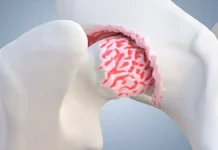
A bone spur, also called osteophyte, manifests itself as a bony outgrowth resulting from overload at the attachment of a tendon or ligament to a bone.
Synonym: exostosis
Introduction
A bone spur, also known as an osteophyte, is a bony outgrowth that develops on the edges of bones. These spurs typically form in response to prolonged stress, pressure, or friction on a particular bone or joint. While they can occur in various parts of the body, common locations include joints in the spine, knees, hips, shoulders, and hands. Bone spurs are often associated with conditions like osteoarthritis, where the protective cartilage covering the ends of bones wears down over time. As the cartilage breaks down, the body may attempt to compensate by forming these bony projections, leading to the development of bone spurs. Additionally, aging plays a significant role in the formation of bone spurs, as the wear and tear on joints over the years can contribute to their growth. Injuries, joint instability, or inflammation can also trigger the formation of bone spurs. While many people may have bone spurs without experiencing any symptoms, these outgrowths can cause issues if they impinge on nearby nerves or affect joint movement. Common symptoms include pain, stiffness, and reduced range of motion in the affected joint.
Diagnosis often involves imaging tests such as X-rays, which can reveal the presence and size of bone spurs. Treatment options vary depending on the severity of symptoms and may include pain management, physical therapy, and anti-inflammatory medications. In more severe cases, where bone spurs significantly impact daily life, surgical intervention might be considered to remove or address the spurs. It’s important to note that preventive measures such as maintaining a healthy weight, staying physically active, and addressing joint injuries promptly can contribute to minimizing the risk of developing bone spurs. While bone spurs are a common occurrence, their management requires a comprehensive approach that considers the underlying causes, the specific location of the spurs, and the individual’s overall health. Seeking medical advice for proper diagnosis and treatment is crucial to address any symptoms and prevent potential complications associated with bone spurs.
Pathophysiology of bone spur formation
The pathophysiology of bone spur formation is an area of study aimed at understanding the underlying mechanisms that lead to the creation of these bony outgrowths. This condition often results from complex pathological processes within the joints, particularly when factors such as joint wear and tear, trauma, chronic inflammation, or mechanical abnormalities are present.
When a joint is subjected to mechanical overload or abnormal stresses, the body reacts by initiating regeneration or stabilization processes. In the case of bone spur formation, these processes can be exacerbated, leading to the growth of osteophytes on bone surfaces.
Osteoarthritis, a common form of joint wear and tear associated with aging, is often associated with bone spur formation. The degenerative process of osteoarthritis leads to a loss of articular cartilage, prompting the body to attempt to compensate for this loss by forming osteophytes. These growths can create problems by interfering with the normal movement of joints, causing pain, stiffness, or other symptoms.
Other factors, such as previous joint trauma, inflammatory diseases, or mechanical imbalances, may also contribute to the pathophysiology of bone spur formation. A thorough understanding of these pathological mechanisms is crucial for developing effective treatment approaches aimed at alleviating symptoms and improving the quality of life of those affected by this condition.
- Triggering Factors: Pathophysiology often begins with triggering factors such as joint wear and tear, trauma, chronic inflammation, or other underlying medical conditions.
- Joint Wear (Osteoarthritis): Osteoarthritis, characterized by the degradation of articular cartilage, is one of the main causes. Cartilage wear exposes bone surfaces, prompting the body to respond.
- Inflammatory Response: In response to wear and exposure of bone surfaces, an inflammatory response occurs in the joint. Inflammatory cells are recruited to attempt to repair the damage.
- Osteophyte Formation: The inflammatory response stimulates the formation of osteophytes, bony growths that emerge from the edges of bones adjacent to the affected joint. These growths are the body’s attempt to stabilize the joint and compensate for the loss of cartilage.
- Bone Strengthening: Osteophytes can act as a strengthening mechanism for damaged bone by providing additional surface area and redistributing the load on the joint.
- Complications and Symptoms: However, these bony growths can also cause complications. They can interfere with the normal movement of the joint, causing pain, stiffness, decreased mobility, and even damage to surrounding tissues.
- Adaptive Response of the Body: Ultimately, bone spur formation can be considered as an adaptive response of the body to stressful or pathological conditions in the joint. It represents an attempt at stabilization and repair, although this response can lead to symptoms and functional limitations.
