Gout is caused by an excess of uric acid in the blood (hyperuricemia). When the blood has more uric acid than it can handle, the body can turn it into sharp crystals and deposit them in one or more joints.
Introduction
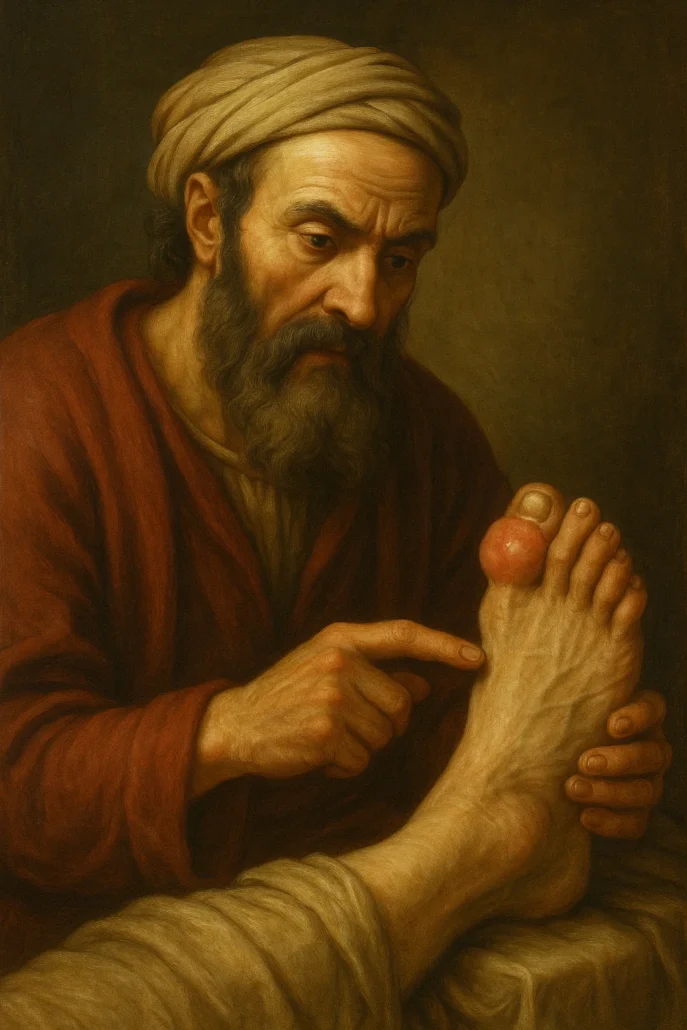
Gout, a form of inflammatory arthritis, often manifests itself dramatically by targeting certain joints in the body. The big toe joint is usually the first to be affected during a gout attack. However, other joints such as the elbows, wrists, fingers, knees, ankles, heels and instep may also be commonly affected, either at the first manifestation of the disease or during recurrent crises.
Interestingly, although gout can affect a variety of joints, the shoulders, spine, and hips are rarely involved. The specificity of involvement of certain joints highlights the distinctive nature of gout and its unique clinical features.
Of all the potentially affected joints, the big toe is the most common location for the first manifestation of gout. In fact, it is estimated that there is a three in four chance that it is the big toe that is affected at some point during the course of the disease. This preference of gout for the big toe is attributed to the crystallization of sodium urate crystals, resulting from a high concentration of uric acid in the blood. These crystals are deposited in the joints, triggering an acute inflammatory response, characterized by severe pain, swelling and redness.
During a gout attack, symptoms can be severe, significantly affecting quality of life. Acute pain can make daily activities difficult and lead to reduced mobility of the affected joint. Gout attacks can be triggered by various factors such as excessive consumption of foods rich in purines, alcohol consumption, stress, or physical trauma.
Managing gout often involves lifestyle changes, such as modifying diet to reduce purine intake, limiting alcohol intake, and losing weight. Medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and uric acid-lowering medications, may also be prescribed to control acute symptoms and prevent future attacks.
Thus, gout presents specific joint manifestations, with a marked preference for the big toe during the first attack. Although other joints may also be affected, recognition of these characteristic patterns of joint damage is essential for the proper diagnosis and management of this form of arthritis. Managing gout often requires a holistic approach, combining lifestyle adjustments and drug treatments to improve the quality of life of those affected.
Gout Throughout History: From Ancient Times to Modern Understanding
The history of gout is fascinating and dates back to ancient times. This brief exploration delves into the evolving understanding of gout and its impact over time:
Antiquity .The history of gout dates back to ancient times, where the first descriptions of symptoms resembling this disease were recorded. Renowned Greek doctors, including the famous Hippocrates (469-399 BC), left testimonies describing cases of intense joint pain, often linked to conditions related to diet and lifestyle. Hippocrates, in his aphorisms, noted that women do not suffer from gout while they have their menses, nor do boys before they initiate sexual activity. This observation hinted at the influence of hormonal and metabolic factors in the development of the disease, laying the groundwork for understanding its complex nature.
Hippocrates’ observations and writings were pioneering, as they provided one of the earliest systematic descriptions of the symptoms and potential causes of gout. His approach to medicine, which emphasized the importance of lifestyle and diet in disease prevention and management, was revolutionary at the time and continues to resonate in modern medical practices. The Hippocratic Corpus, a collection of medical works associated with Hippocrates and his followers, includes detailed accounts of various ailments, including what we now recognize as gout. These writings reflect a sophisticated understanding of how dietary excesses and sedentary lifestyles contribute to health problems, including joint diseases.
The ancient Greeks assigned specific terms to various manifestations of gout, highlighting the diversity of symptoms observed. Among these terms, “podagra” was used to describe the characteristic inflammation of the big toe, which remains a distinctive diagnostic feature. This specific terminology underscored the importance of precise clinical descriptions in diagnosing and understanding diseases. The focus on podagra, in particular, illustrated the recognition of the localized nature of gout attacks, which often begin in the lower extremities and can lead to severe pain and disability.
Additionally, the physician Galen (129-216 AD) described tophi, which are deposits of urate crystals. Galen’s contributions to the understanding of gout were significant, as he provided detailed descriptions of the physical manifestations of the disease. His work built upon the foundation laid by Hippocrates and other early physicians, further advancing medical knowledge. Galen’s extensive writings covered a wide range of medical topics, and his observations on gout included the identification of tophi, which are palpable nodules formed by the deposition of urate crystals in the tissues. These nodules, often found in the ears, joints, and other areas, became a hallmark of chronic gout.
Galen’s influence on medicine extended well beyond his lifetime, and his teachings were revered throughout the Middle Ages and into the Renaissance. His emphasis on the empirical observation of patients and the systematic documentation of symptoms helped shape the practice of medicine for centuries. Galen’s integration of anatomical knowledge with clinical practice was particularly important in the context of gout, as it allowed for a better understanding of the disease’s physical manifestations and progression.
