Temporomandibular joint disorders (TMJ) refer to a group of problems affecting the joints and muscles responsible for jaw movement.
Introduction
The temporomandibular joint (TMJ) is a marvel of anatomy, orchestrating an impressive range of movements essential to our daily lives. Comprised of the mandible and mandibular fossa of the temporal bone, the TMJ is surrounded by a complex network of muscles, ligaments, and discs, creating a sophisticated interface for jaw movements.
The complex movements enabled by the TMJ are essential for activities as varied as chewing, speaking and yawning. When this joint works harmoniously, these actions seem simple and natural. However, disturbances in its delicate balance can give rise to temporomandibular joint (TMJ) disorders. These disorders can manifest in a variety of ways, from persistent pain to limitations in movement, which can have a significant impact on the quality of daily life.
The causes of TMJ disorders are varied, ranging from genetic factors to trauma, bruxism (teeth grinding) and stress. Symptoms, equally diverse, can include facial pain, frequent headaches, cracking or crackling sounds when moving the jaw, and even difficulty opening or closing the mouth. These manifestations can be disconcerting to those who experience them, requiring a thorough understanding of TMJ dynamics for effective management.
Anatomy of the TMJ
The temporomandibular joint (TMJ) is a synovial joint that connects the mandible (lower jaw) to the temporal bone of the skull. This complex joint is essential for jaw movements, including speaking, chewing and yawning. Here is a description of the anatomy of the TMJ:
ATM components:
- Temporal Bone: The temporal bone is a part of the skull and includes a cavity called the mandibular fossa. It is in this fossa that the upper end of the mandible, called the mandibular head, articulates.
- Mandible: The mandible is the lower jaw bone. The mandibular head connects to the temporal bone in the mandibular fossa to form the joint.
- Articular Disc: The temporomandibular joint includes an articular disc located between the mandibular head and the temporal bone. This disc is made of connective tissue and separates the joint into two distinct cavities: an upper cavity and a lower cavity.
- Joint Capsule: A fibrous capsule surrounds the joint, forming a protective sheath. This capsule contains synovial fluid, which lubricates the joint and reduces friction between the joint surfaces.
- Ligaments: Several ligaments surround the TMJ to stabilize the joint. The lateral and medial collateral ligaments are important for the lateral stability of the mandible.
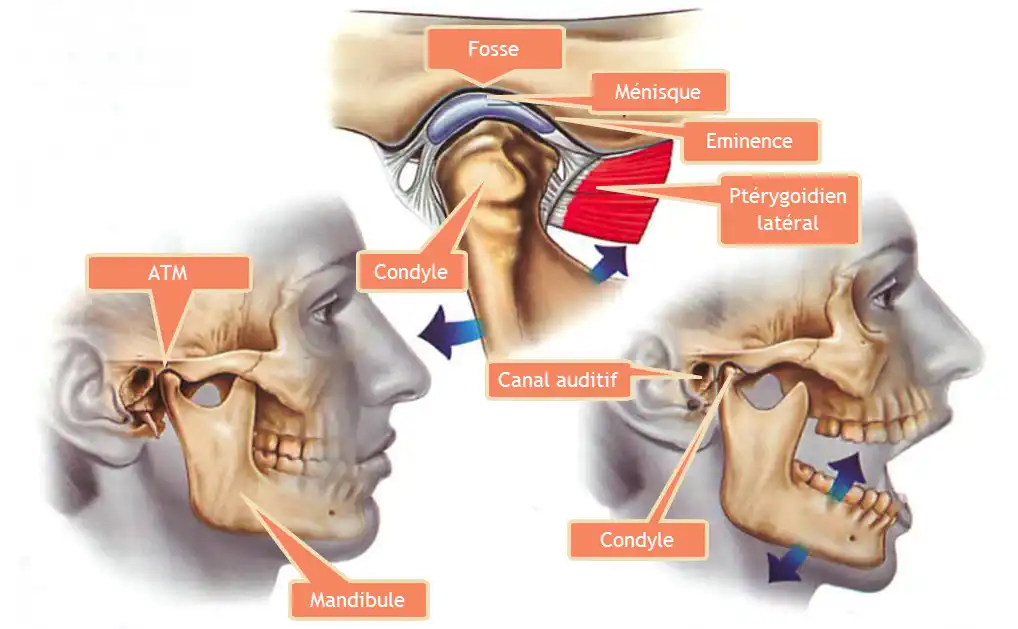
The meniscus is held in position by an anterior (front) band and the tissue attachments of the posterior band. This joint complex is surrounded by a joint capsule lined with a special tissue called the synovial membrane.
