Introduction
Interstitial cystitis (IC) and levator ani myofascial syndrome (LAMS) are two interconnected conditions that often coexist and share similar symptoms, impacting individuals’ daily lives significantly.
Interstitial cystitis, also known as painful bladder syndrome, involves chronic inflammation of the bladder lining. Symptoms include urinary urgency, frequency, and pelvic pain, which worsen as the bladder fills and improve after urination. Despite its name, IC isn’t just about the bladder; it involves complex interactions among the bladder, nervous system, and pelvic floor muscles. While the exact cause remains unclear, factors such as genetics, autoimmune issues, and environmental triggers may contribute.
Levator ani myofascial syndrome primarily affects the pelvic floor muscles, specifically the levator ani muscles. These muscles form a supportive structure at the base of the pelvis, crucial for pelvic organ support and controlling bowel and bladder function. In LAMS, these muscles become tense, tender, and develop trigger points, leading to symptoms like pelvic pain, discomfort with sitting, and urinary and bowel issues.
Interestingly, IC and LAMS often overlap, influencing each other’s symptoms. Chronic pelvic pain from LAMS can exacerbate urinary urgency and frequency in IC patients, while bladder irritation from IC can worsen pelvic floor muscle dysfunction, intensifying LAMS symptoms. This bidirectional relationship highlights the importance of addressing both conditions comprehensively.
Treatment for IC and LAMS typically involves a multidisciplinary approach tailored to each individual’s needs. Conservative options include dietary changes to avoid bladder irritants, pelvic floor physical therapy to release muscle tension, and stress management techniques. Medications such as pentosan polysulfate sodium and tricyclic antidepressants may be prescribed to alleviate pain and urinary symptoms in IC.
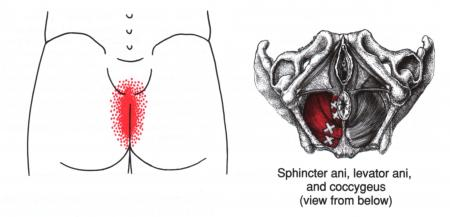
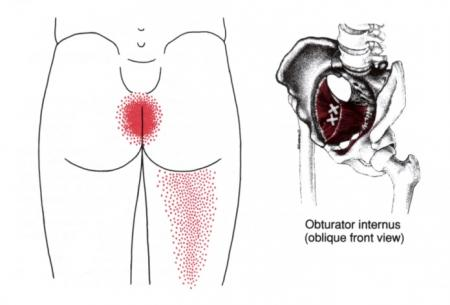
In addition to these conventional treatments, myofascial trigger point therapy can be highly beneficial for managing symptoms of both IC and LAMS. Myofascial trigger points are hyperirritable spots in skeletal muscles that can refer pain to other areas of the body. By releasing these trigger points through manual therapy techniques such as massage, stretching, and dry needling, muscle tension and pain can be reduced, providing relief from pelvic pain and discomfort associated with LAMS. Moreover, addressing trigger points in the pelvic floor muscles may also help alleviate urinary symptoms and improve bladder function in IC patients by reducing pelvic floor muscle dysfunction.
The possible viscero-somatic relationship between IC and LAMS underscores the connection between visceral (bladder) and somatic (muscle) components. Visceral pain from the bladder can manifest as somatic pain in the pelvic floor muscles, contributing to the development or exacerbation of LAMS. Conversely, pelvic floor muscle dysfunction in LAMS can lead to visceral symptoms such as urinary urgency and frequency, exacerbating IC.
Innovative Therapeutic Approaches for Interstitial Cystitis Management
Interstitial cystitis (IC), characterized by chronic pelvic pain, urinary urgency, and frequency, presents a challenging clinical scenario often resistant to conventional treatments. Recent studies have delved into innovative therapeutic approaches aimed at improving IC symptoms, offering hope to patients seeking effective relief.
Weiss (2001) introduced a novel method focusing on levator ani trigger point deactivation to address symptoms in patients with “unexplained” interstitial cystitis. By targeting trigger points in the levator ani muscles, Weiss observed significant improvements in symptomatology. This approach suggests that addressing pelvic floor muscle dysfunction may play a crucial role in managing IC-related pain and urinary symptoms.
