Introduction
Osteoarthritis of the shoulder, also known as glenohumeral osteoarthritis, is a degenerative joint condition that primarily affects the shoulder joint. This form of osteoarthritis involves the gradual deterioration of the cartilage that cushions the ends of the bones within the shoulder joint. As the cartilage wears away, the bones may rub against each other, leading to pain, stiffness, and reduced mobility.
The physiopathology of shoulder osteoarthritis involves various contributing factors. One key element is the breakdown of articular cartilage, the smooth tissue covering the ends of the bones in the shoulder joint. Articular cartilage plays a crucial role in facilitating smooth and pain-free joint movements. In osteoarthritis, this cartilage undergoes degeneration, losing its elasticity and becoming more susceptible to damage.
The process begins with the formation of small cracks or fissures in the cartilage, possibly due to aging, overuse, or previous injuries. As these cracks progress, the cartilage may wear away unevenly, leading to the exposure of the underlying bone. Without the protective cushion of healthy cartilage, joint movements become less smooth, resulting in pain and discomfort.
In response to the loss of cartilage, the body may attempt to repair the damage by forming osteophytes or bone spurs. While these bony outgrowths aim to stabilize the joint, they can contribute to further pain and restriction of movement. Additionally, the synovial membrane, which produces synovial fluid for joint lubrication, may become inflamed, exacerbating symptoms.
The inflammatory response in shoulder osteoarthritis involves the release of pro-inflammatory cytokines and enzymes, contributing to the degradation of cartilage and promoting joint inflammation. The joint capsule, a fibrous structure that surrounds the shoulder joint, may also undergo changes, impacting the joint’s range of motion.
Patients with shoulder osteoarthritis commonly experience pain, especially during movement or weight-bearing activities. Stiffness and reduced flexibility in the shoulder joint are common, making daily tasks challenging. As the condition progresses, individuals may notice a decrease in strength and function, affecting their overall quality of life.
Treatment approaches for shoulder osteoarthritis aim to manage symptoms, improve joint function, and enhance the individual’s quality of life. Conservative measures include pain medications, physical therapy, and lifestyle modifications. In more advanced cases, surgical interventions such as joint replacement may be considered to alleviate pain and restore joint function.
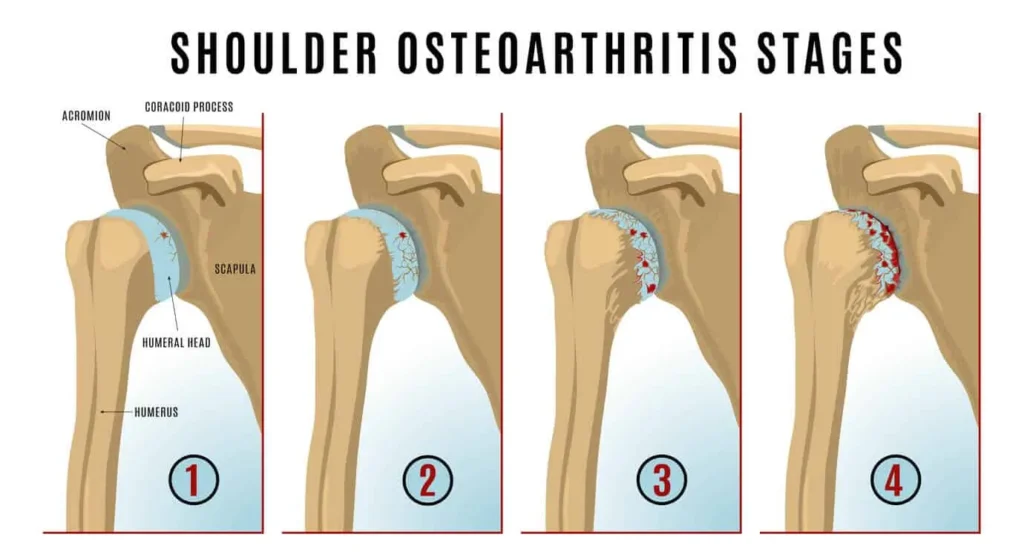
Stage 1: Early osteoarthritis shows minor cartilage wear, with the joint surface still relatively smooth. Mild pain or discomfort may occur, but the joint remains functional.
