Introduction
Lumbar disc herniation is a feared spinal condition that can cause severe pain and significantly impair quality of life. To better understand this condition, let’s explore the complex anatomy of the lumbar spine, the underlying mechanisms of herniated disc, potential causes, associated symptoms, management recommendations, research advances, and the role of osteopathy in this adventure.
The lumbar spine is made up of five vertebrae (L1 to L5) located in the lower part of the back, between the thoracic spine and the sacrum. These vertebrae support the body’s weight and allow a range of motion, but they are also prone to various conditions, including herniated discs.
Disc herniation occurs when the gelatinous core of the intervertebral disc extends beyond its outer structure, putting pressure on adjacent nerves. Causes may include aging, genetics, trauma, or overuse of the spine.
Symptoms of a herniated disc vary, but can include severe lower back pain, numbness, tingling, and weakness in the legs. Treatment may include medications, physical therapy, lifestyle changes, and in some cases, surgery.
Research is continually exploring new approaches to treating herniated discs, such as gene therapy or the use of stem cells. Osteopathy, a holistic approach, can play a role in managing symptoms by improving the body’s mobility and balance.
X-ray images, such as MRI or CT, are used to diagnose a herniated disc by visualizing the structure of the spine. In conclusion, lumbar disc herniation requires a multidisciplinary approach for effective management, with continued advances providing new perspectives to provide relief to patients affected by this debilitating spinal condition.
Anatomy of Intervertebral Discs
The intervertebral discs, located between the vertebrae of the spine, play a crucial role as cushions providing the flexibility and strength necessary for this complex structure. The spine consists of twenty-four movable vertebrae, while five of them fuse together to form the sacrum. Discs, subject to injury, must combine sufficient flexibility to allow movement and robustness capable of withstanding considerable stress. The lower lumbar discs, in supporting the weight of the upper body, are particularly vulnerable and frequently subject to injury.
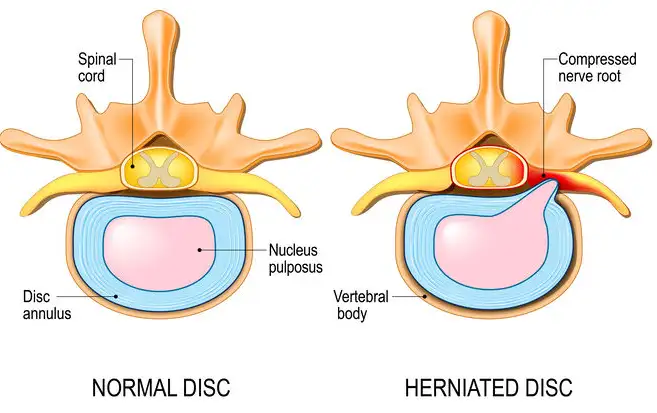
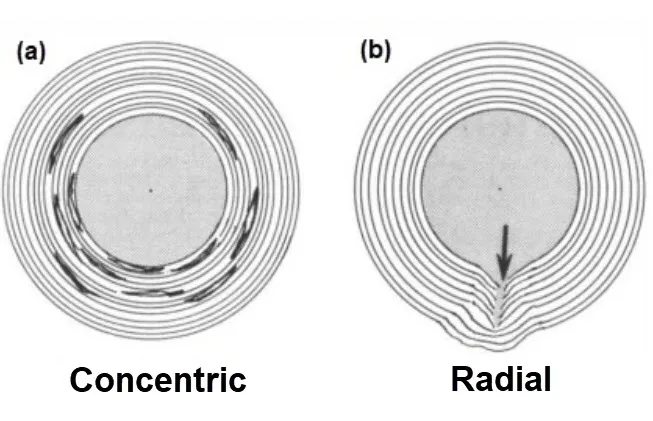
The structure of a disc consists of a rigid outer layer called the “annulus fibrosus” surrounding a gelatinous center called the “nucleus pulposus.” With aging, the nucleus pulposus gradually loses its hydration level, thus reducing its effectiveness as a cushion. A herniated disc occurs when the nucleus pulposus escapes through the outer annulus fibrosus, causing the center of the disc, also known as a herniated or ruptured disc, to move through a crack in the outer layer. Terms such as disc herniation, rupture, protrusion, and extrusion all describe this injury, although with subtle nuances. They refer to a tear in the outer ring allowing part of the inner core to escape.