Biomechanics
The biomechanics of the temporomandibular joint (TMJ) are complex, involving a set of anatomical structures and coordinated movements. Understanding the biomechanics of the TMJ requires exploration of the muscles involved, the role of the articular disc (or meniscus) and associated movements.
Responsible Muscles
Several muscles contribute to the movements of the TMJ. Some of the main muscles involved include:
- Muscles of Mastication:
- Temporal muscle: Located on the temples, it elevates the mandible when closing the mouth.
- Masseter muscle: The most powerful chewing muscle, it also elevates the mandible and helps close the mouth.
- Medial pterygoid muscle: Located inside the mouth, it helps close the jaw.
- Lateral pterygoid muscle: Located inside the mouth, it participates in the lateral movements of the mandible.
- Muscles Accessories:
- Digastric, mylohyoid, and geniohyoid muscles: These muscles influence jaw posture and can be involved in certain movements.
Articular Disc (Meniscus)
The articular disc in the TMJ is composed of connective tissue and is located between the mandibular head and the temporal bone. This contributes to the stability and congruence of the joint. It divides the joint into two distinct cavities: an upper cavity and a lower cavity. The meniscus is designed to allow smooth movement and minimizes friction between joint surfaces.
The movement of the meniscus can be crucial when opening and closing the mouth. It can move within the joint cavity to accompany movements of the mandible, thus helping to maintain optimal joint congruence.
Meniscus Sliding and TMJ Movements
When opening the mouth, the articular disc slides forward with the mandible to maintain congruence between the mandibular head and the temporal bone. When closing the mouth, the disc returns to its original position.
Lateral and rotational movements of the mandible may also involve coordinated movements of the meniscus to maintain adequate congruence and minimize stress on the joint structures.
However, dysfunctions of the meniscus, such as disc displacement, can sometimes occur, leading to symptoms such as clicking, crackling, and pain associated with jaw movements.
In summary, the biomechanics of the TMJ involve a complex interaction between the muscles of mastication, the articular disc (meniscus), and the coordinated movements of the mandible. Any imbalance or dysfunction in these components can contribute to TMJ disorders. An accurate assessment by oral health professionals is often necessary to understand and effectively treat these problems.
Dysfunctional TMJ movement
Dysfunctional movement of the temporomandibular joint (TMJ) is a complex problem that has various implications for oral health and quality of life. The TMJ, a critical joint allowing jaw movement, can be prone to dysfunction, leading to symptoms such as pain, stiffness, and difficulty opening or closing the mouth.
The causes of dysfunctional TMJ movement are varied, ranging from physical trauma to psychological factors such as stress. Dental occlusion disorders, clenching or grinding habits, and structural abnormalities can also contribute to this dysfunction. The complexity of these factors requires a holistic approach in the assessment and management of this condition.
Symptoms of TMJ dysfunction can appear locally, with jaw, temple or ear pain, but they can also have broader repercussions, affecting sleep quality, nutrition and even posture. . People with this disorder may have difficulty eating, speaking, or performing simple jaw movements on a daily basis.
Management of dysfunctional TMJ movement requires a thorough evaluation by an oral health professional who specializes in temporomandibular joint disorders. A personalized treatment plan may include varied approaches, such as rehabilitation exercises, counseling on eating habits and stress control, and dental occlusion devices.
List of dysfunctional TMJ movements
- Jaw dislocation:
- Description: Jaw dislocation occurs when the mandible moves out of its normal position in the temporomandibular joint and cannot return to place spontaneously.
- Causes : This can be caused by trauma, excessive opening of the mouth (such as when yawning), or anatomical abnormalities.
- Symptoms: Pain, difficulty closing the mouth, and sometimes the patient may feel or hear a “click” during the dislocation.
- Treatment: A healthcare professional, often a dentist or maxillofacial surgeon, may be needed to put the jaw back into place. Muscle strengthening exercises and occlusion devices may be recommended to prevent future dislocations.
- Disc Displacement (Displacement of the Meniscus):
- Description: Disc displacement occurs when the articular disc (meniscus) of the TMJ moves from its normal position during jaw movements.
