Introduction
Psoas tendinitis, a painful condition affecting the psoas major muscle, can cause a variety of symptoms and requires a thorough understanding for effective treatment. This muscle, located deep in the abdominal region, is essential for hip flexion and plays a crucial role in pelvic stability.
People with psoas tendonitis may feel localized pain in the groin area, sometimes radiating to the lower back or thigh. Hip flexion movements, such as raising your leg, can make the pain worse. Activities that involve excessive use of the muscle, such as running or strenuous exercise, can contribute to the development of this tendinitis. A thorough understanding of the anatomy and biomechanics of the psoas is crucial to effectively evaluate and treat this condition.
Diagnosis of psoas tendonitis is often based on analysis of symptoms, the patient’s medical history, and physical examinations. Medical imaging, such as ultrasound or MRI, can be used to confirm the diagnosis and assess the extent of lesions. Psoas tendonitis can result from repetitive strain injuries, overuse, or even muscle imbalances. A holistic treatment approach may include osteopathic sessions aimed at strengthening the muscle, stretching techniques, and activity modifications to reduce stress on the psoas.
Preventing psoas tendinitis often involves adjustments in lifestyle and exercise habits. Proper warming up before physical activity, adopting correct training techniques, and strengthening surrounding muscles can help reduce the risk of developing this condition. Taking ergonomic factors into account in daily and professional activities can also play an important preventive role.
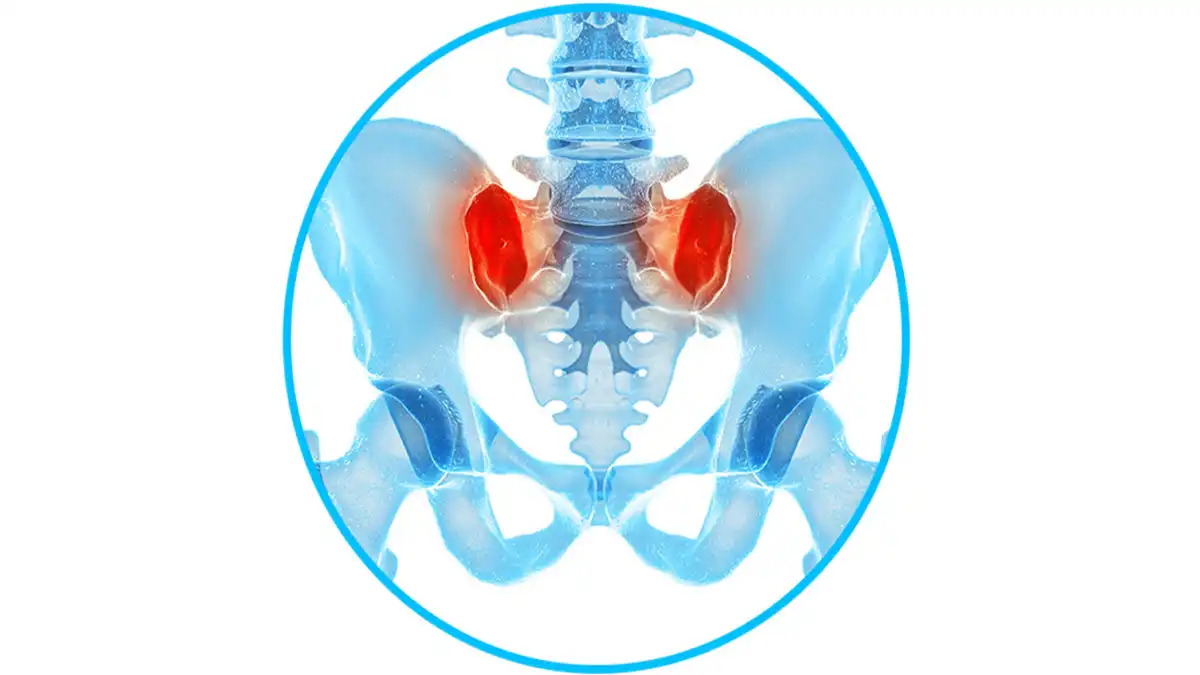
Anatomy of the psoas
The psoas muscle, often overlooked despite its importance, is an essential element of human anatomy, playing a crucial role in trunk stabilization and hip movement. To fully understand its impact on tendinitis, it is necessary to examine its anatomy and function in detail.