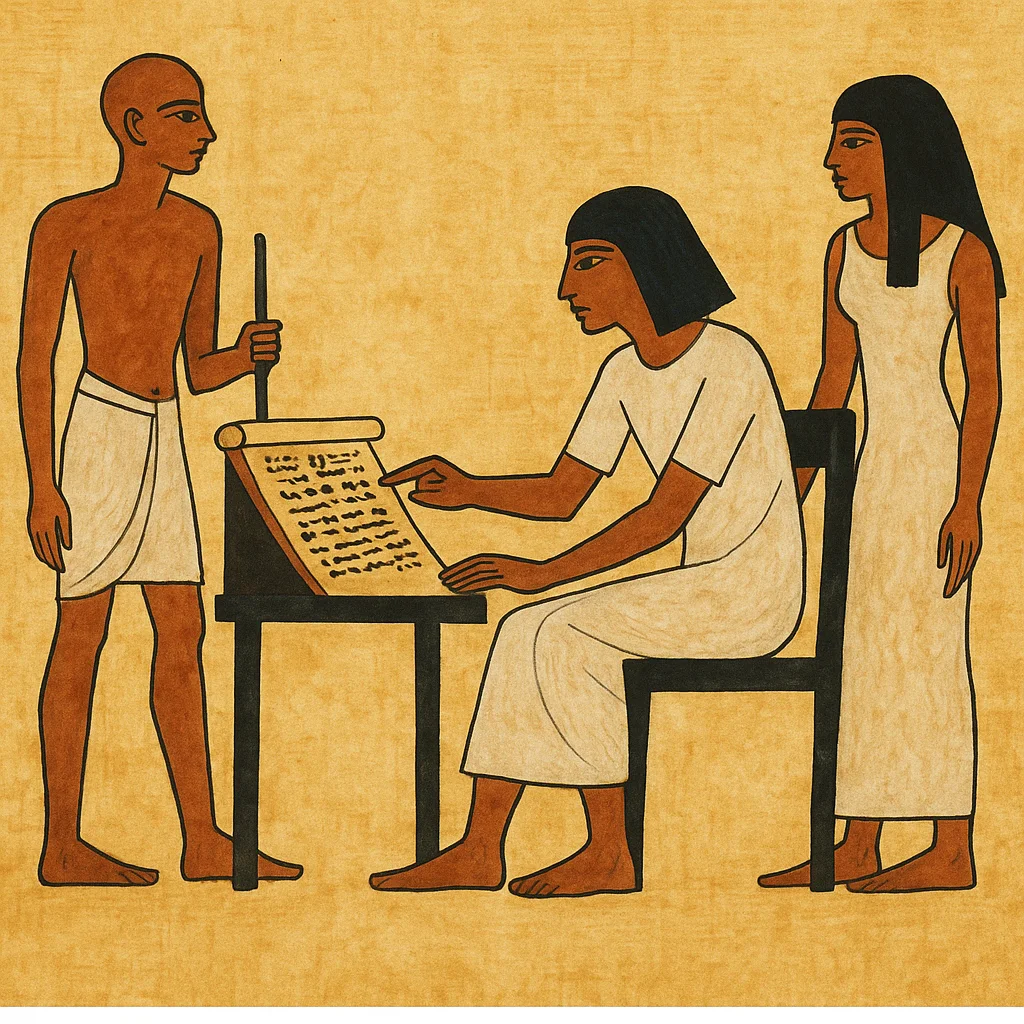
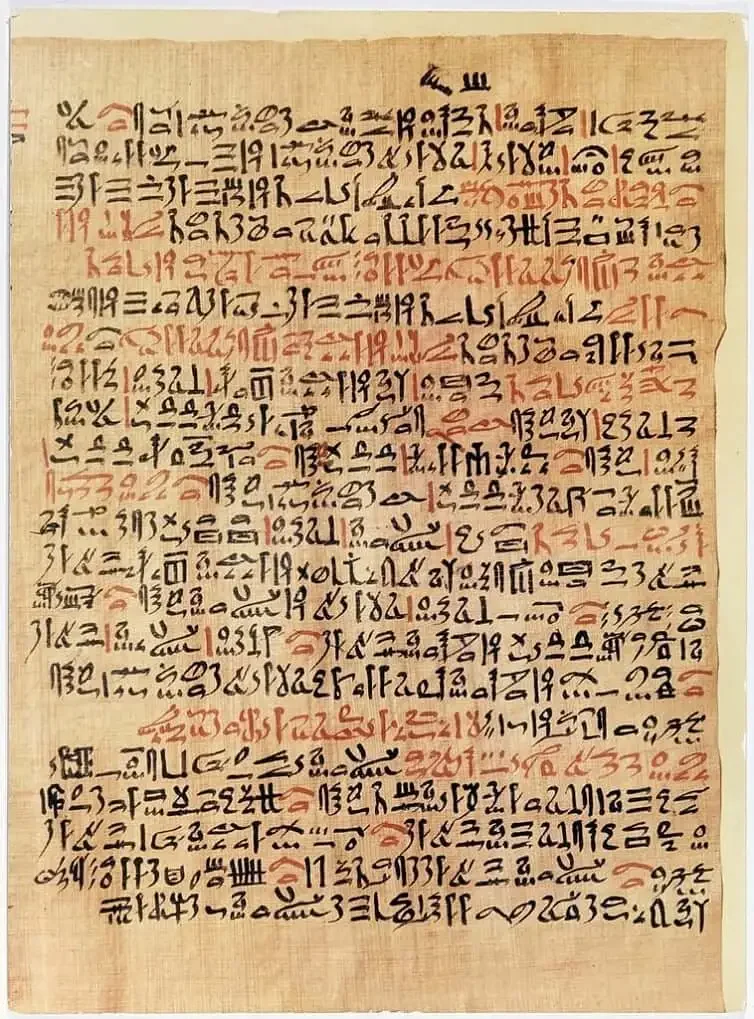
Furthermore, the ancient understanding of gout was not limited to the Greeks. In other parts of the ancient world, similar observations were made. In ancient Egypt, for instance, there are records of treatments for joint pain that align with symptoms of gout. The Ebers Papyrus, an ancient Egyptian medical document dating back to around 1550 BC, contains references to conditions that resemble gout, indicating that the disease was recognized and treated in various cultures.
The ancient understanding of gout also intersected with the broader cultural and philosophical views of health and disease. The concept of humors, which was central to ancient Greek medicine, played a role in the interpretation of gout. According to the humoral theory, the body was composed of four humors: blood, phlegm, black bile, and yellow bile. An imbalance among these humors was believed to cause disease. In the case of gout, an excess of phlegm or black bile was thought to contribute to the formation of urate crystals and the resultant joint inflammation.
The holistic approach to medicine practiced by ancient physicians, which took into account diet, lifestyle, and environmental factors, is echoed in modern approaches to managing gout. Contemporary treatment strategies emphasize the importance of dietary modifications, weight management, and other lifestyle interventions to prevent and control gout attacks. This enduring connection between ancient and modern medical practices highlights the timeless relevance of the insights provided by early physicians like Hippocrates and Galen.
Middle Ages In the Middle Ages, the perception of gout was deeply influenced by the medical beliefs of the time, often tinged with superstition and theories inherited from antiquity. Gout was frequently associated with wealth, as it primarily affected those who had access to foods high in purines, such as red meat and seafood, and who consumed large amounts of alcohol.
The medieval view of gout was sometimes rooted in the theory of humors, a medical concept dating back to ancient Greece. According to this perspective, diseases resulted from imbalances in the body’s humors, which were thought to be vital fluids such as blood, black bile, yellow bile, and phlegm. Gout was thought to be caused by an excess of one of these humors, often attributed to a luxurious lifestyle and overeating.
Medieval medical practitioners, influenced by the works of ancient scholars like Galen and Hippocrates, believed that maintaining a balance among the four humors was essential for health. Gout, often seen as a result of excessive indulgence, was thought to be caused by an excess of black bile or phlegm. Treatments during this period were aimed at restoring this balance and included practices such as bloodletting, purging, and the use of herbal remedies.
Bloodletting, in particular, was a common treatment for gout. Physicians believed that by removing blood, they could reduce the excess humor causing the disease. This practice was often carried out using leeches or by making small incisions to let the blood flow. Despite its widespread use, bloodletting was not always effective and could sometimes lead to further complications.

Dietary recommendations during the Middle Ages also reflected the belief in humoral balance. Individuals with gout were often advised to avoid foods that were considered “hot” or “moist,” as these were thought to exacerbate the condition. Instead, they were encouraged to consume “cooling” foods that would help restore balance. This often meant avoiding rich meats, alcohol, and certain spices, and instead consuming more grains, vegetables, and fruits.
In addition to dietary and medical treatments, gout was also viewed through a moral and social lens during the Middle Ages. Because it was commonly seen in the wealthy, gout was sometimes considered a “disease of kings” or a “patrician malady.” This association with affluence and indulgence led to a degree of moral judgment, with gout sufferers often perceived as having brought the disease upon themselves through gluttony and excess.

Medieval literature and art frequently depicted gout in a way that reinforced these moralistic views. Paintings and manuscripts from the period often show individuals with swollen, painful joints, accompanied by captions or descriptions that highlight the connection between their suffering and their lifestyle choices. This moralistic portrayal contributed to the stigma associated with gout, making it not just a physical ailment but a symbol of excess and moral failing.
Despite these prevailing attitudes, there were also some advances in the understanding of gout during the Middle Ages. The observation of the disease’s hereditary nature, for instance, indicated that genetics played a role, although this understanding was rudimentary compared to modern knowledge. Additionally, some medieval physicians recognized the importance of uric acid, even if they did not fully understand its role in the disease.
Renaissance During the Renaissance, the evolution of the understanding of gout marked a turning point in the approach to this disease. Advances in clinical observations helped refine medical knowledge, and a clearer link between the consumption of purine-rich foods and the onset of gout was established. This period saw a shift from the medieval views, which were often steeped in superstition, to a more scientific and empirical approach to medicine.