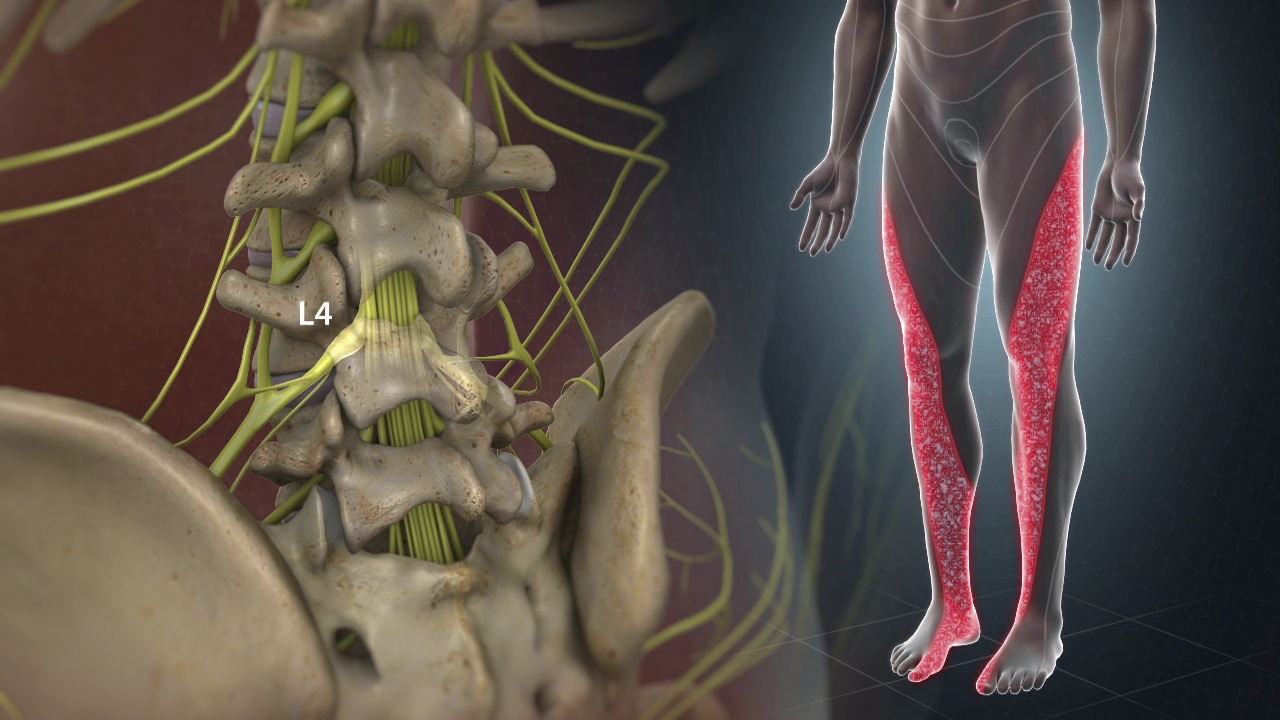
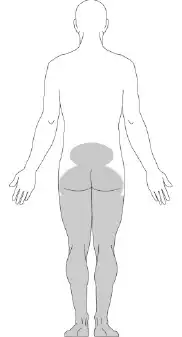
The majority of herniated discs occur in the lower two discs of the lumbar spine. A lumbar disc herniation can put pressure on the nerves in the spine, leading to symptoms such as pain, numbness, tingling, or weakness in the leg, commonly known as “sciatica.” Sciatica affects approximately 1 to 2% of the population, mainly between the ages of 30 and 50.