The psoas is a long and powerful muscle that belongs to the hip flexor muscle group. It is made up of two main parts: the psoas major and the psoas minor.
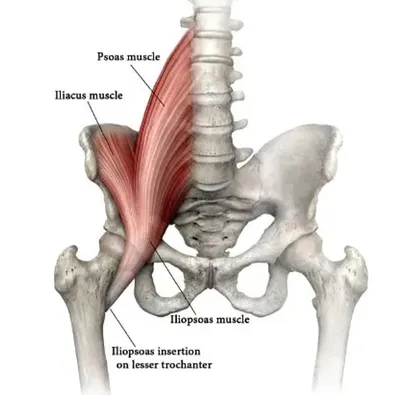
- Psoas major :
- Origin: It arises from the lumbar vertebrae, generally from T12 to L5.
- Path: The psoas major descends diagonally through the abdominal cavity, passing behind the viscera and large blood vessels.
- Insertion: It attaches to the lesser trochanter of the femur, a bony protrusion of the thigh bone.
- Psoas minor :
- Origin: It emerges from the upper lumbar vertebrae, generally from T12 to L1.
- Path: The psoas minor follows a similar path to the psoas major through the abdominal cavity.
- Insertion: It joins the psoas major tendon to attach to the lesser trochanter of the femur.
Psoas function
The psoas muscle performs several essential functions for movement and stability of the body:
- Hip flexion :
- The psoas is mainly responsible for hip flexion, that is, bringing the thigh closer to the trunk. This action is fundamental in movements like walking, running and jumping.
- Stabilization of the lumbar spine :
- In addition to flexing the hip, the psoas plays a crucial role in stabilizing the lumbar spine. It helps maintain correct posture by helping to prevent excessive hyperextension of the lumbar region.
Causes of Psoas Tendonitis
Psoas tendinitis, a painful condition involving inflammation of the psoas major muscle, has varied causes that require in-depth understanding. This muscle, essential for hip flexion, can undergo excessive stress, leading to microtrauma and the inflammation characteristic of tendinitis.
One of the main causes of psoas tendonitis is overuse of the muscle, often seen in athletes or individuals engaged in activities requiring frequent hip flexion. Runners, dancers, and strenuous exercisers can overuse the psoas, increasing the risk of developing this condition. Repetitive microtrauma can lead to damage to the psoas tendon, triggering an inflammatory reaction.
Muscle imbalances can also contribute to psoas tendonitis. Weakness or overactivity of other surrounding muscles can change the load placed on the psoas, leading to overuse and possibly inflammation. For example, weakened gluteal muscles can lead to excessive compensation of the psoas, thereby increasing stress on this muscle.
Anatomical factors may play a role in the development of psoas tendonitis. Particular anatomy, such as an unusual shape of the muscle or variations in the surrounding bone structure, can create points of increased stress on the psoas tendon. These anatomical factors can make the muscle more vulnerable to stress and inflammation.
Direct trauma, although less common, can also cause psoas tendinitis. A fall on the hip or a direct impact on the abdominal region can damage the psoas tendon, triggering an inflammatory response.
Common causes of psoas tendonitis include:
- Overuse or overload: Psoas tendonitis can occur due to repetitive movements or overuse of the muscle. Activities such as running, walking, and exercises that involve frequent hip flexion can contribute to this overload.
- Poor exercise technique: Improperly performed exercises, especially those that frequently strain the psoas muscle, can lead to tendon irritation.
- Traumatic injury: A direct injury to the groin or hip area, such as a fall or impact, can cause inflammation of the psoas tendon.
