Introduction
Overview of Back Pain in Pregnancy
Back pain is a common and often inevitable complaint during pregnancy, affecting a significant number of women. This discomfort typically arises due to the numerous physiological and anatomical changes that occur as the body adapts to support the growing fetus. Understanding the nature and causes of back pain during pregnancy is crucial for effective management and prevention.
Prevalence and Impact on Daily Life
Research indicates that a substantial percentage of pregnant women experience back pain, particularly in the later stages of pregnancy. For instance, one study found that 86% of women at 36 weeks gestation reported difficulty performing simple movements like sit-ups. This widespread prevalence underscores the importance of addressing back pain as a significant concern during pregnancy.
The impact of back pain on daily life can be profound. It can interfere with routine activities, affect sleep quality, and diminish overall well-being. Pregnant women often find themselves struggling with tasks that were previously manageable, leading to frustration and a decreased quality of life. Additionally, the psychological and emotional toll of persistent pain can contribute to stress and anxiety, further complicating the pregnancy experience.
Recognizing the prevalence and impact of back pain during pregnancy is the first step toward implementing effective strategies for relief and support. By raising awareness and providing practical solutions, we can help improve the quality of life for expectant mothers facing this common challenge.
Physiological Changes During Pregnancy
Hormonal Changes
During pregnancy, the body undergoes significant hormonal changes to support the growing fetus and prepare for childbirth. One of the primary hormones involved is relaxin, which increases in production during pregnancy. Relaxin helps to relax the ligaments in the pelvis and soften and widen the cervix in preparation for delivery. However, its effects are not limited to the pelvic area; relaxin also affects ligaments throughout the body, leading to increased joint laxity and a higher risk of sprains and strains. This increased flexibility, while beneficial for childbirth, can contribute to instability and discomfort in the lower back and pelvic regions.
Another important hormone is progesterone, which rises significantly during pregnancy. Progesterone helps maintain the uterine lining and prevent premature contractions, but it also causes smooth muscle relaxation, which can affect the stability of the spine and contribute to back pain. Additionally, the increased levels of estrogen play a role in fluid retention and weight gain, which further impact the musculoskeletal system.
Weight Gain and Its Effects
Weight gain is a natural and necessary part of pregnancy, providing essential nutrients to the developing baby and preparing the mother’s body for breastfeeding. On average, women gain between 25 to 35 pounds during pregnancy. This additional weight places increased stress on the musculoskeletal system, particularly the spine. As the abdomen enlarges, the center of gravity shifts forward, increasing the curvature of the lumbar spine (lordosis). This change in posture can strain the lower back muscles and ligaments, leading to discomfort and pain.
The additional weight also affects the lower extremities, as the legs and feet must support the increased load. This can result in altered gait patterns, swelling, and pain in the legs and feet. The cumulative effect of these changes can significantly impact a pregnant woman’s mobility and overall comfort.
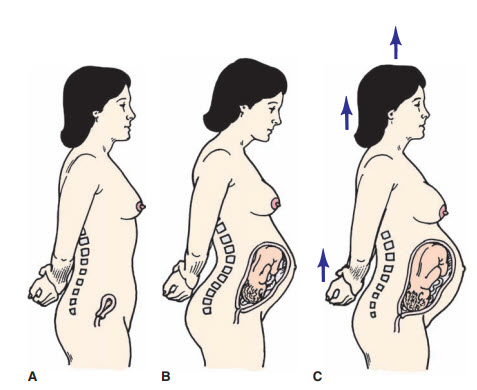
Shifts in the Center of Gravity
As the pregnancy progresses, the growing uterus causes a noticeable shift in the body’s center of gravity. This anterior shift forces the body to adapt by altering posture and muscle activation patterns. To compensate for the forward pull, many pregnant women instinctively lean backward, increasing the curvature of the lower spine. This adjustment, known as lumbar lordosis, can lead to muscle fatigue, tension, and pain in the lower back and pelvis.
Additionally, the shift in the center of gravity affects balance and coordination, making pregnant women more prone to falls and injuries. The altered posture also places additional strain on the neck and upper back as the body tries to maintain an upright position. These compensatory changes can lead to a cascade of musculoskeletal issues, including tension headaches, upper back pain, and sciatica.
