In the palpable silence of the neck, occipital neuralgia orchestrates a symphony of discomfort, challenging the apparent quietude of the head and transforming every movement into a mysterious chapter of pain.
Introduction
What if a sharp pain, located at the base of the skull, could transform every movement of the head into a blinding flash, as destabilizing as it is incomprehensible? Welcome to the world of occipital neuralgia, a still-too-little-known disorder where the line between muscle tension, nerve compression, and chronic suffering blurs.
These pains, often described as electric, burning or pulsing sensations, start at the back of the neck and radiate to the scalp, behind the ears, and even to the temples.
They can appear suddenly, after a trauma or a long period of stress, or they can develop more insidiously, sometimes being confused with migraines or other more classic headaches. This diagnostic vagueness, combined with the general public’s frequent ignorance of this pathology, makes occipital neuralgia particularly confusing.
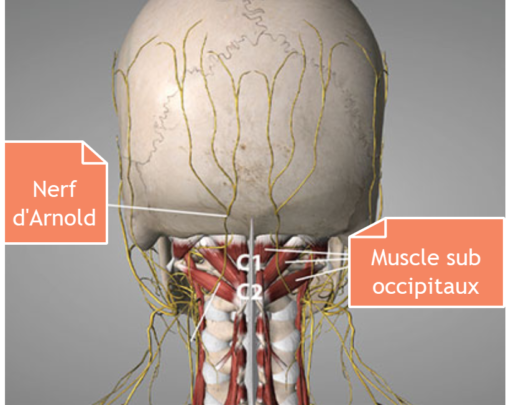
But beyond the pain, there’s an anatomical story. That of the occipital nerves—primarily Arnold’s nerve, also called the greater occipital nerve—which emerge from the first cervical vertebrae (C2 and C3), pass through the suboccipital muscles, and ascend to the scalp. These nerves are like silent sentinels, vulnerable to muscle tension, postural imbalances, and joint abnormalities that mark the cervicocranial region.

In our modern society, dominated by screens, long car journeys, and static postures, the neck pays a heavy price. Hypertonicity of the cervical muscles, spinal misalignments, and chronic tissue compression can create fertile ground for nerve irritation. And it is often there, in this subtle mechanism between bones, muscles, nerves, and fascia, that the origin of occipital neuralgia lies.
But it’s not just a matter of nerves. Occipital neuralgia can also become an emotional and psychological ordeal, affecting quality of life, sleep, concentration, and sometimes even mood. Far from being a simple “headache,” it acts as a silent indicator of a deeper imbalance: in posture, in the pace of life, in the way the body expresses what words sometimes silence.
This article aims to make the invisible visible, to shed light on the anatomical, pathophysiological, and emotional foundations of occipital neuralgia. We will explore its history, mechanisms, clinical forms, as well as the therapeutic approaches—particularly osteopathic ones—that can relieve, support, and prevent this condition.
Whether you’re a healthcare professional, a patient, or simply curious to understand this particular form of head pain, this dive into the heart of the occipital nerves will provide you with the keys to better recognize, understand, and treat it. Because behind every pain lies a message. And sometimes, that message begins… in the back of the head.
From Antiquity to Today: Historical Traces of Occipital Pain
The history of occipital neuralgia is not linear, nor is it even clearly documented under this name. Rather, it is part of a larger body of early descriptions of headaches, head pain, or “pain in the back of the head.” This historical vagueness reflects both the limitations of medical knowledge at the time and the difficulty in distinguishing the different origins of headaches.
In ancient Greece, Hippocrates himself mentioned various head pains in his writings. While the terms used do not allow for precise identification of occipital neuralgia, some passages mention localized headaches, sometimes described as “sharp” or “burning,” which could correspond to neuropathic pain. These manifestations were often interpreted in the context of humoral imbalances—black bile, blood, phlegm—rather than as specific nerve irritations.
Similarly, in Indian Ayurvedic medicine or traditional Chinese medicine, we find descriptions of pain in the neck and base of the skull, sometimes associated with energy imbalances or blockages in the flow of qi. The Huangdi Neijing , a foundational text of Chinese medicine dating back approximately 2,000 years, discusses the meridians connecting the neck and head, emphasizing the importance of tension in this area for overall health. Although neither of these texts identifies the occipital nerve as such, their clinical observations demonstrate a long-standing attention to this anatomical region.
It was not until the emergence of modern anatomical medicine, beginning in the 16th century, that the cervical nerves were described more precisely. Andreas Vesalius, a pioneer of human anatomy, and later Thomas Willis and other 17th-century anatomists, helped to detail the connections between the spinal nerves and the structures of the skull. However, it was not until the 19th century, with the rise of clinical neurology, that occipital neuralgia began to be recognized as a distinct entity.
The term “Arnold’s neuralgia” then appeared in the medical literature, in reference to the German physician Friedrich Arnold (1803–1890), who described the greater occipital nerve. This nerve gradually became a diagnostic target in cases of neck pain radiating to the skull. It was in this context that the first targeted therapeutic approaches emerged, including local infiltrations, massages, and then surgical interventions.

In the 20th century, improvements in medical imaging and dissection techniques led to a better understanding of the complexity of the nerve pathways in the cervicocranial region. It was then understood that occipital pain can be triggered not only by direct nerve damage, but also by postural disorders, muscle tension, or joint abnormalities.
Even today, occipital neuralgia is sometimes underdiagnosed or confused with other forms of headaches, such as cervicogenic migraines. Yet its long and discreet history testifies to an ancient condition, often misinterpreted, but deeply rooted in our human condition.
Inside the Neck: Anatomy of the Occipital Nerves and Associated Structures
To understand occipital neuralgia, it’s essential to delve into the anatomy of the neck, a true crossroads between the cervical spine, peripheral nervous system, and vascular network. It’s in this region, at the junction between the skull and cervical vertebrae, that the pain so characteristic of this condition originates.
The occipital nerves: protagonists of pain
The occipital nerves are central to the clinical picture. The best known, the greater occipital nerve (or Arnold’s nerve), originates at the posterior root of the second cervical vertebra (C2) . It emerges between the deep muscles of the neck, crosses the semispinalis capitis muscle, then the occipital fascia, to innervate the skin of the scalp in the occipital region.