Building upon this concept, Holzberg et al. (2001) explored transvaginal treatments targeting pelvic floor musculature to alleviate IC symptoms. In their study, 90% of IC patients experienced improvement following a regimen of intravaginal massage sessions utilizing the Thiele massage technique. This technique involves deep vaginal massage over the levator ani, obturator internus, and piriformis muscles, coupled with myofascial release targeting trigger points. The close anatomical proximity of these muscles to the bladder suggests a potential mechanism for symptom improvement through the modulation of pelvic floor muscle tone and function.
The Thiele massage technique, with its focus on myofascial release and trigger point deactivation, offers a non-invasive and potentially effective alternative for IC management. By addressing muscular dysfunction in the pelvic floor, this approach aims to alleviate pelvic pain, urinary urgency, and frequency, thus improving overall quality of life for IC patients.
Furthermore, the findings of Holzberg et al. underscore the importance of considering the visceral-somatic relationship in the pathophysiology of IC. Dysfunction in the pelvic floor musculature can contribute to bladder symptoms through mechanisms such as pelvic floor muscle spasm and neural sensitization. By targeting these muscular components, clinicians can potentially modulate bladder symptoms and enhance treatment outcomes in IC patients.
Despite the promising results of these innovative approaches, further research is warranted to elucidate their long-term efficacy and optimal application in clinical practice. Additionally, personalized treatment plans tailored to individual patient needs may enhance the effectiveness of these interventions.
Reference: Weiss, J. (2001). Unexplained” Interstitial Cystitis and Related Diseases: Pathology of Trigger Point Abnormalities in the Pelvic Floor. Journal of Urology, 165(2), 635-642.
Causes of Interstitial Cystitis (IC)
Interstitial cystitis (IC) is a chronic bladder condition characterized by inflammation and irritation of the bladder wall, leading to symptoms such as pelvic pain, frequent urge to urinate, and burning while urinating. Although the exact causes of interstitial cystitis are not fully understood, several factors have been identified as potentially involved in its development.
First, alterations in the protective lining of the bladder may play a crucial role in the occurrence of IC. The glycosaminoglycan (GAG) layer that normally covers the inner lining of the bladder acts as a protective barrier against irritants in the urine. In people with IC, this protective layer may be damaged or missing, making the bladder wall more susceptible to damage and inflammation.
Second, abnormalities of the immune system are also suspected in the development of IC. It has been observed that many patients with IC show signs of an abnormal immune response, characterized by chronic inflammation of the bladder wall. This inflammation can be triggered by a variety of factors, including recurrent bacterial infections, tissue damage, or chemical irritants in the urine.
Third, genetic factors may predispose some people to developing IC. Studies have shown that interstitial cystitis can sometimes occur in several members of the same family, suggesting a genetic component in its development. However, the exact mechanisms by which genes may influence susceptibility to IC are not yet completely understood.
Additionally, some experts have speculated that neurological disorders may contribute to the occurrence of IC. The autonomic nervous system, which regulates involuntary body functions such as urination, may be dysfunctional in people with IC, leading to increased bladder sensitivity and associated painful symptoms.
Finally, certain environmental and behavioral factors can also worsen IC symptoms. For example, excessive consumption of certain foods or drinks, such as spicy foods, citrus fruits, coffee, and alcohol, can irritate the bladder and trigger symptom flare-ups in people with IC.
Interstitial cystitis is a complex condition and the exact causes are not completely understood. However, several factors can contribute to the development of IC, including:
- Mucosal Barrier Alterations: Alterations in the protective layer of the bladder lining can make the bladder more vulnerable to irritation.
- Abnormal Immune Response: An abnormal immune response could cause chronic inflammation of the bladder wall.
- Genetic Factors: Some individuals appear to have a genetic predisposition to developing IC.
- Neurological Defects: Neurological problems can influence pain perception and play a role in the development of IC.
- Previous Infection: Some cases of IC are preceded by urinary tract infections.
- Hormonal Factors: Sex hormones can influence the severity of symptoms, partly explaining why IC is more common in women.