- Causes: Overuse of the joint, bruxism (teeth clenching), trauma, or anatomical disorders can contribute to this dysfunction.
- Symptoms: Clicking, crackling, pain when opening or closing the mouth, and sometimes temporary locking of the jaw.
- Treatment: Treatment may include rehabilitation exercises, relaxation techniques to reduce bruxism, anti-inflammatory medications, or in some cases, surgery.
- Blockage of the Jaw (Osteoarthritis):
- Description: Osteoarthritis of the TMJ can lead to jaw lock, where the mandible cannot perform certain movements due to abnormal cartilage wear.
- Causes: Aging, excessive wear and tear due to untreated TMJ disorders, bruxism, or arthritis.
- Symptoms: Pain, stiffness, difficulty opening or closing the mouth completely.
- Treatment: Treatment may involve medications to relieve pain, stress management techniques, jaw exercises, or in some cases, surgery.
- Limitation of Movements:
- Description: Some patients may have limited jaw movement, where the range of opening or closing is reduced.
- Causes: Tight muscles, muscle spasms, inflammation, or disc displacement.
- Symptoms: Difficulty opening the mouth completely, feeling of tightness, pain during movements.
- Treatment: Osteopathy, muscle stretching, strengthening exercises, and sometimes the use of dental appliances may be recommended to improve mobility.
- Bruxism (Teeth clenching):
- Description: Bruxism is an involuntary movement of clenching or grinding the teeth, often during sleep.
- Causes: Stress, anxiety, sleep disorders, dental malocclusion.
- Symptoms: Excessive tooth wear, jaw muscle pain, headaches, tooth sensitivity.
- Treatment : Occlusal splints to protect teeth, stress management, relaxation exercises.
- Jaw subluxation:
- Description: Subluxation occurs when there is a partial displacement of the jaw from its normal location without a complete dislocation.
- Causes: Trauma, excessive opening of the mouth.
- Symptoms: Pain, feeling of jaw shifting, difficulty closing the mouth.
- Treatment: Manual reduction by a healthcare professional.
- Hypomobility of the TMJ:
- Description: Hypomobility refers to a decrease in normal mobility of the TMJ.
- Causes: Muscle stiffness, inflammation, healing after an injury.
- Symptoms: Difficulty opening the mouth, feeling of stiffness.
- Treatment: Osteopathy, stretching exercises, anti-inflammatory medications.
- Hypermobility of the TMJ:
- Description: Hypermobility involves excessive range of motion of the TMJ, beyond normal.
- Causes: Ligament laxity, dental occlusion disorders.
- Symptoms: Jaw instability, pain during movements.
- Treatment: Muscle strengthening, occlusion devices, Osteopathy.
- Myoclonus of the Jaw:
- Description: Myoclonus are involuntary muscle contractions, often felt as jerks or tremors of the jaw.
- Causes: Neurological factors, stress.
- Symptoms: Involuntary muscle movements.
- Treatment: Stress management, relaxation, sometimes medication
Symptoms of TMJ Dysfunction
Temporomandibular joint (TMJ) dysfunction causes a diverse range of symptoms that can significantly impact the daily life of affected individuals. Among the most common manifestations, we find pain, often localized around the ear, jaw or temples. This pain can be acute or chronic, interfering with simple activities like chewing, speaking, or even just opening and closing your mouth. Some individuals also experience crunching or crackling sounds during jaw movements, indicating functional abnormalities at the joint. Jaw stiffness, another common symptom, can cause difficulty performing normal movements, compromising daily function. Headaches, sometimes associated with migraines, are also symptoms frequently linked to TMJ dysfunction. These headaches can radiate from the jaw region to the skull, increasing the complexity of the symptoms. Sometimes less obvious symptoms like dizziness, tinnitus, or a blocked ear sensation can accompany TMJ dysfunction, reflecting the multiple ways this condition can influence overall well-being. Due to the diversity of symptoms, the diagnosis of TMJ dysfunction requires careful evaluation by an oral health professional who specializes in temporomandibular joint disorders. Early recognition of these symptoms is crucial for appropriate management, as early treatment can often prevent the progression of TMJ disorders and improve the quality of life of those affected.
- Facial Pain: Localized pain in the TMJ region, often near the ear, jaw or temples.
- Chewing Pain: Pain during or after chewing, which may be felt in the upper or lower jaw.