Causes bone formation
One of the main causes is osteoarthritis, a degenerative joint disease that leads to cartilage deterioration. When cartilage wears away, bones can rub directly against each other, which stimulates the growth of bone spurs in response to this constant friction. Additionally, repetitive trauma, such as that caused by high-impact sports activities or repetitive motions, can also trigger the formation of bone spurs.
Age also plays an important role, as joints tend to wear out naturally over time. As people age, the body’s ability to maintain and repair cartilage decreases, promoting the growth of bone spurs. Genetic factors can also influence the propensity to develop bone spurs, with some people being more predisposed due to their genetic heritage.
Additionally, medical conditions such as rheumatoid arthritis, which causes joint inflammation, can contribute to the formation of bone spurs. Chronic inflammation can stimulate abnormal bone growth in response to the inflammatory process. Likewise, other underlying medical conditions, such as metabolic disorders, may play a role in the development of bone spurs.
- Joint wear (Osteoarthritis): Osteoarthritis is one of the main causes of bone spurs. It is characterized by the breakdown of articular cartilage, which results in a response by the body aimed at stabilizing the joint by forming osteophytes.
- Mechanical overload: Constant overload or repetitive movements can cause excessive wear and tear on joints, prompting the body to develop osteophytes to strengthen weakened structures.
- Age: Natural aging of the body can contribute to bone spur formation. Over time, joints can experience normal wear and tear, increasing the risk of developing osteophytes.
- Joint trauma: Joint injuries, such as sprains or fractures, can stimulate bone spur formation in response to the body’s attempt to repair injured tissue.
- Joint instability: Chronic joint instability, often due to ligament problems, can promote the development of osteophytes as a stabilizing mechanism.
- Chronic Inflammation: Chronic inflammatory diseases, such as rheumatoid arthritis, can contribute to bone spur formation due to constant joint inflammation.
- Mechanical dysfunction: Structural abnormalities or joint misalignment can lead to uneven load distribution, increasing the risk of bone spur formation.
- Metabolic Diseases: Certain metabolic conditions, such as gout, can promote bone spur formation due to crystal deposits in the joints.
- Heredity: Some individuals may be genetically predisposed to developing bone spurs due to hereditary factors.
Risk Factors
Understanding the Risk Factors for Bone Spurs
Bone spurs, or osteophytes, are bony projections that form along the edges of bones, often within joints. While they can develop in various parts of the body, their formation is influenced by several risk factors that increase the likelihood of their occurrence. Understanding these risk factors is essential for identifying those at higher risk and implementing preventive measures.
One of the primary risk factors for bone spur development is age. As we age, the wear and tear on our joints accumulate, leading to the degeneration of cartilage that cushions the bones. Over time, the body may respond to this cartilage loss by forming bone spurs to stabilize the affected joints. This is particularly common in conditions like osteoarthritis, where the protective cartilage wears down, prompting the body to create these bony outgrowths. Consequently, individuals over the age of 60 are at a higher risk of developing bone spurs.
Obesity is another significant risk factor. Excess body weight places additional stress on weight-bearing joints such as the knees, hips, and spine. This increased pressure accelerates joint wear and tear, potentially leading to the formation of bone spurs. Furthermore, obesity is often associated with a sedentary lifestyle, which can contribute to joint instability and further exacerbate the risk.
Repetitive stress or trauma to the joints is also a key factor in bone spur formation. Certain occupations, such as construction work or jobs that involve repetitive movements, can place continuous strain on specific joints. Similarly, athletes who engage in high-impact sports like running, football, or ballet are prone to developing bone spurs due to the repetitive stress and minor injuries their joints endure over time.
Genetic predisposition plays a role as well. Some individuals may inherit a tendency to develop bone spurs due to their genetic makeup. If there is a family history of osteoarthritis or other joint-related conditions, the likelihood of developing bone spurs may be higher.
Joint injuries, such as sprains or fractures, can also trigger the formation of bone spurs. When a joint is injured, the body’s natural healing process may result in the formation of excess bone as it attempts to repair the damage. Over time, this can lead to the development of bone spurs, particularly if the joint remains unstable or if the injury causes chronic inflammation.
Chronic inflammatory conditions, such as rheumatoid arthritis, can contribute to bone spur formation as well. In these conditions, ongoing inflammation in the joints can stimulate abnormal bone growth. The presence of systemic inflammation can also exacerbate other risk factors, further increasing the likelihood of bone spur development.
