms behind tension headaches remain complex and multifactorial. At the core, they are believed to result from heightened muscle tension and stress, particularly involving the muscles of the neck, shoulders, and scalp. Prolonged muscle contraction or postural strain—often related to sedentary work, screen overuse, or emotional stress—may trigger pain signals through the myofascial tissues and affect nearby nerves.
Psychological stress is one of the leading contributors to tension headaches. When the body enters a state of heightened alert—whether due to anxiety, fatigue, or emotional strain—it responds with muscle contraction, particularly in the upper back and neck. Over time, this creates sustained pressure on surrounding tissues and pain-sensitive structures, contributing to the onset and perpetuation of headaches.
Posture plays a major role in the development of this condition. Poor ergonomics, such as sitting hunched over a desk or looking down at a smartphone for extended periods, leads to an imbalance in the musculoskeletal system. This imbalance can cause shortening of the suboccipital muscles and overload the trapezius and cervical extensors, leading to tension and referred pain in the head.
In addition to stress and posture, several lifestyle factors can trigger or exacerbate tension headaches. Sleep disturbances, dehydration, skipping meals, excessive caffeine or alcohol intake, and eye strain from prolonged screen time are all well-recognized contributors. Identifying and managing these triggers can be a crucial step in reducing both the frequency and severity of episodes.
Hormonal fluctuations may also influence headache patterns, particularly in women. Although more commonly associated with migraines, hormonal changes during menstruation, pregnancy, or menopause can also affect muscular tone and sensitivity to stress, indirectly contributing to tension headaches.
Understanding the personal triggers behind tension headaches is essential for effective prevention and management. Keeping a headache diary can help identify patterns and contributing factors. Simple interventions—such as improving posture, ensuring regular hydration, maintaining consistent sleep routines, and incorporating stress-reducing practices—can make a meaningful difference.
Ultimately, while tension headaches are not usually dangerous, their chronic nature can significantly impact mental and physical well-being. A holistic, personalized approach that combines lifestyle adjustments with therapeutic interventions like osteopathy or physical therapy offers the best path toward long-term relief.
.

Recognizing Headache Types: Migraine, Tension, and More
Headaches can manifest in different forms, each with distinct characteristics. Some of the most common types include migraines, tension headaches, and cluster headaches. Here is a brief description of each of these types of headaches:
- Migraines:
- Migraines are often characterized by throbbing pain, usually on one side of the head.
- They may be accompanied by nausea, sensitivity to light and sound.
- Some patients may experience visual phenomena called “aura” before the migraine begins.
- Tension headaches:
- Tension headaches are usually described as a feeling of pressure or tightness around the head.
- They can be bilateral and are not aggravated by light to moderate physical activity.
- Stressors, fatigue or poor posture can trigger these headaches.
- Cluster headaches:
- Cluster headaches are characterized by extremely intense and sudden pain, often localized around one eye.
- They occur in episodes (clusters) and can last from 15 minutes to 3 hours.
- These headaches are frequently associated with symptoms such as watery eyes, nasal congestion and restlessness.
- Chronic daily headaches:
- Chronic daily headaches occur more than 15 days per month and may be related to overuse of headache medications.
- They can be of the tension or migraine type.
- Secondary headaches:
- These headaches are associated with an underlying medical condition such as an infection, injury, or vascular disorder.
- Treatment of secondary headaches often involves managing the underlying cause.
It is important to note that each individual may experience headaches uniquely, and some may exhibit mixed characteristics of different headache types. The precise diagnosis and optimal treatment plan will depend on the thorough clinical evaluation performed by a healthcare professional.
Top Headache Triggers: From Stress to Screen Time
Indeed, headaches can have many causes, and several everyday factors can contribute to their triggering. Here are some of the common causes of headaches:
- Stress: Chronic stress can trigger tension headaches. Stress management techniques, such as meditation and relaxation, can be helpful.
- Fatigue: Lack of sleep or prolonged fatigue can lead to headaches. It is important to maintain a regular sleep routine.
- Dehydration: Lack of hydration can cause headaches. Drinking enough water throughout the day is essential.