- Clicks or Crackles: Sounds such as clicks, crackles, or grinding sounds during jaw movements.
- Limitation of Movements: Difficulty opening the mouth completely or making side to side movements.
- Headaches: Headaches, often centered around the temples, may be associated with TMJ dysfunction.
- Ear Pain: A pain or fullness in the ear with no apparent cause.
- Neck and Shoulder Pain: Pain may radiate to the neck and shoulders due to associated muscle tension.
- Jamming or Locking Sensations: A sensation that the jaw is temporarily blocking or locking.
- Muscle Fatigue: A fatigue or feeling of stiffness in the jaw muscles after prolonged use.
- Dizziness: Some individuals may experience dizziness, although this is less common.
Complications of TMJ Dysfunction
Masticatory muscle disorders
Pain in the masticatory muscles, which increases with palpation or manipulation of the muscles, is often associated with restriction of mandibular movements.
Disc dislocation with reduction
Displacement of the disc can lead to partial or complete disarticulation of the disc from the disc space in the condyle-disc assembly. When the mouth closes, the articular disc moves forward of the condylar head, and when it opens, the disc repositions itself on the condylar head in a manner similar to normal. This back and forth movement of the disc explains noises such as clicks, pops, or pops in the ATM. This may be accompanied by jaw deviation when opening the mouth, with an expected normal range of motion. However, in some cases the disc may fail to reduce, resulting in limitation of mouth opening, known as disc displacement with reduction with intermittent locking.
Disk displacement without reduction
When the articular disc repeatedly fails to reduce, causing limited mouth opening, the diagnosis of disc displacement without reduction is made. This situation may result from loss of elasticity of the superior retrodiscal lamella, forcing the disc to pass in front of the condyle. It manifests itself as a blocked jaw during closing, associated with maximum opening difficulty and pain.
Structural inconsistencies with articular surfaces
This disorder arises from changes in the smooth sliding surfaces of the TMJ, leading to frictional adhesions and inhibiting joint function. Shape deviations, adhesions, subluxations and spontaneous dislocations can result from this structural incompatibility.
Disruption of the condyle-disc complex
Micro- or macro-trauma can cause failure of the rotational function of the disc, which may result from lengthening of the ligaments or thinning of the posterior edge of the disc. Contributing factors include micro- or macro-trauma.
Dislocation (dislocation)