- Muscle Imbalances: Muscle imbalances in the hip or pelvis area can lead to overload of the psoas muscle, contributing to tendinitis.
- Poor posture: Poor posture, especially when walking, running or sitting for prolonged periods, can affect the way the psoas is used and potentially lead to tendinitis.
- Underlying medical conditions: Certain medical conditions, such as hip arthritis or musculoskeletal disorders, may increase the risk of developing psoas tendinitis.
- Excessive stress on the tendon: Repetitive movements or strenuous physical activities can cause excessive stress on the psoas tendon, contributing to its inflammation.
Risk factors
Psoas tendonitis can be triggered by a variety of factors, whether related to specific physical activities, muscle imbalances, or repetitive movements. Let’s explore these risk factors in detail:
Lists of risk factors
- Specific physical activities :
- Running : Runners are often at risk for psoas tendonitis due to the constant repetition of hip movement, especially when propelling and landing.
- Jumping sports : Activities that involve repeated jumping, such as high jumping, broad jumping, or volleyball, may also increase the risk of psoas tendonitis due to excessive force placed on the muscle during extension of the hip.
- Muscle imbalances :
- Abdominal Weakness : A weak abdominal core can lead to overuse of the psoas to stabilize the lumbar spine, which can increase the risk of injury.
- Weak glutes : Weak glutes can lead to poor hip mechanics, forcing the psoas to compensate, which can lead to overload and possibly tendonitis.
- Repetitive movements :
- Repetitive movements that constantly strain the psoas, such as sit-ups or traditional ab exercises, can lead to inflammation and tendonitis if not performed correctly or if performed excessively.
- Occupations that involve sitting for long periods of time, such as drivers, secretaries, or computer programmers, may also increase the risk of psoas tendonitis due to prolonged sitting and constant compression of the muscle.
- Bad exercise technique :
- Improper exercise technique when performing hip flexion exercises, such as the squat or deadlift, can put excessive stress on the psoas and increase the risk of injury.
- Poorly performed stretching exercises can also worsen muscle tension and increase the risk of psoas tendonitis.
- Age and physical condition :
- Aging can lead to decreased flexibility and muscle strength, which can increase the risk of tendonitis, including psoas.
- Likewise, insufficient fitness can make muscles more vulnerable to injury, including psoas tendinitis.
- Overuse and overtraining :
- Overuse of the psoas muscle due to a sudden increase in exercise intensity or duration, or an increase in training volume too quickly, can lead to irritation and inflammation of the muscle, increasing the risk of tendonitis.
- Overtraining, which occurs when the body is put under excessive stress without adequate recovery periods, can also contribute to the development of tendinitis.
- Individual anatomy :
- Certain anatomical variations, such as differences in muscle or tendon length, can influence how the psoas is used during movements and increase the risk of injury.
- Bad postural habits :
- Poor posture, whether standing, sitting, or during exercise, can lead to muscle imbalance and overuse of the psoas to compensate, increasing the risk of tendinitis.
- Previous injuries :
- Previous injuries, especially those that affect the hip, lower back, or abdominal muscles, can weaken the psoas and increase the risk of developing tendinitis in the future.
- Metabolic and systemic factors :
- Certain metabolic or systemic conditions, such as rheumatoid arthritis, diabetes, or thyroid disorders, may increase susceptibility to inflammation and injury of the tendons, including the psoas.
- Biomechanical defects :
- Biomechanical defects such as excessive foot pronation, excessive hip internal rotation, or postural imbalances can lead to overload of the psoas muscle, increasing the risk of tendinitis.
- Environmental factors :
- Environmental factors such as hard or uneven running surfaces can increase the impact on the body and increase stress on the psoas muscle, increasing the risk of injury.
- Poor recovery :
- Inadequate recovery after strenuous exercise can lead to persistent muscle fatigue and an increased risk of injury, including psoas tendonitis.