Finally, certain metabolic disorders, such as diabetes, can increase the risk of bone spurs. These conditions often affect the body’s ability to repair and maintain joint tissues, leading to an increased risk of joint degeneration and subsequent spur formation.
Prevention
How to Prevent Bone Spurs: Tips and Strategies
Bone spurs, or osteophytes, are common, especially as people age, but certain preventive measures can help reduce the risk of their development. By adopting healthy lifestyle practices and being mindful of joint health, individuals can minimize the likelihood of bone spur formation and maintain better overall joint function.
One of the most effective ways to prevent bone spurs is by maintaining a healthy weight. Excess body weight places additional stress on weight-bearing joints, such as the knees, hips, and spine. Over time, this increased pressure can accelerate the wear and tear on cartilage, leading to the development of bone spurs. By maintaining a healthy weight through a balanced diet and regular exercise, individuals can reduce the strain on their joints and lower their risk of spur formation.
Regular physical activity is also crucial for preventing bone spurs. Engaging in low-impact exercises, such as swimming, walking, or cycling, helps to keep joints flexible and strengthens the muscles around them, providing better support and reducing the risk of injury. Exercise also promotes healthy circulation, which is essential for maintaining joint health and preventing the deterioration that can lead to bone spur formation.
Stretching exercises are particularly beneficial in preventing bone spurs. Stretching helps maintain the flexibility of tendons, ligaments, and muscles, which in turn supports joint health. Regular stretching can prevent stiffness and reduce the risk of injury during physical activities. It is especially important for individuals who engage in repetitive motions, whether through sports or work, as it helps to counterbalance the stress placed on specific joints.
Proper footwear is another important factor in preventing bone spurs, particularly for those prone to developing spurs in the feet. Wearing shoes that provide adequate support and cushioning can reduce the impact on foot joints and help prevent the overuse injuries that lead to spur formation. Orthotic inserts may also be beneficial for individuals with specific foot issues, such as flat feet or high arches, as they help distribute weight more evenly across the foot and reduce joint stress.
Joint protection techniques are essential for individuals in occupations or sports that involve repetitive movements or heavy lifting. Using proper techniques, such as lifting with the legs instead of the back, can reduce the strain on joints and prevent injuries that could lead to bone spur formation. Additionally, incorporating regular breaks and varying movements can help minimize repetitive stress on the joints.
Managing chronic conditions, such as osteoarthritis or rheumatoid arthritis, is crucial for preventing bone spurs. Regular check-ups with a healthcare provider, following prescribed treatments, and making lifestyle adjustments can help manage these conditions and reduce the risk of spur formation. Anti-inflammatory medications, physical therapy, and other interventions may be necessary to control symptoms and prevent joint deterioration.
Staying hydrated is another simple yet effective way to support joint health. Proper hydration helps maintain the elasticity of cartilage and supports the body’s natural repair processes. Drinking enough water throughout the day is essential, especially for those who engage in physical activities that increase fluid loss.
Finally, being proactive about joint health is key. This includes seeking prompt treatment for joint injuries, avoiding activities that cause joint pain, and listening to your body’s signals. Early intervention can prevent minor issues from escalating into conditions that promote bone spur formation.
In conclusion, while bone spurs are a common part of aging, taking proactive steps to maintain joint health can significantly reduce the risk of their development. By focusing on weight management, regular exercise, proper joint protection, and managing chronic conditions, individuals can support their joint health and minimize the likelihood of bone spurs impacting their quality of life.
Symptoms of bone spur
The presence of a bone spur, or osteophyte, can cause various symptoms in affected individuals. These manifestations can vary in intensity and nature depending on the location of the spur, its size and how it interacts with surrounding structures. The most common symptoms include pain, joint stiffness and loss of mobility.
Pain is often the most predominant symptom. When the bone spur forms, it can irritate surrounding tissues, including ligaments, tendons, and nerves. This irritation can lead to local pain that may be felt when moving the affected joint. For example, a bone spur in the knee may cause pain when flexing or extending the leg.
Joint stiffness is also frequently associated with the presence of bone spurs. Due to irritation of surrounding tissues, the range of motion of the joint may be reduced. Sufferers may experience a feeling of stiffness, particularly after a period of inactivity, such as sleeping or sitting for a long time.