Dislocation occurs when the condyle moves in front of the articular eminence and cannot return to the normal position. It often results from hyperextension of the TMJ, freezing the joint in the open position during mouth opening. It can be partial (subluxation) or complete (dislocation), acute or chronic, and can cause difficulty closing the mouth and pain.
Risk factors for TMJ dysfunction
- Imbalances in the muscles of mastication resulting from hypertonicity, spasms, trigger points and abnormalities in joint mechanics;
- Muscle overuse
- Chew gum
- Chew on one side of the mouth
- Yawning repetitively and prolonged
- Smoking a pipe or cigar
- Malocclusion
- Loss of the vertical dimension of the occlusion
- Misalignment of the cranial bones
- Particularly misalignment of the temporal bones
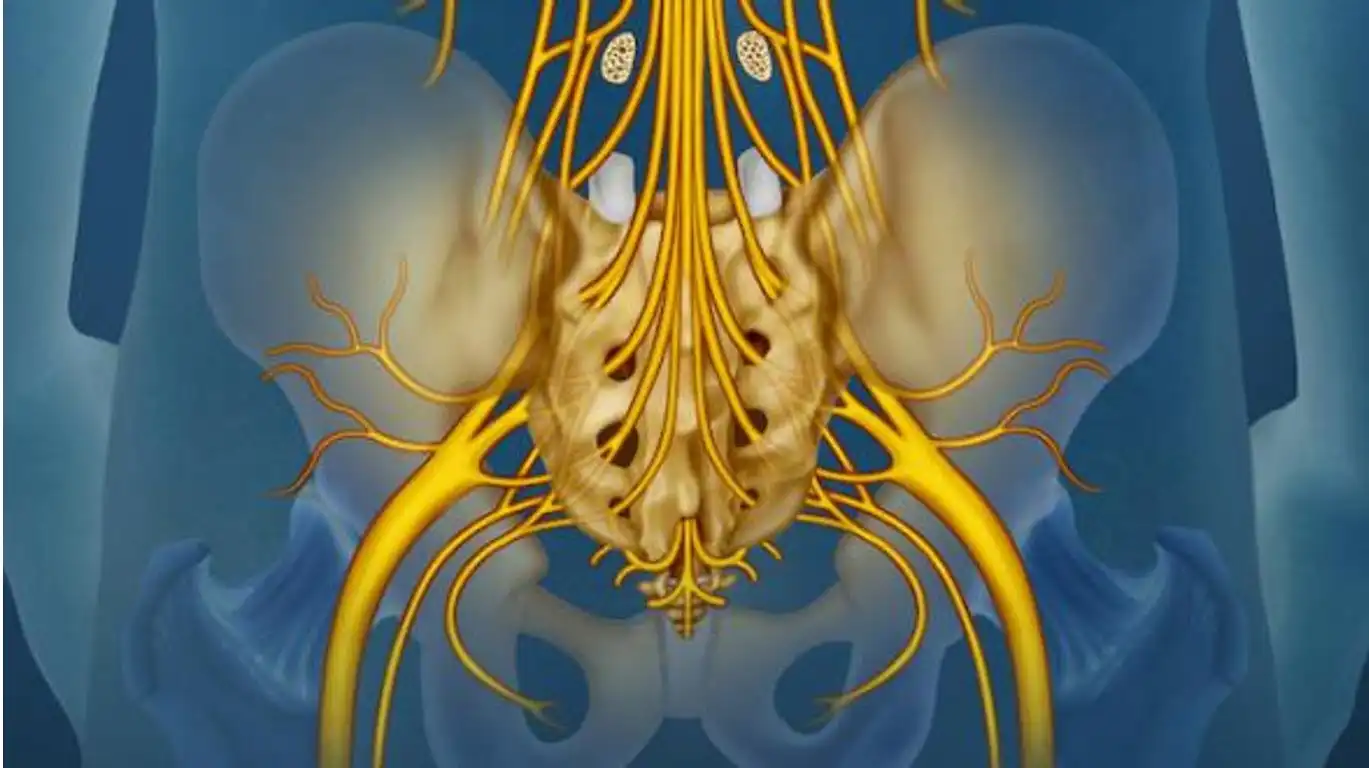
- Postural dysfunctions
- Hyperkyphosis
- Scoliosis leads to muscular imbalances in the neck and shoulders and, therefore, increased activity of the jaw muscles to counterbalance head position
- Lateral tilt of the pelvis due to a difference in leg length or a small hemipelvis (Travel/, Simons, 1983)
- Foot and ankle problems that impair gait, such as flatfoot and ankle sprain, also affect head position (Milne et al, 1997).
- A difference of one centimeter in leg length leads to altered occlusion and changes the resting position of the mandible (Gelb, 1985);
- Increased stress
- Causing jaw clenching (“holding” words by clenching your teeth)
- Bruxism
- Trauma, direct or indirect ;
- A blow to the jaw
- Hyperextension phase of whiplash when the mandible opens forcefully
- Mouth held open for long periods of time due to intubation during general anesthesia
- Prolonged cervical traction or support of the head under the chin by the cupped hand in a seated position;
- Sinus blockage or infection can lead to mouth breathing, forward head posture
Visual examination
- Opening and closing of the mouth : Teeth normally close symmetrically, jaw is normally centered
- Teeth alignment : Note crossbites, underbites or overbites
- Symmetry of facial structures : Eyes, nose, mouth, length of the mandible
- Posture : Forward head posture, rounded shoulders, and scapular protraction are common
- Total jaw opening range : measurement from the upper edge of the tooth to the lower edge of the tooth (normal mouth opening and closing ~ 40-50 mm)
- Listen with a stethoscope if there is crepitus in the joint.
- Lateral movement without return to the midline . Deflections are associated with disc dislocations without reduction or unilateral muscle restriction.
Myofascial Syndromes and TMJ Disorders
Myofascial syndromes related to TMJ usually involve muscle tension or pain in specific areas such as the temporalis muscle, masseter, pterygoid, among others. These disorders can cause various symptoms associated with temporomandibular joint (TMJ) dysfunction.