Right next to it is the lesser occipital nerve , which originates from the cervical plexus , more precisely from the ventral branch of C2 (and sometimes C3 ). This nerve runs along the posterior edge of the sternocleidomastoid muscle to also reach the posterior region of the head, but more laterally, near the mastoid.
The suboccipital muscles: tonic guardians of the skull
The suboccipital region is richly populated with small, deep muscles that provide stability, orientation, and fine mobility to the head. These include:
- The posterior rectus capitis muscle
- The posterior rectus capitis
- The superior and inferior oblique muscles of the head
These muscles form an anatomical triangle called the suboccipital triangle , a critical area crossed by Arnold’s nerve. In the event of spasms, tensions or contractures , they can become a direct source of nerve compression.
The upper cervical vertebrae: articulation and vulnerability
The C1 (atlas) and C2 (axis) vertebrae play a pivotal role in head mobility. The greater occipital nerve passes between these two structures. Any joint imbalance (loss of mobility, blockage, early osteoarthritis) can then contribute to nerve irritation. These vertebrae are also heavily used during rotational movements of the head.
Connective tissues and fascia: tension in the background
Around these nervous and muscular structures extends a network of fascia, ligaments and membranes , which participate in the transmission of forces and the maintenance of postural balance. The deep cervical fascia , in particular, surrounds the suboccipital muscles and can become the site of chronic tension, promoting compression of Arnold’s nerve.
Blood vessels: sometimes intrusive partners
The suboccipital region is also traversed by several blood vessels, including the vertebral artery and occipital veins . In certain situations, such as vascular congestion or local inflammation, these structures can increase pressure on nearby nerves.
Understanding the mechanical and functional causes of nerve irritation
Occipital neuralgia is a disorder whose origins may seem mysterious at first glance, as its symptoms are so varied and sometimes confused with those of other headaches. However, by exploring the underlying mechanical and functional causes, a coherent pattern emerges. This pain at the base of the skull, often unilateral, shooting, or dull, is largely explained by complex interactions between nerves, muscles, joints, and connective tissues.
Occipital nerve compression: the trigger
Common to many cases of occipital neuralgia is compression or irritation of the greater occipital nerve , sometimes the lesser nerve. The greater occipital nerve emerges between the second and third cervical vertebrae (C2-C3), passes through a series of dense anatomical structures, and then ascends to the scalp. Along this path, it may be compressed or irritated by various anatomical structures.
Among the most common causes of compression are:
- Muscle spasms , especially of the suboccipital muscles;
- Fascial fibrosis or thickening in the posterior cervical region;
- Cervical osteoarthritis with the presence of bone spurs;
- Chronic postural imbalances ;
- A high cervical disc herniation or protrusion , exerting indirect pressure on the nerve roots.
This compression results in hypersensitization of the nerve , causing acute pain or paresthesias that spread along its innervation territory, often to the crown of the skull.
Chronic Muscle Tension: The Silent Role of Stress and Posture
Hypertonia of the cervical muscles is a major but often overlooked cause. In our modern daily lives, where screens reign supreme and stress is omnipresent, the suboccipital muscles are particularly stressed. These small, deep muscles act as stabilizers for the head, and prolonged posture with the head tilted forward (reading, screen time, or driving) keeps them in almost permanent contraction.
Over time, this constant tension ends up irritating the adjacent nerves, particularly Arnold’s nerve. The situation can be exacerbated by stress, which increases overall muscle tone, and by poor ergonomics at work or home.
Repetitive movements, microtraumas and functional overload
Certain occupations or sports activities expose individuals to repetitive neck movements , creating cumulative microtraumas . Each excessive stress disrupts the balance between joint mobility, muscle elasticity and nerve adaptation. Over time, these movements can cause reactive muscle spasms or soft tissue inflammation , adding to existing nerve compression.
Head drop syndrome , observed in certain neurological pathologies or in weakened elderly people, is a sign of this functional overload. Actively maintaining the head becomes difficult, forcing the cervical muscles to constantly compensate, often at the cost of extreme tension.
Cervical joint imbalances: alignment to monitor
The C1 (atlas) and C2 (axis) vertebrae play a crucial role in the head’s freedom of movement. When these joints lose their mobility—through blockage, trauma, or joint aging—this can alter the normal dynamics of the occipital nerve. Even slight misalignments can be enough to generate friction, mechanical conflicts, or local tension, worsening nerve irritation.
These imbalances are all the more insidious because they are not always noticeable without a precise clinical examination. Osteopathy, thanks to its precise tissue and joint assessment, can play a leading role in detecting these mobility restrictions.
Neurovascular interactions: when vessels complicate the picture
Sometimes blood vessels near the nerve (such as branches of the occipital artery) exert additional pressure on the nerve, especially if congestion, inflammation, or a vascular reaction is present. This phenomenon, often difficult to objectify by imaging, is nonetheless real and can explain the recurrence or resistance to treatment of certain neuralgias.
The different faces of occipital neuralgia: clinical forms and specificities
Behind the generic term “occipital neuralgia” lies a much more nuanced reality. It is not a single pathology, but rather a syndrome with multiple expressions , whose presentation varies depending on the causes, location, intensity of pain, and the structures involved. Identifying the precise clinical form of occipital neuralgia not only helps guide the diagnosis, but also allows for more targeted treatment.
Primary occipital neuralgia
Primary occipital neuralgia is the most classic and most frequent form . It is often described as:
- Unilateral or bilateral pain at the base of the skull;
- Radiating upwards from the scalp, sometimes behind the eye or toward the temples;
- Pulsating, burning or shooting, like an electric shock;
- Accompanied by local hypersensitivity (allodynia) or pain to light touch.
This type of neuralgia can appear without any obvious cause. It is then called an idiopathic form , although an osteopathic examination often reveals muscle tension, joint restrictions or postural imbalances that contribute to its onset.
Secondary occipital neuralgia
Here, the pain is a symptom of another identifiable medical condition , such as:
- Cervical osteoarthritis (spondylosis) with osteophyte formation;
- Cervical trauma (whiplash, fall, sprain);
- Tumor or cyst compressing the cervico-occipital region;
- Myofascial syndrome with trigger points in the suboccipital muscles;
- High disc herniation .