Loss of mobility can be a significant symptom, especially if the bone spur interferes with normal movement of the joint. This can be particularly problematic in weight-bearing joints, such as the hips or knees. Reduced mobility can impact daily activities and overall quality of life.
Sometimes the presence of a bone spur can also cause grinding or crackling sensations during joint movements. This is often due to the spur rubbing against other bony or cartilaginous structures. These noises may be accompanied by unpleasant sensations.
It is essential to note that symptoms can change over time. Some individuals may not experience symptoms for a long time, while others may experience rapid deterioration in joint health. Treating symptoms related to the presence of a bone spur may involve approaches such as pain management, physical therapy to improve mobility, and in some cases, surgical procedures to remove the spur. A thorough medical evaluation is usually necessary to determine the most appropriate treatment plan based on each individual’s specific situation.
- Pain: One of the most common symptoms is pain, which can vary in intensity. Pain may be localized to the location of the osteophyte and may be exacerbated by movement or pressure.
- Stiffness: The presence of a bone spur can cause joint stiffness, limiting the range of motion in the affected area.
- Inflammation: Irritation of surrounding tissues can lead to inflammation, characterized by swelling and redness in the affected area.
- Decreased mobility: Bone spurs in joints can restrict mobility and make movement difficult.
- Crepitation: When the bone spur rubs against other bony structures or tissues, it can cause a crepitation sound during movement.
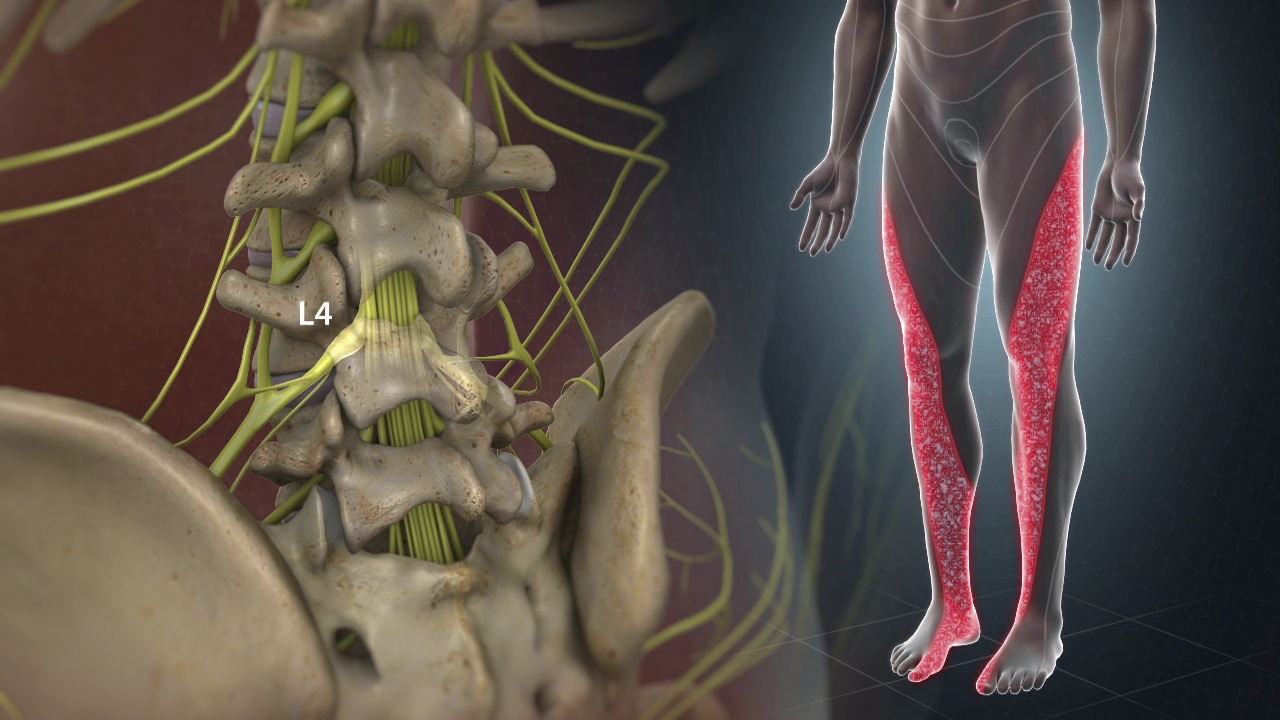
- Numbness or tingling: If the bone spur puts pressure on adjacent nerves, it may cause numbness or tingling sensations in the affected area.