- Psychosocial factors :
- Emotional or psychological stress can affect the perception of pain and the body’s ability to recover, which can increase vulnerability to injury, including tendinitis.
- Working conditions :
- Occupations that involve lifting heavy objects or remaining in uncomfortable positions for long periods of time can place excessive pressure on the psoas, increasing the risk of injury.
- Poor hydration and nutrition :
- Insufficient hydration and an unbalanced diet can compromise muscle health and recovery, increasing the risk of psoas tendonitis and other injuries.
- Genetic factors :
- Some individuals may be genetically predisposed to musculoskeletal problems, including tendonitis, due to variations in soft tissue structure or function.
Symptoms of Psoas Tendonitis
Symptoms of psoas tendinitis can vary in intensity and manifestation, but they often share common features that signal inflammation of the psoas major muscle. This condition, characterized by pain in the groin or upper thigh region, can have a significant impact on the mobility and quality of life of affected individuals.
Pain is the most common symptom of psoas tendonitis. It is usually felt in the anterior groin area, sometimes radiating up the thigh. The pain may be sharp, stabbing, or dull, depending on the severity of the inflammation. Movements that involve hip flexion, such as raising the knee, can trigger or worsen pain.
Stiffness or restricted mobility in the hip is a common symptom of psoas tendonitis. Individuals may experience difficulty performing bending movements or lifting the leg, which may limit their range of motion.
Tenderness on palpation in the groin area is a common indicator of psoas inflammation. When a healthcare professional applies light pressure to the affected area, the patient may feel tenderness or discomfort, confirming the presence of tendinitis.
Clicks or crackles can sometimes accompany psoas tendonitis. These sounds, known as crepitations, often result from tendons or surrounding structures rubbing together during hip movements. Although not specific to psoas tendonitis, these noises may be observed in some individuals with this condition.
Pain associated with psoas tendonitis can affect daily activities, including walking, climbing stairs, and other hip movements. Some individuals also experience increased pain during the night, which can disrupt their sleep.
Symptoms of psoas tendonitis can vary from person to person, but they are generally related to pain and discomfort in the groin and hip area. Here are some of the common symptoms associated with psoas tendonitis:
- Groin pain: The pain is usually felt deep in the groin area on the affected side. It can be dull, throbbing or sharp.
- Pain radiating towards the thigh: The pain may extend towards the top of the thigh, following the trajectory of the psoas muscle.
- Pain when flexing the hip: Pain is often worse during activities that use the psoas muscle, such as flexing the hip. This may include walking, running, stair climbing, or knee lifting.
- Sensitivity to touch: The area around the psoas tendon may be sensitive to touch.
- Localized swelling: There may be slight swelling in the groin area.
- Muscle stiffness: A feeling of stiffness or tension in the groin and hip area.
- Worsening during or after activity: Pain may worsen during or after activities that put pressure on the psoas muscle.
Screening test
Here are some commonly used orthopedic tests to evaluate this condition, along with instructions on how to perform them:
Resisted hip flexion test :
- The patient lies on his back with his legs extended.
- The practitioner asks the patient to raise one straight leg upwards against the practitioner’s resistance.
- Increased pain in the groin area or apparent weakness may indicate psoas tendinitis.
Modified Thomas test :
- The patient lies on his back at the end of a table with both legs dangling over the edge.
- The patient brings one knee toward the chest while the other leg remains dangling.
- If the knee of the hanging leg rises involuntarily or the back arches, this may indicate psoas shortening or excessive tension.
Traditional Thomas test :
- The patient lies on a table with both legs extended.
- The patient brings one knee toward the chest and holds it at the chest.
- If the other leg involuntarily bends at the knee or the lower back lifts off the table, this may indicate excessive psoas tension.
Hip flexion strength test in supine position :
- The patient lies on his back with his legs extended.
- The practitioner applies resistance to the anterior aspect of the patient’s knee while the patient attempts to flex the hip against the resistance.
- Increased pain in the groin area may indicate psoas tendinitis.