Stage 2: Moderate wear and tear become evident, with more pronounced cartilage erosion. Small cracks and roughness may appear, leading to increased stiffness and pain during movement.
Stage 3: Advanced osteoarthritis is marked by significant cartilage loss, exposing the bone beneath. Pain becomes more persistent, and mobility is further restricted due to bone-on-bone contact.
Stage 4: Severe osteoarthritis is characterized by near-complete cartilage deterioration, with bones rubbing directly against each other, causing extreme pain, inflammation, and limited movement. Bone spurs may also form, contributing to joint deformity.
These stages highlight the degenerative nature of osteoarthritis, requiring appropriate management to preserve joint function.
Causes of shoulder osteoarthritis
Shoulder osteoarthritis, a debilitating condition, has its origins in several factors. The natural aging of articular cartilage, with its gradual wear over time, is one of the main causes. Previous trauma, such as shoulder dislocations or fractures, can also predispose to osteoarthritis. Repetitive or excessive activities, particularly in occupations that place intense demands on the shoulder, can contribute to cartilage deterioration. Anatomical disorders, such as muscle imbalances or abnormalities in joint structure, are also predisposing factors. Additionally, underlying medical conditions, such as rheumatoid arthritis, can contribute to the development of shoulder osteoarthritis. Understanding these causes allows for more targeted prevention and management approaches to mitigate the impact of this painful condition on individuals’ quality of life.
- Aging: Natural aging is one of the main risk factors for shoulder osteoarthritis. With age, articular cartilage tends to gradually wear away, which can lead to degenerative changes in the joint.
- Previous trauma or injuries: Previous injuries to the shoulder, such as fractures, dislocations, or labrum injuries, can increase the risk of developing shoulder osteoarthritis. Structural damage to the joint can disrupt normal balance, contributing to premature wear of cartilage.
- Overuse: Repetitive or excessive shoulder activities, common in certain professions or sports, can contribute to cartilage wear over time. Repetitive movements can cause increased friction in the joint, contributing to the development of osteoarthritis.
- Joint instability: Shoulder instability, often due to labrum damage or weakened ligaments, can alter the normal distribution of forces in the joint. This can lead to uneven wear of the cartilage and promote the development of osteoarthritis.
- Genetic factors: There is a genetic component in the development of osteoarthritis. If family members have been affected by this condition, this may increase the risk for other family members.
- Other medical conditions: Conditions such as rheumatoid arthritis, which causes chronic inflammation of the joints, may also be associated with an increased risk of shoulder osteoarthritis.
- Obesity: Being overweight or obese puts increased pressure on joints, including the shoulder, which can contribute to cartilage wear and the development of osteoarthritis.
Symptoms of shoulder osteoarthritis
Symptoms of shoulder osteoarthritis may include persistent pain in the shoulder, often made worse by movement. Patients may experience joint stiffness, limiting shoulder mobility. A crackling or rubbing sensation during movement may also be present. Discomfort can worsen over time, affecting daily quality of life. Activities such as lifting your arm, carrying heavy objects, or performing repetitive movements may become difficult. Additionally, some individuals may experience decreased muscle strength in the shoulder.
- Pain: Pain is one of the main symptoms. At first, the pain may be mild and occur occasionally. However, as osteoarthritis progresses, pain may become more frequent and severe. It is usually felt deep in the shoulder and may worsen with specific movements.
- Stiffness: People with shoulder osteoarthritis may experience joint stiffness, especially after a period of inactivity, such as sleeping. Stiffness can limit shoulder mobility.
- Loss of mobility: Osteoarthritis can cause a progressive loss of mobility in the shoulder. Movements such as raising your arm above your head or reaching behind your back can become difficult and painful.