One of the key figures in the advancement of gout understanding during the Renaissance was Paracelsus (1490-1541). Paracelsus, a Swiss physician and alchemist, made significant contributions to the study of various diseases, including gout. He described calcareous material deposits in the joints, which he referred to as “stone-like” formations. This was an important step in recognizing the physical manifestations of the disease and understanding its pathology. Paracelsus’ approach to medicine, which emphasized observation and experimentation, laid the groundwork for future scientific inquiry into gout and other conditions.

The Renaissance was also a time of increased interest in anatomy and physiology, spurred by the rediscovery of classical texts and the publication of new works that challenged old paradigms. This intellectual curiosity led to significant advances in understanding the underlying mechanisms of gout. Anatomical studies, often based on dissections, revealed more about the structure and function of joints, providing a better context for understanding how gout affected the body.
One of the most groundbreaking advancements in the study of gout during this period came from Anton van Leeuwenhoek (1632-1723), a Dutch scientist known for his pioneering work in microscopy. Van Leeuwenhoek’s use of the microscope allowed him to observe biological specimens at unprecedented magnifications. In his examinations, he became the first to describe crystals from a gouty tophus, identifying them as urate crystals. This discovery was a monumental step forward in diagnosing gout, as it provided concrete evidence of the disease’s presence at the microscopic level.
Van Leeuwenhoek’s observations were revolutionary, as they provided a tangible link between the symptoms of gout and its physical causes. His meticulous documentation and descriptions of these crystals offered new insights into the nature of gout and its development. This advancement also highlighted the importance of technological innovations, such as the microscope, in advancing medical knowledge and improving diagnostic accuracy.

Antonie van Leeuwenhoek, a pioneering Dutch scientist, revolutionized the understanding of microscopic life with his detailed observations using a self-designed microscope. His groundbreaking work extended to the study of gout, where he was the first to describe crystals from a gouty tophus. Leeuwenhoek’s meticulous documentation of these crystals laid the foundation for future research into the disease, advancing the knowledge of its pathophysiology and helping to demystify its causes. His contributions remain a cornerstone in the field of medical microscopy and gout research.
The increased understanding of gout during the Renaissance was not limited to anatomical and physiological insights. There was also a growing recognition of the role of diet and lifestyle in the development and management of the disease. Early Renaissance physicians began to advise patients to avoid foods high in purines, such as red meat and seafood, which were believed to contribute to the buildup of uric acid in the body. This dietary advice represented a more targeted and preventive approach to managing gout, moving away from the humoral theories of the medieval period.
The recognition of the importance of diet in gout management during the Renaissance also led to the development of specific dietary regimens aimed at reducing the risk of gout attacks. These regimens often included recommendations to increase the intake of fruits and vegetables, which were thought to have a beneficial effect on overall health and help mitigate the effects of uric acid buildup. This holistic approach to treatment, which considered both dietary and lifestyle factors, marked a significant shift in medical practice and laid the foundation for modern approaches to gout management.
In addition to dietary recommendations, the Renaissance also saw the introduction of various herbal remedies and potions aimed at relieving the symptoms of gout. These remedies were often derived from plants known for their anti-inflammatory properties, such as colchicine, which is extracted from the autumn crocus (Colchicum autumnale). Colchicine became a popular treatment for acute gout attacks, providing relief from the intense pain and inflammation associated with the disease. The use of such remedies represented an early form of pharmacological intervention in gout treatment, complementing dietary and lifestyle modifications.

The Renaissance period was thus a time of significant progress in the understanding and management of gout. The contributions of figures like Paracelsus and Anton van Leeuwenhoek, along with the broader advancements in anatomy, physiology, and medical practice, helped to transform the approach to this disease. The shift from medieval superstitions to a more scientific and empirical framework laid the groundwork for future developments in gout research and treatment, many of which continue to influence modern medical practices. The legacy of the Renaissance in the context of gout is one of innovation, discovery, and a deeper appreciation for the complex interplay between diet, lifestyle, and disease.
18th and 19th Centuries In the 18th and 19th centuries, gout continued to be closely linked to historical figures, giving the disease a special aura. Notable figures of European royalty, such as King George IV of England, were known to suffer from this condition, reinforcing the perception of gout as a disease of the affluent and influential. The association of gout with such prominent individuals helped to raise awareness of the disease and spark growing interest in its understanding and treatment.

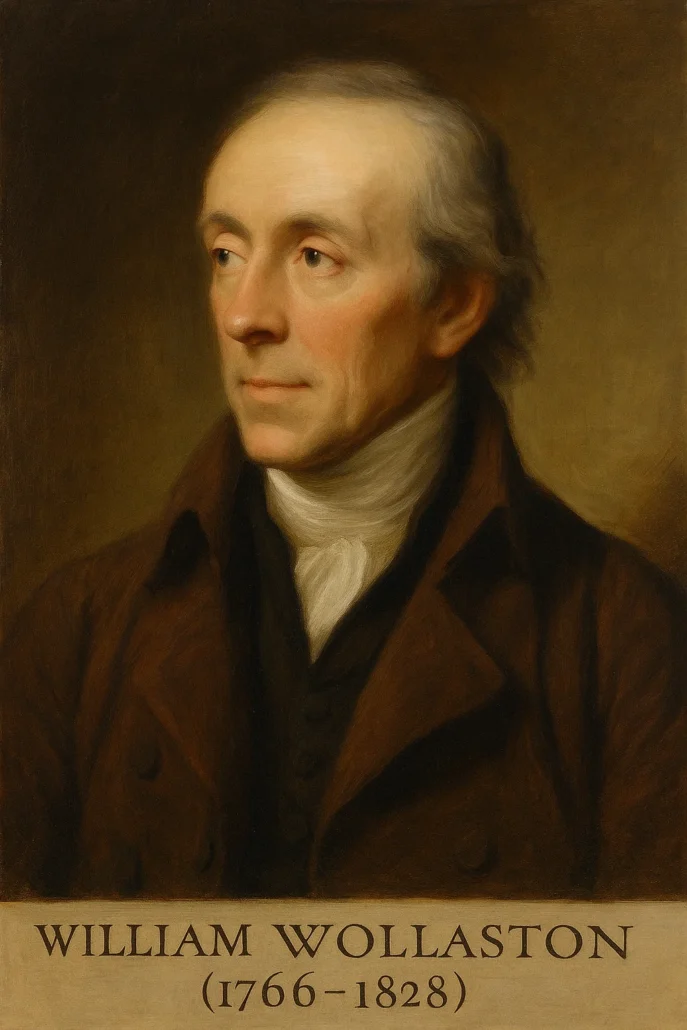
During this period, significant advances were made in understanding the mechanisms underlying gout. One major breakthrough was the identification of the composition of gouty deposits. William Wollaston (1766-1828) discovered that tophi, the characteristic nodular masses seen in gout, are made of urate crystals. This finding was crucial in understanding the chemical nature of the deposits that caused the painful symptoms of gout.
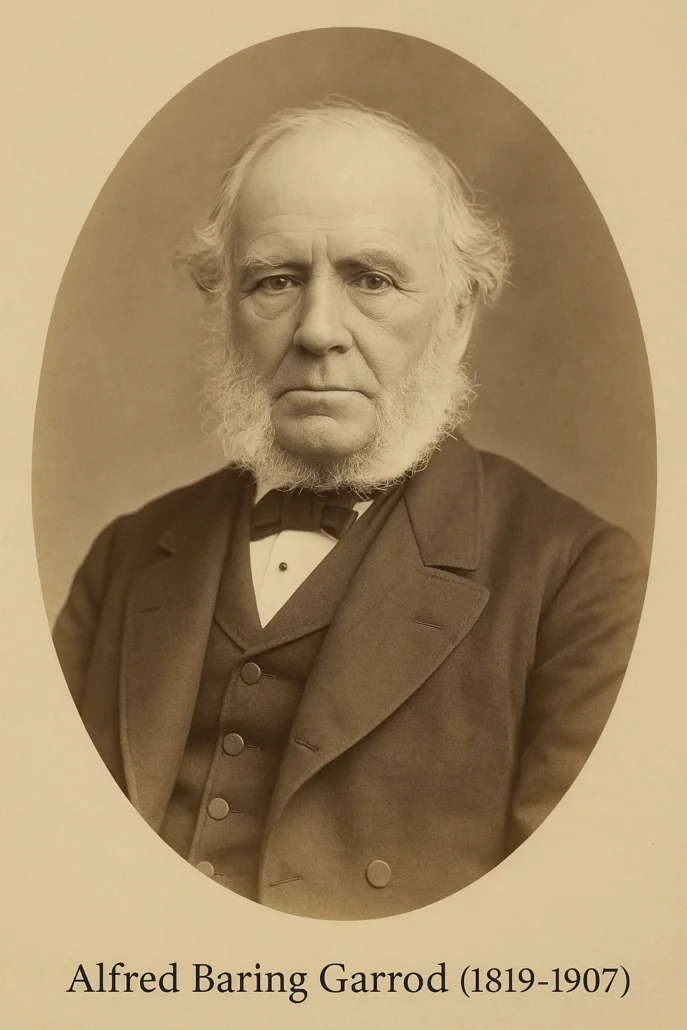
Another significant advancement was made by Alfred Baring Garrod (1819-1907), who discovered that patients with gout have hyperuricaemia, an abnormally high level of uric acid in the blood. This discovery was pivotal as it established a clear link between uric acid and gout, providing a biochemical basis for the disease. Garrod’s work laid the foundation for understanding the pathophysiology of gout and opened up new avenues for its treatment.