Pathophysiology of Lumbar Disc Herniation
Here are the stages of the pathophysiology of lumbar disc herniation in a clear and precise manner:
- Trauma or Wear:
- A herniated disc can result from acute trauma, such as improper lifting of heavy objects, or from gradual wear and tear due to aging and natural wear and tear of the intervertebral discs.
- Disc Degradation:
- The intervertebral disc undergoes degenerative changes over time. Dehydration of the nucleus pulposus and loss of elasticity of the annulus fibrosus make the disc more vulnerable to cracking.
- Fibrosus Ring Cracking:
- Due to wear and tear, the annulus fibrosus may develop cracks or tears. These cracks can allow the nucleus pulposus to move out of its normal position.
- Protrusion of the nucleus pulposus:
- The nucleus pulposus, or part of it, may protrude through the crack in the annulus fibrosus. This forms a protrusion or protrusion of the disc, sometimes called a herniation.
- Nerve Root Compression:
- Disc protrusion can put pressure on nerve roots that emerge from the nearby spinal cord. This can lead to irritation of the nerves and cause symptoms such as pain, numbness or muscle weakness in the lumbar region, buttocks, legs and sometimes even the feet.
- Inflammatory Response:
- Compression of nerve roots triggers a local inflammatory response, contributing to the intensification of symptoms. The inflammation can also irritate surrounding nerves.
- Muscular and Postural Reaction:
- To protect the spine and compensate for pain, surrounding muscles may contract involuntarily, leading to altered posture and sometimes muscle spasms.
- Clinical Symptoms:
- Symptoms of lumbar disc herniation can vary depending on the location of the protrusion and the affected nerve root. These symptoms include lower back pain, sciatica (pain along the sciatic nerve), numbness, muscle weakness, and possibly problems with bladder or bowel control.
Narrowing of the posterior longitudinal ligament
The posterior longitudinal ligament (PLL) is a fibrous structure found at the back of the spine, within the spinal canal. It extends along the posterior surface of the vertebrae and helps hold the intervertebral discs in place. When there is narrowing of the posterior longitudinal ligament, it can lead to symptoms that are often related to compression of the spinal cord or nerve roots in the spinal canal.
When there is narrowing of the posterior longitudinal ligament in association with a lumbar disc herniation, this can worsen symptoms by increasing compression of the nerve structures in the spinal canal. Symptoms may include lower back pain, pain radiating down the buttocks and legs, muscle weakness, numbness and tingling.
Causes of Lumbar Disc Herniation
- Aging: The natural aging process causes changes in the intervertebral discs. Over time, discs lose their elasticity and ability to absorb shock, making them more prone to herniation.
- Wear and Tear: Repetitive movements or overuse of the spine, often associated with certain jobs or activities, can cause wear and tear of the intervertebral discs.
- Poor Body Mechanics: Adopting poor posture, lifting heavy objects incorrectly, or making sudden movements without using supporting muscles can increase the risk of a herniated disc.
- Obesity: Excessive weight can put additional pressure on the intervertebral discs, increasing the risk of disc herniation.
- Genetics: Some individuals may be genetically predisposed to developing intervertebral disc problems, increasing their susceptibility to herniations.
- Sedentary Lifestyle: Low physical activity and lack of exercise can contribute to weakness in the supporting muscles of the spine, increasing the risk of herniated discs.
- Trauma: Trauma, such as a car accident, a fall, or a direct blow to the spine, can lead to a herniated disc.
- Genetic Factors: Genetic factors may play a role in predisposing to conditions such as disc degeneration, thereby increasing the risk of disc herniation.
What levels do lumbar disc herniation occur most often?
L4-5 > L5-S1 > L3-4 > L2-3 > L1-2
Symptoms of Lumbar Disc Herniation
- Lower back pain: Pain in the lower back region is one of the most common symptoms. The pain may be localized to the spine or radiate to the buttocks and legs.