- Muscle tension: Tension in the neck and shoulder muscles can cause tension headaches. Proper posture and relaxation exercises can help prevent this.
- Caffeine: Excessive consumption or abrupt withdrawal of caffeine can lead to headaches. Moderate consumption may be recommended.
- Vision problems: Uncorrected vision problems can contribute to headaches. Glasses or corrective lenses may be necessary.
- Food: Certain foods or food additives can trigger headaches in some people. Keeping a food diary can help identify triggers.
- Hormones: Hormonal fluctuations, such as those that occur during the menstrual cycle or menopause, may be associated with headaches in some people.
- Weather: Some individuals are sensitive to changes in weather, atmospheric pressure or extreme temperatures, which can trigger headaches.
- Screens and lighting: Prolonged exposure to computer screens, phones and inadequate lighting can cause headaches. Regular breaks and appropriate lighting can help.
It is important to note that these factors can vary from person to person, and sometimes there can be a combination of several causes. If headaches are frequent, severe, or persist, it is recommended to consult a healthcare professional for a thorough examination and personalized management advice.
How Food Affects Your Head: Dietary Triggers and Tips
Diet can play a significant role in triggering headaches in some people. Identifying food triggers and making specific food choices can help prevent headaches. Here are some things to consider:
Food Triggers for Headaches
- Caffeine: Both excessive consumption and abrupt withdrawal of caffeine can trigger headaches. Moderate consumption may be recommended.
- Tyramine: Found in foods like aged cheese, smoked meats, and fermented foods, tyramine can trigger migraines in some people.
- Monosodium glutamate (MSG): Found in some prepared foods and condiments, MSG can be a headache trigger for some people.
- Aspartame: Some artificial sweeteners, including aspartame, have been linked to headaches in some sensitive people.
- Nitrates and nitrites: Found in cured meats and processed meats, these compounds can trigger headaches in some people.
- Alcohol: Consumption of alcohol, particularly red wine, beer, and certain spirits, may be associated with headaches, especially in sensitive individuals.
- Chocolate: Although the link is not clear to everyone, some people report that eating chocolate can trigger headaches.
- Fermented foods: Some fermented foods, such as yogurt and sauerkraut, contain bacteria that produce compounds that can trigger headaches in some people.
Diets that can help prevent headaches
Anti-migraine diet: Some migraine patients report improvement by following specific diets, such as the ketogenic diet, the gluten-free diet, or the low-tyramine diet.
- Mediterranean diet: This diet, rich in fruits, vegetables, whole grains, fish and olive oil, is associated with a reduced risk of headaches.
- Avoiding known triggers: An individual approach involves identifying and avoiding specific foods that trigger headaches in a given person.
- Maintain a balanced diet: Ensuring a balanced diet by including a variety of fresh foods can help prevent headaches related to nutritional deficiencies.
- Hydration: Drinking enough water throughout the day can help prevent headaches related to dehydration.
It’s important to note that food triggers vary from person to person. Keeping a food diary can help identify links between food choices and headaches. If you suffer from frequent headaches, it is recommended to consult a healthcare professional for personalized advice.
Mastering Stress: Relaxation, Meditation, and Yoga for Relief
Stress management is crucial to preventing headaches, and relaxation techniques, meditation and yoga can be powerful tools to promote mental and physical well-being. Here are some details about each of these approaches:
Relaxation techniques
- Deep breathing: Practice deep breathing by slowly inhaling through your nose, expanding your belly, then slowly exhaling through your mouth. Focus on the rhythm of your breathing to calm the nervous system.
- Progressive muscle relaxation: Gradually contract and relax different muscle groups in your body. Start at the feet and work your way up to the head, releasing tension with each step.
- Guided Imagery: Visualize a peaceful, positive place. Imagine the details of this place to create a feeling of calm and relaxation.
Meditation
- Mindfulness meditation: Focus your attention on the present moment. Observe your thoughts and feelings without judging them. Mindfulness meditation can reduce anxiety and stress.
- Transcendental meditation: Consists of silently repeating a mantra. This can help achieve a state of inner calm and reduce stressful thoughts.
- Guided meditation: Follow audio recordings or in-person sessions that guide you through relaxing scenarios and visualizations.