Symptoms of Interstitial Cystitis (IC)
Symptoms of interstitial cystitis (IC) can vary from person to person, but they are often debilitating and have a significant impact on patients’ quality of life. IC is characterized by chronic inflammation of the bladder wall, leading to a variety of persistent urinary and pelvic symptoms.
Pelvic pain is one of the most common and disabling symptoms associated with IC. Patients with this condition may experience intense, persistent pain in the pelvic area, sometimes described as a burning or pressure sensation. This pain may be constant or come in spurts, and it may be exacerbated by urination or sexual activity, making daily activities difficult for many patients to tolerate.
Another common feature of IC is increased urinary frequency. Patients may feel the need to urinate frequently, even if their bladder is not full, which can disrupt their sleep and daily routine. This increase in urinary frequency is often accompanied by an urgent feeling to urinate, where patients feel a strong need to go to the toilet that can be difficult to delay.
In addition to pelvic pain and increased urinary frequency, many patients with IC experience pain when urinating. This pain, often described as a burning or tingling sensation, can be particularly intense and unpleasant, making the process of urination very uncomfortable.
Additionally, some patients experience nonspecific symptoms such as muscle pain, fatigue, and sleep disturbances, which may be associated with IC. These additional symptoms can worsen patients’ emotional and physical distress, contributing to a decrease in their overall quality of life.
It is important to note that IC symptoms can vary in intensity and frequency over time, with periods of remission and symptom flares. Some patients may experience a spontaneous improvement in their symptoms, while others may experience a worsening of their symptoms in response to certain triggers such as stress, certain foods or drinks, or urinary infections.
Symptoms of interstitial cystitis vary from individual to individual, but they generally include:
- Pelvic Pain: Patients often feel pain in the pelvic area, between the vagina and anus in women and between the scrotum and anus in men (perineum).
- Chronic Pelvic Pain: Persistent and chronic pain in the pelvic region is commonly observed.
- Urgent and Persistent Need to Urinate: Patients experience a frequent and urgent need to urinate, often in small quantities, throughout the day and night (up to 60 times per day).
- Pain or Discomfort During Urination: Urination can be painful, and relief is usually felt after urinating.
- Pain during Sexual Intercourse: Pain can also be felt during sexual intercourse.
- Evolution of Symptoms: Symptoms may change over time and periodically clear up in response to triggers such as menstruation, prolonged sitting, stress, physical and sexual activity.
Triggering Factors and Prevalence
Interstitial cystitis (IC), also known as painful bladder syndrome, is a condition characterized by chronic inflammation of the bladder wall. Although the triggers for IC are not always clear, certain things can worsen symptoms and trigger episodes of intense discomfort.
Potential triggers for interstitial cystitis include various acidic foods such as tomatoes, citrus fruits, coffee, chocolate, and caffeinated drinks. These elements can irritate the bladder wall and exacerbate symptoms of inflammation, contributing to the occurrence of painful attacks. Food sensitivity varies from person to person, and people with IC are often recommended to maintain a food diary to identify specific triggers that may worsen their symptoms.
Stress is also recognized as a potential trigger for interstitial cystitis. Stressful situations can impact the immune system and trigger inflammatory responses, worsening IC symptoms. Managing stress through relaxation techniques, meditation, or other methods can play an important role in reducing episodes of discomfort associated with IC.
Certain body positions can also influence the frequency and severity of interstitial cystitis symptoms. Positions that put increased pressure on the pelvic region can make discomfort worse. This may include strenuous physical activities or prolonged positions, such as sitting for long periods of time. Lifestyle adjustments, such as changes in postural habits, may be recommended to minimize these impacts.
Regarding the prevalence of interstitial cystitis, although it can affect both sexes, it is more common in women. Statistics indicate that the prevalence of IC increases with age, often affecting people over the age of 40. However, it is important to note that interstitial cystitis can also occur in young adults.
In conclusion, interstitial cystitis is a complex condition whose triggers are not always clear. However, factors such as acidic foods, caffeine, stress and certain body positions have been identified as things that can make symptoms worse. The prevalence of IC is higher in women and increases with age, although cases can also occur in younger people. Managing potential triggers and adopting stress management strategies can play a crucial role in improving the quality of life of people with interstitial cystitis.
