Introduction: When the knee says stop
Patellar tendinopathy, often nicknamed “jumper’s knee,” is not the exclusive preserve of elite athletes. Although it is common among athletes who jump, run, or make rapid changes of direction, this tendon pathology can also affect people who are active in their daily lives, particularly those whose movement patterns or biomechanics are altered. At the junction of the quadriceps muscle and the tibia, the patellar tendon plays a vital role in transmitting forces from the thigh to the leg, ensuring simple movements such as standing up, climbing stairs, or running. When overused, this tendon becomes irritated, weakened, and even suffers repeated micro-tears. The result: localized, persistent, and sometimes debilitating pain that can become chronic if not properly managed.
Understanding patellar tendinopathy means first recognizing that it is not simply a temporary inflammation. Contrary to popular belief, patellar tendinitis is very rarely an acute inflammation. It is most often a progressive degenerative process, marked by a disorganization of collagen fibers, anarchic vascularization, and a loss of elasticity of the tendon. Pain is not only a reflection of “too much” activity, but also a signal of an imbalance between repeated mechanical stress and the adaptive capacity of the tendon tissue. As such, it becomes crucial not to give in to the temptation of simple rest or systematic anti-inflammatory medication: these solutions can provide temporary relief, but rarely offer lasting improvement.
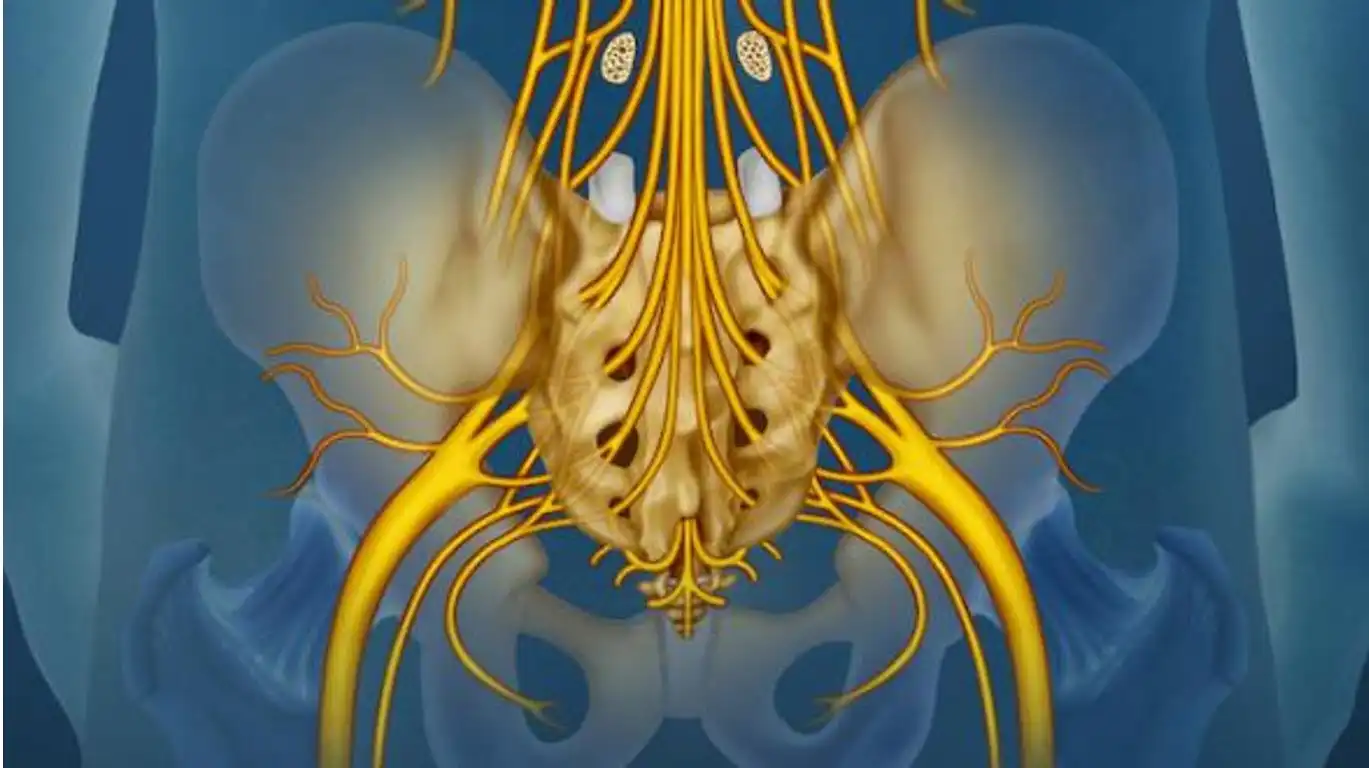
What makes this condition so tricky to treat is that it relies on a constellation of factors. Weak gluteal muscles, poor shock absorption by the foot, an unbalanced pelvis, or even stiffness in the posterior chain can all contribute to overloading the patellar tendon. It is therefore not just a localized injury, but a global functional imbalance. From this perspective, a purely symptomatic approach risks missing the point. This is where osteopathy can play a fundamental role: by identifying and treating the root causes of the imbalance, it gives the body a better ability to regain its dynamic harmony.
