Introduction
Osteochondritis dissecans of the elbow is a medical condition that affects the articular cartilage and subchondral bone of the elbow. This condition is characterized by the formation of lesions or detached fragments in the joint region of the elbow, which can lead to pain, limitation of movement and, in severe cases, long-term complications. Understanding the key aspects of this pathology is essential for the clinical management and well-being of affected patients.
This condition is often attributed to repetitive strain injuries, which can be caused by specific sporting activities. Studies indicate that sports such as racquetball, baseball, weight training, cheerleading, and competitive gymnastics are often associated with the development of osteochondritis dissecans of the elbow. Young male athletes, in particular, seem to be more predisposed to this condition, and it is common to see a predominance of the involvement on the dominant elbow.
One of the fundamental characteristics of osteochondritis dissecans is the presence of repetitive microtrauma that leads to disruption of vascularization to the cartilage and supporting structures of the elbow. These microtraumas can cause local ischemia, leading to separation of articular cartilage and subchondral bone. This separation results in the formation of lesions and, in some cases, fragments of detached cartilage.
Symptoms of osteochondritis dissecans of the elbow are varied but usually include persistent pain when using the affected elbow. The pain is often described as deep, dull and ill-defined. It may be accompanied by rubbing or cracking sensations when the elbow is flexed or extended, particularly in the presence of mobile joint fragments. It is common for pain to decrease with rest, sometimes leading patients to downplay their symptoms.
A peculiarity of this condition is the frequent presence of free bodies in the elbow joint. These loose fragments of cartilage can cause additional discomfort, grinding, and even locking of the joint, thereby limiting mobility and affecting the patient’s quality of life. Bilateral cases, although less common, have also been documented.
The diagnosis of osteochondritis dissecans of the elbow is based on a thorough clinical evaluation, x-rays, magnetic resonance imaging (MRI) scans, and sometimes arthroscopies. These tools allow healthcare professionals to assess the extent of injuries, the presence of joint fragments and other abnormalities.
Management of osteochondritis dissecans of the elbow depends on the severity of the symptoms and lesions. In mild cases, conservative approaches such as rest, osteopathy and pain management may be considered. However, in more severe cases, especially when there are loose joint fragments, surgery may be necessary to remove the fragments, repair the damage, or stabilize the joint.
In conclusion, osteochondritis dissecans of the elbow is a complex medical condition that often results from repetitive microtrauma associated with specific sports activities. Understanding risk factors, symptoms and treatment options is essential to ensure adequate management of this condition, thereby improving patients’ quality of life and minimizing long-term complications. Multidisciplinary approaches involving healthcare professionals such as orthopedists, radiologists and osteopaths are often necessary for optimal treatment.
Causes of Osteochondritis dissecans of the elbow
The causes of osteochondritis dissecans (OCD) of the elbow encompass a combination of biomechanical, traumatic, and genetic factors that contribute to the development and progression of this debilitating condition. One primary cause is repetitive microtrauma and overuse of the elbow joint, particularly in athletes engaged in sports that involve repetitive throwing, such as baseball, softball, tennis, and gymnastics. The repetitive stress placed on the elbow during overhead throwing motions can lead to compression and shear forces within the joint, disrupting blood supply to the subchondral bone and cartilage, and predisposing individuals to the development of OCD lesions. Additionally, traumatic injuries, such as acute elbow sprains, fractures, or dislocations, can disrupt the blood flow to the articular cartilage and subchondral bone, leading to ischemia, necrosis, and subsequent OCD lesion formation. These traumatic events may occur during sports-related activities, accidental falls, or direct blows to the elbow, further exacerbating the risk of OCD development.
Structural abnormalities and anatomical variations within the elbow joint can also contribute to the pathogenesis of OCD, predisposing individuals to abnormal joint loading and increased susceptibility to cartilage and bone injuries. For example, congenital abnormalities, such as osteochondral defects, loose bodies, or incongruities in the joint surfaces, may alter the distribution of forces across the elbow joint, leading to focal areas of increased stress and vulnerability to OCD lesion formation. Additionally, genetic factors, including hereditary predispositions to osteochondral disorders and connective tissue abnormalities, may influence the development and progression of OCD, though the specific genetic mechanisms underlying OCD remain poorly understood.