Overall, the physiological changes during pregnancy are profound and multifaceted, affecting the hormonal, musculoskeletal, and postural systems. Understanding these changes is essential for developing effective strategies to manage and alleviate back pain, thereby improving the quality of life for expectant mothers. By addressing hormonal influences, managing weight gain, and accommodating shifts in the center of gravity, healthcare providers can offer targeted interventions to support the health and well-being of pregnant women.

Postural Adaptations
Changes in Lumbar and Cervical Curves
During pregnancy, the body’s center of gravity shifts forward due to the growing fetus, leading to significant postural adaptations. One of the most noticeable changes is the increased curvature of the lumbar spine, known as lordosis. This exaggerated curve helps to balance the body’s weight and accommodate the expanding abdomen, but it also places additional strain on the lower back muscles and ligaments.
Similarly, the cervical spine may also experience changes. To compensate for the forward shift in the center of gravity, pregnant women often extend their necks and tilt their heads backward, increasing the cervical curve. This adjustment can lead to tension and discomfort in the neck and upper back.
These changes in spinal curvature are necessary to maintain balance and stability but can contribute to discomfort and pain as the body adapts to its new alignment.
Muscle Imbalances and Their Consequences
The postural adaptations during pregnancy lead to muscle imbalances, as some muscles become overstretched while others become overly tight. The lumbar and cervical extensor muscles, responsible for maintaining an upright posture, often become shortened and contracted due to the increased spinal curves. This constant state of contraction can result in muscle fatigue and micro-tearing, contributing to pain and discomfort.
On the other hand, the flexor muscles of the lumbar and cervical regions tend to become elongated and weakened. The abdominal muscles, in particular, are stretched as the uterus expands, reducing their ability to support the spine and maintain proper posture. The pectoral muscles also become shortened and tight as the shoulders roll forward to accommodate the changing body shape.
These muscle imbalances can lead to a lack of harmony between opposing muscle groups, resulting in joint instability and an increased risk of injuries. The lumbosacral and sacroiliac joints, as well as the lumbar facet joints, are particularly susceptible to slippage and misalignment due to these imbalances.
Common Postural Issues
The postural changes and muscle imbalances during pregnancy can lead to several common postural issues:
- Anterior Pelvic Tilt: As the pelvis tilts forward to accommodate the growing abdomen, the lower back arch increases, placing additional stress on the lumbar spine and potentially leading to lower back pain.
- Rounded Shoulders: The forward shift in the center of gravity and the weight of the growing breasts can cause the shoulders to round forward. This posture can lead to tightness in the chest muscles and weakness in the upper back muscles, contributing to upper back and neck pain.
- Forward Head Posture: To counterbalance the forward shift of the upper body, many pregnant women develop a forward head posture, where the head juts out in front of the shoulders. This posture can strain the neck muscles and contribute to tension headaches and neck pain.
- Knee Hyperextension: To maintain balance, some pregnant women may lock their knees into hyperextension. This posture can place additional stress on the knee joints and lead to discomfort in the lower limbs.
Understanding these common postural issues is crucial for developing strategies to alleviate discomfort and prevent further complications. Interventions such as targeted exercises, proper body mechanics, and supportive equipment can help manage these postural adaptations and promote better alignment and comfort during pregnancy.
Common Types of Back Pain
Lumbosacral Pain
Lumbosacral pain is the most frequently reported type of back pain among pregnant women. This pain is typically localized in the lower back, specifically in the area where the lumbar spine meets the sacrum. Several factors contribute to lumbosacral pain during pregnancy:
- Increased Lumbar Lordosis: The forward shift in the center of gravity causes an increased curvature of the lower spine, placing additional stress on the lumbar vertebrae and surrounding muscles.
- Weight Gain: The additional weight gained during pregnancy adds extra load to the lower back, exacerbating pain and discomfort.
- Hormonal Changes: Elevated levels of relaxin and progesterone lead to ligamentous laxity, making the lumbosacral region more susceptible to strain and injury.