The recognition of hyperuricaemia as a key factor in gout led to the development of more targeted treatment approaches. Dietary adjustments became an important aspect of managing gout. Patients were advised to reduce their intake of purine-rich foods, such as red meat, seafood, and alcoholic beverages, which were known to contribute to the buildup of uric acid in the blood. This dietary guidance was a significant shift from earlier, less specific recommendations.
In addition to dietary changes, the 18th and 19th centuries saw the introduction of specific medications aimed at alleviating the symptoms of gout. One of the notable treatments was colchicine, derived from the autumn crocus plant, Colchicum autumnale. Colchicine was found to be effective in reducing the inflammation and pain associated with acute gout attacks, and it became a standard treatment for managing the disease.
The 19th century also witnessed advancements in the understanding of the genetic and environmental factors contributing to gout. Physicians began to observe that gout tended to run in families, suggesting a hereditary component to the disease. This observation pointed towards the genetic predisposition to gout, although the specific genetic mechanisms were not yet fully understood.
Additionally, the development of better diagnostic techniques helped improve the identification and management of gout. The use of chemical analysis to measure uric acid levels in the blood became more refined, allowing for more accurate diagnoses. This period also saw the emergence of more detailed clinical descriptions of gout, helping to distinguish it from other forms of arthritis and joint diseases.
The association of gout with notable historical figures and the advancements in medical science during the 18th and 19th centuries played a crucial role in demystifying the disease. Gout was increasingly seen as a medical condition that could be studied, diagnosed, and treated, rather than merely a consequence of a luxurious lifestyle. These developments marked a significant step forward in the understanding and management of gout, setting the stage for further advancements in the 20th century.
20th Century During the 20th century, medical advances significantly improved the understanding of the pathophysiology of gout. A major breakthrough was the identification of urate crystals in joints, a discovery that laid the foundation for a better understanding of the underlying mechanisms of the disease. Folin & Denis (1913) developed the first reliable method of measuring uric acid, further aiding in diagnosis and management.
JL Hollander (1910-2000) perceived the presence of what he thought were crystals in the synovial fluid of gouty patients, while Daniel J McCarthy (1960) identified CPPD and MSU crystals, which are always present in synovial fluid samples obtained at the time of attacks. These discoveries enhanced diagnostic accuracy and treatment efficacy.
21st Century In the 21st century, gout remains a global health problem, and research is intensifying to better understand the genetic and environmental factors that contribute to this complex disease. Advances in genetics have identified variations that may increase an individual’s predisposition to developing gout. Researchers are exploring the underlying molecular mechanisms and genetic interactions to inform the understanding of disease susceptibility.
Modern treatment approaches include agents that reduce uric acid levels and more targeted anti-inflammatory medications. Personalized dietary interventions aim to minimize potential triggers such as foods high in purines, alcohol, and added sugars, reflecting the continued importance of dietary management.
Pathophysiology of gouty arthritis
The pathophysiology of gouty arthritis relies on the accumulation of monosodium urate (MSU) crystals in the joints, triggering an inflammatory response in the body. This complex process begins with hyperuricemia, a condition where the level of uric acid in the blood exceeds the body’s ability to eliminate it. Uric acid, produced during the breakdown of purines, forms MSU crystals which are deposited in the joints.
When these crystals enter the joints, the immune system responds, causing acute inflammation. Macrophages recognize MSU crystals as foreign bodies and release inflammatory mediators such as interleukin-1β (IL-1β). This cytokine plays a central role in the inflammatory cascade, activating other immune cells and causing a chain response.
The resulting inflammation leads to classic symptoms of gouty arthritis, such as pain, swelling, redness and warmth in the affected joints. The release of pro-inflammatory cytokines contributes to the destruction of cartilage and joint tissue, worsening the damage.
The gouty arthritis cycle is characterized by acute bouts of joint pain, known as gout attacks. These attacks often come on suddenly, often at night, and can be triggered by factors such as eating too much purine-rich foods, dehydration or stress.
The pathophysiology of gouty arthritis is not limited to the joints. The accumulation of MSU crystals can also cause the formation of tophi, visible deposits of crystals under the skin, in tendons and joints. These tophi can cause permanent deformity and damage to surrounding tissues.
Additionally, gouty arthritis is often associated with comorbidities, such as hypertension, renal failure, and diabetes, highlighting the complexity of its pathophysiological ramifications. Hyperuricemia itself may contribute to these comorbidities, creating a vicious cycle of medical complications.
- Formation of urate crystals: Uric acid is a natural product of the breakdown of purines, compounds present in certain foods and in body cells. When uric acid levels in the blood become too high, urate crystals tend to form. These crystals are deposited in the joints, triggering the inflammatory process.
- Phagocytosis of crystals by immune cells: Urate crystals cause an immune system reaction. Immune cells, called phagocytes, attempt to neutralize the crystals by phagocytosing them.
- Activation of inflammation: When phagocytes attempt to destroy urate crystals, they release inflammatory mediators, such as interleukin-1β (IL-1β), which play a key role in triggering inflammation.
- Inflammatory response: IL-1β and other inflammatory mediators activate immune cells and recruit more phagocytes to the site of inflammation. This results in an inflammatory response characterized by redness, warmth, swelling, and pain in the affected joint.
- Acute and chronic attacks: Acute attacks of gout are triggered by the sudden release of urate crystals in a joint, causing intense inflammation. Over time, deposits of urate crystals, called tophi, can form in and around joints, leading to chronic inflammation and joint damage.
- Adaptive immune response: Repeated gout attacks can result in an adaptive immune response, where the immune system remembers the presence of the urate crystals and reacts more quickly and intensely during subsequent attacks.
The pathophysiology of gouty arthritis is complex and involves an interaction between uric acid levels, crystal formation, innate and adaptive immune response, and inflammation. Management of this condition aims to reduce uric acid levels, control inflammation and prevent recurrent attacks.

Causes of Gouty Arthritis
The causes of gouty arthritis are deeply rooted in uric acid metabolism. Hyperuricemia, characterized by a high level of uric acid in the blood, is the main trigger for this rheumatic condition. Understanding the causes of gouty arthritis requires a thorough examination of how uric acid is produced, metabolized, and eliminated by the body.
Uric acid is a natural byproduct of the breakdown of purines, compounds found in some foods and cellular products. Under normal conditions, uric acid is filtered by the kidneys and excreted in urine. However, when uric acid production increases or elimination is compromised, hyperuricemia can develop, creating a breeding ground for the formation of monosodium urate (MSU) crystals that cause gouty arthritis.
Several factors contribute to hyperuricemia. One of them is diet, especially excessive consumption of foods high in purines such as red meats, seafood, organ meats and sugary drinks. The purines from these foods are broken down into uric acid, contributing to the buildup.
Genetics also play a role in predisposition to gouty arthritis. Some individuals may have a reduced ability to effectively eliminate uric acid, increasing the risk of hyperuricemia and development of the disease. A family history of gouty arthritis may therefore increase the likelihood of this condition.
Underlying medical conditions, such as obesity, hypertension, and kidney disease, can make hyperuricemia worse. Obesity, in particular, is associated with increased production of uric acid and reduced excretion, creating an environment conducive to crystallization.