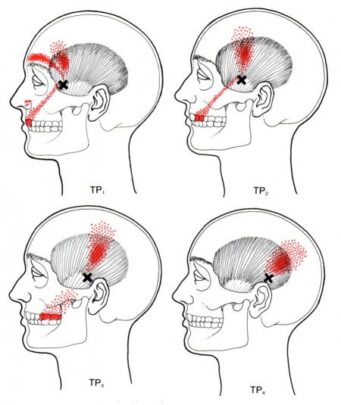
- Temporal Muscle:
- Myofascial Syndrome: Tension or pain in the temporalis muscle.
- Associated symptoms: Headaches, temple pain.
- Masseter:
- Myofascial Syndrome: Tension or pain in the masseter muscle.
- Associated symptoms: Facial pain, difficulty opening the mouth.
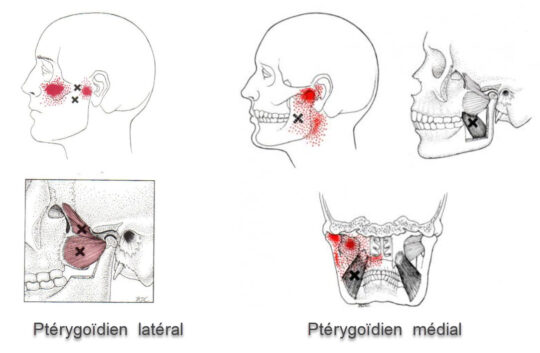
- Lateral Pterygoid:
- Myofascial Syndrome: Tension or pain in the lateral pterygoid muscle.
- Associated symptoms: Ear pain, difficulty chewing.
- Medial Pterygoid:
- Myofascial Syndrome: Tension or pain in the medial pterygoid muscle.
- Associated symptoms: Pain in the back of the throat, difficulty swallowing.
- Links to TMJ Disorder Symptoms:
- Muscle tension in these areas can contribute to TMJ disorders.
- Symptoms such as jaw pain, joint cracking, and limited mouth opening may be exacerbated by these myofascial syndromes.
- Management Approaches:
- Manual therapy: Massages and myofascial release techniques.
- Stretching: Exercises to relax affected muscles.
- Physical therapy: Muscle strengthening and joint rehabilitation.
- Professional Consultation:
- If symptoms persist or are severe, consult a healthcare professional, such as an osteopath.
Masseter
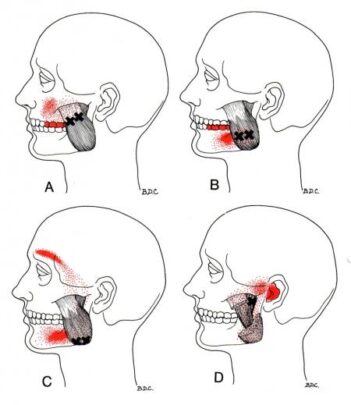
Temporal
Lateral and medial pterygoid
Restricted mobility
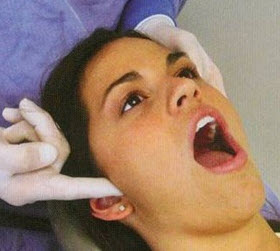
The temporamendibular joint is essentially anterior and posterior. Thus, to determine these fields of movement, the osteopath will make contact anteriorly and superiorly to the tragus of the ear. Indeed, this location is ideal for evaluating the TMJ, because it is in direct contact with the condyle. The patient will have to open and close the mouth as well as to send the jaw sideways. The contact will verify any possible resistance to movements. The osteopath will thus be able to mobilize the TMJ depending on the dysfunction.
Crepitation
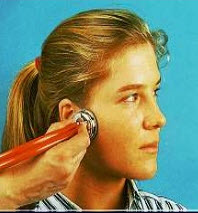
A poor occlusion, often caused by non-uniform teeth, will cause premature wear of the disc. Over time, the joint surfaces will wear down and remodel. With the help of the stethoscope, it is possible to hear this crepitation during the opening and closing of the mouth. TMJ noises are a symptom of dysfunction in these joints. Sounds commonly produced by TMD are generally described as a “click” or “pop” when only one sound is heard and as a “crepitation” or “crepitus” when there are multiple rough, rasping sounds.
TMJ syndrome prevention
- Maintain good oral hygiene: Good oral hygiene contributes to the overall health of the mouth. Brush your teeth regularly, floss, and see your dentist for regular checkups.
- Avoid harmful habits: Avoid chewing gum frequently, as this can put excessive pressure on the TMJ. Also avoid chewing hard objects like pens or ice cubes.