Yoga
- Asanas (postures): Practice yoga postures that combine fluid movements and breathing, promoting flexibility and relaxation. Poses like Child’s Pose and Savasana are particularly calming.
- Pranayama (breathing exercises): Incorporate yogic breathing techniques, such as abdominal breathing, to calm the nervous system and increase mental clarity.
- Yoga nidra: Also called “mindful sleep,” yoga nidra is a guided deep relaxation practice that can reduce stress and improve sleep.
Additional Tips
- Daily routine: Establish a daily routine that includes time dedicated to relaxation, even if it’s just a few minutes a day.
- Limiting stimuli: Reduce exposure to stressful stimuli, such as social media or negative information, especially before bed.
- Communication: Share your concerns with friends, family members or a healthcare professional. Communication can be an effective way to release stress.
- Physical activity: Regular exercise releases endorphins, thereby reducing stress. Find a physical activity you enjoy, like walking, running, or dancing.
Incorporating these techniques into your daily life regularly can not only help prevent stress-related headaches, but also improve your overall mental health. If headaches persist despite these strategies, consult a healthcare professional for further evaluation.
Hormones and Headaches: Cycles, Pregnancy, and Menopause
The link between hormones and headaches is well established, and hormonal fluctuations can play a significant role in triggering headaches in some people. Here’s how the different hormone-related phases of life can influence headaches:
Headaches related to the menstrual cycle
- Menstrual Migraines: Some women may experience migraines specifically related to their menstrual cycle. These migraines can occur before, during or after menstruation.
- Hormonal changes: Fluctuations in hormones, particularly estrogen levels, can trigger headaches in some women.
- Premenstrual syndrome (PMS): Headaches can be one of the symptoms associated with PMS, a condition characterized by various physical and emotional symptoms before the start of menstruation.
Headaches during pregnancy
- Pregnancy hormones: Significant hormonal changes during pregnancy, such as increased estrogen levels, can affect headaches.
- Improvement or Worsening: Some women find that their headaches improve during pregnancy, while others may experience them more intensely.
Headaches during menopause
- Decrease in hormones: Menopause is characterized by a significant decrease in hormones, particularly estrogen. This hormonal transition can influence the frequency and severity of headaches.
- Hormonal fluctuations: Hormonal fluctuations during perimenopause (the time before menopause) can also be associated with headaches.
Management approaches
- Hormonal contraceptives: Some hormonal contraceptives may affect headaches. It is essential to discuss contraceptive options with a healthcare professional.
- Hormone replacement therapy (HRT): For postmenopausal women, HRT may be considered under the supervision of a healthcare professional to alleviate symptoms, including headaches.
- Healthy lifestyle: Maintaining a healthy lifestyle, including a balanced diet, adequate hydration, regular exercise and stress management, can help alleviate hormone-related headaches.
- Medical Consultation: If headaches are frequent, severe, or disrupt daily life, it is recommended to consult a healthcare professional for an accurate diagnosis and appropriate management advice.
It’s important to note that each individual reacts differently to hormonal fluctuations, and managing hormone-related headaches can vary from person to person. A personalized approach under the supervision of a health professional is often the key to finding effective solutions.
Digital Fatigue: How Screens Contribute to Headaches
Frequent use of computer and phone screens can contribute to eye strain, a phenomenon also called computer vision syndrome, and potentially trigger digital headaches. Here is how these factors can interact:
Eye fatigue from screens
- Blue light emission: Computer screens, phone screens and other electronic devices emit blue light, which can strain the eyes and disrupt the sleep cycle if used before bedtime.
- Contrast and Illuminance: Inadequate contrast levels, excessive or insufficient screen brightness can strain the eyes and cause eye fatigue.
- Screen positioning: Poor screen positioning, causing glare or forcing the user into an awkward posture, can contribute to eye fatigue.
- Extended usage time: Continuous, prolonged use of screens without breaks can increase eye fatigue.
Digital headaches
- Eye strain: Eye strain from prolonged use of screens can cause tension in the eye muscles, triggering headaches.
- Bad posture: Uncomfortable posture or increased tension in the neck and shoulders from using screens can contribute to headaches.