Modified Craig test :
- The patient is in a supine position, with the practitioner flexing and rotating the affected hip.
- The practitioner feels the angle formed by the greater trochanter of the femur as he rotates the hip.
- An abnormally small angle may indicate excessive internal rotation, which may be associated with excessive psoas tension.
Recommendations for people with psoas tendonitis
- Rest: Avoid activities that exacerbate pain. Rest allows the psoas tendon to recover.
- Ice application: Apply ice to the painful area for 15 to 20 minutes every few hours for the first few days to reduce inflammation.
- Regular Stretches: Incorporate gentle stretches into your daily routine to improve psoas flexibility.
- Activity modification: Avoid activities that could make psoas tendonitis worse, such as repetitive movements or heavy lifting.
- Ergonomics: Make sure your posture and ergonomics at work and at home are not contributing to strain on the psoas.
- Stress management: Stress can influence muscle tension. Consider stress management techniques, such as meditation or relaxation.
- Appropriate shoes: Choose comfortable, well-fitting shoes to avoid any disruption to posture and walking.
- Maintaining a Healthy Weight: If necessary, work with your doctor to maintain a healthy weight, as excess weight can worsen strain on the psoas.
Exercises and stretches for people with psoas tendonitis
The exercises and stretches below may be considered, but should not be performed without the supervision or approval of a healthcare professional.
1. Psoas Stretch:
- Kneel on one knee with the other leg bent 90 degrees in front of you.
- Tilt your pelvis forward, keeping your back straight, until you feel a stretch in the psoas region.
- Hold the position for 15 to 30 seconds and repeat on the other side.
2. Quadriceps Stretch:
- While standing, bend one leg and grab your ankle with the hand on the same side.
- Bring your heel toward your buttock until you feel a stretch in the front of your thigh.
- Hold the position for 15 to 30 seconds and repeat on the other side.
3. Hip Stretch:
- Lie on your back with your knees bent.
- Cross one ankle over the other knee, forming a figure 4 with your legs.
- Gently pull the crossed leg toward your chest until you feel a stretch in the hip.
- Hold the position for 15 to 30 seconds and repeat on the other side.
4. Piriformis Stretch:
- Sitting on the floor, cross one leg over the other.
- Place the elbow opposite the crossed leg against the knee, then gently twist backwards.
- Hold the position for 15 to 30 seconds and repeat on the other side.
5. Abdominal strengthening exercise:
- Perform abdominal exercises such as planks and controlled leg raises to strengthen the abdominal muscles and stabilize the lower back region.
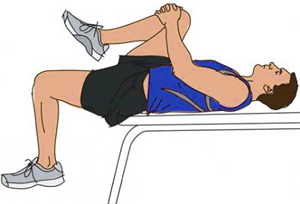
6. Lying knee raise exercise:
- Lie on your back, bend your knees and lift one knee toward your chest.
- Hold the position for a few seconds, then slowly lower the leg.
- Repeat with the other leg.
It is crucial to start slowly, avoid any painful movements and progress gradually. If you experience increased pain during or after exercise, stop immediately and consult a healthcare professional.
Osteopathy therapeutic treatment
Here are some osteopathic techniques that could be considered for psoas tendinitis:
- Gentle manipulation of the psoas: The osteopath can use gentle manipulations to release tension in the psoas muscle. This may involve massaging and kneading movements to encourage muscle relaxation.
- Psoas Stretching: Specific stretching techniques can be applied to improve the flexibility of the psoas and reduce pressure on the tendon.
- Myofascial release techniques: The osteopath may use myofascial release techniques to release tension in the connective tissues surrounding the psoas.
- Muscle Energy Techniques (MET): These techniques involve active participation from the patient, where they contract and relax the muscle while the osteopath applies light resistance. This can help improve flexibility and muscle function of the psoas.
- Joint manipulation: Gentle manipulations can be applied to nearby joints, such as the hip and lumbar spine, to improve mobility and reduce strain on the psoas.