Impacts on Patient Quality of Life
Interstitial cystitis has a significant impact on patients’ quality of life, going beyond medical aspects to encompass physical, emotional and social dimensions. The disabling symptoms of this condition, such as persistent pelvic pain and increased urinary frequency, can cause significant limitations in patients’ ability to lead normal lives.
On a physical level, daily activities are often compromised due to interstitial cystitis. Labor may become difficult to maintain due to frequent interruptions to satisfy the urgent need to urinate. Social relationships may also be impacted, as patients may feel reluctant to participate in social activities due to the pain and constraints associated with the condition. Leisure and relaxation activities can become a challenge, which can lead to a reduction in overall quality of life.
From a psychological perspective, constantly dealing with the pain and symptoms of interstitial cystitis can lead to feelings of frustration, anxiety, and depression. Patients may have difficulty coping with the chronic nature of the disease and unpredictable fluctuations in their symptoms. The stress of dealing with interstitial cystitis on a daily basis can also affect individuals’ overall mental health.
The management of interstitial cystitis is not limited to the medical dimension. In addition to medical treatments aimed at relieving symptoms, a holistic approach also involves emotional support and lifestyle adaptation. Healthcare professionals can provide psychological support to help patients cope with the emotional aspects of the illness. Lifestyle changes, such as dietary adjustments and stress management strategies, can help improve overall quality of life.
It is crucial that patients with interstitial cystitis are encouraged to express their concerns and work collaboratively with their medical team to develop a management plan tailored to their specific needs. Educating patients about the disease, access to support resources and integrating coping strategies into their daily lives are essential elements to mitigate the negative impacts on quality of life and promote better management of the disease. interstitial cystitis.
Diagnosis of Interstitial Cystitis
The diagnosis of interstitial cystitis can be complex due to the variability of symptoms and the lack of specific markers. Diagnostic methods include:
- Medical History and Clinical Examination: The doctor collects information about symptoms, medical history and performs a physical examination to rule out other possible causes.
- Cystoscopy: A cystoscopy may be performed to examine the inside of the bladder. Signs of inflammation and lesions characteristic of IC may be observed.
- Biopsy: A biopsy of the bladder wall may be performed during cystoscopy to confirm the diagnosis by identifying changes characteristic of IC.
- Eliminating Other Conditions: Since IC symptoms can mimic other conditions, the doctor may perform tests to rule out UTIs, kidney stones, and other conditions.
- Diagnostic Criteria: The diagnostic criteria for IC have been defined by the International Interstitial Cystitis Society (ICSI). These criteria include the presence of persistent bladder-related pelvic pain and the frequent and urgent need to urinate, among others.
- Voiding Diary: The patient may be asked to keep a voiding diary to record times and triggers of symptoms, providing valuable information for diagnosis.
Osteopathy and Interstitial Cystitis (IC)
Osteopathy, as a holistic approach focused on understanding the interactions between different structures of the body, offers an interesting perspective in the management of the symptoms of interstitial cystitis (IC). Although research into the specific effectiveness of osteopathy in the context of IC is ongoing, some studies and clinical cases suggest that this approach may play a beneficial role in the management of this condition.
Potential Role of Osteopathy
- Reduction of Muscle Tension: Osteopathy focuses on the structural and functional balance of the body. In the case of IC, where symptoms may be associated with pelvic floor muscle tension, osteopathy may aim to reduce this tension, thereby promoting a more relaxed environment for the bladder.
- Improving Pelvic Mobility: By working on the mobility of joints and soft tissues in the pelvic region, osteopathy can help alleviate movement restrictions that could worsen IC symptoms.
- Influence on Neurological Connections: Osteopathy can also act on the nervous system, improving communication between different parts of the body. This could potentially have a positive impact on the perception of pain associated with IC.
Clinical Studies and Cases
Although research into the effectiveness of osteopathy specifically for IC is limited, some studies suggest encouraging results in managing symptoms associated with pelvic disorders.
A study by Weiss in 2001 reported significant improvement in symptoms of patients with “unexplained” IC using methods of deactivating levator ani trigger points, thus highlighting the importance of muscle treatment in the management of IC. THIS.
Another study by Holzberg et al in 2001 evaluated the effectiveness of transvaginal treatments in patients with IC using the Thiele massage technique on the pelvic floor musculature. The results showed improvement in 90% of treated patients.