- Sciatica pain: A herniated lumbar disc can put pressure on the sciatic nerve, causing pain that travels down the leg. This pain is often called sciatic pain.
- Numbness and Tingling: Sensations of numbness, tingling or weakness may occur in the lower back, buttocks, thighs or legs.
- Muscle Weakness: Nerve compression can lead to muscle weakness in the leg or foot. This may affect the ability to lift the foot, flex the knee, or perform other movements.
- Pain Worsened by Activity: Pain may worsen during certain activities, such as walking, coughing, sneezing, or sitting for prolonged periods.
- Burning Sensation: Some individuals report a burning sensation along the affected nerve.
- Coughing or Sneezing Makes Pain Worse: Movements that increase pressure in the spine, such as coughing or sneezing, can make pain worse.
- Alteration of Reflexes: In some cases, a herniated disc can cause an alteration of reflexes, notably the patella reflex or the Achilles reflex.
Osteopathy: A Natural Ally Against Lumbar Disc Herniation
- Soft Tissue Techniques:
- Massage and Stretching: Using massage and stretching techniques to relax tense muscles.
- Myofascial Release: Manipulation of connective tissue layers (fascia) to improve mobility.
- Cranial Techniques:
- Cranial Osteopathy: Gentle manipulation of the skull to influence the circulation of cerebrospinal fluid and restore balance.
- Visceral Techniques:
- Visceral Manipulation: Gentle manipulation of internal organs to improve mobility and function.
- Global Treatment Techniques:
- Holistic Approach: Consideration of the whole body to treat problems at the source.
- Exercises and Tips:
- Exercise Prescription: Recommendation of specific exercises to strengthen muscles and improve posture.
- Lifestyle Advice: Guidance on nutrition, sleep and other aspects of lifestyle to promote health.
Exercise and stretching
It is important to note that osteopaths generally assess the patient as a whole, looking not only at the symptomatic area, but also at other parts of the body that may be contributing to the problem. The techniques used may vary depending on the practitioner and the specific needs of the patient.
- Posterior Chain Stretch:
- Lie on your back, bend your knees and place your feet flat on the floor.
- Slowly lift the pelvis by contracting the glutes, creating a straight line from the shoulders to the knees.
- Hold the position for a few seconds, then slowly lower back down.
- This stretch relieves tension in the lumbar region.
- Cat and Cow Stretch:
- Get on all fours with your hands under your shoulders and your knees under your hips.
- Slowly curl your back upwards while exhaling (cat position).
- While inhaling, arch your back downward, arching your spine (cow position).
- Repeat this sequence several times to improve mobility of the lumbar spine.
- Psoas Stretch:
- From your knees, step one leg forward at a 90-degree angle.
- Hold the position, feeling the stretch in the back side hip.
- Alternate legs to stretch both sides.
- Core Strengthening Exercises:
- The abdominal and lower back muscles play a crucial role in supporting the spine. Exercises such as planks, leg raises, and modified crunches can strengthen these muscles without putting too much strain on the lumbar spine.
- Yoga:
- Certain yoga poses, such as downward-facing dog and child’s pose, can help stretch and strengthen the muscles surrounding the lumbar spine.
- Walk :
- Regular walking is a low-impact activity that can promote blood circulation, relieve pressure on the spine and help maintain a healthy weight.
It is crucial to remember that each person responds differently to exercises, and it is essential to proceed with caution.
Examination of herniated disc
The gold standard for diagnosing a herniated disc is usually medical imaging, such as magnetic resonance imaging (MRI) or computed tomography (CT). These exams provide detailed images of the spine, intervertebral discs and surrounding structures, providing a precise view of the herniated disc and its impact on surrounding tissues.
1. Magnetic Resonance Imaging (MRI): MRI is commonly used to diagnose a herniated disc. This exam uses magnetic fields and radio waves to create detailed images of soft tissues, allowing precise visualization of the intervertebral discs, nucleus pulposus, annulus fibrosus, spinal cord and nerve roots. MRI can help determine the location, size and severity of the herniated disc.