Treatment of secondary neuralgia must first address the underlying cause , while relieving symptoms. This form sometimes requires interdisciplinary work (physician, osteopath, neurologist).
Arnold’s neuralgia (or Arnold’s syndrome)
Sometimes used as a synonym for major occipital neuralgia, this term more specifically refers to irritation of Arnold’s nerve , that is, the greater occipital nerve .
Typical signs are:
- Very localized pain along the path of the nerve (from C2 to the top of the skull);
- Pain triggered by pressure on the area just below the occiput;
- Sometimes a feeling of cold, tingling or burning.
Direct involvement of Arnold’s nerve often warrants the use of diagnostic anesthetic blocks , which help confirm the nerve source of the pain.
Occipital cervicogenic neuralgia
Here, the pain originates in the joint structures of the cervical spine , but radiates to the occipital region. It is often:
- Associated with vertebral dysfunctions (C1-C2, C2-C3);
- Related to loss of mobility or misalignment;
- Exacerbated by neck movements;
- Accompanied by cervical stiffness.
This form is particularly receptive to osteopathic treatment , which aims to restore joint mobility and reduce mechanical tension.
Occipital nummular neuralgia
Less common, this variant manifests itself by pain located in a restricted area , circular or oval in shape , generally at the back of the skull.
Unlike classic forms, the pain will not necessarily radiate along the scalp. It remains localized in a well-defined area, often a few centimeters in diameter. This form is sometimes linked to a muscular or cutaneous trigger point , or to a local alteration of the peripheral nerves.
Occipital neuralgia and migraine
In some cases, occipital neuralgia coexists or is confused with migraines . Patients may experience throbbing pain in the occipital region, accompanied by:
- Nausea;
- Photophobia (sensitivity to light);
- Dizziness or visual disturbances.
It is important to distinguish between migraine and neuralgia because the therapeutic approaches differ . However, chronic neuralgia can also become a trigger for migraine attacks in some people.
Post-traumatic neuralgia
This form appears after a head or neck trauma , sometimes even mild. It can develop:
- Immediately after the shock;
- Or in a delayed manner, weeks later.
Pain can be persistent, localized or diffuse, and often associated with other post-traumatic symptoms (sleep disorders, concentration problems, anxiety). Treatment must take into account the entire traumatic experience , including emotional ones.
Occipital neuralgia of dental or mandibular origin
Less well known, this form is linked to tensions in the temporomandibular joint (TMJ) or to occlusal disorders, such as bruxism. Poor coordination of the craniocervical muscle chains can generate tensions that affect the occipital nerve.
Characteristic signs: recognizing occipital neuralgia
Occipital neuralgia is distinguished by specific symptoms, which are still too often misunderstood or confused with other types of headaches. However, it has well-defined clinical features that, when correctly identified, can guide diagnosis and treatment. Recognizing these signs is essential for both professionals and patients themselves.
A typical pain at the base of the skull
The central symptom is pain located in the occipital region , that is, at the back of the head, often at the junction between the skull and the neck. This pain is usually unilateral , but can also be bilateral in some cases. It can occur suddenly or develop gradually.
Patients describe this pain as:
- Throbbing, throbbing, or electric , like a shock rising from the neck to the scalp;
- Sometimes burning or stinging , suggesting nervous irritation rather than simple muscular tension;
- Radiating to the top of the skull , the temporal region, or even behind the eye;
- At times paroxysmal , that is to say occurring in crises, interspersed with phases of respite.
This radiating and fulminating character distinguishes occipital neuralgia from a classic headache, which is more diffuse or heavy.
Increased sensitivity to palpation
A common sign found during clinical examination is tenderness to pressure over the greater occipital nerve exit area, located a few centimeters from the external occipital protuberance. Simply palpating this area can reproduce pain or cause a sharp sensation, a sign of nerve involvement.
Additionally, the scalp in the back of the head may be hypersensitive , sometimes to simple touch, such as the passage of a comb or the rubbing of a pillow. This phenomenon, called allodynia , is common in neuropathic pain.
Pain triggered by certain movements
Certain head and neck movements can exacerbate pain , particularly:
- Cervical rotations and extensions;
- Prolonged posture with the head tilted forward (e.g., working on a screen, reading);
- Rapid movements or efforts to straighten up.
This postural worsening is an additional clue that allows us to suspect a mechanical or myotensive origin of the neuralgia, often linked to the suboccipital muscles.
Neck stiffness and restricted mobility
Even if the pain is of nervous origin, it is often accompanied by stiffness in the neck . The patient may experience discomfort when turning the head, looking up, or maintaining certain postures. This functional limitation is linked to the associated muscular tension, but also to a possible loss of mobility of the upper cervical vertebrae (C1-C2).
Possible associated symptoms
In some cases, occipital neuralgia may be accompanied by other less specific signs, but revealing a broader condition:
- Persistent headaches , sometimes confused with migraines;
- Transient visual disturbances , such as blurred vision or light discomfort;
- Dizziness or feelings of instability , especially when the pain is intense;
- Nausea , linked to the intensity of the pain or to the posture maintained.
It is important to distinguish these symptoms from those of other, more serious pathologies. This is why a thorough clinical examination , accompanied if necessary by medical imaging, is recommended in case of doubt.
Pain often misidentified
Unfortunately, occipital neuralgia is still poorly diagnosed , often confused with migraines, tension headaches, or isolated musculoskeletal disorders. This confusion delays the implementation of appropriate treatment and can lead to chronic pain.
What are the common causes of occipital neuralgia?
Occipital neuralgia, although it may appear suddenly or unexplained, most often results from a combination of mechanical, functional, or pathological factors that exert pressure or irritation on the occipital nerves. Identifying common causes is essential not only for making an accurate diagnosis, but also for guiding long-term therapeutic management.
Chronic muscle tension and spasms
The suboccipital muscles play a major role in maintaining head posture. Their chronic contraction, linked to poor posture, stress or visual overload (prolonged time in front of a screen, driving, reading), is one of the leading causes of occipital neuralgia. By shortening or spasming, these muscles can directly compress the occipital nerves , causing stabbing pain, often unilateral.