But beyond therapeutic intervention, the key also lies in the patient’s active involvement. Adapting training loads, strengthening key muscle groups, correcting technical movements, and improving diet are all elements that contribute to healing. Patellar tendinopathy is not inevitable, but it does require discipline, patience, and consistency. It’s a path that requires listening to the body’s signals, careful guidance, and in-depth reeducation of movements and postures. Effective solutions exist, provided they are integrated into a comprehensive, individualized, and sustainable approach.
In this article, we will explore the various facets of this little-known but common pathology: its mechanisms, warning signs, medical treatments, the specific contribution of osteopathy, as well as preventive strategies to avoid relapses. Drawing on research data, clinical experience, and accessible practical solutions, we will seek to give the patient an active role in their healing process. Because knee pain, as frustrating as it may be, can become an opportunity: that of restoring a more balanced movement, posture, and body awareness.
Understanding Patellar Tendinopathy
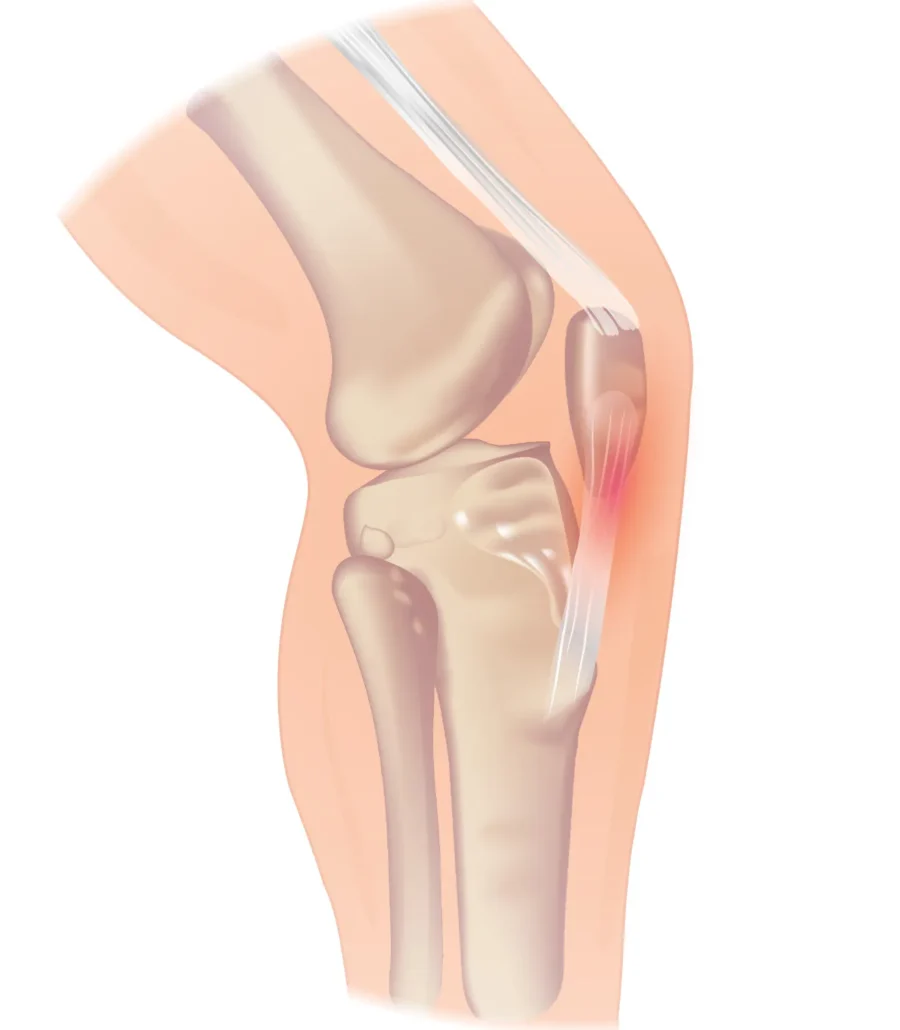
Patellar tendinopathy manifests as pain located in the patellar tendon, just below the kneecap. This condition most often affects people who participate in sports that place a high demand on the lower limbs, such as volleyball, basketball, football, or running. However, it can also affect less athletic individuals, when a mechanical imbalance or excessive stress disrupts the tendon’s ability to adapt. Contrary to popular belief, this condition does not always result from acute inflammation, but rather is part of a chronic process of overload and progressive degeneration of the tendon fibers.