- Muscle weakness: Muscle weakness may develop if the bone spur interferes with normal muscle function.
- Lameness: Bone spurs in weight-bearing joints, such as the hips or knees, can cause lameness while walking.
Differential Diagnosis
Differential Diagnosis of Bone Spurs: Understanding the Differences
Bone spurs, or osteophytes, can cause symptoms similar to other musculoskeletal conditions, making accurate diagnosis crucial for effective treatment. Understanding how bone spurs are differentiated from other conditions such as fractures, bursitis, or tendonitis helps healthcare providers ensure that patients receive the appropriate care.
- Fractures are a common condition that can be confused with bone spurs, especially when pain and reduced mobility are present. However, the cause and nature of the pain are different. Fractures result from a break or crack in the bone, usually due to trauma or excessive stress. The pain from a fracture is typically sharp and immediate, and the affected area may show signs of bruising or swelling. In contrast, bone spurs develop gradually, and the associated pain is more often chronic and dull, resulting from the friction between the spur and surrounding tissues. X-rays are essential in differentiating between these conditions, as fractures will show a clear break in the bone, while bone spurs appear as bony outgrowths.
- Bursitis is another condition that shares symptoms with bone spurs, such as pain and inflammation. Bursitis occurs when the bursae, small fluid-filled sacs that cushion bones and joints, become inflamed. This inflammation can cause pain and stiffness, similar to the symptoms caused by a bone spur. However, bursitis pain is often more acute and localized to the inflamed bursa, usually near a joint like the shoulder, elbow, or hip. Bone spurs, on the other hand, may cause more generalized joint pain and are often associated with degenerative changes in the joint, such as osteoarthritis. An ultrasound or MRI can help distinguish bursitis from bone spurs by revealing the presence of inflamed bursae versus bony growths.
- Tendonitis, the inflammation of tendons, can also present with symptoms similar to those of bone spurs, including pain, swelling, and limited joint movement. Tendonitis is typically caused by overuse or repetitive strain on a tendon, leading to inflammation and pain during movement. In contrast, bone spurs cause pain due to the irritation they create when pressing against surrounding soft tissues, such as tendons, ligaments, or nerves. While tendonitis pain tends to be more focused around the inflamed tendon, bone spur pain may be more diffuse and related to joint movement. MRI and physical examination can help differentiate tendonitis from bone spurs, with the imaging showing inflammation in tendons versus bony projections on the bones.
- Arthritis, particularly osteoarthritis, often coexists with bone spurs, as both conditions involve joint degeneration. However, arthritis is a broader condition that affects the entire joint, leading to symptoms like joint pain, stiffness, and swelling. Bone spurs are a secondary development in arthritis, forming as a result of the body’s attempt to repair damaged cartilage. Distinguishing between arthritis and the pain caused specifically by bone spurs involves a thorough clinical evaluation, including imaging tests like X-rays or MRIs, which can show the extent of joint degeneration and the presence of osteophytes.
- Neurological conditions, such as a herniated disc in the spine, can also mimic the symptoms of bone spurs, particularly when they cause nerve compression. A herniated disc can lead to radiating pain, numbness, or weakness, similar to the symptoms caused by bone spurs pressing on nerves. However, the underlying cause is different, with a herniated disc involving the displacement of disc material rather than bony growths. Diagnostic imaging, including MRIs and CT scans, can help differentiate between these conditions by showing the specific cause of nerve compression.