Lumbosacral pain can vary in intensity, from mild discomfort to severe, debilitating pain. It often worsens with prolonged standing, sitting, or physical activity and can significantly impact a pregnant woman’s quality of life and mobility.
Pelvic Girdle Pain
Pelvic girdle pain (PGP) refers to pain experienced in the pelvic region, including the sacroiliac joints, pubic symphysis, and hip joints. PGP is distinct from lumbosacral pain but often occurs concurrently. The causes of pelvic girdle pain during pregnancy include:
- Hormonal Influences: Relaxin and other hormones soften the ligaments of the pelvis to prepare for childbirth, leading to instability and pain in the pelvic joints.
- Biomechanical Changes: The growing uterus and shifting center of gravity alter the biomechanics of the pelvis, contributing to joint misalignment and stress on the pelvic girdle.
- Muscle Imbalances: Weakness and tightness in the muscles surrounding the pelvis, including the glutes, hip flexors, and pelvic floor muscles, can exacerbate PGP.
Symptoms of PGP can range from mild to severe and may include pain in the front or back of the pelvis, groin, hips, and thighs. The pain is often aggravated by activities such as walking, climbing stairs, and turning in bed.
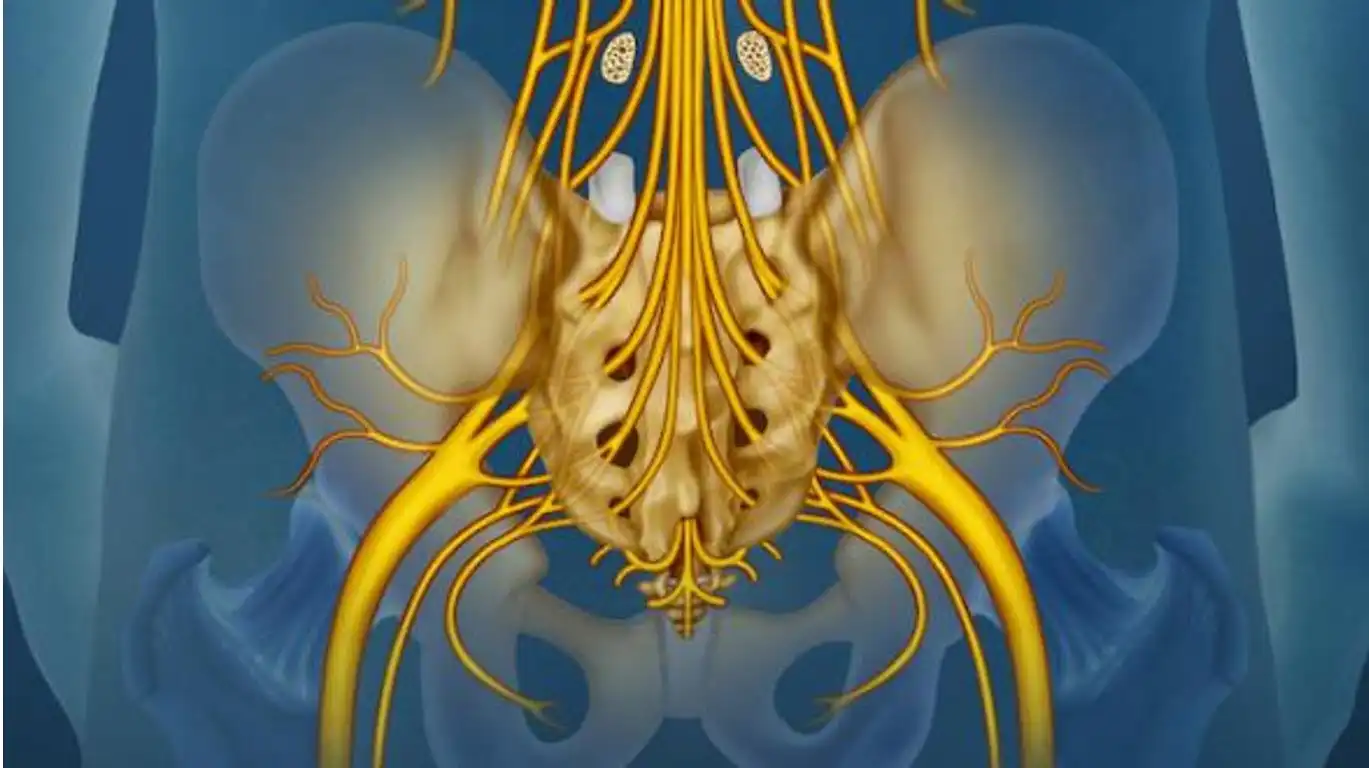
Sciatica and Nerve Pain
Sciatica and nerve pain during pregnancy are typically caused by compression or irritation of the sciatic nerve, which runs from the lower back down through the buttocks and legs. The contributing factors to sciatica during pregnancy include:
- Postural Changes: The increased curvature of the lumbar spine and the forward shift in the center of gravity can place pressure on the sciatic nerve.