From a pathophysiological perspective, recent research, particularly the work of Cook and Purdam, has proposed a classification of tendinopathy into three progressive stages: reactive, disorganization, and degeneration. The reactive stage corresponds to an early response of the tendon to unusual overload, with temporary thickening due to increased water and protein content. At this stage, pain may appear quickly after physical activity and disappear at rest. If the stresses persist, the tendon enters a phase of disorganization, where the collagen fibers lose their alignment and cohesion. Finally, in the degenerative stage, there is a profound alteration of the tendon structure, with areas of necrosis, anarchic neovascularization, and a loss of tensile strength. The patient then describes persistent pain, sometimes at rest, with a notable decline in functional performance.
The risk factors for patellar tendinopathy are multiple and must be assessed individually. From a biomechanical perspective, quadriceps or gluteal muscle weakness, triceps surae hypertonia, posterior chain stiffness, pelvic tilt, or dynamic valgus can all contribute to abnormal overload of the patellar tendon. Plantar static disorders (flat feet, hyperpronation), imbalances in the abdominal core, or poor coordination of the muscle chains also play a significant role. In addition to these intrinsic factors, there are extrinsic factors such as a sudden increase in training load, unsuitable support surfaces, worn or inappropriate shoes, or technical errors in the sporting movement.
The pain felt is typically well localized at the lower tip of the kneecap, increased by pressure and exacerbated by movements that strongly stress the quadriceps: climbing stairs, running uphill, repeated jumping, squatting. It may initially appear only during exercise, then become permanent if the pathology progresses. The patient often reports a feeling of stiffness or discomfort at the start of the activity, which tends to decrease when warm, only to reappear when cold. This phenomenon is typical of the chronic tendon picture.
Understanding patellar tendinopathy therefore means moving beyond a purely symptomatic view to place the tendon in its overall environment: muscle chain, posture, gestures, lifestyle habits. It also means recognizing that pain is not an enemy to be fought, but an intelligent signal from the body that indicates a loss of balance. By identifying the specific causes for each patient, we can direct treatment toward real functional rehabilitation and prevent the tendon from further damage.
With this in mind, osteopaths have valuable tools at their disposal to identify imbalances that disrupt knee mechanics and restore harmonious function. But for support to be effective, it must be part of a co-construction approach with the patient: understanding, correcting, strengthening, and preventing. The rest of this article will explore these concrete avenues.
Clinical signs and precise diagnosis
When faced with anterior knee pain, it is essential to make an accurate diagnosis. Patellar tendinopathy is characterized by a very specific location of pain, generally centered on the lower tip of the kneecap, at the insertion of the patellar tendon. The patient describes discomfort that appears gradually, often after intense or unusual exertion, and that worsens over time if no treatment is initiated. In early forms, the pain only occurs during or after physical activity, and tends to disappear at rest. But in more advanced cases, it becomes more constant, impacting simple everyday movements such as sitting, climbing stairs, or standing for long periods.
Clinically, examination of the knee reveals marked tenderness upon palpation of the tendon insertion on the patella. This pain is well-focused, sometimes accompanied by slight local thickening or perceptible tension in the tendon. The osteopath may also note discomfort during resisted contraction of the quadriceps or after a prolonged squat. The single-leg decline squat test is particularly useful in this context: performed on a board inclined at 25°, this test places tension on the patellar tendon and typically causes pain on descent, especially when the patient is on the affected leg. It constitutes a simple, reproducible and sensitive tool to guide clinical diagnosis.