Excessive alcohol consumption, particularly beer, is a well-established risk factor for gouty arthritis. Alcohol interferes with the elimination of uric acid by the kidneys, thus promoting its accumulation. Additionally, alcohol can stimulate increased production of uric acid in the liver.
List of Causes
- Hyperuricemia: The main cause of gout is a high concentration of uric acid in the blood, called hyperuricemia. Uric acid is a byproduct of the breakdown of purines, compounds found in certain foods and in the body’s cells.
- Diet: Certain foods high in purines can contribute to increased uric acid levels. This includes red meat, organ meats, seafood, sugary drinks, and alcohol, especially beer.
- Genetic Factors: There is a genetic component to the predisposition to gouty arthritis. If family members have had a history of gout, there may be an increased likelihood of developing the condition.
- Kidney problems: The kidneys play a crucial role in eliminating uric acid. Kidney problems, such as kidney failure, can lead to a buildup of uric acid in the body.
- Obesity: Obesity is associated with an increased risk of gout, possibly due to increased production of uric acid and a reduction in its excretion through the kidneys.
- Alcohol Consumption: Excessive alcohol consumption, especially beer, can increase uric acid levels and increase the risk of developing gout.
- Certain medications: Certain medications, such as diuretics, used to treat high blood pressure, can increase uric acid levels in the blood, which can contribute to gout.
- Age and gender: Gout is more common in men, especially between the ages of 30 and 60. Women tend to have a lower risk before menopause, but the risk increases after menopause.
- Metabolic diseases: Certain metabolic conditions such as diabetes and hyperlipidemia may be associated with an increased risk of gout.
- Joint trauma: Injury or trauma to the joints can trigger a gout attack by causing the release of urate crystals built up in the joints.
- Certain illnesses: Certain medical conditions, such as high blood pressure, kidney failure, and psoriasis, can increase the risk of gout.
- Chemotherapy: Some chemotherapy drugs can influence uric acid levels, increasing the risk of gout.
- Acidosis: An acid-base imbalance in the body, known as acidosis, can promote the formation of urate crystals and contribute to the development of gout.
- Dehydration: Insufficient hydration can lead to an increased concentration of uric acid in the body, thereby promoting crystallization and the formation of deposits in the joints.
- Bariatric Surgery: Some patients who have undergone bariatric surgery, such as gastric bypass surgery, may be at increased risk of gout due to changes in metabolism.
- Metabolic syndrome: The presence of factors associated with metabolic syndrome, such as abdominal obesity, hypertension, and insulin resistance, may increase the risk of developing gout.
- Environmental factors: Certain environmental elements, such as exposure to heavy metals, may be associated with an increased risk of gout, although research on this topic is still limited.
- Thyroid disorders: Thyroid disorders, such as hypothyroidism, may be associated with an increased risk of gout.
- High levels of triglycerides: High levels of triglycerides, a type of fat found in the blood, may be associated with an increased risk of gout.
- Use of certain medications: Certain medications, such as thiazide diuretics used to treat hypertension, can increase uric acid levels, contributing to the development of gout.
- Sleep apnea syndrome: It has been suggested that sleep apnea syndrome may be linked to an increased risk of gout.
- Alcohol abuse: Excessive alcohol consumption, particularly beer and hard liquor, is associated with an increased risk of gout.
- Inflammatory factors: Chronic inflammatory diseases, such as rheumatoid arthritis, may be associated with an increased risk of gout.
- High blood pressure: High blood pressure may be an independent risk factor for the development of gout.
- Major surgeries or severe trauma: Events such as major surgeries or severe trauma can sometimes trigger gout attacks.
- Genetic sensitivity to urate crystals: Individual genetic susceptibility can influence how the body responds to urate crystals, thereby contributing to gout.
Symptoms of Gouty Arthritis
The symptoms of gouty arthritis are often acute, marked by sudden and intense painful attacks, usually localized in the joints. This inflammatory condition, resulting from the crystallization of uric acid, causes characteristic symptoms that mainly affect the joints, but can also have repercussions on other parts of the body.
The most emblematic manifestation of gouty arthritis is the gout attack. These painful episodes generally occur suddenly, often at night, and frequently affect the big toe joint. The pain peaks within a few hours, causing intense discomfort, redness, swelling, and tenderness to the touch in the affected area. Joint movements become extremely painful, limiting mobility.
Besides the gout attack, other joints can also be affected, such as the knees, ankles, elbows and wrists. The frequency and severity of attacks vary from person to person, with some experiencing sporadic episodes while others experience chronic gout with persistent symptoms.
Inflammation resulting from gouty arthritis can cause the formation of tophi, deposits of urate crystals visible under the skin. These hard masses may develop around affected joints, fingers, elbows, or other areas of the body. Tophi can cause joint deformity and, in some cases, pierce the skin, causing a discharge of white crystals.
Over time, untreated recurring attacks can lead to permanent joint damage, decreased mobility, and kidney stone formation. Gouty arthritis may also be associated with systemic symptoms such as fever, general fatigue, and feeling unwell.
It is essential to note that not everyone who has high levels of uric acid in their blood will necessarily develop gouty arthritis, and some people may have high levels of uric acid without experiencing symptoms. However, when symptoms do occur, proper medical diagnosis and management are essential to alleviate pain, reduce inflammation, and prevent long-term complications associated with this particular form of arthritis.
- Acute joint pain: One of the most characteristic symptoms of gouty arthritis is sudden, intense pain in one or more joints. The pain is often described as extremely sharp and can be triggered by factors such as alcohol consumption, meals high in purines, stress or trauma.
- Joint inflammation: Joints affected by gout may become swollen, red, and warm to the touch. Inflammation is a reaction to the presence of urate crystals in the joint.
- Skin redness: The skin over the affected joint may become red and tight due to the underlying inflammation.
- Tenderness to touch: Affected joints may be tender to touch, and even light pressure can trigger severe pain.
- Reduced Mobility: Due to pain and inflammation, the mobility of the affected joint may be significantly reduced. Movements can become difficult.
- Recurrent attacks: Symptoms of gouty arthritis often present with recurrent attacks. After an acute attack, the person may go through interictal periods without apparent symptoms.
- Tophus: As the disease progresses, deposits of urate crystals, called tophi, may form under the skin, forming visible and palpable nodules. Tophi can cause joint deformities and can also form in other areas of the body.
Factors causing excess uric acid
Excess uric acid in the body, known as hyperuricemia, can be caused by several factors. Uric acid is a natural product of the breakdown of purines, compounds found in certain foods and in body cells. When the body produces too much uric acid or eliminates too little through the kidneys, it can cause a buildup, leading to problems such as gout or kidney stone formation. Factors causing excess uric acid include:
- Diet rich in purines: Certain foods are rich in purines, promoting the production of uric acid. Examples of foods high in purines include red meats, organ meats, seafood, fatty fish, sugary drinks, and alcohol.
- Obesity: Being overweight is associated with an increased risk of hyperuricemia. Excess adipose tissue can influence the production of uric acid and its elimination capacity by the kidneys.
- Kidney failure: The kidneys play a crucial role in the elimination of uric acid. Kidney failure can lead to a buildup of uric acid in the blood.
- Heredity: Genetic predisposition can make some people more likely to develop hyperuricemia.
- Certain diseases and conditions: Diseases such as metabolic syndrome, diabetes, high blood pressure, and Lesch-Nyhan syndrome may be associated with excess uric acid.
- Certain medications: Certain medications, such as diuretics, immunosuppressive medications, and some cancer medications, can influence uric acid levels.
- Lifestyle: Lifestyle factors, such as a sedentary lifestyle and excessive alcohol consumption, may contribute to hyperuricemia.
Managing excess uric acid often involves diet changes, weight loss, reducing alcohol consumption, and taking medications as needed.
Areas of the body that can be affected by gout
- Foot: Gout often affects the big toe, causing a painful inflammation known as podagra. However, other parts of the foot, such as the ankle, heel, and top of the foot, may also be affected.
- Ankle: The ankle joint can be the site of gout attacks, causing swelling, redness and severe pain.
- Knee: The knee is another joint commonly affected by gout. Inflammation of the knee joint can lead to severe pain and reduced mobility.
- Hand: Although less common, gout can affect the joints of the hands, including the fingers, wrists and elbows.
- Elbow: The elbow joint may be affected by urate crystal deposits, causing pain, swelling and tenderness.
- Wrist: The wrist joints can also be affected by gout attacks, leading to similar symptoms such as swelling and pain.