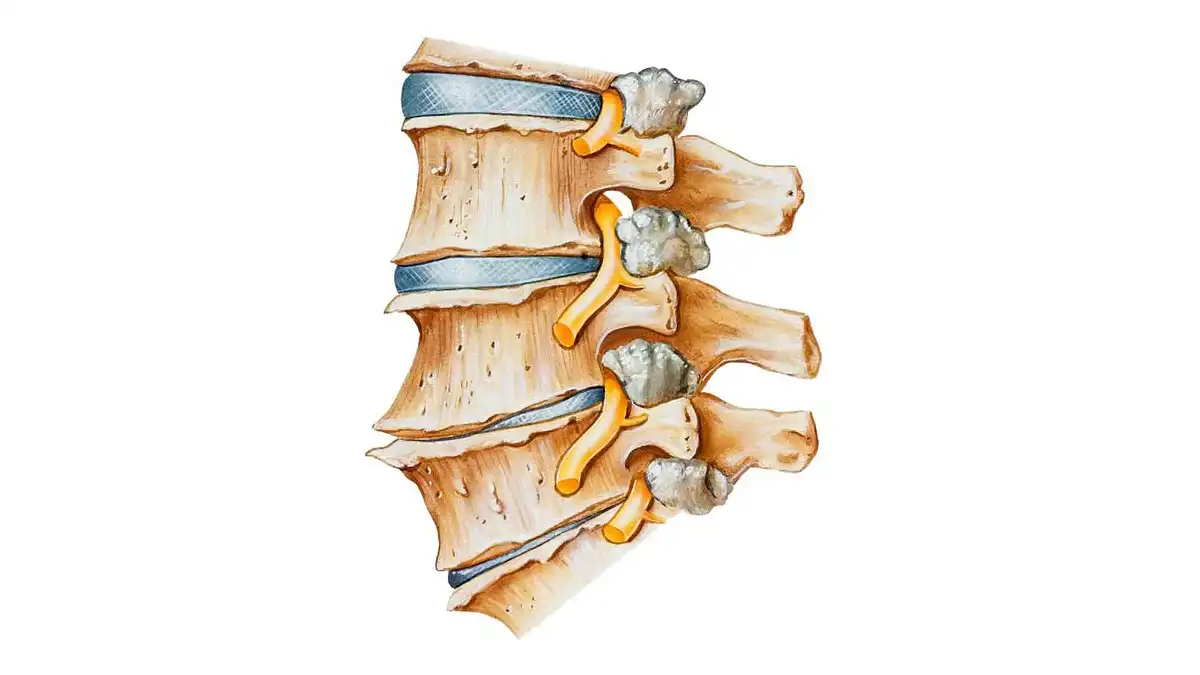
Two main types of osteophyte
Bone spurs, or osteophytes, come in different forms, and two main types can be identified based on their location and characteristics. These two types of bone spurs are marginal spurs and central spurs, each with distinct characteristics and implications for joint health.
Marginal spurs are the most common and form at the edges of joints where the bones come into contact. These spurs are often associated with conditions such as osteoarthritis, where the joint cartilage gradually breaks down. In response to this deterioration, the body forms bony growths at the edges of joints to stabilize the affected area. These marginal spurs may be visible on x-ray images, and their presence is often associated with pain and loss of joint mobility.
On the other hand, central spurs form inside the joint, usually affecting the joint socket itself. These spurs can result from wear and tear on the central cartilage of the joint, causing the body to respond in the form of bone growth. Central spurs may be more difficult to detect without medical imaging tests such as X-rays or MRIs because they are not directly visible to the naked eye. However, they can cause similar symptoms such as joint pain and stiffness.
When it comes to marginal spurs, they can be associated with specific conditions, such as spondylosis in the vertebrae of the spine. In this case, marginal spurs can form around the vertebrae as the cartilage wears away, causing the body to respond to stabilize the area. These spurs can potentially cause compression of nearby nerves, leading to associated pain and discomfort.
For central spurs, their presence may be a sign of inflammatory joint diseases such as rheumatoid arthritis. In these conditions, chronic inflammation can contribute to the formation of spurs inside the joints, leading to additional complications.
Enthesophytes
Enthesophytes represent bony growths specifically formed at the sites of attachment of tendons, ligaments or joint capsules to bone. These structures are often the result of repeated stress, chronic inflammation, or injury to the entheses, the points where these structures attach to the skeleton.
One of the main causes of enthesophytes is overuse or constant repetition of specific movements, often seen in athletes or individuals engaging in certain physical activities. Enthesophytes can also result from traumatic injuries, such as sprains or partial tendon tears, which can trigger a response by the body to strengthen the affected area.
Inflammatory diseases, such as ankylosing spondylitis, can also promote the formation of enthesophytes. In these conditions, chronic inflammation of the entheses can lead to structural changes, including abnormal bone growth. Enthesophytes associated with inflammatory diseases can often be identified by radiographs and are frequently seen in specific regions of the body, such as the spine or peripheral joints.
Another contributing factor is the aging process, which can lead to degeneration of connective tissues, including tendons and ligaments. This degeneration can create an environment conducive to the formation of enthesophytes, particularly in regions subject to increased pressure over time.