This tension is commonly seen in people who adopt a forward head posture or work in unergonomic environments.
Cervical joint dysfunctions
The upper cervical vertebrae , particularly C1 (atlas) and C2 (axis) , form a critical passage area for the greater occipital nerve. Any mobility restriction, misalignment, or joint blockage at this level can irritate or compress the nerve.
These malfunctions can occur following:
- From trauma (whiplash, fall, cervical shock);
- From a sudden or poorly controlled movement;
- Poor nighttime support (unsuitable pillow, prolonged twisting of the neck).
Prolonged poor posture
Maintaining a prolonged static posture with the head tilted forward or turned to one side is an insidious, but common cause. This includes:
- Non-ergonomic computer work;
- Intensive use of mobile phones;
- Reading in a slumped position.
This posture puts constant pressure on the posterior cervical region and can trigger or maintain neuralgia.
Cervical osteoarthritis and bone abnormalities
Joint aging , often accompanied by cervical osteoarthritis , can lead to the formation of osteophytes (bony spurs) or narrowing of the intervertebral foramina, where nerves pass.
These anatomical changes can compress the C2 or C3 nerve roots , causing secondary occipital neuralgia. This is a common cause in older people or those with a history of chronic neck pain.
Cervical disc herniation or protrusion
Although rarer in the upper cervical spine, a herniated disc located at the C2-C3 level can exert direct pressure on the nerve root of the occipital nerve. This type of nerve root compression can generate pain similar to that of occipital neuralgia, sometimes accompanied by paresthesia or motor disturbances.
Craniocervical trauma
A direct blow to the back of the head, a fall on the buttocks with indirect impact on the cervical spine, or a car accident can cause post-traumatic neuralgia , linked to:
- Local irritation of the nerve;
- Persistent inflammation;
- A reflex tension of the cervical muscles.
These pains can occur immediately after the trauma, or in a delayed manner, several days to several weeks later.
Underlying pathologies or rare compressions
Less commonly, certain medical conditions can cause occipital neuralgia, including:
- A tumor or cyst in the cervicocranial region;
- A vascular malformation compressing a nerve;
- A viral infection (shingles), which can irritate the posterior cervical nerves.
These causes should be considered if the pain is atypical, resistant to treatment, or accompanied by unusual neurological signs.
Assessing occipital neuralgia: clinical diagnosis and further investigations
Faced with pain located at the base of the skull, radiating towards the scalp, the diagnosis of occipital neuralgia deserves rigorous clinical attention . Often confused with migraines, tension headaches or cervicogenic pain, it requires a structured approach, combining attentive listening , targeted physical examination , and, when necessary, additional tests to confirm the nervous origin of the pain.
Anamnesis: the first step in discernment
The patient interview is a valuable opportunity. It allows us to gather information about the characteristics of the pain, its triggers, its frequency, its progression, as well as personal history.
Elements to explore:
- Location of pain : usually unilateral, at the base of the skull, radiating to the top of the skull, sometimes behind the eye.
- Quality of pain : Often described as shooting , stabbing , electric , or burning .
- Duration and frequency : paroxysmal pain or continuous pain interspersed with attacks.
- Triggers : head movements, prolonged posture, stress, pressure on the neck.
- Associated symptoms : scalp hypersensitivity, blurred vision, dizziness, nausea, photophobia, sleep disturbances.
- Traumatic history : whiplash, fall, head impact.
The anamnesis also aims to eliminate possible serious secondary causes (tumor, infection, vascular damage), which would require urgent treatment.
Clinical examination: precision of gesture and listening to the body
The physical examination primarily targets the craniocervical region . It allows for the identification of suggestive clinical signs and the differentiation of occipital neuralgia from other pathologies.
Key tests and observations:
- Palpation of the greater occipital nerve exit points : pain when pressing a point approximately 2-3 cm from the external occipital protuberance, slightly outside the midline.
- Assessment of scalp sensitivity : detection of allodynia (pain to simple touch) or localized hypoesthesia.
- Cervical mobility tests : look for stiffness, joint blockage or pain increased by certain amplitudes (extension, rotation).
- Muscle examination : detection of tension or spasms in the suboccipital, trapezius, splenius or SCM muscles.
- Search for myofascial trigger points : differentiating referred muscle pain from true neuralgia.
In osteopathy, manual tissue examination also allows us to identify areas of fascial tension , restrictions in spinal mobility , or global postural imbalances which contribute to nerve irritation.
Additional examinations: to be used in a targeted manner
In case of diagnostic doubt or suspicion of a secondary cause, the practitioner may refer to imaging tests:
- Cervical MRI : to visualize soft structures, discs, nerve roots and look for compressions or abnormalities (hernia, cyst, tumor).
- CT scan : useful in cases of suspected bone damage or advanced cervical osteoarthritis.
- Cervical X-rays : Less accurate, but may show postural abnormalities, loss of cervical curvature, or signs of instability.
- Electromyogram (EMG) : Rarely used, but can help assess nerve activity if peripheral neuropathy is suspected.
In more complex cases, a diagnostic nerve block may be suggested by a specialist physician. This involves injecting a local anesthetic into the occipital nerve. If the pain temporarily disappears, this confirms the direct involvement of the nerve in the symptoms.
The diagnostic nerve block test
This procedure, which is both diagnostic and therapeutic, can be considered in collaboration with pain specialists.
Relieve pain at home: heat, posture, stretching and relaxation
When occipital pain sets in, it can become a hindrance to daily life. Fortunately, some simple and natural actions can help soothe discomfort at home. While they are not a substitute for professional therapeutic monitoring, these tools help reduce tension , prevent worsening , and restore a sense of well-being .
Heat or cold: calm inflammation and relax tissues
Applying heat or cold to the painful area is one of the most accessible and effective reflexes.
- Heat (hot water bottle, heating pad) relaxes tense muscles, stimulates blood circulation, and helps loosen contracted fascia. It is particularly useful if the pain is related to chronic muscle tension.