Metabolic factors, such as hormonal imbalances and nutritional deficiencies, may also play a role in the pathogenesis of OCD by affecting the overall health and integrity of the articular cartilage and subchondral bone. Hormonal changes, such as those occurring during puberty or pregnancy, can influence bone metabolism and growth plate development, potentially impacting the susceptibility to OCD lesions in adolescents and young adults. Furthermore, nutritional deficiencies in vitamins and minerals essential for bone health, such as vitamin D, calcium, and magnesium, may compromise the structural integrity of the bone and cartilage, increasing the risk of OCD development and progression.
Moreover, inflammatory conditions, such as juvenile idiopathic arthritis (JIA) or systemic lupus erythematosus (SLE), can affect the elbow joint and predispose individuals to the development of OCD lesions. Inflammatory arthritis conditions can lead to synovial inflammation, cartilage degradation, and subchondral bone erosions, resulting in secondary OCD lesions within the affected joint. Additionally, systemic inflammatory processes may disrupt the normal healing and remodeling processes within the bone and cartilage, further exacerbating the risk of OCD development and complicating the management of the condition. Overall, the causes of OCD of the elbow are multifactorial, involving a complex interplay of biomechanical, traumatic, genetic, metabolic, and inflammatory factors that contribute to the pathogenesis of this challenging orthopedic condition.
Osteochondritis dissecans of the elbow has multifactorial origins, and although the precise cause is not always clear, several factors may contribute to the development of this condition. Here are some of the potential causes of osteochondritis dissecans of the elbow:
- Repetitive microtrauma: The most frequently cited cause is exposure to repetitive microtrauma, particularly in the context of specific sporting activities. Repetitive movements of the elbow, associated with sports like racquetball, baseball, weight training, cheerleading, and competitive gymnastics, can place excessive strain on the elbow joint, leading to damage to the cartilage and bone underneath. -chondral.
- Genetic factors: Some individuals may have a genetic predisposition to developing joint problems such as osteochondritis dissecans. Studies suggest that there may be a genetic component increasing susceptibility to this type of pathology.
- Vascular problems: Disruption of blood supply to the articular cartilage and subchondral bone can play a crucial role. Vascular problems, such as local ischemia, may be associated with the development of osteochondritis dissecans.
- Acute trauma: Although the condition is often linked to repetitive microtrauma, acute trauma, such as direct injuries or impacts to the elbow, can also contribute to the development of osteochondritis dissecans.
- Growth Disorders: In young patients, growth disorders may also be a contributing factor. Incomplete ossification or irregularities in cartilage development can increase vulnerability to this type of joint problem.
- Mechanical Stress: Repetitive movements, excessive loads or strenuous physical activities can place significant mechanical stress on the elbow joint, increasing the risk of developing osteochondritis dissecans.
- Dysplasia: Structural abnormalities of the joint, such as dysplasia, can predispose to uneven stress on the cartilage and contribute to the development of osteochondritis dissecans.
Symptoms of Osteochondritis dissecans of the elbow
Symptoms of osteochondritis dissecans (OCD) of the elbow typically manifest gradually and worsen over time, reflecting the progressive nature of this orthopedic condition. One primary symptom experienced by individuals with OCD of the elbow is persistent pain, localized to the inner or outer aspect of the elbow joint. This pain may be dull and achy in nature, initially occurring during activities that stress the elbow, such as lifting, gripping, or throwing, and gradually worsening with continued use of the affected arm. Additionally, pain may be elicited by specific movements or positions of the elbow, such as fully extending or flexing the joint, and may be accompanied by swelling, tenderness, and warmth over the affected area, indicative of inflammation and joint irritation.
Functional impairment is a hallmark symptom of OCD of the elbow, impacting the individual’s ability to perform activities of daily living and participate in sports or recreational activities that require repetitive or forceful use of the elbow joint. Reduced range of motion, stiffness, and instability in the elbow are commonly reported, as the presence of loose or detached osteochondral fragments within the joint can interfere with smooth joint movement and cause mechanical symptoms, such as locking, catching, or clicking sensations during elbow motion. Furthermore, individuals may experience weakness and muscle atrophy in the affected arm, as pain and functional limitations limit their ability to engage in physical activity and maintain muscle strength and tone.