To objectify the progression of tendinopathy and assess its functional impact, the VISA-P (Victorian Institute of Sport Assessment for Patellar Tendinopathy) scale is often used. This standardized questionnaire allows the patient’s progress to be monitored over time and the treatment strategy to be adapted. It takes into account not only pain intensity, but also the patient’s ability to engage in sports, limitations in daily life, and tolerance to certain mechanical loads.
In some cases, particularly when pain persists despite proper treatment or when other diagnoses are considered (patellar syndrome, meniscal pathology, referred lumbar pain), imaging tests may be useful. Ultrasound is often the first choice: it allows visualization of tendon thickening, areas of collagen disorganization, and sometimes the presence of calcifications or new vessels. MRI, on the other hand, is more accurate for evaluating all the joint structures of the knee and detecting associated lesions. It can also confirm the stage of tendinopathy according to the Cook & Purdam criteria, which helps to adjust treatment according to severity.
It is important to remember, however, that images never replace clinical examination or careful listening to the patient’s feelings. Pain can be very disabling without abnormalities visible on imaging, just as a pathological tendon on ultrasound can be painless and functional. The goal therefore remains to integrate all the information into a coherent reading, centered on the patient’s experience, posture, activity, and level of commitment to rehabilitation.
Furthermore, differential diagnosis is essential, as several pathologies can mimic patellar tendinopathy. In particular, it will be necessary to eliminate patellofemoral pain, which is more diffuse and often linked to poor patellar centering; growth apophysitis such as Osgood-Schlatter disease in adolescents; or referred pain of lumbar origin, especially if the patient has irradiation or nocturnal pain. Fine palpation, analysis of the gesture, and the practitioner’s ability to listen make all the difference here.
Thus, making an accurate diagnosis means offering the patient a reassuring framework, a clear explanation of their pain, and targeted therapeutic guidance. For the osteopath, it is also the starting point for an individualized support approach, taking into account the mechanical, postural, and emotional factors that contribute to the chronicity of the pain.
Classification by severity
Patellar tendinopathy is often classified based on the severity of symptoms and the impact on physical activity. The most commonly used classification system is the four-stage system proposed by Blazina et al.:
- Stage 1: Pain only after activity, without interference with performance.
- Stage 2: Pain during and after activity, but still able to perform.
- Stage 3: Prolonged pain during and after activity, with decreased performance.
- Stage 4: Complete rupture of the tendon, requiring surgery.
The classification system helps guide treatment options, from conservative approaches such as osteopathy in the early stages to more aggressive treatments, such as surgery, in advanced cases.
Diagnosis of patellar tendinopathy requires a combination of clinical examination, imaging techniques, and differential diagnosis to rule out other pathologies. Below is a description of the main steps in the diagnostic process:
Physical examination
A complete physical examination is the first step in diagnosing patellar tendinopathy. During this process, the healthcare professional typically focuses on identifying classic symptoms of the disease, such as anterior knee pain localized to the patellar tendon, particularly during activities involving jumping, running, or climbing stairs.
Key elements of the physical examination:
- Medical History: The healthcare provider begins by taking a detailed medical history from the patient, including information about symptom onset, severity, and activities that aggravate pain. Athletes or those involved in high-impact sports are at higher risk, and their medical history provides essential information.
- Inspection and palpation: The healthcare professional will inspect the knee for signs of inflammation, swelling, or visible deformities. Palpation of the patellar tendon is crucial. The patient may feel tenderness when the practitioner presses on the tendon just below the kneecap.
- Functional testing: Functional movements such as resisted knee bends, lunges, or extensions can be used to assess pain and mobility. Pain during these movements, particularly at the bottom of the squat or when standing up, is indicative of patellar tendinopathy.
- Quadriceps and hamstring assessment: The strength and flexibility of the quadriceps and hamstrings are assessed, as tightness or weakness in these muscles is often associated with knee problems. A tight quadriceps muscle can increase the load on the patellar tendon, while weak hamstrings can affect the overall balance of the leg muscles.
This examination aims to identify not only the location of the pain, but also the level of stress the patellar tendon experiences during various physical activities. In some cases, the healthcare professional may also assess the biomechanics of the lower limb to identify contributing factors such as poor foot alignment or improper running techniques.