- Weight Gain: Additional weight can compress the sciatic nerve, leading to pain and discomfort.
- Uterine Expansion: The growing uterus can press against the sciatic nerve, particularly in the later stages of pregnancy.
Symptoms of sciatica include sharp, shooting pain that radiates from the lower back down to the buttocks and legs, as well as numbness, tingling, and weakness in the affected leg. Sciatic pain can be intermittent or constant and may worsen with certain movements or positions.
Risk Factors for Back Pain
Pre-existing Conditions
Certain pre-existing conditions can increase the likelihood of experiencing back pain during pregnancy. Women with a history of back pain or musculoskeletal issues are particularly susceptible. Conditions such as scoliosis, herniated discs, and previous back injuries can predispose pregnant women to more severe and persistent back pain. Additionally, women with pelvic floor dysfunction or sacroiliac joint dysfunction may experience exacerbated symptoms due to the added strain and hormonal changes during pregnancy.
Pre-existing conditions related to systemic health, such as obesity or arthritis, can also contribute to an increased risk of back pain. Excess body weight places additional stress on the spine and joints, while inflammatory conditions like arthritis can be aggravated by the hormonal and biomechanical changes of pregnancy.
Occupational and Lifestyle Factors
Occupational and lifestyle factors play a significant role in the development and severity of back pain during pregnancy. Jobs that require prolonged standing, heavy lifting, or repetitive movements can increase the risk of back pain. For example, healthcare workers, retail employees, and manual laborers may be more susceptible due to the physical demands of their work.
Sedentary occupations also contribute to back pain, as prolonged sitting can lead to poor posture and muscle imbalances. Office workers who spend extended periods sitting at a desk may develop lower back pain due to inadequate lumbar support and improper ergonomics.
Lifestyle factors such as poor posture, inadequate rest, and high levels of stress can exacerbate back pain during pregnancy. Engaging in activities that strain the back, such as lifting heavy objects or performing high-impact exercises, can also increase the risk.
Physical Activity Levels
Physical activity levels before and during pregnancy can significantly influence the risk of back pain. Women who lead a sedentary lifestyle with little regular exercise are more likely to experience back pain due to weak core and back muscles. A lack of physical fitness can lead to muscle imbalances and poor posture, making it harder for the body to adapt to the physical changes of pregnancy.
Conversely, maintaining an appropriate level of physical activity during pregnancy can help mitigate back pain. Prenatal exercise programs focusing on strengthening the core, improving posture, and enhancing flexibility can reduce the risk of back pain. Activities such as prenatal yoga, swimming, and walking are particularly beneficial for maintaining musculoskeletal health during pregnancy.
However, it is important to avoid overexertion and high-impact activities that may strain the back. Pregnant women should consult their healthcare providers to develop a safe and effective exercise routine tailored to their individual needs and fitness levels.
Impact on Daily Activities
Difficulty with Routine Tasks
Back pain during pregnancy can significantly interfere with a woman’s ability to perform routine tasks. The increased discomfort and limited mobility can make everyday activities, such as bending, lifting, and standing, particularly challenging. Simple actions like getting in and out of bed, picking up objects from the floor, or even walking can become painful and cumbersome.