Moreover, symptoms of OCD of the elbow may vary depending on the severity and location of the osteochondral lesion within the joint. In early stages of the disease, individuals may experience intermittent pain and stiffness that resolve with rest and activity modification, making it challenging to diagnose the condition based solely on clinical symptoms. However, as the condition progresses and the osteochondral lesion worsens, symptoms may become more persistent and debilitating, with pain occurring even at rest and during nighttime hours, disrupting sleep and affecting overall quality of life. Additionally, individuals may notice a decrease in grip strength and coordination, as well as difficulty performing tasks that require fine motor control or precision, such as writing, typing, or buttoning clothing.
Furthermore, symptoms of OCD of the elbow can have a significant impact on psychosocial well-being, leading to frustration, anxiety, and depression as individuals struggle to cope with chronic pain and functional limitations. Sleep disturbances, mood changes, and social withdrawal may occur as a result of ongoing pain and disability, further exacerbating the overall burden of the condition on the individual. Overall, the symptoms of OCD of the elbow encompass a spectrum of physical, functional, and psychosocial manifestations, highlighting the importance of early recognition, accurate diagnosis, and comprehensive management strategies aimed at addressing the underlying causes of pain and dysfunction while optimizing patient outcomes and quality of life.
- Joint pain: Pain in the elbow is one of the most characteristic symptoms of osteochondritis dissecans. This pain is often described as deep, dull and ill-defined. It may be felt during or after activities that put strain on the elbow, such as sports or repetitive movements.
- Pain on exertion: Pain in the elbow is generally exacerbated during use of the joint, particularly when practicing physical activities or specific movements requiring the elbow.
- Decreased pain at rest: A characteristic feature of osteochondritis dissecans is decreased pain at rest. Patients often find that the pain improves significantly when the elbow is at rest.
- Rubbing or cracking sensations: In the presence of detached joint fragments, movement of the elbow can cause rubbing or cracking sensations. Patients may experience these sensations when flexing or extending the joint.
- Joint stiffness: Some individuals with osteochondritis dissecans may experience joint stiffness, particularly after a prolonged period of rest.
- Swelling: Mild swelling can sometimes be seen around the elbow joint, particularly in response to inflammation caused by cartilage damage and joint fragments.
- Limitation of mobility: The presence of free bodies in the joint, or the lesions themselves, can lead to limited mobility of the elbow. Some movements may become difficult or painful.
- Tenderness to palpation: The affected area of the elbow may be tender to the touch. Palpation of the joint can trigger or worsen the pain.
- Locking sensations: In the presence of joint fragments, some patients may experience locking or instability sensations during elbow movements.
Pathophysiology
The pathophysiology of osteochondritis dissecans of the elbow involves complex mechanisms that lead to the separation of articular cartilage and subchondral bone. Although the precise details may vary from individual to individual, here is a general description of the processes involved in the development of this condition:
- Repetitive microtrauma: One of the predominant factors in the pathophysiology of osteochondritis dissecans of the elbow is exposure to repetitive microtrauma. These strain injuries typically result from specific sports activities or repetitive movements of the elbow, such as those associated with racquetball, baseball, weight training, cheerleading, and competitive gymnastics.
- Ischemia and disruption of vascularization: Repetitive microtrauma can disrupt the normal vascularization of the cartilage and supporting structures of the elbow. This disruption leads to local ischemia, i.e. a reduction in blood flow to the affected area.
- Impaired cartilage metabolism: Ischemia causes disruption of cartilage metabolism, compromising its ability to regenerate and maintain its structural integrity. The cartilage becomes more vulnerable to damage.
- Separation of cartilage and subchondral bone: Due to disruption of vascularity and metabolic alteration, separation of articular cartilage and subchondral bone occurs. This separation can manifest itself by the formation of lesions in the cartilage, sometimes associated with detached joint fragments.
- Inflammatory response: Separation of cartilage can trigger a local inflammatory response, contributing to pain, swelling, and other symptoms associated with osteochondritis dissecans.
- Free body formation: Cartilage damage and loose fragments can result in free bodies in the elbow joint. These loose bodies can lead to blockages, rubbing sensations, and other symptoms described by patients.