- Other Joints: Although less common, gout can also affect other joints in the body, including the shoulders, hips, and ears.
Gout stages
- Asymptomatic hyperuricemia: In the early stages of gout, levels of uric acid in the blood (hyperuricemia) may be high, but there are no obvious symptoms yet. This can go on for years without the person being aware of it.
- Acute gout: The first attack of acute gout usually occurs suddenly and intensely. It is characterized by sharp pain, inflammation, redness and heat in one or more joints, often the big toe. These attacks can be triggered by factors such as excessive alcohol consumption, meals high in purines, stress or trauma.
- Interictal interval: After the first attack, an interictal period may occur, during which the person has no symptoms. However, over time, these intervals may shorten, and acute gout attacks may become more frequent.
- Tophaceous gout: If gout is not well controlled, deposits of urate crystals, called tophi, can form under the skin near affected joints. Tophi are often visible and can cause joint deformities. They can also form in other parts of the body, including the ears and tendons.
- Chronic gout: As the disease progresses, it may progress to a chronic stage characterized by more frequent attacks of gout, persistent joint damage, and complications such as kidney stones due to the buildup of urate in the kidneys. .
A Day in the Life of Someone Living with Gout
Living with gout involves navigating a chronic condition that can significantly impact daily life. Gout, a form of inflammatory arthritis, is characterized by sudden and severe attacks of pain, swelling, and redness in the joints, often the big toe. Here’s a glimpse into a typical day for someone managing this condition.
Morning
The day often begins with stiffness and discomfort. The mornings are particularly challenging as joints that have been immobile during the night may be more painful upon waking. Many individuals with gout experience morning stiffness in the affected joints, which can make getting out of bed and starting the day difficult. A warm shower or bath can help ease this stiffness, providing some relief and making it easier to move around.
Breakfast must be carefully considered, as diet plays a crucial role in managing gout. Foods high in purines, such as red meat, seafood, and certain vegetables, can increase uric acid levels in the blood, triggering gout attacks. A typical breakfast might include low-purine options like whole grains, low-fat dairy products, and plenty of water to help flush uric acid from the body.
Mid-Morning
Work or daily activities can be hindered by the persistent pain and limited mobility caused by gout. For those with a sedentary job, sitting for extended periods can exacerbate joint stiffness. Regular breaks to stand up, stretch, and move around are essential to maintain joint flexibility. Pain management is a constant concern, and over-the-counter anti-inflammatory medications or prescribed treatments may be needed to keep symptoms at bay.
Lunch
Lunch choices are just as important as breakfast. A balanced diet with a focus on low-purine foods is crucial. A salad with lean proteins, such as chicken or tofu, and plenty of vegetables, is a typical choice. Hydration continues to be a priority, with water being the drink of choice to help reduce uric acid levels.
Afternoon
The afternoon can bring fatigue, both from dealing with chronic pain and from the side effects of medications. Simple tasks like walking or standing for extended periods can be exhausting. For those who are still working, it might be necessary to discuss accommodations with an employer, such as ergonomic furniture or the flexibility to take breaks as needed.
Evening
Dinner must be chosen carefully to avoid triggering a gout flare-up. Meals often include low-fat dairy, whole grains, and plenty of fruits and vegetables. Alcohol, particularly beer and spirits, is typically avoided as it can increase uric acid levels. Staying hydrated remains important, so water is again the drink of choice.
After dinner, some light exercise, like walking or swimming, can help maintain joint flexibility without putting too much strain on the affected areas. However, during a flare-up, rest becomes the priority, and activities are minimized to avoid exacerbating the pain.
Night
Bedtime routines may include taking medications prescribed to manage uric acid levels or prevent flare-ups. Elevating the affected joint can help reduce swelling and discomfort during the night. A comfortable and supportive mattress is essential to ensure a good night’s sleep, as pain can often disrupt rest.
Living with gout requires constant vigilance and management. Dietary choices, pain management strategies, and adjustments to daily routines are all part of coping with this chronic condition. Despite the challenges, many people with gout find ways to manage their symptoms and lead fulfilling lives. Regular check-ups with a healthcare provider are essential to monitor the condition and adjust treatment plans as needed, ensuring the best possible quality of life.
Differential diagnosis of gouty arthritis
- Rheumatoid Arthritis: Rheumatoid arthritis is an autoimmune disease that causes inflammation of the joints. It can also cause joint pain, swelling and stiffness, symptoms shared with gouty arthritis. However, the two conditions have different pathological mechanisms.
- Pseudogout (joint chondrocalcinosis): Pseudogout is a condition similar to gouty arthritis, but the crystals responsible are calcium pyrophosphate crystals. It can cause acute attacks of pain and joint inflammation.
- Osteoarthritis: Osteoarthritis is a degenerative joint disease characterized by wear and tear of the articular cartilage. Although symptoms may include joint pain, the stiffness and inflammation characteristic of gouty arthritis may be less pronounced.
- Reactive arthritis: Reactive arthritis can occur in response to an infection in another part of the body. It can also cause joint symptoms similar to gouty arthritis.
- Systemic lupus erythematosus (SLE): Lupus is an autoimmune disease that can affect the joints, causing symptoms similar to gouty arthritis.
- Ankylosing spondylitis: This form of inflammatory arthritis primarily affects the spine, but it can also involve other joints. Symptoms may include pain, stiffness and inflammation.
- Bursitis: Inflammation of the bursae around joints can cause pain and swelling similar to gouty arthritis.
- Joint infections: Bacterial or viral joint infections can also present with symptoms similar to gouty arthritis.
Treatment of arthritic gout
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs, such as ibuprofen or naproxen, are often prescribed to relieve pain and inflammation during a gout attack. However, they do not influence uric acid levels.
- Colchicine: Colchicine is a specific medication for gout that can be used to relieve pain and inflammation. It is often prescribed in combination with other medications.
- Corticosteroids: Corticosteroid injections into the affected joint can help quickly relieve inflammation and pain.
- Medicines to reduce uric acid levels:
- Allopurinol: It inhibits the production of uric acid.
- Febuxostat: It also reduces the production of uric acid.
- Probenecid: It improves the elimination of uric acid by the kidneys.
- Hydration and diet: Drinking plenty of water can help flush out uric acid. A suitable diet, limiting foods rich in purines (red meats, seafood, offal) and alcohol, can help prevent attacks.
- Avoiding Triggers: Identifying and avoiding triggers, such as excessive alcohol consumption, can help prevent gout attacks.
- Weight loss: For overweight people, weight loss can reduce uric acid levels and decrease the frequency of seizures.
- Regular medical monitoring: Regular medical monitoring is essential to adjust treatment according to individual response and prevent long-term complications.
It is important to note that treatment for arthritic gout must be tailored to each patient based on the severity of symptoms, medical history and the presence of risk factors. People with gout should consult a healthcare professional for an accurate diagnosis and personalized treatment plan.
Foods to avoid
List of food to avoid
- Red meats: Excessive consumption of red meats, especially meat from organs like liver and kidneys, may be associated with high levels of purines.
- Seafood: Some seafood, such as mussels, anchovies, sardines, and shellfish, are high in purines and may contribute to hyperuricemia.
- Organ meats: Organ meats, such as liver, kidney, and tongue, are also high in purines and should be consumed in moderation.
- Foods high in saturated fat: Foods high in saturated fat, such as fried foods and deli meats, can worsen the inflammation associated with gout.
- Alcohol: Consuming alcohol, especially beer and spirits, can increase uric acid levels and trigger gout attacks.
- Sugary Drinks: Sweetened drinks, especially those containing high fructose corn syrup, have been linked to an increased risk of gout.
- Certain vegetables: Although most vegetables are good for people with gout, it is recommended to limit the consumption of spinach, asparagus and mushrooms, as they contain moderate amounts of purines.
- High-fat dairy products: Some high-fat dairy products can contribute to inflammation. It is recommended to choose low-fat dairy options.
- Foods High in Fructose: Foods and drinks high in fructose can increase uric acid levels. This includes fruit juices, sodas, and processed foods containing high fructose corn syrups.
- Refined grains: Refined grains, such as white bread and pasta, may be associated with an increased risk of gout. It is best to favor whole grains.
- Caffeine: Caffeine may have mixed effects on gout. Some studies suggest that moderate coffee consumption may be beneficial, but monitoring individual response is recommended.