- Cold (ice pack wrapped in a thin cloth) is indicated in cases of acute pain or visible inflammation, for example after a sudden trigger episode or trauma.
Practical advice: Apply heat or cold for 15 to 20 minutes, 2 to 3 times a day, without ever placing it directly on the skin to avoid burns or frostbite.
Conscious posture: reducing pressure on the neck
Poor posture is often the cause or cause of occipital pain. Whether you’re sitting, standing, or lying down, certain habits can make all the difference.
- Sitting: Keep your feet flat, your back straight, your shoulders relaxed, and your chin slightly tucked in. Use an ergonomic backrest if possible.
- Standing: distribute your weight equally on both feet, avoid throwing your head forward.
- Lying down: Choose an ergonomic pillow that supports the natural curvature of your neck. Sleeping on your back or side is preferable, rather than on your stomach.
Tip: Set a visual reminder on your desk or phone to regularly correct your posture throughout the day.
Gentle stretching: releasing accumulated tension
Simple exercises, performed daily, can help restore flexibility to the neck muscles and improve joint mobility.
Examples of suitable stretches:
- Lateral neck tilt
- Slowly tilt your head toward your right shoulder, without shrugging your shoulder.
- Hold for 15 to 30 seconds, then switch sides.
- Forward bend
- Gently tilt your chin toward your chest.
- Feel the stretch in the back of your neck. Hold for 20 seconds.
- Smooth rotation
- Turn your head to the right, without forcing, then to the left.
- Repeat 3 to 5 times on each side.
- Upper Trapezius Self-Stretch
- Place your right hand on your head, pull slightly to the right, lowering your left shoulder.
- Take a deep breath. Hold for 20 to 30 seconds.
Caution: Stop any movement that increases pain. Stretching should be gradual, without jerking.
Relaxation and breathing: calming the nervous system
Chronic pain is often accompanied by a heightened state of alertness of the autonomic nervous system. Learning to slow down can reduce muscle tension and pain perception.
Techniques to explore:
- Diaphragmatic Breathing
Lie down or sit comfortably. Inhale slowly through your nose, feeling your belly expand. Exhale gently through your mouth. Repeat for 5 to 10 minutes. - Cardiac coherence
Inhale 5 seconds, exhale 5 seconds, for 5 minutes, 3 times a day. - Progressive muscle relaxation
Successively contract and release different areas of the body (shoulders, neck, jaw), concentrating on the feeling of relaxation. - Guided meditation or body scan:
Use apps or videos to guide you. These practices promote mental calm and bodily reconnection.
Create a healing space at home
Finally, relieving pain at home also involves creating a space conducive to rest : soft lighting, a calm atmosphere, supportive cushions, relaxing essential oils (such as lavender or peppermint), soothing music… Every detail counts to send a message of safety to the nervous system.
The psychological impact of chronic occipital pain
Chronic occipital pain is not limited to physical discomfort located at the base of the skull. When it becomes persistent, it becomes part of a person’s daily life and can profoundly affect their emotional, cognitive, and social balance. In a comprehensive and humanistic approach to health, it is essential not to dissociate pain from the psychological experience it generates, because the two dimensions constantly influence each other.
A pain that exhausts the mind
Living with chronic pain, even localized pain, constantly demands attention. Occipital pain can occur upon waking, persist throughout the day, and disrupt sleep at night. This omnipresence ultimately impairs concentration, working memory, and the ability to plan ahead. The person becomes more irritable, more tired, and less available to themselves and others.
Added to this is often a lack of understanding from those around them. Occipital pain is not always visible, and because it is located in a little-known area, it is sometimes minimized. The patient may then feel isolated, or even guilty for not being able to “overcome” this suffering. This form of invisibility reinforces the discomfort.
Anxiety and bodily hypervigilance
Persistent pain in the cervical and cranial region can quickly become a source of anxiety. Concern about the origin of the pain, fear of a serious illness, or the anticipation of a new painful episode fuels constant psychological tension. This anxiety can itself increase muscle tone, particularly in the trapezius, neck, and suboccipital muscles, thus perpetuating the pain through a vicious cycle.
The individual also develops hypervigilance of the body. They begin to scrutinize the slightest sensation, avoid certain movements, and restrict their activities for fear of triggering pain. This reduction in activity can ultimately lead to muscular maladaptation, a loss of body confidence, and social or professional limitations.
Depressive risk and withdrawal
Chronic occipital pain, by impacting quality of life, can lead to depressive mood. Feelings of helplessness, decreased energy, altered sleep, and loss of interest in previously enjoyable activities are all signs that should be taken seriously. Progressive isolation exacerbates this picture, particularly in people whose pain has not received satisfactory medical recognition.
It’s important to note that depression isn’t just a consequence of pain; it can also amplify the perception of pain. Studies have shown that negative emotions alter how the brain interprets pain signals, increasing sensitivity to pain.
The importance of an integrative approach
Faced with these psychological impacts, a purely biomechanical approach is not enough. It is essential to integrate an emotional and relational dimension into the support of patients suffering from chronic occipital neuralgia. This includes:
- Attentive and empathetic listening, without judgment.
- A recognition of the reality of pain, even in the absence of a clearly visible cause.
- Multidisciplinary work including, if necessary, a psychologist, body therapist, or pain doctor.
- The introduction of stress management techniques: relaxation, cardiac coherence, mindfulness meditation, conscious breathing.
- Therapeutic education: better understanding pain often allows you to better experience it and regain some control.
A therapeutic space for reconstruction
Osteopathy, when practiced with a stance of respect, non-intrusion, and presence, can provide a framework conducive to this reconstruction. Touch, when reassuring, can help soothe hypervigilance, release anxiety-related tension, and promote better regulation of the autonomic nervous system.
Chronic occipital pain reminds us that the body and mind are inextricably linked. By caring for one, we positively influence the other. It is in this integrative approach that the possibility opens up not only to relieve, but also to transform the experience of pain into a path of knowledge, regulation… and sometimes, resilience.
Relief without surgery: conservative treatments and comprehensive approaches
- Drugs :
- Pain relievers: Over-the-counter medications, such as acetaminophen, can be used to relieve mild to moderate pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs, such as ibuprofen, can reduce inflammation and relieve pain.