Household chores, such as cooking, cleaning, and laundry, may require frequent breaks and modifications to avoid exacerbating pain. Carrying groceries or caring for other children can also be difficult, leading to a reliance on family members or support systems for assistance. This dependence can be frustrating and may contribute to feelings of helplessness.
Additionally, the physical strain of back pain can affect a woman’s ability to engage in recreational activities, leading to a decrease in overall quality of life. Social interactions may be limited, as attending events or outings can become too physically taxing.
Effects on Sleep and Rest
One of the most profound impacts of back pain during pregnancy is on sleep and rest. Pain can make it difficult to find a comfortable sleeping position, resulting in frequent awakenings and poor sleep quality. The inability to achieve restorative sleep can lead to chronic fatigue, affecting a woman’s energy levels and overall well-being.
Side sleeping, which is often recommended during pregnancy, can exacerbate pain if not properly supported. Using pillows to support the belly, back, and between the knees can help alleviate some discomfort, but finding the right combination can be a challenge. The lack of adequate rest can also contribute to increased pain sensitivity, creating a vicious cycle of pain and sleep disruption.
Daytime rest may also be compromised, as lying down or sitting for extended periods can aggravate back pain. This constant struggle to find comfort can lead to exhaustion and decreased productivity, impacting daily functioning.
Psychological and Emotional Impact
The persistent nature of back pain during pregnancy can take a significant toll on a woman’s psychological and emotional health. Chronic pain is associated with increased levels of stress, anxiety, and depression. The anticipation of pain with every movement can create a constant state of tension and worry, affecting mood and emotional stability.
The inability to perform routine tasks and the disruption of sleep can lead to feelings of frustration, helplessness, and isolation. Pregnant women may feel a loss of control over their bodies and their daily lives, contributing to decreased self-esteem and overall life satisfaction.
Moreover, the emotional strain of coping with chronic pain can impact relationships with partners, family members, and friends. Pregnant women may withdraw from social activities, leading to a sense of loneliness and further emotional distress. The increased stress and emotional burden can also have negative effects on the pregnancy itself, potentially leading to complications.
Diagnosis and Assessment
Clinical Evaluation
The first step in diagnosing and assessing back pain during pregnancy is a thorough clinical evaluation. This typically begins with a detailed patient history, where the healthcare provider will ask about the onset, duration, and nature of the pain. Questions about previous back issues, pre-existing conditions, daily activities, and any recent injuries will help in understanding the context of the pain.
The clinical evaluation also includes a physical examination. The healthcare provider will assess the patient’s posture, gait, and range of motion. Specific tests may be conducted to evaluate muscle strength, flexibility, and reflexes. Palpation of the spine and surrounding muscles can help identify areas of tenderness, spasm, or inflammation. Additionally, the provider may use specific maneuvers to differentiate between different sources of pain, such as testing for sacroiliac joint dysfunction or lumbar spine issues.
Imaging and Diagnostic Tests
While the clinical evaluation provides valuable information, imaging and diagnostic tests may be necessary to confirm the diagnosis and rule out other conditions. However, the use of imaging tests during pregnancy is approached with caution due to potential risks to the fetus.
Exercises and Stretching for Back Pain Relief
Exercises and stretching routines tailored to alleviate back pain during pregnancy can help strengthen muscles, improve flexibility, and support the spine. It’s essential to perform these exercises under the guidance of a healthcare provider or certified prenatal fitness instructor to ensure safety and effectiveness. Here are some recommended exercises and stretches:
1. Pelvic Tilt
- Purpose: Strengthen abdominal muscles and stabilize the lower back.
- How to do it:
- Lie on your back with knees bent and feet flat on the floor.
- Slowly tighten your abdominal muscles and press your lower back into the floor, tilting your pelvis upward.
- Hold for a few seconds, then relax.
- Repeat 10-15 times, gradually increasing repetitions as tolerated.
2. Cat-Cow Stretch
- Purpose: Improve flexibility and mobility in the spine, relieve tension in the back.