Diagnosis and treatment
Diagnostic
Diagnosis of osteochondritis dissecans of the elbow is based on a combination of clinical assessment, medical imaging, and sometimes more invasive procedures. Here are the steps commonly involved in diagnosis:
- History and Clinical Examination: The doctor will collect the patient’s medical history, paying particular attention to symptoms, injury history, and physical activities. A physical examination, including palpation of the elbow joint, will assess pain, mobility, and the possible presence of loose bodies.
- Medical imaging :
- X-rays: X-rays help visualize bony structures and can reveal early signs of osteochondritis dissecans, such as cartilage damage or loose joint fragments.
- MRI (Magnetic Resonance Imaging): MRI is often more sensitive in detecting cartilage damage and providing detailed information on the extent of the damage.
- Arthroscopy: In some cases, arthroscopy, a minimally invasive surgical procedure, may be performed. This involves inserting a small camera through small incisions to directly view the inside of the joint and confirm the diagnosis while allowing for simultaneous therapeutic interventions.
Treatment
The choice of treatment depends on the severity of symptoms, the extent of lesions and other individual factors. Approaches can vary from conservative measures to more invasive surgical procedures:
- Rest and Activity Modification: Reducing activities that put strain on the elbow and taking relative rest can help relieve symptoms and allow healing. Changing movement habits may also be recommended.
- Osteopathy: Osteopathy aims to strengthen surrounding muscles, improve mobility and promote healing. Specific exercises may be prescribed to stabilize the elbow joint.
- Medications: Pain relievers and nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to relieve pain and reduce inflammation.
- Intra-Articular Injections: Corticosteroid injections may be considered to reduce inflammation in the joint.
- Surgery :
- Arthroscopy Debridement: When there are joint fragments present, arthroscopy may be used to remove these fragments and debride the lesions.
- Fixation or Grafting: In more severe cases, surgical procedures such as fragment fixation or cartilage grafting may be necessary to restore the integrity of the joint.
- Post-Surgical Rehabilitation: After surgery, a period of rehabilitation supervised by an osteopath is often recommended to restore muscle strength, mobility and function of the joint.
Diagnostic differentiel
The differential diagnosis of osteochondritis dissecans of the elbow involves the exclusion of other medical conditions with similar symptoms. Here are some of the conditions that may be considered when evaluating a patient with elbow pain and other associated symptoms:
- Epicondylitis (Tennis Elbow or Golfer’s Elbow): Inflammation of the tendons at the origin or insertion of the elbow, known as lateral (tennis elbow) or medial (golfer’s elbow) epicondylitis, can cause pain in the elbow. elbow. However, unlike osteochondritis dissecans, these conditions primarily involve the tendons rather than the cartilage.
- Elbow Bursitis: Inflammation of the bursa near the elbow can cause pain and swelling. Bursitis can be caused by repetitive movements or trauma, but it usually does not directly involve cartilage or loose joint fragments.
- Elbow Arthritis: Inflammatory arthritis, such as rheumatoid arthritis, or osteoarthritis, can also affect the elbow. These conditions can cause joint pain, stiffness, and inflammation. Radiographic changes and clinical features can help differentiate these conditions from osteochondritis dissecans.
- Elbow Fractures: Elbow fractures, especially those involving the joint surface, can cause similar symptoms, including pain, swelling, and limitations in mobility. Imaging, such as x-rays, can help distinguish fractures from osteochondritis dissecans.
- Joint Infection: Infections of the elbow joint can cause pain, swelling and inflammation. The presence of fever and other signs of infection can help differentiate this condition from osteochondritis dissecans.
- Bone or Joint Tumors: Although less common, bone or joint tumors can cause similar symptoms. Medical imaging, such as MRI, can be crucial in assessing the nature of the lesions.
- Cubital Tunnel Syndrome: Compression of the ulnar nerve in the elbow area can cause symptoms such as pain, numbness, and weakness. However, this is not a joint condition, but rather nerve damage.
Radiographic signs
Radiographic signs of osteochondritis dissecans of the elbow may vary depending on the severity of the lesions and the stage of the disease. Radiographs are often one of the first imaging modalities used to evaluate changes in the elbow joint. Here are some radiographic signs that may be observed:
- Cartilage Damage: X-rays may reveal signs of articular cartilage damage. Areas of irregularity or loss of joint space may be visible, indicating damage to the cartilage.