- Nerve-specific pain relievers: Certain medications, such as tricyclic antidepressants or antiepileptics, may be prescribed to treat nerve pain.
- Nerve Block:
- Diagnostic or therapeutic nerve blocks, performed by local injection of anesthetic, can temporarily relieve pain by blocking nerve signals.
- Osteopathy:
- Osteopathy sessions can help restore the structural balance of the body, particularly in the cervical region, which can help relieve pressure on the occipital nerve.
- Manual Therapy:
- Manual therapy techniques, such as gentle spinal manipulation, can be used to improve cervical joint mobility.
- Stress Management Techniques:
- Relaxation, meditation, biofeedback, and other stress management techniques can help reduce muscle tension and lessen the perception of pain.
- Posture and Ergonomics:
- Adjusting postural habits and improving ergonomics at work can reduce pressure on the cervical region.
- Heat or Ice:
- Applying hot or cold compresses can provide temporary relief by reducing inflammation and easing pain.
- Lifestyle Education:
- Patient education about lifestyle modifications, such as adjusting daily activities and adopting ergonomic postures, can help prevent painful episodes.
The osteopathic approach: release, realign, relieve
Occipital neuralgia, as a pain of nerve origin, is not simply a localized inflammation. It is often the result of a broader imbalance involving muscle tension, joint restrictions and alterations in overall mobility. Osteopathy, as a comprehensive manual therapy, is well positioned to act on the root causes , while providing lasting relief .
A global reading of the body, beyond the painful area
Unlike a purely symptomatic approach, the osteopath is not only interested in the occipital pain itself. He seeks to understand the origin of the imbalance : a restriction of cervical mobility? A compensated locking of the pelvis up to the head? Chronic stress that would increase the overall muscle tone? Osteopathy is based on an interconnected reading of the body , where each region can influence another from a distance.
Thus, when treating occipital neuralgia, the osteopath assesses not only the cervicocranial region, but also the areas likely to maintain upward tension: diaphragm, thorax, pelvis, plantar supports . The aim is to restore the mechanical and functional harmony of the body as a whole .
Release deep muscular tension
The suboccipital muscles (rectus minor and rectus femoris, superior and inferior obliques), which are heavily used to maintain head posture, are often in chronic contraction . This tension can lead to compression of the greater occipital nerve, causing or maintaining pain.
The osteopath uses specific techniques to relax these deep muscles , often inaccessible to classic self-massage. This may include:
- Myofascial release techniques : gentle and progressive work on fascia and soft tissues.
- Muscle inhibitions : targeted pressure on tension points to deactivate reflex contraction zones.
- Assisted stretching , adapted to the breathing rhythm, promoting relaxation of the posterior chains.
These techniques help reduce nerve compression , improve local vascularization, and create lasting relief in the area.
Restore joint mobility: realign without forcing
An important part of osteopathic work consists of reharmonizing joint mobility , particularly that of the C0-C1, C1-C2 and C2-C3 vertebrae . These segments play a crucial role in the passage of the occipital nerve, and their loss of mobility can create friction or repeated micro-compression.
The techniques used are gentle, precise and unforced , aiming to restore fluid and symmetrical movement. In some cases, the osteopath may resort to structural manipulations (high velocity low amplitude), but always after a rigorous assessment of contraindications.
This joint work is often accompanied by a global postural rebalancing , so that the neck is no longer under permanent overload. The osteopath can thus intervene on the pelvis, the thorax, or even the jaw (TMJ) if it contributes to the ascending tensions.
Soothe the autonomic nervous system
Chronic pain, especially when it affects an area as sensitive as the neck, can activate the sympathetic nervous system , leading to hypervigilance, fatigue, and difficulty releasing tension.
Osteopathy also acts on this dimension, in particular by:
- Cranial techniques , aimed at regulating membranes and nerve flows;
- Visceral or diaphragmatic techniques , promoting better breathing and deep relaxation;
- A caring therapeutic presence , which allows the patient to regain a state of inner security.
Long-term support
Finally, osteopathy is part of an educational and empowering approach . The osteopath can recommend stretching exercises, postural adjustments, or stress management strategies adapted to each individual.
Preventive stretching: release cervical tension and prevent recurrence
Muscle stretching can play a role in preventing suboccipital neuralgia by promoting flexibility and reducing muscle tension in the cervical region. Here are some specific stretches that target the suboccipital muscles to help prevent tension and irritation of the occipital nerve:
- Seated Neck Stretch:
- Sit comfortably on a chair.
- Gently tilt your head to one side, trying to bring your ear closer to your shoulder.
- Hold the position for 15 to 30 seconds, feeling the stretch in the side of your neck.
- Repeat on the other side.
- Standing Neck Rotation:
- Stand with feet shoulder-width apart.
- Slowly turn your head to the left, trying to look over your shoulder.
- Hold the position for 15 to 30 seconds, then rotate to the other side.
- Repeat the movement several times.
- Forward Head Tilt:
- Sit or stand in a neutral position.
- Gently tilt your head forward, bringing your chin toward your chest.
- Hold the position for 15 to 30 seconds, feeling the stretch in the back of your neck.
- Return to the neutral position.
- Back Head Stretch:
- Standing or sitting in a neutral position.
- Gently tilt your head back, looking up at the ceiling.
- Hold the position for 15 to 30 seconds, feeling the stretch in the front of your neck.
- Return to the neutral position.
- Seated Rotation Stretch:
- Sit with your back straight.
- Gently turn your head to one side, using your hand to apply light pressure.
- Hold the position for 15 to 30 seconds, feeling the stretch in the side of your neck.
- Repeat on the other side.
- Standing Trapezius Stretch:
- Stand with feet shoulder-width apart.
- Gently tilt your head to one side while lowering the opposite shoulder.
- Hold the position for 15 to 30 seconds, feeling the stretch in the side of the neck and trapezius.
- Repeat on the other side.
It is important to practice these stretches gently and gradually, avoiding sudden movements.