2. Computed tomography (CT): CT is an imaging technique that uses x-rays to create detailed cross-sectional images of the spine. Although less common than MRI for diagnosing herniated discs, CT can be used to evaluate the bony structure of the spine and detect certain features of the herniated disc.
3. Radiography (XR): X-rays can be used to identify structural changes in the spine, such as bone spurs (osteophytes) or loss of disc height. However, they do not provide as detailed visualization of soft tissues as MRI.
4. Clinical Evaluation: Apart from medical imaging, clinical evaluation by a healthcare professional is also crucial. The doctor may take a detailed medical history, perform a physical examination, assess the patient’s symptoms, and perform neurological tests to determine the presence and severity of the herniated disc.
Living with Lumbar Disc Herniation: A Day in the Life”
Living with lumbar disc herniation presents a daily challenge that requires both physical and mental resilience. Lumbar disc herniation occurs when the intervertebral discs, which act as cushions between the vertebrae, become damaged and protrude, pressing on the spinal nerves. This condition can cause significant pain and discomfort, affecting a person’s ability to perform everyday tasks. Here’s a glimpse into a typical day for someone living with this condition.
Morning Routine
The day begins with the challenge of getting out of bed. Mornings can be particularly tough due to stiffness and pain that often peak after a night of inactivity. A gentle stretching routine is crucial to loosen up the muscles and reduce stiffness. Exercises like pelvic tilts, knee-to-chest stretches, and gentle yoga poses can help. Taking a warm shower also aids in relieving some of the morning discomfort by increasing blood flow and relaxing the muscles.
Preparing for the Day
After managing to get out of bed, dressing up can be another difficult task. Simple activities like bending down to put on socks or shoes can trigger intense pain. Using aids like a long-handled shoehorn or a sock aid can make this process easier. Choosing clothes that are easy to put on and take off can also reduce strain on the back.
Working with Lumbar Disc Herniation
For those who work, the type of job they have significantly affects their day. Office workers need to ensure their workspace is ergonomically friendly. Using an adjustable chair with proper lumbar support, positioning the computer screen at eye level, and taking regular breaks to stand up and stretch can help manage the pain. For those with physically demanding jobs, modifications might be necessary. This could include avoiding heavy lifting, using support belts, or seeking alternative tasks that are less strenuous on the back.
Daily Activities
Throughout the day, maintaining good posture is critical. Whether sitting, standing, or walking, keeping the spine in a neutral position helps reduce the strain on the herniated disc. Activities like cooking, cleaning, or even simple tasks like reaching for items on a shelf need to be done with caution. Bending at the knees rather than the waist, avoiding twisting motions, and using tools designed to reduce the need for bending can be beneficial.
Pain Management
Pain management is an ongoing task. Over-the-counter pain relievers like ibuprofen or acetaminophen can provide temporary relief. For more severe pain, prescription medications or corticosteroid injections might be necessary. Non-pharmacological approaches like heat or ice therapy, physical therapy, and alternative treatments such as acupuncture or chiropractic care can also play a significant role in managing pain and improving mobility.
Exercise and Physical Therapy
Regular exercise tailored to their condition is vital for those with lumbar disc herniation. Engaging in low-impact activities like walking, swimming, or using a stationary bike helps maintain overall fitness without placing undue stress on the back. Physical therapy sessions are essential as they provide specific exercises aimed at strengthening the core muscles, improving flexibility, and promoting proper posture.
Evening and Nighttime Routine
As the day winds down, unwinding with gentle stretches or relaxation techniques can help reduce the day’s accumulated tension. Using a lumbar support pillow while sitting and a proper mattress while sleeping ensures that the spine remains aligned. Finding a comfortable sleeping position, often on the back with a pillow under the knees or on the side with a pillow between the knees, is crucial for a good night’s rest.