- Bone Fragmentation: In more advanced cases, bone fragments detached from the joint surface may be visible on x-rays. These fragments, called “loose bodies” or “intra-articular foreign bodies,” are pieces of bone or cartilage that have broken away and may float within the joint.
- Separation of Bone Fragment: When bone fragments are present, the x-ray may show clear separation of these fragments from the underlying bone bed. This separation is characteristic of advanced cases of osteochondritis dissecans.
- Joint Line Thickening: In some cases, an increase in joint line thickness may be observed, indicating an inflammatory response or the presence of scar tissue.
- Joint Swelling: X-rays may show signs of joint swelling or swelling, although MRI is often more sensitive in detecting these changes.
- Signs of Early Osteoarthritis: In untreated chronic cases, signs of early osteoarthritis, such as the formation of osteophytes (bone spurs) or reduction in joint space, may be observed.

A well-defined ossifying structure is seen in the center of the olecranon fossa, measuring approximately 15 mm in diameter, with several adjacent smaller ossifying fragments that are more irregular in appearance.
The anterior fat pad is not elevated.
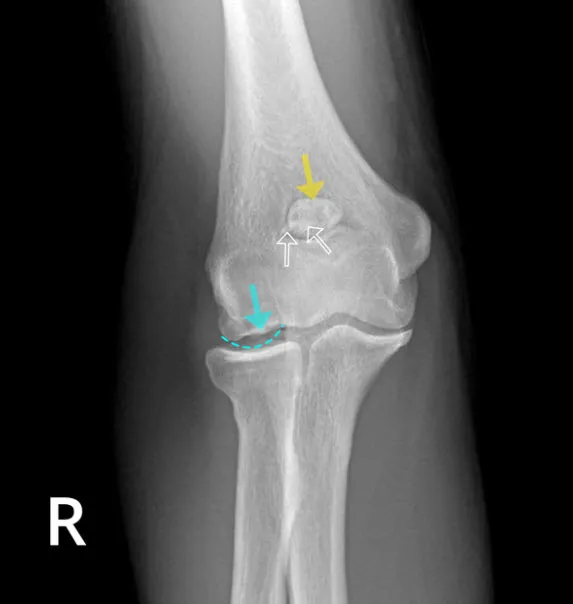
The yellow arrow points to the ossicle, which appears to represent a normal variant ossicle, but the other two bone fragments (open white arrows) suggest that this is degenerative (secondary) synovial osteochondromatosis. Case courtesy of Matt Skalski, Radiopaedia.org . From the case rID: 31759
Conclusion
In conclusion, osteochondritis dissecans of the elbow is an orthopedic condition that often results from repetitive microtrauma affecting the articular cartilage and subchondral bone of the elbow joint. This condition can cause symptoms such as pain, limited mobility, rubbing sensations, and joint loose bodies. It is more common in young athletes, particularly those practicing sports that put intensive strain on the elbow.
The diagnosis of osteochondritis dissecans involves a multidisciplinary approach, combining history, clinical examination, and radiological investigations such as x-rays and MRI. Treatment varies depending on the severity of symptoms, ranging from conservative measures like rest and physical therapy to surgical interventions to stabilize the joint and repair damage.
Regular medical follow-up, supervised post-surgical rehabilitation, and possible lifestyle adaptations can help improve the quality of life of affected individuals. It is also crucial to perform a differential diagnosis to rule out other conditions with similar symptoms.
Ultimately, a personalized approach, tailored to the severity of the disease and the specific needs of each patient, is essential to ensure effective management of osteochondritis dissecans of the elbow and to minimize long-term impacts on joint health. Close collaboration between healthcare professionals, including orthopedists, osteopaths and radiologists, is fundamental to achieving optimal results in the management of this condition.