Cross-pain: interactions between neuralgia and myofascial syndrome
Occipital neuralgia, classically considered as neuropathic pain, and myofascial syndrome , identified as muscular pain of tissue origin, seem a priori to belong to two different worlds. However, in clinical practice, these two entities frequently intertwine , feeding off each other, and complicating the pain picture. Understanding their interactions is therefore fundamental to making an accurate diagnosis and implementing truly effective treatment.
Two mechanisms, one common suffering
Occipital neuralgia is caused by irritation or compression of the occipital nerve , often at its emergence between the C2 and C3 vertebrae, or through the suboccipital tissues. It manifests as a sharp pain, sometimes like an electric shock, radiating to the scalp.
Myofascial syndrome , on the other hand, is a soft tissue pathology characterized by the presence of trigger points . These are hyperirritable areas in a contracted muscle, responsible for local or referred pain, often deep, dull, or even throbbing.
These two types of pain can overlap , particularly in the suboccipital region, which is very rich in innervation and subject to a lot of postural tension.
The role of the suboccipital muscles: the crossroads of tensions
The suboccipital muscles—particularly the rectus capitis minor and major, as well as the superior and inferior obliques—are key stabilizers of the craniocervical junction. They participate in ongoing, often unconscious, postural micro-adjustments, particularly in response to gaze or head position.
Under the effect of stress, poor posture or eye fatigue, these muscles can contract chronically , generating trigger points. These points can themselves cause referred pain in the occipital region , sometimes similar to that of neuralgia .
Furthermore, persistent contraction of these muscles can compress the occipital nerve , maintaining or aggravating pre-existing neuralgia. This sets in a vicious cycle of pain : neuropathic pain → muscle tension → myofascial activation → worsening of pain.
Referred pain or nerve irritation? A diagnostic challenge
One of the major difficulties lies in differentiating between myofascial referred pain and purely nerve pain . The two can coexist, intensify each other, or mask the true source of the problem.
Some guidelines:
- Myofascial pain is often more diffuse, deep, constant , with a wide area of pain .
- Neuralgic pain is briefer, sharp, well localized , sometimes with sensations of burning, tingling or numbness.
- Active trigger points may elicit referred pain on pressure, whereas Arnold’s nerve is often painful on palpation specific to its trajectory.
A precise manual examination, including palpation, mobility tests and search for reflex zones, is essential to refine the diagnosis.
Integrative osteopathic approach: freeing both planes
The major interest of the osteopathic approach is its ability to integrate the nervous and myofascial dimensions , without opposing them. The osteopath can act on:
- Muscle tension : through myofascial release techniques, trigger point inhibition, or functional stretching.
- Nerve decompression : by improving the mobility of the cervical vertebrae, by reducing pressure on the areas where the occipital nerve passes.
- The overall postural pattern : by rebalancing the myofascial chains and correcting remote biomechanical imbalances (pelvis, thorax, diaphragm, etc.).
- Regulation of the autonomic nervous system , often hyperactivated in chronic pain, via cranial, visceral or respiratory techniques.
Breaking out of the vicious circle: patient and gradual work
In cases of crossed pain, relief may not be instantaneous . It is often a gradual process, involving several sessions, postural rehabilitation, home stretching exercises, and sometimes psycho-corporal support.
Recognizing the myofascial component in neuralgia, or the nerve irritation in muscle pain, changes everything in the therapeutic approach . This prevents misdiagnosis, inappropriate treatments, or unrealistic expectations.

Preventing neuralgia: posture, ergonomics and healthy lifestyle
While occipital neuralgia is often approached from a treatment perspective, prevention is key. Although some cases are linked to non-modifiable medical factors (advanced osteoarthritis, malformation, traumatic after-effects), the majority of neuralgia can be avoided or alleviated by paying careful attention to our daily lives: our posture, our work environment, our stress management, and our lifestyle habits.
Posture: alignment at the heart of prevention
Maintaining a neutral and balanced posture, particularly in the head and neck, is one of the pillars of prevention. The cervico-occipital region is susceptible to prolonged imbalances: a head too far forward, rounded shoulders, a slumped back, etc. These positions create continuous tension on the suboccipital muscles, promoting irritation of the surrounding nerves.
Here are some concrete tips:
- Keep your head aligned with your spine, neither tilted forward nor tilted down.
- Avoid holding your phone between your ear and shoulder or looking down for long periods of time (e.g., prolonged reading on a smartphone).
- Alternate positions (sitting, standing, walking) throughout the day.
- Take regular active breaks , especially if you work in a prolonged sitting position.
Ergonomics: a workspace adapted to your body
Ergonomics refers to adapting the environment to our physical abilities. To prevent occipital neuralgia, well-designed ergonomics can reduce the load on the cervical spine and limit microtrauma due to repetitive strain.
Some essential elements to adjust:
- Screen height : It should be at eye level, so that the neck remains straight.
- Office chair : with a backrest that supports the lower back and a seat that keeps the feet flat.
- Keyboard and mouse : close to the body, to avoid tension in the shoulders and neck.
- Teleworking : Avoid working from the sofa or bed, which induces prolonged poor posture.
Simple ergonomic adjustments can prevent the development of a breeding ground for chronic tension.
Hygiene of life: move, breathe, relax
Modern lifestyles tend to increase sedentary lifestyles and stress, two major factors in the onset of neck and occipital pain. To counteract this, lifestyle choices become a real prevention tool.
Here are some areas to integrate:
- Regular physical activity : it promotes joint mobility, muscle relaxation, and good tissue vascularization. Walking, swimming, yoga, or tai chi are particularly suitable.
- Gentle stretches : Daily, targeting the muscles of the neck, shoulders and upper back.
- Conscious breathing : Slow, deep abdominal breathing can help decrease the background tone of the cervical muscles.
- Quality sleep : Choose an ergonomic pillow that respects the natural curvature of the neck. Sleep on your back or side, avoiding twisted positions.
- Adequate hydration : Muscle and fascial tissues need water to maintain their elasticity. Dehydration can promote tension and pain.
Listening to yourself: preventing rather than reacting
Effective prevention also relies on the ability to listen to the body’s signals . Morning stiffness, diffuse pain at the base of the skull, neck fatigue at the end of the day: these are all clues that the body sends before the onset of more pronounced pain.