Mental Health and Support
Living with chronic pain can take a toll on mental health. It’s important to address the emotional aspect of dealing with lumbar disc herniation. Joining support groups, talking to a therapist, or practicing mindfulness and relaxation techniques can help manage stress and anxiety. Staying connected with friends and family and communicating openly about the challenges can also provide emotional support and understanding.
Radiographic Signs of Lumbar Disc Herniation
Radiographic signs of a lumbar disc herniation can be seen on imaging tests such as x-rays, CT scans (computed tomography scans), or MRI scans (magnetic resonance imaging). However, it is important to note that radiographic signs do not always perfectly match clinical symptoms, and some people may experience herniated discs without experiencing significant symptoms. Here are some radiographic signs healthcare professionals can look for:
- Loss of Disc Height: A herniated disc can cause a decrease in the height of the affected intervertebral disc.
- Osteophytes (Bone Spurs): Osteophytes, or bone spurs, can form around the intervertebral discs in response to a herniated disc.
- Displacement of Surrounding Structures: A herniated disc can cause displacement of surrounding structures, including compression of nerve roots or spinal cord.
- Foramen Enlargement: The intervertebral foramen is the opening through which nerve roots exit the spine. A herniated disc can cause this opening to widen.
- Widening of the Spinal Canal: In some cases, a herniated disc can contribute to the widening of the spinal canal, leaving less space for the spinal cord.
- Joint Effusion: The presence of fluid around the joints may be an x-ray sign.
- MRI to Visualize Soft Tissues: MRI is particularly useful for visualizing soft tissues, including intervertebral discs, spinal cord, and nerve roots. It can show the precise location of the herniated disc and the impact on surrounding structures.
It is important to emphasize that the diagnosis of herniated disc is often based on a combination of clinical information, imaging studies, and neurological assessments.

Straightening of the lumbar spine with preserved alignment. Irregular margins of end plate L5. Decreased hydration of the L4-5 disc represented by reduced T2 hyperintensity of the disc.
L4-5 disc posterior bulge with central annular tear and protrusion indenting the ventral thecal sac, both obliterating the lateral recess and compressing the two exiting nerve roots.
Posterior L5-S1 disc bulging with left postlateral annular tear and protrusion indenting the ventral thecal sac, obliterating both the lateral cavity and compressing the two exiting nerve roots.
The nerve roots of Conus medullaris and cauda equina are normal. The pre- and paravertebral soft tissues are normal.
Conclusion
By diving into the complex anatomy of the lumbar spine and exploring the underlying mechanisms of herniated disc, we have unraveled the mysteries surrounding this dreaded spinal condition. The causes, symptoms and radiographic signs associated with lumbar disc herniation have been demystified, providing an in-depth understanding of this pathology.
The different phases of pathophysiology, from initial trauma to nerve root compression, have been described clearly and precisely. It is essential to note that lumbar disc herniation can be the result of various factors such as aging, wear and tear, repetitive movements, and even genetic predispositions.
The crucial role of the posterior longitudinal ligament in worsening symptoms was also explored, highlighting the importance of considering all of the anatomical structures involved in disc herniation.
In this quest for lasting relief, osteopathy emerges as a natural ally. Soft tissue techniques, cranial manipulations, visceral manipulations, and a holistic approach are all tools that osteopaths use to improve mobility, relieve pain, and restore balance.
Specific exercises and stretches, combined with lifestyle advice, complete the arsenal of osteopathy to help treat and prevent recurrence of lumbar disc herniation. Specific recommendations, such as posterior chain stretching and core strengthening exercises, add to the patient’s toolbox for proactive management of their spinal health.
Finally, radiographic signs were highlighted, emphasizing the importance of imaging examinations such as MRIs to precisely visualize the location of the herniated disc and its impact on surrounding structures.
In summary, this in-depth exploration of lumbar disc herniation offers valuable keys to understanding, managing and treating this complex condition. Through osteopathy and a holistic approach, lasting relief becomes a reality, paving the way to a better quality of life for those facing this spinal health challenge.