These findings suggest that osteopathic approaches, particularly those focused on treating the pelvic floor muscles, may play a significant role in managing IC symptoms. However, further research is needed to consolidate these findings and better understand the mechanisms underlying the potential effectiveness of osteopathy in the context of IC.
Levator Ani Muscle Syndrome
Levator ani muscle syndrome is a condition characterized by chronic tension or spasm of the levator ani muscle, which is part of the pelvic floor. This syndrome can cause a variety of unpleasant symptoms and affect the quality of daily life of affected individuals.
Characteristics of Levator Ani Muscle Syndrome
- Muscle Tension or Spasm: The levator ani muscle, located in the pelvic region, may develop persistent tension or spasm, causing uncomfortable sensations.
- Pelvic Pain: People with levator ani syndrome often experience chronic pain in the pelvic area. This pain can be localized and can vary in intensity.
- Urinary Symptoms: Urinary symptoms such as increased urinary frequency, urgent need to urinate, and pain during urination may be associated with this syndrome due to the proximity of the levator ani muscle to the bladder structures.
- Pain During Sex: As with interstitial cystitis (IC), levator ani syndrome may also be associated with pain during sex.
Relationship with Interstitial Cystitis (IC)
The relationship between levator ani syndrome (LAMS) and interstitial cystitis (IC) is a complex topic that requires an in-depth understanding of the physiological mechanisms and interactions between these two conditions. The levator ani muscle, a group of muscles located in the pelvic floor, plays a vital role in supporting the pelvic organs, including the bladder. Excessive tension or spasms in this muscle can have implications on bladder function and worsen interstitial cystitis symptoms.
It is important to note that levator ani syndrome and interstitial cystitis can coexist in some individuals, creating a situation where the symptoms of one condition may influence or worsen those of the other. The levator ani muscle surrounds the opening to the urethra and anus, and its tension can cause compression of the bladder, causing symptoms similar to interstitial cystitis, such as pelvic pain and urinary frequency. increased.
Some patients with interstitial cystitis may develop levator ani syndrome in response to chronic pain or other factors associated with IC. Persistent pain in the pelvic region can cause the levator ani muscle to become protective, resulting in increased tension. Additionally, fear of pain during urination can lead to involuntary contraction of the muscle, causing painful spasms.
The coexistence of these two conditions can create a vicious cycle, where the pain of interstitial cystitis leads to tension in the levator ani muscle, in turn worsening the symptoms of IC. Patients may also experience difficulty urinating due to muscle contraction, which adds a layer of complexity to the management of these co-occurring conditions.
Diagnosis of levator ani syndrome in patients with interstitial cystitis can be complicated due to overlapping symptoms. Specialized physical examinations, such as palpation of the levator ani muscle, may be used to identify the presence of muscle tension. Medical imaging, such as pelvic MRI, may also be performed to assess muscle structure and function.
Management of this complex association of interstitial cystitis and levator ani syndrome often involves a multidisciplinary approach. Treatments may include muscle relaxation techniques, pelvic physiotherapy, medications to relieve pain, and psychological approaches to manage the stress and anxiety associated with these conditions.
So, the relationship between levator ani muscle syndrome and interstitial cystitis is intrinsically linked to complex mechanisms. The coexistence of these two conditions can create diagnostic and therapeutic challenges. A holistic approach, taking into account physical and emotional aspects, is essential to optimize the care of these patients. Thoroughly understanding the dynamics between these two conditions helps guide treatment strategies aimed at improving the quality of life of affected individuals.
Osteopathy and Levator Ani Muscle Syndrome
Osteopathy offers a holistic approach that can be beneficial in relieving symptoms associated with levator ani syndrome. By working on the structure and function of the pelvic floor, osteopaths aim to reduce muscle tension, improve mobility and restore balance to the body. Here is how osteopathy can be used to help people suffering from levator ani muscle syndrome:
Full Assessment
- The osteopath will begin by performing a comprehensive evaluation by taking a medical history, assessing symptoms, and performing a physical exam. This assessment will help understand muscle tension patterns and specific structural imbalances.