- Crepitation: Some patients may feel or hear a rubbing, cracking, or crackling sensation when they move their shoulder. This may be due to friction from worn joint surfaces.
- Inflammation: Osteoarthritis can cause local inflammation, leading to swelling around the shoulder joint. This can contribute to feeling hot and stiff.
- Muscle weakness: Due to pain and loss of mobility, the muscles surrounding the shoulder can weaken over time.
Differential diagnoses of shoulder osteoarthritis
- Adhesive capsulitis (frozen shoulder): This condition is characterized by inflammation and thickening of the shoulder joint capsule, leading to progressive stiffness and loss of mobility. Although adhesive capsulitis can cause pain similar to that of osteoarthritis, it is distinguished by a more marked limitation of mobility.
- Rotator cuff tendonitis: Inflammation or injury to the rotator cuff tendons can cause shoulder pain, especially during specific movements. Rotator cuff tendinitis can be differentiated from osteoarthritis by the specific location of pain and specific clinical tests.
- Shoulder bursitis: Inflammation of the bursa, a small sac of fluid between the tendons and bones of the shoulder, can cause pain similar to osteoarthritis. Symptoms may include pain on palpation and worsening with movement.
- Labrum Injuries: Injuries to the labrum, which is the rim-like cartilage around the shoulder joint, can cause pain, cracking, and instability. These symptoms may be similar to those of osteoarthritis.
- Rheumatoid arthritis: Although less common, rheumatoid arthritis can affect the shoulder and cause inflammation, pain and loss of mobility. It can be differentiated from osteoarthritis by its systemic inflammatory nature.
- Cervico-brachial neuralgia: Problems in the neck can cause painful symptoms that radiate to the shoulder. Nerve compression in the cervical region can mimic the pain associated with shoulder osteoarthritis.
Recommendations
To manage the symptoms of shoulder osteoarthritis, certain recommendations can be considered. Firstly, osteopathy can play a vital role in strengthening the muscles around the shoulder, improving stability and reducing pain. Specific exercises may be prescribed to maintain joint mobility. It is also crucial to maintain a healthy body weight, as excess weight can worsen osteoarthritis symptoms. Lifestyle changes, such as adopting correct posture and avoiding repetitive movements that can worsen the condition, may be beneficial. If pain persists, analgesic or anti-inflammatory medications may be recommended, under the supervision of a healthcare professional. In more severe cases, where quality of life is significantly impaired, surgical procedures such as shoulder replacement surgery may be considered. However, all treatment options should be discussed with a healthcare professional to develop a personalized management plan based on each patient’s specific situation.
- Resting the shoulder joint
- Perform range of motion exercises. These exercises serve to increase flexibility.
- Apply moist heat.
- Apply ice to the shoulder. Ice is applied for 20 minutes two or three times a day to decrease inflammation and pain.
- Take the food supplements glucosamine and chondroitin (discuss with your doctor, as this supplement may interact with certain medications)
Radiographic signs of shoulder osteoarthritis
Radiographic signs of shoulder osteoarthritis provide a detailed view of the structural changes occurring in this joint. X-ray images usually reveal a narrowing of the joint space, resulting from the loss of cartilage between the bony surfaces. Osteophyte formations, or bony growths, may appear around the joint, reflecting the body’s attempt to compensate for the loss of cartilage. The margins of the bones may show changes, and bone spurs may develop. Joint alignment may be altered, and the head of the humerus may show deformities. These radiographic signs, interpreted by health professionals, are essential to diagnose and assess the severity of shoulder osteoarthritis, thus guiding appropriate treatment options.
- Narrowing of the joint space: One of the first radiographic manifestations of shoulder osteoarthritis is the narrowing of the joint space between the head of the humerus (upper arm bone) and the glenoid socket of the scapula. . This indicates loss of articular cartilage.
- Osteophyte Formation: Bony growths, called osteophytes, can form around the edges of the joint in response to cartilage deterioration. These osteophytes may be visible on x-rays and contribute to joint deformity.