Imaging techniques
Imaging is often used to confirm the diagnosis of patellar tendinopathy, especially when the physical examination is inconclusive or symptoms are chronic. The two most common imaging modalities are ultrasound and magnetic resonance imaging (MRI).
Ultrasound:
Ultrasound is a non-invasive and inexpensive imaging technique that allows for real-time visualization of the patellar tendon. During the ultrasound, the healthcare professional will look for characteristic changes such as:
- Thickening of the patellar tendon.
- Hypoechoic areas (regions that appear darker on ultrasound), indicating tendon degeneration.
- Neovascularization, where new blood vessels form in response to chronic damage, often seen in chronic cases of tendinopathy.
Ultrasound also has the advantage of being dynamic, meaning that the tendon can be assessed in real time during movement, thus providing information on the behavior of the tendon under stress.
Magnetic resonance imaging (MRI) :
MRI is another diagnostic tool used for a more detailed assessment, especially in complex cases or when surgery is being considered. MRI can provide a clearer image of soft tissues and is useful for detecting:
- Micro-tears or ruptures of the tendon.
- Advanced stages of tendon degeneration, called tendinosis.
- Any involvement of surrounding tissues, such as bone marrow edema or fat pad inflammation, which may contribute to or complicate the disease.
Although MRI is more expensive and time-consuming than ultrasound, it provides superior detail, particularly in ruling out other pathologies.
Differential diagnosis
The final step in the diagnostic process is differential diagnosis, which involves ruling out other conditions that may present with similar symptoms. Patellar tendinopathy can be confused with several other knee conditions, making this step crucial for accurate diagnosis and treatment planning.
Common conditions to exclude:
- Patellofemoral pain syndrome (PFPS): Although both conditions present with anterior knee pain, PFPS is usually associated with pain around or behind the kneecap, rather than directly located on the patellar tendon.
- Meniscal tears: A meniscal tear can also cause knee pain, especially during activity, but it is usually associated with mechanical symptoms such as clicking, locking, or knee instability.
- Osgood-Schlatter disease: This condition is common in adolescents and involves inflammation of the growth plate at the tibial tuberosity (just below the knee), rather than the patellar tendon itself.
- Quadriceps tendinopathy: This condition affects the quadriceps tendon located above the kneecap, rather than the patellar tendon located below.
Differential diagnosis ensures that the treatment plan addresses the appropriate underlying problem, thus avoiding unnecessary treatments or interventions.
Osteopathic care for patellar tendinopathy involves both conservative and advanced treatments. Osteopaths focus on promoting natural healing through manual therapies and rehabilitation strategies that improve biomechanics, reduce tendon tension, and improve overall mobility.
Conservative treatments
- Manual therapy: Osteopaths use gentle manipulation techniques to improve joint function and relieve tension around the knee, thereby optimizing the body’s self-healing mechanisms.
- Activity modification: Adjust or limit aggravating activities while the tendon heals.
- Eccentric strengthening exercises: Exercises that help develop quadriceps strength, thereby reducing stress on the patellar tendon.
- Stretching and soft tissue techniques: Osteopathic practitioners may use soft tissue techniques, including myofascial release, to relieve tension in surrounding muscles and tendons.
- Posture and Gait Correction: Osteopaths often assess and correct any abnormal posture or gait that may be contributing to tendon stress, ensuring proper body alignment to prevent further injury.
Advanced treatments
- Shockwave therapy: This non-invasive therapy is sometimes used in osteopathic practices to stimulate tissue repair and reduce chronic pain.
- Dry needling: Some osteopaths use dry needling techniques to reduce muscle tension and promote healing of the affected area.
- Referral for surgical or advanced interventions: In cases where conservative treatments fail, osteopaths may refer patients to specialists for surgical or more advanced treatments, such as platelet-rich plasma (PRP) injections or percutaneous tenotomy.
When a reference is needed
In osteopathy, it is necessary to consult a specialist if conservative treatments do not produce improvement after a few months or if symptoms worsen. Advanced imaging (such as MRI) may be necessary for a more detailed assessment if tendon injuries are suspected to be serious. Additionally, referral is essential when patients present with a complete tendon rupture or when they require advanced interventions such as platelet-rich plasma (PRP) injections, corticosteroid injections, or surgery. An osteopath will refer patients if these conditions exceed the scope of manual therapy and rehabilitation strategies.