Rather than waiting for pain to set in, it is recommended to act at the first signs:
- Through a preventive osteopathic consultation;
- By adjusting certain habits;
- Through simple self-stretching or relaxation exercises.
Your questions about occipital neuralgia: clear and practical answers
Q: What are the typical symptoms of occipital neuralgia and how is it diagnosed?
Symptoms of occipital neuralgia typically include pain at the base of the skull, throbbing headaches, and sometimes tingling or numbness. Diagnosis often involves a thorough physical examination, a detailed medical history, and sometimes imaging tests to rule out other possible causes of head and neck pain. It is essential to consult a healthcare professional for an accurate assessment and appropriate treatment advice.
Q: What are the most common causes of occipital neuralgia?
Common causes of occipital neuralgia include muscle tension, trauma, posture problems, migraines, and sometimes nerve or blood vessel problems. It is important to consult a healthcare professional to determine the specific cause in each case.
Q: Is occipital neuralgia related to any underlying medical conditions?
In some cases, occipital neuralgia may be associated with underlying medical conditions such as cervical arthritis, neurological disorders, or nerve compression. An accurate diagnosis is essential to determine the relationship with other medical conditions.
Q: How is occipital neuralgia treated?
Treatment for occipital neuralgia depends on the underlying cause. Common approaches include conservative methods such as physical therapy, pain management medications, and sometimes relaxation techniques. In some cases, more advanced options such as surgery may be considered.
Q: Is occipital neuralgia curable?
Complete recovery from occipital neuralgia depends on the specific cause and response to treatment. In many cases, proper symptom management can lead to a significant improvement in quality of life, although a complete recovery is not always guaranteed.
Towards a better understanding and comprehensive management of occipital neuralgia
Occipital neuralgia, long relegated to the rank of “atypical” or “resistant” headaches, now deserves recognition commensurate with its complexity. This disorder, often misunderstood, actually turns out to be the result of a subtle imbalance, located at the intersection of several systems: nervous, muscular, articular, postural, and even emotional. As medical science and manual approaches advance, one thing is becoming clear: to effectively treat this pain, it is not enough to silence the symptom. It must be listened to, understood… and addressed in its entirety.
Understanding occipital neuralgia means first recognizing its multifactorial nature . It does not arise from nothing. It often reflects an overload: mechanical, postural, functional, emotional overload. The Arnold nerve, by its position and its path, becomes an alarm signal, a sensitive sentinel to the tensions accumulated in the neck, whether muscular, fascial, or articular. The resulting pain, although intense, is often the expression of a profound, but reversible, imbalance .
This understanding requires a change of perspective. Rather than seeking a quick solution at all costs—a medication, an infiltration, a surgical procedure—modern management of occipital neuralgia invites a return to the origin of the disorder . This is where osteopathy finds its full meaning. Thanks to a detailed assessment of mobility restrictions, tissue tension, and postural disorganization, the osteopath can, with precise and non-invasive gestures, relieve nerve compression and restore a lasting functional balance.
But osteopathy is not limited to mechanical action. It is part of a systemic vision of the body , where each area of tension can be the echo of another segment, of another story. An imbalance of the pelvis, blocked breathing, chronic unverbalized stress can, from a distance, keep the occipital region on permanent alert. Pain then becomes a body language, an attempt at regulation, even an invitation to slow down.
This is why comprehensive care cannot be reduced to local treatment. It must integrate, beyond manual techniques, postural education, ergonomics at work, stress management, adapted physical activity, and sometimes psychological support . Because living with chronic pain, even discreet, changes self-esteem, relationships with others, and the ability to project oneself. It is not simply a stubborn headache, but often an invisible and disabling experience.
In this regard, interdisciplinary collaboration becomes a valuable resource. Osteopaths, general practitioners, neurologists, physiotherapists, psychologists—all can contribute, each in their own way, to providing patients with consistent care that respects their experience. To be relieved, pain needs to be understood… but also acknowledged.
Finally, let’s not forget the central role of the patient themselves in this process. By giving them an active role in their healing—through stretching, habit changes, and better listening to their body—we not only strengthen the effectiveness of treatments, but also their ability to prevent recurrences. Autonomy is a fundamental pillar of any sustainable care strategy.
References
Scientific and medical references
- International Headache Society . (2018). The International Classification of Headache Disorders, 3rd edition (ICHD-3) . This document is the authoritative document for the classification of headache disorders, including occipital neuralgia .
Link: https://ichd-3.org/ - Vanelderen, P., Lataster, A., Levy, R., Mekhail, N., van Zundert, J. (2010). Occipital neuralgia . Pain Practice , 10(2), 137–144.
DOI : 10.1111/j.1533-2500.2009.00335.x - Govindarajan, R., & Ropper, A. H. (2002). Occipital neuralgia: a neglected cause of headache. BMJ, 324(7335), 1217–1218.
Lien : https://www.bmj.com/content/324/7335/1217 - Bogduk, N. (2003). Anatomy and pathophysiology of occipital neuralgia . Spine , 28(24), S17–S21.
A key reference on the anatomy of Arnold’s nerve and its clinical implications.
Osteopathic references
- Fryer, G. (2016). Principles of manual medicine in the treatment of headache and cervical pain . International Journal of Osteopathic Medicine , 21, 20–27.
Discusses the integrated osteopathic approach to neck pain and headaches. - Bochurberg, C. (2014). Introduction to psychosomatic osteopathy . Paris: Sully.
Useful for exploring the link between chronic pain, emotional experience and tissue regulation. - Goldstein, M., & Pons, J. (2010). Neck pain: diagnosis and treatment . Masson.
Includes a review of occipital pain and the role of posture.
References on chronic pain and its psychological impact
- Eccleston, C. (2001). Role of psychology in pain management . British Journal of Anaesthesia , 87(1), 144–152.
Highlights the role of cognition, mood and coping strategies in pain perception. - Bouhassira, D. et al. (2008). Neuropathic pain: diagnostic criteria and clinical tools . La Revue du Praticien , 58(2), 183–190.
- Melzack, R., & Wall, PD (1996). The challenge of pain . Penguin Books.
A classic in the multidimensional understanding of pain.



