- Subchondral sclerosis: Sclerosis, or densification, of the bone beneath the cartilage (subchondral sclerosis) is another radiographic sign of osteoarthritis. This may indicate an abnormal bone response to loading resulting from cartilage loss.
- Subchondral Cysts: Subchondral cysts can form in the bone beneath the cartilage due to osteoarthritis. These cysts may be visible on x-rays.
- Joint deformities: As osteoarthritis progresses, x-rays may reveal structural changes, such as deformities of the head of the humerus or glenoid fossa.

The main signs of shoulder osteoarthritis are:
- Subchondral sclerosis
- Joint space narrowing
- Formation of marginal osteophytes
- Bone erosions/subchondral cyst formation
Conclusion
In conclusion, glenohumeral arthritis and acromioclavicular joint osteoarthritis represent significant clinical challenges, particularly in individuals over 50 years of age. The diversity of etiologies, ranging from osteoarthritis to rheumatoid arthritis and post-traumatic arthritis, highlights the complexity of these joint conditions. These conditions can lead to progressive deterioration, limiting mobility and causing debilitating pain.
Treating these conditions requires a well-considered approach, often involving conservative strategies such as physical therapy and anti-inflammatory medications, as well as more invasive options like surgery in some cases. Effective management of glenohumeral arthritis and AC osteoarthritis requires close collaboration between healthcare professionals and patients, with particular attention paid to personalizing treatment plans based on individual needs. .
Continuing research in the field of rheumatology offers hope for new therapeutic advances that could improve the quality of life of those affected by these conditions. In the meantime, awareness, education, and early diagnosis remain crucial elements in mitigating the effects of glenohumeral arthritis and AC osteoarthritis.
Ultimately, an integrated approach focused on understanding the etiologies, preventing aggravating factors and applying appropriate treatments can play a decisive role in the management of these joint disorders. The ultimate goal is to provide affected individuals with a better quality of life by minimizing pain, preserving functionality, and encouraging active participation in their own joint well-being.
References
- Centers for Disease Control and Prevention (CDC) Prevalence and most common causes of disability among adults—United States, 2005. Morbidity and Mortality Weekly Report (MMWR) 2009;58(16):421–426. [ PubMed ] [ Google Scholar ]
- Kerr R, Resnick D, Pineda C, Haghighi P. Osteoarthritis of the glenohumeral joint: a radiologic-pathologic study. American Journal of Roentgenology. 1985;144(5):967–972. [ PubMed ] [ Google Scholar ]
- Petersson CJ. Degeneration of the glenohumeral joint. An anatomical study. Acta Orthopedica Scandinavica. 1983;54(2):277–283. [ PubMed ] [ Google Scholar ]
- Lo IKY, Litchfield RB, Griffin S, Faber K, Patterson SD, Kirkley A. Quality-of-life outcome following hemiarthroplasty or total shoulder arthroplasty in patients with osteoarthritis: a prospective, randomized trial. The Journal of Bone & Joint Surgery A. 2005;87(10):2178–2185. [ PubMed ] [ Google Scholar ]
- Gartsman GM, Brinker MR, Khan M, Karahan M. Self-assessment of general health status in patients with five common shoulder conditions. Journal of Shoulder and Elbow Surgery. 1998;7(3):228–237. [ PubMed ] [ Google Scholar ]
- Cushnaghan J, Dieppe PA. Study of 500 patients with limb joint osteoarthritis. I. Analysis by age, sex, and distribution of symptomatic joint sites. Annals of the Rheumatic Diseases. 1991;50(1):8–13. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cole BJ, Yanke A, Provencher MT. Nonarthroplasty alternatives for the treatment of glenohumeral arthritis. Journal of Shoulder and Elbow Surgery. 2007;16(5, supplement):S231–S240. [ PubMed ] [ Google Scholar ]