Quizz
Questionnaire (1)
1. What is the main cause of lumbar disc herniation according to the text?
a. Poor body mechanics
b. Aging
c. Genetics
d. Obesity
2. What are the common symptoms of lumbar disc herniation?
a. Lower back pain
b. Numbness and tingling
c. Muscle weakness
d. All previous choices
3. What is the main function of the intervertebral discs in the spine?
a. Support body weight
b. Produce stem cells
c. Control digestion
d. Regulate body temperature
4. How can lumbar disc herniation be diagnosed?
has. Radiography
b. MRI
v. Computed tomography (CT)
d. All previous choices
5. What is the gold standard examination method for diagnosing a herniated disc?
a. Radiography
b. MRI
c. Clinical assessment
d. CT
6. What are the possible radiographic signs of a lumbar disc herniation?
a. Loss of disc height
b. Osteophytes (bone spurs)
c. Displacement of surrounding structures
d. All previous choices
7. What is the inflammatory response associated with nerve root compression?
a. Improvement of symptoms
b. Intensification of symptoms
c. No impact
d. Temporary improvement
8. What are the potential benefits of osteopathy in the treatment of lumbar disc herniation?
a. Improved mobility
b. Pain relief
c. Muscle strengthening
d. All previous choices
9. What can make lumbar disc herniation symptoms worse?
a. Complete rest
b. Moderate physical activities
c. Prolonged sitting positions
d. No impact
10. What is the conclusion of the text on lumbar disc herniation?
a. Herniated disc has no effective treatment.
b. Osteopathy is a useless approach.
c. A multidisciplinary approach is necessary for effective management.
d. Traditional treatments are always the best.
Answers:
- b
- d
- a
- d
- b
- d
- b
- d
- c
- c
References
- Sharma SB, Kim JS. A Review of Minimally Invasive Surgical Techniques for the Management of Thoracic Disc Herniations. Neurospin. 2019 Mar;16(1):24-33. [ PMC free article ] [ PubMed ]2.
- Huang R, Meng Z, Cao Y, Yu J, Wang S, Luo C, Yu L, Xu Y, Sun Y, Jiang L. Nonsurgical medical treatment in the management of pain due to lumbar disc prolapse: A network meta-analysis. Semin Arthritis Rheum. 2019 Oct;49(2):303-313. [ PubMed ]3.
- Tang C, Moser FG, Reveille J, Bruckel J, Weisman MH. Cauda Equina Syndrome in Ankylosing Spondylitis: Challenges in Diagnosis, Management, and Pathogenesis. J Rheumatol. 2019 Dec;46(12):1582-1588. [ PubMed ]4.
- Park CH, Park ES, Lee SH, Lee KK, Kwon YK, Kang MS, Lee SY, Shin YH. Risk Factors for Early Recurrence After Transforaminal Endoscopic Lumbar Disc Decompression. Pain Physician. 2019 Mar;22(2):E133-E138. [ PubMed ]5.
- Huang JS, Fan BK, Liu JM. [Overview of risk factors for failed percutaneous transforaminal endoscopic discectomy in lumbar disc herniation]. Zhongguo Gu Shang. 2019 Feb 25;32(2):186-189. [ PubMed ]6.
- Fjeld OR, Grøvle L, Helgeland J, Småstuen MC, Solberg TK, Zwart JA, Grotle M. Complications, reoperations, readmissions, and length of hospital stay in 34,639 surgical cases of lumbar disc herniation. Bone Joint J. 2019 Apr;101-B(4):470-477. [ PubMed ]7.
- Jordan J, Konstantinou K, O’Dowd J. Herniated lumbar disc . BMJ Clin Evid. 2009 Mar 26;2009 [ PMC free article ] [ PubMed ]8.
- Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. The prevalence and clinical characteristics of internal disc disruption in patients with chronic low back pain. Spine (Phila Pa 1976). 1995 Sep 01;20(17):1878-83. [ PubMed ]9.