- Postural balancing: The osteopath can assess and correct postural imbalances that could contribute to psoas tendinitis.
- Exercises and advice: The osteopath can recommend specific exercises aimed at strengthening the surrounding muscles, improving stability and promoting better posture.
Recovery and rehabilitation
Rest and reduction of activities
- Rest :
- Give your body time to rest and recover. Avoid activities that exacerbate pain or tension in the psoas area.
- Reduction of high impact activities :
- Avoid high-impact activities, such as running or jumping, which could worsen psoas tendonitis during the initial recovery phase.
Pain and inflammation management
- Ice application :
- Apply ice to the groin area for 15 to 20 minutes several times a day to reduce inflammation and relieve pain.
- Anti-inflammatories :
- If necessary, take nonsteroidal anti-inflammatory drugs (NSAIDs) as recommended by your doctor to reduce inflammation and relieve pain.
Physical therapy and stretching
- Physical therapy :
- See a physical therapist for physical therapy sessions aimed at strengthening surrounding muscles, improving flexibility, and restoring normal function to the psoas.
- Gentle stretches :
- Once pain and inflammation begin to subside, incorporate gentle psoas stretches into your routine to help reduce muscle tension and improve flexibility.
Muscle strengthening and rehabilitation
- Progressive reinforcement :
- Gradually begin a strength training program for the hip stabilizing muscles, including the glutes and abdominal muscles, to strengthen and stabilize the pelvic region.
- Functional rehabilitation :
- Work with your physical therapist for functional rehabilitation that aims to restore your body’s ability to perform functional movements without pain or restriction.
Gradual return to activities
- Gradual return to activities :
- Once you have progressed in your rehabilitation and the pain has subsided, gradually return to incorporating low-impact activities, then progress to more intensive activities as your strength and endurance improve.
- Monitoring and adjustment :
- Continue to monitor your pain and progress as you return to activities. If you experience increased pain or discomfort, stop and consult your healthcare professional to adjust your rehabilitation plan.
Conclusion
In conclusion, psoas tendonitis is a painful condition that can affect the hip and compromise musculoskeletal function. Understanding risk factors, diagnostic methods, treatment options, and prevention strategies is essential to effectively managing this condition.
Risk factors include specific physical activities, muscle imbalances, repetitive movements, and other anatomical, metabolic, and environmental factors. Diagnosing psoas tendonitis involves a thorough evaluation including a history, physical examination, orthopedic testing, and, if necessary, medical imaging techniques.
To prevent psoas tendonitis, it is important to practice adequate warm-up, balance physical activities, adopt good exercise technique, manage stress and lifestyle, and strengthen and balance the hip muscles.
Recovery and rehabilitation for psoas tendonitis involves rest, pain and inflammation management, physical therapy, stretching, progressive muscle strengthening, and a gradual return to activities.
Reference
- Page P (2007) The Janda approach to musculoskeletal pain
- Bullock-Saxton JE, Janda V, Bullock MI (1993) Reflex activation of gluteal muscles in walking. Spine 18(6):704–708 [ PubMed ]
- Bullock-Saxton JE, Janda V, Bullock MI (1994) The influence of ankle sprain injury on muscle activation during hip extension. Int J Sports Med 15(6):330–334 [ PubMed ]
- Cowen SM, Schache AG et al (2004) Delayed onset of transversus abdominus in long-standing groin pain. Med Sci Sports Exerc 36(12):2040–2045 [ PubMed ]
- Panjabi MM (1992) The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Dis 5(4):383–389 [ PubMed ]
- Janda V (1987) Muscles and motor control in low back pain: assessment and management. In: Twomey LT (ed) Physical therapy of the low back. Churchill Livingstone, New York, pp 253–278
- Pettman E (2007) Lecture presented for the NAIOMT Lecture Series. Andrews University, Berrien Springs, Michigan
- Gracovetsky SA, Iacono S (1987) Energy transfers in the spine engine. J Biomed Eng 9(2):99–114 [ PubMed ]