Symptoms associated with enthesophytes can vary depending on their location. In general, however, the presence of an enthesophyte can lead to pain at the attachment site, joint stiffness, and loss of mobility. In some cases, enthesophytes can also cause local symptoms such as swelling or redness.
Diagnosing enthesophytes often involves imaging tests such as X-rays or MRIs to visualize structural changes in soft and bony tissues. A thorough clinical evaluation is also necessary to understand the patient’s overall medical context and determine the underlying cause of the enthesophytes.
Treatment for enthesophytes generally aims to relieve pain, reduce inflammation, and restore joint function. This may include approaches such as anti-inflammatory medications, physical therapy sessions to strengthen the surrounding muscles, and in some cases, surgical procedures to remove the enthesophyte.
In summary, enthesophytes represent bony growths formed at the attachment sites of tendons, ligaments or joint capsules in response to various factors such as repeated stress, injury or inflammatory diseases. Their management requires a holistic approach, taking into account the underlying cause and developing a treatment plan tailored to each specific case.
Bone spurs
Are found at the edge of a bone, at the level of a joint.
- They are considered to be the result of friction and stress on the bone and are often associated with osteoarthritis.
- Minitraumas cause the body to build more bone in an attempt to repair itself.
- Osteophytes can be found in all joints
- Most are asymptomatic.
- Symptoms depend on the location of the bone spur.
- A bone spur on the knee can cause pain when the knee is bent; while a spur on the spinal cord can affect the nerves, producing numbness in the extremities.
- The development of osteophytes is a typical sign of the presence of osteoarthritis.
- The incidence of developing a bone spur increases with age and becomes common in people over 60 years of age and older.
Enthesophytes
Develop where the ligament or tendon inserts into a bone.
- They develop due to ligaments and tendons rubbing against bone, soft tissue injury, or inflammatory disease.
- These osteophytes form where soft tissues – tendons, fascia, ligaments or joint capsules – insert into bones.
- Enthesophytes can appear throughout the body, from the spine to the upper and lower limbs.
- They are common at the heel.
- Symptoms may include pain and swelling of the joint or redness.
- Often associated with:
- Local trauma
- High levels of physical activity
- Sometimes they are a symptom of a systemic condition
- seronegative spondyloarthritis;
- Diabetes
Therapeutic approach
- Osteophytes do not require treatment unless they cause pain or damage other tissues.
- Preventive treatment:
- weight loss to relieve joints (especially; osteoarthritis/plantar fasciitis)
- Joint stretching
- Treatment directed at symptoms may include:
- Rest
- ice
- stretching
- If an osteophyte is found in the foot
- change shoes
- add padding to the heel
- an orthosis.
- A podiatrist may be consulted if corns and calluses become a larger problem.
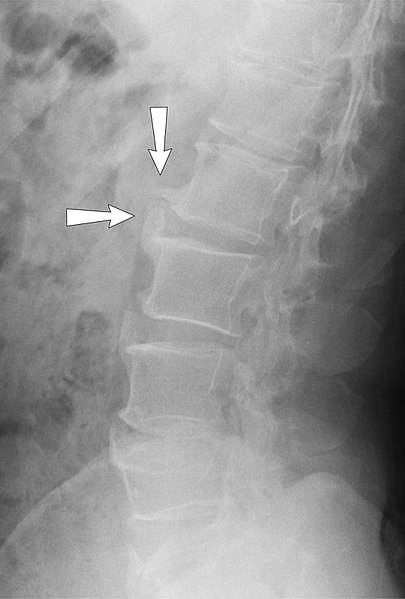
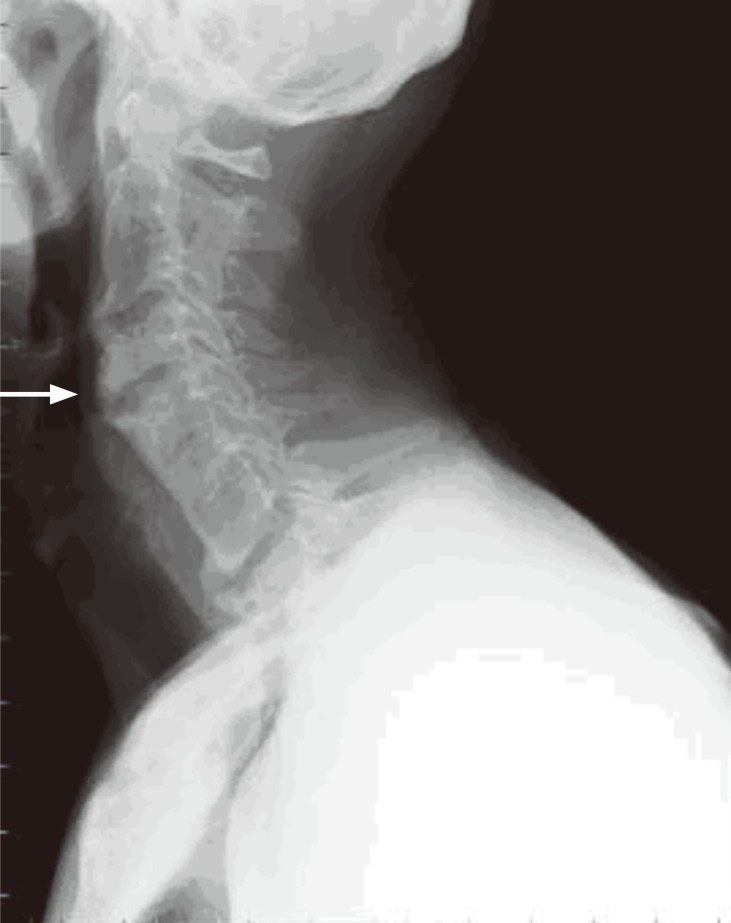
Radiographic sign of bone spur formation