Frequently Asked Questions
- What is patellar tendinopathy?
- Patellar tendinopathy is a condition of the patellar tendon, usually characterized by inflammation, microtrauma, or degeneration of the tendon.
- What are the typical symptoms of patellar tendinopathy?
- Symptoms include pain in the front of the knee, tendon tenderness, stiffness, and sometimes swelling.
- What activities can worsen patellar tendinopathy?
- Activities involving repeated jumping, frequent squatting, or a sudden increase in physical activity can aggravate patellar tendinopathy.
- How is patellar tendinopathy diagnosed?
- Diagnosis is based on a clinical examination, medical history, and imaging tests such as X-rays, ultrasound, or MRI.
- What treatments are available for patellar tendinopathy?
- Treatments include rest, osteopathy, ice use, anti-inflammatories, injections, activity changes, orthotics, and, in some cases, surgery.
- How long does it take to heal from patellar tendinopathy?
- Recovery varies depending on the severity of tendinopathy and response to treatment, but can take several weeks to several months.
- Can I exercise while receiving treatment for patellar tendinopathy?
- It depends on the severity of your symptoms. Some activities may be appropriate, but it is essential to follow the advice of your healthcare professional.
- Does patellar tendinopathy require surgery?
- Surgery is rarely necessary, except in cases of severe lesions or non-response to conservative treatments.
- Can patellar tendinopathy be prevented?
- Preventive measures include adequate warm-up, progressive training, strengthening exercises, and correction of biomechanical risk factors.
- When should I see a healthcare professional for patellar tendinopathy?
- A consultation is recommended in case of persistent pain, functional limitations or worsening of symptoms despite self-care measures.
Prevention and rehabilitation of patellar tendinopathy
Prevention of patellar tendinopathy and effective rehabilitation require a combination of lifestyle changes, strengthening exercises, and appropriate recovery strategies. The main approaches include:
- Strengthening and flexibility exercises: Regularly strengthen your quadriceps, hamstrings, and calf muscles to improve knee stability. Eccentric exercises, where the muscles lengthen under tension, are particularly effective.
- Activity modification: Gradually increase the intensity of sports and exercises to avoid overloading the patellar tendon. Incorporating rest days is also essential to avoid overuse.
- Proper Footwear and Posture: Be sure to use supportive footwear during physical activities and maintain proper leg and knee alignment to reduce stress on the patellar tendon.
- Rehabilitation Program: After an injury, a structured rehabilitation plan that includes eccentric exercises, flexibility exercises, and progressive strengthening is essential. It helps improve tendon healing, restore mobility, and prevent recurrence.
- Regular Manual Therapy: Osteopathic manual therapy can be integrated into both prevention and rehabilitation to address muscle imbalances, improve joint function, and support optimal biomechanics.
Radiographic results
In the diagnosis of patellar tendinopathy, radiographic findings can be helpful in assessing the condition of the knee and identifying potential structural abnormalities associated with this condition. However, it is important to note that radiographic findings of patellar tendinopathy can be subtle and may not always fully reflect the severity of the symptoms experienced by the patient.
When examining the knee of a patient with patellar tendinopathy, several signs may be observed. First, osteophytosis, or bone spur formation, may be visible at the lower end of the patella or at the junction between the patella and the patellar tendon. These bone spurs may result from chronic irritation of the patellar tendon and the underlying bone in response to excessive stress.
Additionally, a decrease in joint space between the patella and femur may be observed, which may indicate joint wear associated with patellar tendinopathy. This reduction in joint space may be the result of a decrease in articular cartilage or the presence of calcium deposits in the patellar tendon.
In some cases, signs of biomechanical knee misalignment may also be visible on X-rays. For example, excessive lateral tilt of the kneecap, called patellofemoral syndrome, may be observed, which can contribute to the development of patellar tendinopathy by altering the distribution of forces on the patellar tendon.
It is important to note that although radiographic findings can provide valuable information in the diagnosis of patellar tendinopathy, they are not always specific and may not be present in all patients with this condition. Therefore, other imaging modalities such as ultrasound or MRI may be necessary to more accurately assess the condition of the patellar tendon and surrounding structures.
- Bone spur (enthesophyte): Bony growths, called bone spurs or enthesophytes, may sometimes be visible where the patellar tendon attaches to the kneecap or anterior tibial tuberosity.