- How to do it:
- Start on your hands and knees, with wrists aligned under shoulders and knees under hips.
- Inhale and arch your back, dropping your belly towards the floor (Cow Pose).
- Exhale and round your back, tucking your chin towards your chest (Cat Pose).
- Alternate between Cow and Cat poses, moving slowly and gently.
- Repeat 10-15 times, gradually increasing repetitions.
3. Knee-to-Chest Stretch
- Purpose: Stretch the lower back and gluteal muscles, alleviate tension.
- How to do it:
- Lie on your back with knees bent and feet flat on the floor.
- Slowly bring one knee towards your chest, using your hands to gently pull it closer.
- Hold the stretch for 15-30 seconds, feeling a gentle pull in the lower back and buttocks.
- Switch legs and repeat on the other side.
- Perform 2-3 repetitions on each leg, as tolerated.
4. Prenatal Yoga Poses
- Purpose: Promote relaxation, improve flexibility, and strengthen muscles.
- Recommended Poses:
- Modified Downward-Facing Dog: Use a chair for support to stretch the spine and hamstrings.
- Warrior II Pose: Strengthens legs, opens hips, and stretches the torso.
- Child’s Pose: Relieves tension in the lower back and promotes relaxation.
- Guidelines: Attend prenatal yoga classes or follow online tutorials designed specifically for pregnant women. Avoid poses that involve deep twists, backbends, or lying flat on the back after the first trimester.
5. Swimming
- Purpose: Provides low-impact cardiovascular exercise, strengthens muscles, and reduces strain on the back.
- How to do it:
- Engage in gentle swimming strokes such as breaststroke or backstroke.
- Water buoyancy supports the body, alleviating pressure on the spine.
- Avoid diving or vigorous swimming movements that could strain the back.
Understanding Ligamentous Hypermobility in Pregnancy
During pregnancy, hormonal changes play a pivotal role in preparing the body for childbirth and accommodating the growing fetus. One such hormone, relaxin, secreted initially by the ovaries and later by the placenta, significantly impacts the body’s ligaments. Relaxin, as its name suggests, promotes relaxation and stretching of ligaments throughout the body, particularly in the pelvic region. This physiological adaptation aims to increase the flexibility of pelvic joints, facilitating the passage of the baby during delivery.
Tips for Safe Exercise
- Listen to Your Body: Stop if you experience pain or discomfort.
- Stay Hydrated: Drink plenty of water before, during, and after exercise.
- Warm Up and Cool Down: Begin with gentle stretches and end with relaxation exercises.
- Use Proper Form: Maintain good posture and alignment during exercises.
Consult with your healthcare provider before starting any new exercise routine, especially during pregnancy. They can provide personalized recommendations based on your health status and stage of pregnancy, ensuring safe and effective management of back pain.
Back Pain During Pregnancy: A Patient Perspective
Experiencing back pain during pregnancy is a common concern for many women, often attributed to the physical changes and increased demands placed on the body. As the uterus expands to accommodate the growing baby, it shifts the center of gravity forward, causing the curvature of the spine to increase and placing additional stress on the lower back. This change in posture, combined with hormonal changes like the release of relaxin, which loosens ligaments in preparation for childbirth, can contribute to discomfort and pain in the back and pelvis.
For pregnant women, back pain can range from mild discomfort to severe, affecting daily activities such as walking, sitting, and sleeping. The pain is often exacerbated by activities that involve prolonged standing or sitting, lifting heavy objects, or sudden movements. Many women also report pain that radiates down the legs or into the buttocks, known as sciatica, which can be particularly challenging to manage.
Case Studies and Testimonials
Personal Experiences
Case Study 1: Sarah’s Journey with Prenatal Yoga
While ligamentous flexibility is essential for childbirth, it can also pose challenges. Ligaments are connective tissues that stabilize joints by limiting excessive movement. In some pregnant individuals, the increased laxity in ligaments can lead to joint instability. This instability occurs when the muscles fail to adequately compensate for the excessive range of motion allowed by relaxed ligaments. As a result, joints may become more susceptible to injury or strain, particularly in weight-bearing areas such as the hips, knees, and ankles.