References
- Konig F, The classic The classic: on loose bodies in the joint. Clin Orthop Relat Res. 2013;471(4):1107–15. doi: 10.1007/s11999-013-2824-y. – DOI – PMC – PubMed
- Edmonds EW, Polousky J. A review of knowledge in osteochondritis dissecans: 123 years of minimal evolution from Konig to the ROCK study group. Clin Orthop Relat Res. 2013;471(4):1118–26. doi: 10.1007/s11999-012-2290-y. – DOI – PMC – PubMed
- Nissen CW. Osteochondritis dissecans of the elbow. Clin Sports Med. 2014;33(2):251–65. doi: 10.1016/j.csm.2013.11.002. – DOI – PubMed
- Jones KJ, et al. Arthroscopic management of osteochondritis dissecans of the capitellum: mid-term results in adolescent athletes. J Pediatr Orthop. 2010;30(1):8–13. doi: 10.1097/BPO.0b013e3181c3be83. – DOI – PubMed
- Shimada K, et al. Cylindrical costal osteochondral autograft for reconstruction of large defects of the capitellum due to osteochondritis dissecans. J Bone Joint Surg Am. 2012;94(11):992–1002. doi: 10.2106/JBJS.J.00228. – DOI – PMC – PubMed
- Ahmad CS, Vitale MA, ElAttrache NS. Elbow arthroscopy: capitellar osteochondritis dissecans and radiocapitellar plica. Instr Course Lect. 2011;60:181–90. – PubMed
- Baker CL, 3rd, Romeo AA, Baker CL., Jr Osteochondritis dissecans of the capitellum. Am J Sports Med. 2010;38(9):1917–28. doi: 10.1177/0363546509354969. – DOI – PubMed
- Ahmad CSENS. Treatment of capitellar osteochondritis dissecans. Techniques in Shoulder and Elbow Surgery. 2006;7(4):169–74. doi: 10.1097/01.bte.0000235401.59599.31. – DOI
- Tis JE, et al. Short-term results of arthroscopic treatment of osteochondritis dissecans in skeletally immature patients. J Pediatr Orthop. 2012;32(3):226–31. doi: 10.1097/BPO.0b013e31824afeb8. – DOI – PubMed
- Zlotolow DA, Bae DS. Osteochondral autograft transplantation in the elbow. J Hand Surg [Am] 2014;39(2):368–72. doi: 10.1016/j.jhsa.2013.09.003. – DOI – PubMed
- Schub DL, et al. Mapping of cartilage depth in the knee and elbow for use in osteochondral autograft procedures. Am J Sports Med. 2013;41(4):903–7. doi: 10.1177/0363546513475343. – DOI – PubMed
- Claessen FM et al., Osteochondritis dissecans of the humeral capitellum: reliability of four classification systems using radiographs and computed tomography. J Shoulder Elbow Surg. 2015. Demonstrated that radiographic findings have poor to fair interobserver reliability and that MRI is needed for cases of osteochondritis dissecans of the capitellum. – PubMed
- Lewine EB et al. Early results of drilling and/or microfracture for grade IV osteochondritis dissecans of the capitellum. J Pediatr Orthop. 2015. – PubMed
- Uchida S, et al. Arthroscopic fragment fixation using hydroxyapatite/poly-L-lactate acid thread pins for treating elbow osteochondritis dissecans. Am J Sports Med. 2015;43(5):1057–65. doi: 10.1177/0363546515570871. – DOI – PubMed
- Maruyama M, et al. Outcomes of an open autologous osteochondral plug graft for capitellar osteochondritis dissecans: time to return to sports. Am J Sports Med. 2014;42(9):2122–7. doi: 10.1177/0363546514538759. – DOI – PubMed
- Kida Y, et al. Prevalence and clinical characteristics of osteochondritis dissecans of the humeral capitellum among adolescent baseball players. Am J Sports Med. 2014;42(8):1963–71. doi: 10.1177/0363546514536843. – DOI – PubMed
- Mihata T, et al. Biomechanical characteristics of osteochondral defects of the humeral capitellum. Am J Sports Med. 2013;41(8):1909–14. doi: 10.1177/0363546513490652. – DOI – PubMed
- Miyake J, et al. In-vivo biomechanical analysis of osteochondritis dissecans of the humeral trochlea: a case report. J Pediatr Orthop B. 2013;22(4):392–6. doi: 10.1097/BPB.0b013e32835f5821. – DOI – PubMed
- Greiwe RM, Saifi C, Ahmad CS. Pediatric sports elbow injuries. Clin Sports Med. 2010;29(4):677–703. doi: 10.1016/j.csm.2010.06.010. – DOI – PubMed