Muscle Relaxation
- Osteopathic muscle release techniques can be used to reduce excess tension in the levator ani muscle. This may include gentle manipulation, stretching, and myofascial release techniques.
Pelvic Floor Rebalancing
- Osteopathy aims to restore the structural balance of the pelvic floor by working on all structures, including the muscles, joints and surrounding tissues. Specific manipulations can be applied to improve symmetry and mobility.
Trigger Point Deactivation Techniques
- Osteopaths can use trigger point deactivation techniques to release specific areas of the levator ani muscle that may be causing pain and spasm. These techniques aim to reduce irritation and restore normal muscle function.
Global approach
- By adopting a global approach, the osteopath can also explore other regions of the body likely to influence levator ani muscle syndrome. This may include examining the spine, pelvis, and other related structures.
Lifestyle Advice
- In addition to manual techniques, the osteopath can provide lifestyle advice, including specific exercises, postures and relaxation practices that can help maintain the benefits of treatment.
Self-Care Tips for Interstitial Cystitis (IC) and Levator Ani Muscle Syndrome
- Adequate Hydration: Maintain adequate hydration by drinking enough water throughout the day. This can help dilute urine and reduce bladder irritation.
- Avoid Food Irritants: Identify and avoid foods and drinks that may worsen symptoms, such as caffeine, citrus fruits, spicy foods, and products containing alcohol.
- Gentle Intimate Cleansing: Practice gentle intimate cleansing using a fragrance-free soap and avoiding irritating products. Avoid bubble baths and favor showers.
- Heat Application: Use a hot water bottle or heating pad to relieve pelvic pain. Heat can help relax muscles and ease discomfort.
- Stress Management: Adopt stress management techniques such as meditation, deep breathing, yoga or cognitive therapy. Stress can exacerbate symptoms.
- Toilet Scheduling: Establish a regular schedule for toilet visits to reduce pressure on the bladder and avoid prolonged urinary retention.
- Pelvic Floor Strengthening Exercises: Practice pelvic floor strengthening exercises, such as Kegel exercises, to strengthen the pelvic muscles and improve stability.
- Avoid Tight Clothing: Choose loose, comfortable clothing to avoid excessive pressure on the pelvic region.
- Maintain a Healthy Weight: Maintain a healthy weight, as excess weight can put extra pressure on the pelvic area.
- Trigger Tracker: Keep a symptom diary to identify specific triggers and adjust your lifestyle accordingly.
- Regular Medical Consultation: Schedule regular medical consultations with your healthcare professional for appropriate follow-up and to adjust the treatment plan as needed.
- Relaxation Practices: Incorporate relaxation practices into your daily routine, such as warm baths, reading, or listening to calming music.
- Communication with Healthcare Professional: Communicate openly with your healthcare professional about the effectiveness of treatments and any changes in your symptoms.
Importance of Medical Collaboration in the Management of Interstitial Cystitis (IC) and Levator Ani Muscle Syndrome:
List
- Accurate Diagnosis:
- IC and levator ani syndrome can have complex clinical presentations. Collaboration between doctors and osteopaths allows for a more accurate diagnosis by combining traditional medical knowledge and holistic approaches to osteopathy.
- Complete Treatment Plan:
- By collaborating, healthcare professionals can design a comprehensive treatment plan that integrates medical, osteopathic, and potentially other therapeutic modalities. This provides patients with a comprehensive, personalized approach to managing their symptoms.
- Regular Monitoring:
- Collaboration allows for regular monitoring and ongoing assessment of the patient’s progress. Necessary adjustments can be made based on response to treatment, thus ensuring dynamic and appropriate care.
- Exchange of information :
- Healthcare professionals share crucial information about medical histories, test results and clinical observations. This allows for a complete understanding of the clinical picture, thereby improving coordination of care.
- Multidisciplinary support:
- Disorders such as IC and levator ani syndrome often involve physical, emotional and psychological aspects. Multidisciplinary care which includes osteopaths, urologists, physiotherapists and other health professionals ensures a holistic approach addressing all these aspects.
- Optimization of Results:
- Medical collaboration aims to optimize patient outcomes. By working together, healthcare professionals can identify the best complementary treatments, maximizing the chance of improving the patient’s quality of life.