- Visual Stress: The need to constantly focus on the screen can put strain on the eyes, increasing visual stress and causing headaches.
Management approaches
- Eye break and rest: Adopt the 20-20-20 rule: Every 20 minutes, look at something at least 20 feet away for at least 20 seconds to give the eyes a break.
- Blue light reduction: Use screen filters or enable blue light reduction mode on your devices, especially in the evening.
- Adjust brightness and contrast: Adjust the brightness and contrast of your screen for optimal visual comfort.
- Screen positioning: Place your screen at an appropriate distance and make sure it is at eye level to avoid uncomfortably lowering or raising your head.
- Hydration: Make sure you stay well hydrated, as dehydration can contribute to eye fatigue.
- Eye consultation: If eye fatigue and headaches persist despite these measures, consult a healthcare professional for a complete eye examination.
- Stress Management: Practice stress management techniques to reduce muscle tension and visual stress.
It is crucial to take preventative measures to alleviate eye strain related to screen use and thus reduce the risk of digital headaches. If symptoms persist, consult a healthcare professional for advice tailored to your individual situation.
Symptoms of Tension Headaches: Patterns, Duration, and Muscles
- Widespread pain: The pain is often described as a tight band sensation around the head, without throbbing.
- Duration: Tension headaches can last from a few minutes to several days, and they are often chronic, occurring recurrently.
- Location: The pain is usually bilateral and can affect the frontal, temporal or occipital region of the head.
- Varying Intensity: The pain is usually mild to moderate, but can sometimes be more severe.
- Triggers: Stress, fatigue, anxiety, muscle tension and awkward positions can trigger or worsen a tension headache.
- No accompaniment: Unlike other types of headaches, tension headaches are generally not accompanied by symptoms such as nausea, vomiting, or sensitivity to light.
Muscles responsible for tension headaches
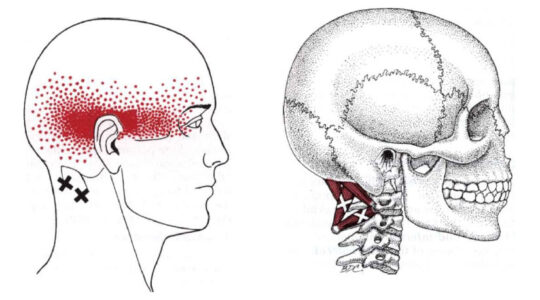
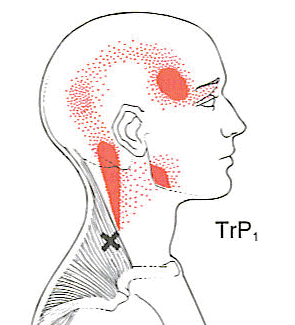
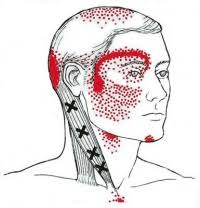

Occipitofrontal

The temporal gives a headache which is temporal
How Osteopathy Eases Tension Headaches: A Manual Approach
Here is how osteopathy can be approached for tension headaches:
- Postural assessment: An osteopath can assess the patient’s overall posture, including the position of the head, neck and spine. Adjustments can be made to improve alignment.
- Joint manipulation: The osteopath can use gentle joint manipulation techniques to improve mobility in the joints of the neck, head and back.
- Muscle release: Muscle release techniques, such as therapeutic massage, can be used to relax the neck and shoulder muscles.
- Craniosacral techniques: Some osteopaths use specific techniques linked to the mobilization of the craniosacral system, that is to say the skull and the sacrum, to promote balance in the cranial structures.
- Lifestyle advice: Osteopaths can also provide advice on lifestyle, ergonomics and specific exercises to help prevent muscle tension and headaches.
It is important to note that the effectiveness of osteopathy may vary from person to person, and it is recommended to consult a healthcare professional before undertaking any treatment, particularly if the headaches are frequent or serious. A qualified osteopath will assess the situation holistically and tailor interventions based on the patient’s individual needs.




