- Patellar tendon thickening: An X-ray may show thickening of the patellar tendon, indicating the body’s response to chronic stress on the tendon.
- Abnormal patella position: X-rays may reveal abnormal patella position, such as malalignment of the patella, which may be associated with tendinopathy.
- Joint space widening: In some cases, the joint space between the patella and femur may be widened, suggesting patellar instability.


Conclusion
In conclusion, patellar tendinopathy is a common knee condition that can cause persistent pain and limit participation in daily activities and sports. This condition typically results from a combination of intrinsic and extrinsic factors, including anatomical abnormalities, muscle imbalances, repetitive sports activities, and individual factors such as age and injury history.
Symptoms of patellar tendinopathy primarily include pain around or behind the kneecap, patellar tendon tenderness, joint stiffness, and decreased muscle strength. These symptoms may be exacerbated by certain activities and may vary in intensity depending on the severity of the condition.
The diagnosis of patellar tendinopathy is based on clinical examination, which may be supplemented by imaging tests such as X-rays, ultrasound or MRI to confirm the diagnosis and assess the extent of the lesions.
Treatment for patellar tendinopathy generally aims to relieve pain, reduce inflammation, and restore normal tendon function. Conservative approaches such as relative rest, osteopathy, muscle strengthening exercises, and treatment modalities such as extracorporeal shock wave therapy can be effective in many cases. In more severe cases or those refractory to conservative treatment, surgery may be considered.
References
- Lian OB, Engebretsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005 Apr;33(4):561-7. [PubMed]
- Fredberg U, Bolvig L. Jumper’s knee. Review of the literature. Scand J Med Sci Sports. 1999 Apr;9(2):66-73. [PubMed]
- Ferretti A. Epidemiology of jumper’s knee. Sports Med. 1986 Jul-Aug;3(4):289-95. [PubMed]
- Khan KM, Cook JL, Kannus P, Maffulli N, Bonar SF. Time to abandon the “tendinitis” myth. BMJ. 2002 Mar 16;324(7338):626-7. [ PMC free article ] [ PubMed
- Tibesku CO, Pässler HH. [Jumper’s knee–a review]. Sportverletz Sportschaden. 2005 Jun;19(2):63–71. [ PubMed ]
- van der Worp H, van Ark M, Roerink S, Pepping GJ, van den Akker-Scheek I, Zwerver J. Risk factors for patellar tendinopathy: a systematic review of the literature. Br J Sports Med. 2011 Apr;45(5):446-52. [ PubMed ]
- Rudavsky A, Cook J. Physiotherapy management of patellar tendinopathy (jumper’s knee). J Physiother. 2014 Sep;60(3):122-9. [PubMed]
- Lian O, Engebretsen L, Ovrebø RV, Bahr R. Characteristics of the leg extensors in male volleyball players with jumper’s knee. Am J Sports Med. 1996 May-Jun;24(3):380-5. [PubMed]
- Durcan L, Coole A, McCarthy E, Johnston C, Webb MJ, O’Shea FD, Gissane C, Wilson F. The prevalence of patellar tendinopathy in elite academy rugby: a clinical and imaging study. J Sci Med Sport. 2014 Mar;17(2):173-6. [PubMed]
- Schwartz A, Watson JN, Hutchinson MR. Patellar Tendinopathy. Sports Health. 2015 Sep-Oct;7(5):415-20. [PMC free article] [PubMed]
- Almekinders LC, Temple JD. Etiology, diagnosis, and treatment of tendonitis: an analysis of the literature. Med Sci Sports Exerc. 1998 Aug;30(8):1183-90. [PubMed]
- Fornaciari P, Kabelitz M, Fucentese SF. [Jumper’s Knee]. Praxis (Bern 1994). 2018 Apr;107(9-10):513-519. [PubMed]
- Dixit S, DiFiori JP, Burton M, Mines B. Management of patellofemoral pain syndrome. Am Fam Physician. 2007 Jan 15;75(2):194-202. [PubMed]
- Malliaras P, Cook J, Purdam C, Rio E. Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. J Orthop Sports Phys Ther. 2015 Nov;45(11):887-98. [PubMed]
- Rath E, Schwarzkopf R, Richmond JC. Clinical signs and anatomical correlation of patellar tendinitis. Indian J Orthop. 2010 Oct;44(4):435-7. [PMC free article] [PubMed]