- Dydyk AM, Khan MZ, Singh P. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Oct 24, 2022. Radicular Back Pain. [ PubMed ]10.
- M Das J, Nadi M. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Mar 27, 2023. Lasegue Sign. [ PubMed ]11.
- Carlson BB, Albert TJ. Lumbar disc herniation: what has the Spine Patient Outcomes Research Trial taught us? Int Orthop. 2019 Apr;43(4):853-859. [ PubMed ]12.
- Hassan KZ, Sherman AL. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Jul 17, 2023. Epidural Steroids. [ PubMed ]13.
- Johnson SM, Shah LM. Imaging of Acute Low Back Pain. Radiol Clin North Am. 2019 Mar;57(2):397-413. [ PubMed ]14.
- Brazilian Medical Association. Silvinato A, Simões RS, Buzzini RF, Bernardo WM. Lumbar herniated disc treatment with percutaneous hydrodiscectomy. Rev Assoc Med Bras (1992). 2018 Sep;64(9):778-782. [ PubMed ]15.
- Harper R, Klineberg E. The evidence-based approach for surgical complications in the treatment of lumbar disc herniation. Int Orthop. 2019 Apr;43(4):975-980. [ PubMed ]16.
- Lavi ES, Pal A, Bleicher D, Kang K, Sidani C. Imaging of the Spine: Urgent and Emergent Indications. Semin Ultrasound CT MR. 2018 Dec;39(6):551-569. [ PubMed ]17.
- Alvin MD, Lubelski D, Alam R, Williams SK, Obuchowski NA, Steinmetz MP, Wang JC, Melillo AJ, Pahwa A, Benzel EC, Modic MT, Quencer R, Mroz TE. Spine Surgeon Treatment Variability: The Impact on Costs. Global Spine J. 2018 Aug;8(5):498-506. [ PMC free article ] [ PubMed ]18.
- Qaseem A, Wilt TJ, McLean RM, Forciea MA, Clinical Guidelines Committee of the American College of Physicians. Denberg TD, Barry MJ, Boyd C, Chow RD, Fitterman N, Harris RP, Humphrey LL, Vijan S. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017 Apr 04;166(7):514-530. [ PubMed ]19.
- Landau WM, Nelson DA, Armon C, Argoff CE, Samuels J, Backonja MM. Assessment: use of epidural steroid injections to treat radicular lumbosacral pain: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2007 Aug 07;69(6):614; author reply 614-5. [ PubMed ]20.
- Chou R, Hashimoto R, Friedly J, Fu R, Bougatsos C, Dana T, Sullivan SD, Jarvik J. Epidural Corticosteroid Injections for Radiculopathy and Spinal Stenosis: A Systematic Review and Meta-analysis. Ann Intern Med. 2015 Sep 01;163(5):373-81. [ PubMed ]21.
- Chou R, Loeser JD, Owens DK, Rosenquist RW, Atlas SJ, Baisden J, Carragee EJ, Grabois M, Murphy DR, Resnick DK, Stanos SP, Shaffer WO, Wall EM., American Pain Society Low Back Pain Guideline Panel. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: an evidence-based clinical practice guideline from the American Pain Society. Spine (Phila Pa 1976). 2009 May 01;34(10):1066-77. [ PubMed ]22.
- Amlie E, Weber H, Holme I. Treatment of acute low-back pain with piroxicam: results of a double-blind placebo-controlled trial. Spine (Phila Pa 1976). 1987 Jun;12(5):473-6. [ PubMed ]23.
- Schoenfeld AJ, Weiner BK. Treatment of lumbar disc herniation: Evidence-based practice. Int J Gen Med. 2010 Jul 21;3:209-14. [ PMC free article ] [ PubMed ]24.
- Buttermann GR. Treatment of lumbar disc herniation: epidural steroid injection compared with discectomy. A prospective, randomized study. J Bone Joint Surg Am. 2004 Apr;86(4):670-9. [ PubMed ]