The consequences of ligamentous hypermobility during pregnancy vary. Some women may experience discomfort or pain in the joints due to the reduced stability caused by overly flexible ligaments. This discomfort is often exacerbated by activities that require repetitive or prolonged use of affected joints. Additionally, micro-tears in ligaments can occur when joints are subjected to sudden or excessive stress, leading to further pain and potential long-term joint issues if not properly managed.
For osteopathic professionals, understanding these dynamics is crucial in providing effective care. Pregnant patients with ligamentous hypermobility may benefit from osteopathic manipulative treatment (OMT) aimed at improving joint alignment and function. OMT techniques can help alleviate discomfort by promoting proper biomechanics and reducing strain on compromised joints.
Moreover, it is essential to caution against self-treatment, especially when considering lumbar supports or other orthopedic devices. While these supports can provide temporary relief, their improper use or selection can exacerbate underlying issues. Pregnant individuals should always consult with a qualified osteopath or healthcare provider before purchasing or using lumbar supports. A professional assessment ensures that any support device is tailored to individual needs, taking into account specific anatomical changes and musculoskeletal conditions associated with pregnancy.
Sarah, 32, experienced persistent lower back pain during her second trimester of pregnancy. Frustrated with limited mobility and discomfort, she consulted a prenatal yoga instructor for guidance. Over several weeks of attending weekly classes, Sarah noticed significant improvement in her back pain. The gentle stretches and poses tailored for pregnant women helped relieve muscle tension and promote relaxation. Sarah found that incorporating prenatal yoga into her routine not only alleviated her back pain but also improved her overall well-being and mood throughout her pregnancy.
Case Study 2: John’s Experience with Osteopathic Treatment
John, 35, sought relief for chronic back pain aggravated by his wife’s pregnancy. As a supportive partner, he experienced increased stress and physical strain while assisting with household chores and caring for their toddler. His osteopath recommended a series of gentle manipulations and soft tissue techniques to address muscle imbalances and improve spinal alignment. After several sessions, John noticed a significant reduction in his back pain and an improvement in his ability to manage daily activities without discomfort. The holistic approach of osteopathic treatment not only relieved his symptoms but also enhanced his overall quality of life during this demanding period.
Success Stories with Different Treatments
Success Story 1: Massage Therapy for Pregnancy-Related Back Pain
Marie, 28, struggled with sciatica and pelvic girdle pain during her third trimester. Seeking non-pharmacological relief, she opted for regular prenatal massages with a certified therapist specializing in pregnancy massage. The gentle techniques focused on releasing tension in her lower back, hips, and glutes, providing immediate relief and promoting better sleep. Marie found that combining massage therapy with warm compresses at home helped manage her pain effectively, allowing her to enjoy the final weeks of her pregnancy with reduced discomfort.
Success Story 2: Exercise and Physical Therapy for Lumbosacral Pain
Peter, 30, experienced lumbosacral pain early in his wife’s pregnancy while juggling a demanding job and household responsibilities. With guidance from his physiotherapist, Peter started a tailored exercise program focusing on core strengthening and postural awareness. He incorporated pelvic tilts, gentle stretches, and stability exercises into his daily routine, gradually building strength and flexibility in his back muscles. Peter’s commitment to regular exercise, combined with ergonomic adjustments at work, significantly reduced his back pain and improved his ability to support his wife during this transformative time.
Conclusion
Managing back pain during pregnancy is about enhancing comfort, maintaining mobility, and supporting overall health. It’s essential for pregnant women to prioritize self-care, including regular exercise, proper posture, and relaxation techniques. Partner support, ergonomic adjustments, and adopting healthy lifestyle habits can also contribute to a more comfortable pregnancy experience.
In conclusion, while back pain during pregnancy can be challenging, it is manageable with the right strategies and support. By addressing symptoms early, exploring safe treatment options, and maintaining open communication with healthcare providers, expectant mothers can navigate this period with greater ease and enjoy the journey of pregnancy more fully. Each woman’s experience is unique, and personalized care plays a vital role in promoting a healthy and positive pregnancy experience.