- Artificial sweeteners: Some artificial sweeteners, particularly aspartame, have been linked to an increased risk of gout in some studies. However, the evidence is limited and reactions may vary.
- Certain fruits: Although most fruits are generally considered healthy, some people with gout may be sensitive to specific fruits due to their fructose content. This may vary from person to person.
- Foods High in Oxalates: Certain foods high in oxalates, such as spinach, rhubarb, and beets, can contribute to the formation of urate crystals and may need moderation.
- Salt: Excessive salt consumption may be associated with increased blood pressure, which can worsen gout symptoms. It is recommended to limit salt consumption and opt for healthier alternatives.
- Vitamin C supplements: Studies have shown that high doses of vitamin C supplements can increase uric acid levels. It is advisable to speak with a healthcare professional before taking any supplements.
- Processed meats: Processed meats, such as sausages, hot dogs and deli meats, may contain ingredients that promote inflammation and should be consumed in moderation.
- High-dose aspirin: High doses of aspirin can reduce the elimination of uric acid through the kidneys, thereby increasing urate levels. It is important to discuss the use of aspirin with a healthcare professional.
- Spicy foods: Certain spicy foods can trigger inflammatory reactions in some people. It may be helpful to monitor individual reaction to spicy foods.
- Some cruciferous vegetables: Although most vegetables are good, some individuals may experience an increase in symptoms when eating cruciferous vegetables such as cabbage and broccoli. It is recommended to observe individual reactions.
Radiographic signs of gouty arthritis
Radiographic signs of gouty arthritis may include characteristic changes that reflect urate crystal deposits in the joints and surrounding tissues. However, these changes may not be immediately visible in the early stages of the disease. Here are some possible radiographic signs of gouty arthritis:
- Sawtooth-shaped opacities: Urate crystals can form sawtooth-shaped opacities along the contours of affected joints. These deposits may be visible on x-rays, particularly in periarticular areas.
- Bone erosions: Chronic gouty arthritis can lead to bone erosions around affected joints. These erosions can appear in the form of gaps or destruction of bone tissue.
- Tophus: Tophi are deposits of urate crystals that can form palpable nodules under the skin or around joints. In advanced stages of the disease, x-rays may show images of tophi, often near the ends of long bones.
- Deposits in cartilage: Urate crystals can be deposited in the cartilage of joints, which may be visible on x-rays. These deposits can contribute to the destruction of cartilage.
- Joint narrowing: Advanced gouty arthritis can cause narrowing of the joint space, indicating cartilage deterioration.

Case courtesy of Bahman Rasuli, Radiopaedia.org . From the case rID: 62537
Quizz
Questionnaire 1
Question 1:
What is the main cause of gout?
A) Excess weight
B) Excessive alcohol consumption
C) Excess uric acid in the blood (hyperuricemia)
D) Genetic factors
E) Lack of exercise
Question 2:
Which part of the body is usually affected first by gout?
A) Shoulders
B) Knees
C) Big toe
D) Wrist
E) Hips
Question 3:
Which ancient physician described cases of joint pain associated with diet and lifestyle?
A) Galen
B) Hippocrates
C) Avicenna
D) Paracelsus
E) Rhazes
Question 4:
What is the outlook associated with gout during the Middle Ages?
A) Disease associated with sedentary lifestyle
B) Disease associated with poverty
C) Disease associated with wealth
D) Disease caused by infections
E) Disease linked to consumption of spices
Question 5:
What is the key step in the pathophysiology of gouty arthritis linked to the formation of urate crystals?
A) Activation of inflammation
B) Phagocytosis of crystals by immune cells
C) Formation of urate crystals
D) Inflammatory response
E) Adaptive immune response
Question 6:
Which food is often associated with an increased risk of gouty arthritis due to its high purine content?
A) Seafood
B) Green vegetables
C) Dairy products
D) Red fruits
E) Whole grains
Question 7:
Which stage of gout is characterized by recurrent attacks, urate crystal deposits under the skin, and persistent joint damage?
A) Acute gout
B) Interictal intervals
C) Tophaceous gout
D) Chronic gout
E) Asymptomatic hyperuricemia
Question 8:
Which drug inhibits uric acid production in the treatment of gout?
A) Colchicine
B) Corticosteroids
C) Allopurinol
D) Ibuprofen
E) Febuxostat
Question 9:
Which autoimmune disease can present with symptoms similar to gouty arthritis?
A) Diabetes
B) Systemic lupus erythematosus (SLE)
C) High blood pressure
D) Metabolic syndrome
E) Osteoarthritis
Question 10:
Which radiographic sign of gouty arthritis is associated with the formation of urate crystal deposits in the joints?
A) Sawtooth-shaped opacities
B) Bone erosions
C) Tophi
D) Deposits in cartilage
E) Joint narrowing
The answers
- C) Excess uric acid in the blood (hyperuricemia)
- C) Big toe
- B) Hippocrates
- C) Disease associated with wealth
- C) Formation of urate crystals
- A) Seafood
- D) Chronic gout
- C) Allopurinol
- B) Systemic lupus erythematosus (SLE)
- C) Tophi
Questionnaire 2
- What is the term used to describe a symptom-free period between gout attacks?
- A) Interictal interval
- B) Chronic gout
- C) Tophus
- D) Acute gout
- Which joint is often the site of gout attacks, causing swelling, redness and severe pain?
- A) Elbow
- B) Wrist
- C) Knee
- D) Shoulder
- What disease mechanism distinguishes rheumatoid arthritis from gouty arthritis?
- A) Tophi formation
- B) Calcium pyrophosphate crystal deposits
- C) Phagocytosis of urate crystals
- D) Immune attack against the joints
- What is the characteristic of osteoarthritis that distinguishes it from gouty arthritis on x-rays?
- A) Sawtooth-shaped opacities
- B) Joint space narrowing
- C) Bone erosions
- D) Deposits in cartilage
- What is the role of the kidneys in eliminating uric acid?
- A) Uric acid production
- B) Phagocytosis of urate crystals
- C) Elimination of uric acid
- D) Activation of inflammation
- What is the main symptom of gouty arthritis?
- A) Skin redness
- B) Sensitivity to touch
- C) Acute joint pain
- D) Reduced mobility
- Which century saw significant advances in the understanding of gout, including recognition of the role of uric acid?
- A) 21st century
- B) 18th and 19th centuries
- C) Renaissance
- D) Middle Ages
- What medication is prescribed to improve the elimination of uric acid through the kidneys?
- A) Colchicine
- B) Allopurinol
- C) Probenecid
- D) Corticosteroids
- Which autoimmune disease can cause symptoms similar to gouty arthritis?
- A) Osteoarthritis
- B) Systemic lupus erythematosus (SLE)
- C) Ankylosing spondylitis
- D) Pseudo-gout
- What is the first step in the pathophysiology of gouty arthritis?
- A) Activation of inflammation
- B) Phagocytosis of crystals
- C) Inflammatory response
- D) Formation of urate crystals
Answers
- A) Interictal interval
- C) Knee
- B) Calcium pyrophosphate crystal deposits
- B) Joint space narrowing
- C) Elimination of uric acid
- C) Acute joint pain
- B) 18th and 19th centuries
- C) Probenecid
- B) Systemic lupus erythematosus (SLE)
- D) Formation of urate crystals
Questionnaire 3
- What is the first place to usually be affected by gout?
- Kneeling
- B) Ankle
- C) Big toe
- D) Wrist
- E) Elbow
- What is the main substance responsible for the formation of crystals in gout?
- A) Calcium
- B) Cholesterol
- C) Uric acid
- D) Sodium
- E) Glucose
- What is the main mechanism by which urate crystals trigger an inflammatory response?
- A) Phagocytosis by immune cells
- B) Fusion with other crystals
- C) Dissolution in synovial fluid
- D) Transformation into calcium
- E) Evaporation in the joint
- What is the common feature of gouty arthritis symptoms?
- A) Low mobility
- B) Skin discoloration
- C) Intense and sudden pain
- D) Asymmetric swelling
- E) Excessive sweating
- What is the stage of gout where deposits of urate crystals, called tophi, can form under the skin?
- A) Asymptomatic hyperuricemia
- B) Acute gout
- C) Interictal interval
- D) Tophaceous gout
- E) Chronic gout
- What is the preferred diagnostic method for detecting radiographic signs of gouty arthritis?
- A) Computed tomography (CT)
- B) Ultrasound
- C) Magnetic resonance imaging (MRI)
- D) Radiography
- E) Bone scintigraphy
- What is the specific medication for gout that inhibits uric acid production?