- Stress management: Stress can contribute to muscle tension, including in the TMJ region. Learn stress management techniques such as meditation, deep breathing or yoga.
- Avoid hard, sticky foods: Limit your intake of hard, sticky foods that require excessive mouth opening. This may include hard candy, nuts, or foods that are difficult to chew.
- Avoiding bruxism: If you suffer from bruxism (clenching your teeth while sleeping), consult your dentist to discuss solutions such as occlusal splints to protect your teeth.
- Maintain good posture: Correct posture, especially in the head, neck and shoulders, can help reduce muscle tension that can affect the TMJ.
- Avoid bad yawning habits: Try not to yawn excessively or in a way that overstretches your jaw.
- Muscle-strengthening exercises: Certain specific exercises can help strengthen the jaw muscles and improve TMJ stability. Consult an oral health professional for advice on appropriate exercises.
- Monitor symptoms: Be alert for symptoms such as facial pain, clicking or crackling sounds during jaw movements, and consult a healthcare professional if symptoms persist.
Gentle self-treatment of the lateral pterygoid
The lateral pterygoid muscle is inevitably quite tender in most individuals suffering from TMJ problems or bruxism. To palpate, place the index finger in the mouth. Apply pressure in a cranial direction just below the zygomatic arch.
Be gentle with palpation, this muscle is very sensitive to touch (the mucous membranes of the mouth can also form an ulcer if the pressure is too strong). The best technique is to go gradually by pressing the muscle between the index finger and thumb.
It is possible to compress the lateral pterygoid muscle yourself for 1 minute several times a day.
- Place the thumb on the opposite side of the TMJ on the pterygoid muscle in the mouth.
- With the help of the middle or index finger of the same hand pinch the knot of the pterygoid muscle on the inner side in the mouth (zygomatic arch)
- Relief from headaches, jaw or face pain is sometimes immediate.
It is important to note that these techniques may require extensive knowledge of anatomy and an understanding of specific TMJ issues. If you are considering practicing these techniques, it would be recommended to do so under the supervision of a healthcare professional, such as an osteopath who specializes in TMJ disorders. It is always best to consult a healthcare professional before undertaking self-treatment techniques for health conditions.
Remember, these suggestions are not a substitute for professional medical consultation. If you have ongoing problems related to the lateral pterygoid, consult a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Conclusion
In conclusion, temporomandibular joint (TMJ) disorders encompass a set of complex problems affecting the joints and muscles responsible for jaw movement. TMJ plays a crucial role in daily activities such as eating, speaking and yawning, and associated disorders can lead to a variety of symptoms, from pain to movement limitations.
The detailed anatomy of the TMJ, the biomechanics involved, and the muscles responsible for jaw movements were presented. TMJ dysfunctions, such as jaw dislocation, disc displacement, osteoarthritis, movement limitation, bruxism, and others, were explained in detail, highlighting the various risk factors and associated symptoms.
Prevention of TMJ disorders involves recommendations such as maintaining good oral hygiene, avoiding harmful habits, managing stress, maintaining good posture, and monitoring symptoms. Additionally, gentle self-treatment techniques have been suggested, but it is essential to apply them carefully and under the supervision of a healthcare professional.
If symptoms persist or are severe, consultation with an oral health professional specializing in TMJ disorders is recommended. Accurate assessment by experts is necessary for a proper diagnosis and tailored treatment plan, emphasizing the importance of a multidisciplinary approach to effectively treat TMJ disorders.
Question and Answer
- What are the main components of the temporomandibular joint (TMJ)?
- A. Temporal bone
- B. Mandible
- C. Articular disc
- D. Joint capsule
- E. All choices are correct
- What is the function of the articular disc in TMJ?
- A. Stabilize the joint
- B. Divide the joint into two cavities
- C. Allow fluid movements
- D. Minimize friction
- E. All of the above
- Which muscles are responsible for TMJ movements related to chewing?
- A. Temporal muscle
- B. Masseter muscle
- C. Medial pterygoid muscle
- D. Lateral pterygoid muscle
- E. All choices are correct
- Which movement of the meniscus is crucial when opening and closing the mouth?
- A. Rotation
- B. Sliding forward
- C. Sliding backwards
- D. Lateral movement
- E. All of the above
- What can cause meniscus dysfunction, such as disc displacement?
- A. Clicks
- B. Crackles
- C. Pain associated with jaw movements
- D. All of the above
- E. None of the above
- What is jaw dislocation?