- Boselli KJ, Ahmad CS, Levine WN. Treatment of glenohumeral osteoarthritis. American Journal of Sports Medicine. 2010;38(12):2558–2572. [ PubMed ] [ Google Scholar ]
- van der Meijden OA, Gaskill TR, Millett PJ. Glenohumeral joint preservation: a review of management options for young, active patients with osteoarthritis. Advanced Orthopedics. 2012;2012:9 pages.160923 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Matsen FA, III, Rockwood CA, Jr., Wirth MA, Lippitt SB. Glenohumeral arthritis and its management. In: Rockwood CA Jr., Matsen FA III, editors. The Shoulder. 2nd edition. Philadelphia, Pa, USA: Elsevier Saunders; 1998.pp. 879–888. [ Google Scholar ]
- Denard PJ, Wirth MA, Orfaly RM. Management of glenohumeral arthritis in the young adult. The Journal of Bone & Joint Surgery A. 2011;93(9):885–892. [ PubMed ] [ Google Scholar ]
- McCarty LP, III, Cole BJ. Nonarthroplasty treatment of glenohumeral cartilage lesions. Arthroscopy. 2005;21(9):1131–1142. [ PubMed ] [ Google Scholar ]
- Izquierdo R, Voloshin I, Edwards S, et al. Treatment of glenohumeral osteoarthritis. Journal of the American Academy of Orthopedic Surgeons. 2010;18(6):375–382. [ PubMed ] [ Google Scholar ]
- Silverstein E, Leger R, Shea KP. The use of intra-articular hylan GF 20 in the treatment of symptomatic osteoarthritis of the shoulder: a preliminary study. American Journal of Sports Medicine. 2007;35(6):979–985. [ PubMed ] [ Google Scholar ]
- Zhang W, Jones A, Doherty M. Does paracetamol (acetaminophen) reduce the pain of osteoarthritis?: a meta-analysis of randomized controlled trials. Annals of the Rheumatic Diseases. 2004;63(8):901–907. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pincus T, Koch G, Lei H, et al. Patient Preference for Placebo, Acetaminophen (paracetamol) or Celecoxib Efficacy Studies (PACES): two randomized, double blind, placedo controlled, crossover clinical trials in patients with knee or hip osteoarthritis. Annals of the Rheumatic Diseases. 2004;63(8):931–939. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kelley MJ, Ramsey ML. Osteoarthritis and traumatic arthritis of the shoulder. Journal of Hand Therapy. 2000;13(2):148–162. [ PubMed ] [ Google Scholar ]
- Bishop JY, Flatow EL. Management of glenohumeral arthritis: a role for arthroscopy? Orthopedic Clinics of North America. 2003;34(4):559–566. [ PubMed ] [ Google Scholar ]
- Cameron BD, Iannotti JP. Alternatives to total shoulder arthroplasty in the young patient. Techniques in Shoulder and Elbow Surgery. 2004;5(3):135–145. [ Google Scholar ]
- Cameron BD, Galatz LM, Ramsey ML, Williams GR, Iannotti JP. Non-prosthetic management of grade IV osteochondral lesions of the glenohumeral joint. Journal of Shoulder and Elbow Surgery. 2002;11(1):25–32. [ PubMed ] [ Google Scholar ]
- Richards DP, Burkhart SS. Arthroscopic debridement and capsular release for glenohumeral osteoarthritis. Arthroscopy. 2007;23(9):1019–1022. [ PubMed ] [ Google Scholar ]
- Van Thiel GS, Sheehan S, Frank RM, et al. Retrospective analysis of arthroscopic management of glenohumeral degenerative disease. Arthroscopy. 2010;26(11):1451–1455. [ PubMed ] [ Google Scholar ]
- Weinstein DM, Bucchieri JS, Pollock RG, Flatow EL, Bigliani LU. Arthroscopic debridement of the shoulder for osteoarthritis. Arthroscopy. 2000;16(5):471–476. [ PubMed ] [ Google Scholar ]
- Burgess DL, McGrath MS, Bonutti PM, Marker DR, Delanois RE, Mont MA. Shoulder resurfacing. The Journal of Bone & Joint Surgery A. 2009;91(5):1228–1238. [ PubMed ] [ Google Scholar ]