- A) Colchicine
- B) Corticosteroids
- C) Allopurinol
- D) Non-steroidal anti-inflammatory drugs (NSAIDs)
- E) Febuxostat
- What factor is often associated with increased uric acid production in people with gout?
- A) Weight loss
- B) Excessive alcohol consumption
- C) Sedentary lifestyle
- D) Vegan diet
- E) Genetic hypersensitivity
- Which joint is rarely affected by gout?
- Kneeling
- B) Ankle
- C) Shoulder
- D) Big toe
- E) Elbow
- What is the distinct characteristic of tophi in gout?
- A) Swelling of the fingers
- B) Joint deformities
- C) Nodules visible under the skin
- D) Skin redness
- E) Loss of sensitivity to touch
Answers
- C) Big toe
- C) Uric acid
- A) Phagocytosis by immune cells
- C) Intense and sudden pain
- D) Tophaceous gout
- D) Radiography
- C) Allopurinol
- B) Excessive alcohol consumption
- C) Shoulder
- C) Nodules visible under
Questionnaire 1
Question 1:
What is the main cause of gout?
A) Excess weight
B) Excessive alcohol consumption
C) Excess uric acid in the blood (hyperuricemia)
D) Genetic factors
E) Lack of exercise
Question 2:
Which part of the body is usually affected first by gout?
A) Shoulders
B) Knees
C) Big toe
D) Wristsinn
E) Hips
Question 3:
Which ancient physician described cases of joint pain associated with diet and lifestyle?
A) Galen
B) Hippocrates
C) Avicenna
D) Paracelsus
E) Rhazes
Question 4:
What is the outlook associated with gout during the Middle Ages?
A) Disease associated with sedentary lifestyle
B) Disease associated with poverty
C) Disease associated with wealth
D) Disease caused by infections
E) Disease linked to consumption of spices
Question 5:
What is the key step in the pathophysiology of gouty arthritis linked to the formation of urate crystals?
A) Activation of inflammation
B) Phagocytosis of crystals by immune cells
C) Formation of urate crystals
D) Inflammatory response
E) Adaptive immune response
Question 6:
Which food is often associated with an increased risk of gouty arthritis due to its high purine content?
A) Seafood
B) Green vegetables
C) Dairy products
D) Red fruits
E) Whole grains
Question 7:
Which stage of gout is characterized by recurrent attacks, urate crystal deposits under the skin, and persistent joint damage?
A) Acute gout
B) Interictal intervals
C) Tophaceous gout
D) Chronic gout
E) Asymptomatic hyperuricemia
Question 8:
Which drug inhibits uric acid production in the treatment of gout?
A) Colchicine
B) Corticosteroids
C) Allopurinol
D) Ibuprofen
E) Febuxostat
Question 9:
Which autoimmune disease can present with symptoms similar to gouty arthritis?
A) Diabetes
B) Systemic lupus erythematosus (SLE)
C) High blood pressure
D) Metabolic syndrome
E) Osteoarthritis
Question 10:
Which radiographic sign of gouty arthritis is associated with the formation of urate crystal deposits in the joints?
A) Sawtooth-shaped opacities
B) Bone erosions
C) Tophi
D) Deposits in cartilage
E) Joint narrowing
The answers
- C) Excess uric acid in the blood (hyperuricemia)
- C) Big toe
- B) Hippocrates
- C) Disease associated with wealth
- C) Formation of urate crystals
- A) Seafood
- D) Chronic gout
- C) Allopurinol
- B) Systemic lupus erythematosus (SLE)
- C) Tophi
References
- Neogi T. Gout. Ann Intern Med. 2016 Jul 05;165(1):ITC1-ITC16. [ PubMed ]2.
- Dalbeth N, Merriman TR, Stamp LK. Taste. Lancet. 2016 Oct 22;388(10055):2039-2052. [ PubMed ]3.
- Richette P, Bardin T. Gout. Lancet. 2010 Jan 23;375(9711):318-28. [ PubMed ]4.
- Nuki G, Simkin PA. A concise history of gout and hyperuricemia and their treatment. Arthritis Res Ther. 2006;8 Suppl 1(Suppl 1):S1. [ PMC free article ] [ PubMed ]5.
- Loeb JN. The influence of temperature on the solubility of monosodium urate. Arthritis Rheum. 1972 Mar-Apr;15(2):189-92. [ PubMed ]6.
- Nian YL, You CG. Susceptibility genes of hyperuricemia and gout. Hereditas. 2022 Aug 04;159(1):30. [ PMC free article ] [ PubMed ]7.
- Merriman TR, Choi HK, Dalbeth N. The genetic basis of taste. Rheum Dis Clin North Am. 2014 May;40(2):279-90. [ PubMed ]8.
- Choi HK, Mount DB, Reginato AM., American College of Physicians. American Physiological Society. Pathogenesis of taste. Ann Intern Med. 2005 Oct 04;143(7):499-516. [ PubMed ]9.
- Tan PK, Farrar JE, Gaucher EA, Miner JN. Coevolution of URAT1 and Uricase during Primate Evolution: Implications for Serum Urate Homeostasis and Gout. Mol Biol Evol. 2016 Sep;33(9):2193-200. [ PMC free article ] [ PubMed ]10.
- Abhishek A, Roddy E, Doherty M. Gout – a guide for the general and acute physicians. Clin Med (Lond). 2017 Feb;17(1):54-59. [ PMC free article ] [ PubMed ]11.
- Scott J.T. Asymptomatic hyperuricaemia. Br Med J (Clin Res Ed). 1987 Apr 18;294(6578):987-8. [ PMC free article ] [ PubMed ]12.
- Dalbeth N, Phipps-Green A, Frampton C, Neogi T, Taylor WJ, Merriman TR. Relationship between serum urate concentration and clinically evident incident taste : an individual participant data analysis. Ann Rheum Dis. 2018 Jul;77(7):1048-1052. [ PubMed ]13.
- Wu EQ, Patel PA, Mody RR, Yu AP, Cahill KE, Tang J, Krishnan E. Frequency, risk, and cost of taste-related episodes among the elderly: does serum uric acid level matter? J Rheumatol. 2009 May;36(5):1032-40. [ PubMed ]14.
- Dalbeth N, So A. Hyperuricaemia and taste: state of the art and future perspectives. Ann Rheum Dis. 2010 Oct;69(10):1738-43. [ PubMed ]15.
- Choi HK, Atkinson K, Karlson EW, Willett W, Curhan G. Purine-rich foods, dairy and protein intake, and the risk of taste in men. N Engl J Med. 2004 Mar 11;350(11):1093-103. [ PubMed ]16.
- Juraschek SP, Yokose C, McCormick N, Miller ER, Appel LJ, Choi HK. Effects of Dietary Patterns on Serum Urate: Results From a Randomized Trial of the Effects of Diet on Hypertension. Arthritis Rheumatol. 2021 Jun;73(6):1014-1020. [ PMC free article ] [ PubMed ]17.
- Rai SK, Fung TT, Lu N, Keller SF, Curhan GC, Choi HK. The Dietary Approaches to Stop Hypertension (DASH) diet, Western diet, and risk of taste in men: prospective cohort study. BMJ. 2017 May 09;357:j1794. [ PMC free article ] [ PubMed ]18.
- Huang HY, Appel LJ, Choi MJ, Gelber AC, Charleston J, Norkus EP, Miller ER. The effects of vitamin C supplementation on serum concentrations of uric acid: results of a randomized controlled trial. Arthritis Rheum. 2005 Jun;52(6):1843-7. [ PubMed ]19.
- Gao X, Curhan G, Forman JP, Ascherio A, Choi HK. Vitamin C intake and serum uric acid concentration in men. J Rheumatol. 2008 Sep;35(9):1853-8. [ PMC free article ] [ PubMed ]20.
- Juraschek SP, Miller ER, Gelber AC. Effect of oral vitamin C supplementation on serum uric acid: a meta-analysis of randomized controlled trials. Arthritis Care Res (Hoboken). 2011 Sep;63(9):1295-306. [ PMC free article ] [ PubMed ]21.
- Choi HK, Gao X, Curhan G. Vitamin C intake and the risk of taste in men: a prospective study. Arch Intern Med. 2009 Mar 09;169(5):502-7. [ PMC free article ] [ PubMed ]
