- Patient Education:
- Physicians and osteopaths play a vital role in educating patients about their condition. Collaboration facilitates the communication of consistent and accurate information, allowing patients to understand their condition and be fully involved in their own care.
- Risk Reduction:
- Collaboration reduces the risks associated with making unilateral decisions. Healthcare professionals work together to minimize the potential risks of treatments, particularly when it comes to medical or osteopathic procedures.
- Better Acceptance of Treatment:
- Collaboration promotes an inclusive approach that takes into account patient preferences. This contributes to greater acceptance of treatment, thereby improving compliance and long-term outcomes.
- Research and Innovation:
- Collaboration between the medical and osteopathic fields can encourage research and innovation. By sharing clinical experiences, data and observations, professionals contribute to the advancement of knowledge and the improvement of clinical practices.
Reference
- Weiss JM. Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. J Urol. 2001 Nov;166(5):2226-31. doi: 10.1016/s0022-5347(05)65534-7. PMID: 11586239.
- Holzberg AS, Kellog-Spadt S, Lukban JC, Whitmore KE. Pelvic floor muscle physical therapy for patients with interstitial cystitis. Am J Obstet Gynecol. 2001 Jun;184(7):1381-3. doi: 10.1067/mob.2001.114465. PMID: 11349278.
- van de Merwe JP, Nordling J, Bouchelouche P, Bouchelouche K, Cervigni M, Daha LK, Elneil S, Fall M, Hohlbrugger G, Irwin P, Mortensen S, van Ophoven A, Osborne JL, Peeker R, Richter B, Riedl C , Sairanen J, Tinzl M, Wyndaele JJ. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: an ESSIC proposal. Eur Urol. 2008 Jan;53(1):60-7. doi: 10.1016/j.eururo.2007.09.019. Epub 2007 Sep 27. PMID: 17911066.
- Tomaszewski JE, Landis JR, Russack V, Williams TM, Wang LP, Hardy C, Brensinger C, Matthews YL, Abele ST, Kusek JW, Nyberg LM; Interstitial Cystitis Database Study Group. Biopsy features are associated with primary symptoms in interstitial cystitis: results from the interstitial cystitis database study. Urology. 2001 Oct;58(4):552-7. doi: 10.1016/s0090-4295(01)01319-7. PMID: 11597547.
- Kavvadias T, Baessler K, Schuessler B. Effect of intravaginal electrical stimulation on pelvic floor muscle strength. Int Urogynecol J Pelvic Floor Dysfunct. 2006 Sep;17(5):487-92. doi:10.1007/s00192-005-0032-9. Epub 2006 Feb 8. PMID: 16465399.
- Fariello JY, Whitmore KE. Pelvic floor disorders and interstitial cystitis. Urol Clin North Am. 2008 Nov;35(4):499-506, vii. doi: 10.1016/j.ucl.2008.07.013. PMID: 18992618.
- Parsons CL, Zupkas P, Parsons JK. Intravesical potassium sensitivity in patients with interstitial cystitis and urethral syndrome. Urology. 2001 Feb;57(2):428-32. doi: 10.1016/s0090-4295(00)00915-4. PMID: 11182357.
- Parsons CL, Benson G, Childs SJ, Hanno P, Sant GR, Webster G. A quantitatively controlled method to study prospectively interstitial cystitis and demonstrate the efficacy of pentosanpolysulfate. J Urol. 1993 Apr;149(4):1035-8. doi: 10.1016/s0022-5347(17)36001-4. PMID: 8455257.
- Rackley RR, Abdelmalak JB, Madigan EM, Goldman HB. The effect of intravesical dimethyl sulfoxide, sodium bicarbonate, and pentosan polysulfate on urothelial permeability. J Urol. 1999 Mar;161(3):948-51. doi: 10.1016/s0022-5347(01)61906-8. PMID: 10022776.
- Nickel JC, Moldwin R, Lee S, Davis EL, Henry RA, Wyllie MG. Intravesical alkalinized lidocaine (PSD597) offers sustained relief from symptoms of interstitial cystitis and painful bladder syndrome. BJU Int. 2009 Apr;103(7):910-8. doi: 10.1111/j.1464-410X.2008.08136.x. Epub 2009 Jan 13. PMID: 19143914.