- A. Disc displacement
- B. Exit of the mandible from its normal position
- C. Jaw lock
- D. Hypomobility of the TMJ
- E. None of the above
- What are the possible causes of TMJ disc displacement?
- A. Overuse of the joint
- B. Bruxism
- C. Trauma
- D. All of the above
- E. None of the above
- What can TMJ osteoarthritis cause?
- A. Jaw lock
- B. Pain
- C. Stiffness
- D. All of the above
- E. None of the above
- What factors can contribute to TMJ disorders?
- A. Muscular imbalances
- B. Muscle overuse
- C. Malocclusion
- D. All of the above
- E. None of the above
- What are the approaches to managing TMJ-related myofascial syndromes?
- A. Manual therapy
- B. Stretching
- C. Physical therapy
- D. Professional consultation
- E. All of the above
- What is the role of the lateral pterygoid muscle in TMJ?
- A. Opening the mouth
- B. Closing the mouth
- C. Lateral jaw movements
- D. All of the above
- E. None of the above
- What are common symptoms of TMJ dysfunction?
- A. Ear pain
- B. Headaches
- C. Teeth clenching
- D. All of the above
- E. None of the above
- What is bruxism and how is it related to TMJ?
- A. Involuntary teeth grinding
- B. Disc displacement
- C. Osteoarthritis
- D. All of the above
- E. None of the above
- What types of movements are possible in ATM?
- A. Rotation
- B. Translation
- C. Elevation
- D. All of the above
- E. None of the above
- What is the difference between an open dislocation and a closed jaw dislocation?
- A. Open dislocation involves permanent displacement
- B. Closed dislocation involves a temporary blockage
- C. Both involve permanent movement
- D. Both involve a temporary blockage
- E. None of the above
- You
Answers:
- E
- E
- E
- E
- D
- B
- D
- D
- D
- E
- VS
- D
- D
- D
- B
References
- Lomas J, Gurgenci T, Jackson C, Campbell D. Temporomandibular dysfunction. Aust J Gen Pract. 2018 Apr;47(4):212-215. [ PubMed ]
- Sharma S, Gupta DS, Pal US, Jurel SK. Etiological factors of temporomandibular joint disorders . Natl J Maxillofac Surg. 2011 Jul;2(2):116-9. [ PMC free article ] [ PubMed ]
- Bordoni B, Varacallo M. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Jul 26, 2021. Anatomy, Head and Neck, TemporomandibularJoint . [ PubMed ]
- Scrivani SJ, Keith DA, Kaban LB. Temporomandibulardisorders . N Engl J Med. 2008 Dec 18;359(25):2693-705. [ PubMed ]
- Liu F, Steinkeler A. Epidemiology, diagnosis, and treatment of temporomandibular disorders . Dent Clin North Am. 2013 Jul;57(3):465-79. [ PubMed ]
- Young AL. Internal derangements of the temporomandibular joint : A review of the anatomy, diagnosis, and management. J Indian Prosthodont Soc. 2015 Jan-Mar;15(1):2-7. [ PMC free article ] [ PubMed ]
- Sharma NK, Singh AK, Pandey A, Verma V, Singh S. Temporomandibularjoint dislocation. Natl J Maxillofac Surg. 2015 Jan-Jun;6(1):16-20. [ PMC free article ] [ PubMed ]
- Solberg WK. Temporomandibularjoint syndrome. Semin Neurol. 1988 Dec;8(4):291-7. [ PubMed ]
- Cooper BC, Kleinberg I. Examination of a large patient population for the presence of symptoms and signs of temporomandibular disorders . Cranio. 2007 Apr;25(2):114-26. [ PubMed ]
- Stepan L, Shaw CL, Oue S. Temporomandibular disorder in otolaryngology: systematic review. J Laryngol Otol. 2017 Jan;131(S1):S50-S56. [ PubMed ]
- Okeson JP, de Leeuw R. Differential diagnosis of temporomandibular disorders and other orofacial pain disorders . Dent Clin North Am. 2011 Jan;55(1):105-20. [ PubMed ]
- Reneker J, Paz J, Petrosino C, Cook C. Diagnostic accuracy of clinical tests and signs of temporomandibular joint disorders : a systematic review of the literature. J Orthop Sports Phys Ther. 2011 Jun;41(6):408-16. [ PubMed ]