The radiographic signs of bone spur formation are crucial for accurate diagnosis and understanding the extent of skeletal changes. When examining X-rays, one of the prominent indicators is the presence of bony outgrowths along the edges of bones, known as osteophytes or bone spurs. These spurs appear as irregular, often pointed, projections extending from the normal bone structure. Radiographically, they manifest as increased bone density or abnormal bony enlargements, providing a clear visual indication of their formation. The size and shape of the bone spurs can vary, and their presence is frequently associated with underlying conditions such as osteoarthritis, where the joint cartilage undergoes degeneration, prompting the body to react by forming these bony projections. In addition to osteoarthritis, radiographic signs of bone spur formation are observed in conditions involving joint instability, repeated trauma, or inflammatory joint diseases.
The X-ray images capture the skeletal changes, showcasing the location, size, and configuration of the bone spurs. Precise interpretation of these radiographic signs is vital for healthcare professionals to formulate an appropriate treatment plan and address any associated symptoms. While bone spurs themselves may not always cause discomfort, their impact on adjacent structures, such as nerves or neighboring joints, can result in pain and restricted mobility. Radiographic assessment aids in determining the severity of bone spur-related complications and guides decisions regarding potential interventions, ranging from conservative measures such as pain management and physical therapy to more invasive options like surgical removal of the bone spurs. Moreover, monitoring the progression of bone spur formation over time through radiographic imaging is essential for assessing the effectiveness of treatment strategies and making informed adjustments when necessary. In summary, the radiographic signs of bone spur formation serve as a fundamental diagnostic tool, offering a visual representation of skeletal changes. They enable healthcare professionals to identify the presence, location, and characteristics of bone spurs, facilitating a comprehensive understanding of the underlying conditions contributing to their development. This, in turn, guides the formulation of tailored treatment plans aimed at alleviating symptoms, improving joint function, and enhancing the overall quality of life for individuals affected by bone spur formation.
- Enlargement of the bone: X-rays may show localized enlargement of the bone near the affected joint. This may indicate the presence of a bone spur.
- Bone Edge Irregularities: Bone edges may appear irregular or have abnormal growths. These irregularities may be signs of additional bone growth.
- Formation of Bony Growths: X-rays may reveal the presence of abnormal bony growths on joint surfaces. These growths are osteophytes.
- Joint Narrowing: The affected joint may show signs of narrowing due to the formation of osteophytes, which may be visible on x-rays.
- Calcifications: The x-ray may also show calcifications around the joints, which may be associated with the presence of osteophytes.
- Marginal Spur: Some bone spurs can form on the edges of bones, creating a distinctive appearance on x-rays, known as a marginal spur.
- Joint deformities: Depending on the location and size of the osteophytes, joint deformities may be observed on x-rays.