Introduction
Lumbar spondylosis is a common spinal pathology, characterized by the progressive degeneration of the anatomical structures of the lumbar region. It mainly affects older people, but factors such as posture, intense physical activity, repetitive microtrauma, and even genetic predispositions can accelerate this process. Lumbar spondylosis manifests itself by wear and tear of the intervertebral discs, vertebrae, and posterior joints, leading to loss of flexibility, pain, and neurological dysfunction. This condition, although often perceived as an inevitable aspect of aging, can have a significant impact on the quality of life of individuals, making management essential to prevent complications and maintain good mobility.
As a degenerative pathology, lumbar spondylosis is distinguished by a series of anatomical and functional changes that alter the spine. The most common changes include a reduction in the thickness of the intervertebral discs, bone changes such as the formation of osteophytes (bony growths), as well as alterations of the joint facets. These changes lead to an increase in mechanical stress on the spine, causing pain, stiffness and, in some cases, neurological complications such as nerve compressions.
General Presentation and Definition
Lumbar spondylosis refers to a series of degenerative changes affecting the structures of the lumbar spine, which usually develop with age. It is a general term that includes several degenerative conditions such as arthrosis of the facet joints, disc degeneration and the appearance of osteophytes. This degenerative process affects the bony elements and soft tissues surrounding the vertebrae, with particular involvement of the intervertebral discs and the zygapophyseal joints. The discs, losing their elasticity and ability to absorb shocks, become thinner and more rigid, increasing the pressure on the joints and neighboring vertebrae.
The appearance of these lesions can lead to compensation phenomena and an overall imbalance of spinal mechanics. In response to degenerative changes, the body often develops bony growths, called osteophytes, to stabilize the spine. However, these growths can cause nerve compressions or narrowing of the spinal canal, generating pain and neurological symptoms.
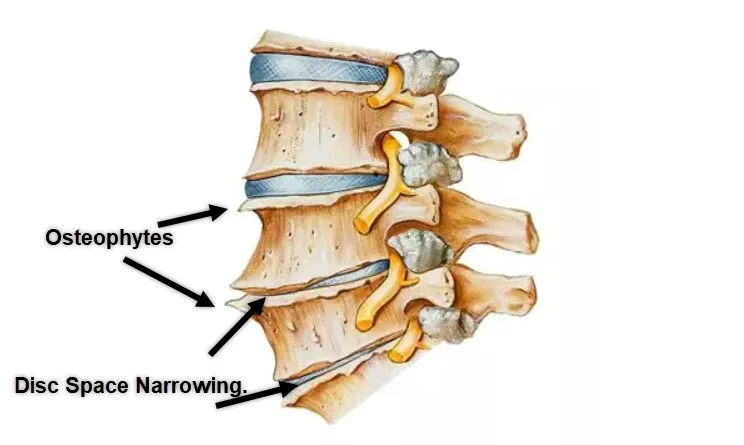
Osteophytes, commonly known as bone spurs, are bony growths that develop along the edges of vertebrae in response to wear and tear or inflammation. These growths often form as a compensatory mechanism to stabilize the spine but can lead to stiffness, limited mobility, and nerve compression, causing pain or discomfort.
Disc space narrowing refers to the reduction in the height of the intervertebral discs, which act as shock absorbers between the vertebrae. Over time, wear and tear, dehydration, or injury can cause the discs to lose elasticity and thickness, resulting in reduced space between vertebrae. This can lead to increased friction, joint stress, and potentially pinched nerves.
Together, these degenerative changes can contribute to conditions like lower back pain, sciatica, or spinal stenosis. While these changes are common with aging, they may also result from repetitive stress, obesity, or poor posture. Treatment typically includes physical therapy, medications, or, in severe cases, surgery to alleviate symptoms and improve quality of life.
Importance of Osteopathy in Care
Osteopathy plays a central role in the management of lumbar spondylosis. Unlike a purely symptomatic approach, osteopathy offers a global assessment of the body to understand the origin of pain and dysfunction. Osteopathic practitioners analyze postural imbalances and mechanical dysfunctions that could promote or aggravate lumbar degeneration. Thanks to a range of manual techniques, the osteopath can mobilize restricted vertebral segments, release muscular and fascial tensions, and correct structural misalignments.
Osteopathic intervention aims not only to reduce painful symptoms, but also to improve mobility, flexibility and functionality of the spine. Myofascial release techniques, for example, help reduce tension in the paravertebral muscles, while joint mobilization techniques aim to restore flexibility in the lumbar segments.
In addition, osteopathy can play a preventive role in the management of lumbar spondylosis. The osteopath helps patients adopt a better posture, strengthen their stabilizing muscles and integrate specific exercises to maintain the health of their spine. Osteopathic support can also include advice on lifestyle, ergonomics at work and adapted physical activity, in order to prevent the worsening of degenerative lesions.
Anatomy and Pathophysiology of Lumbar Spondylosis
Lumbar spondylosis is a degenerative process that involves various structures of the spine, including the vertebrae, intervertebral discs, ligaments, and zygapophyseal joints (or facet joints). To better understand this pathology, it is essential to become familiar with the anatomy of the lumbar region and explore how degenerative changes affect these structures.
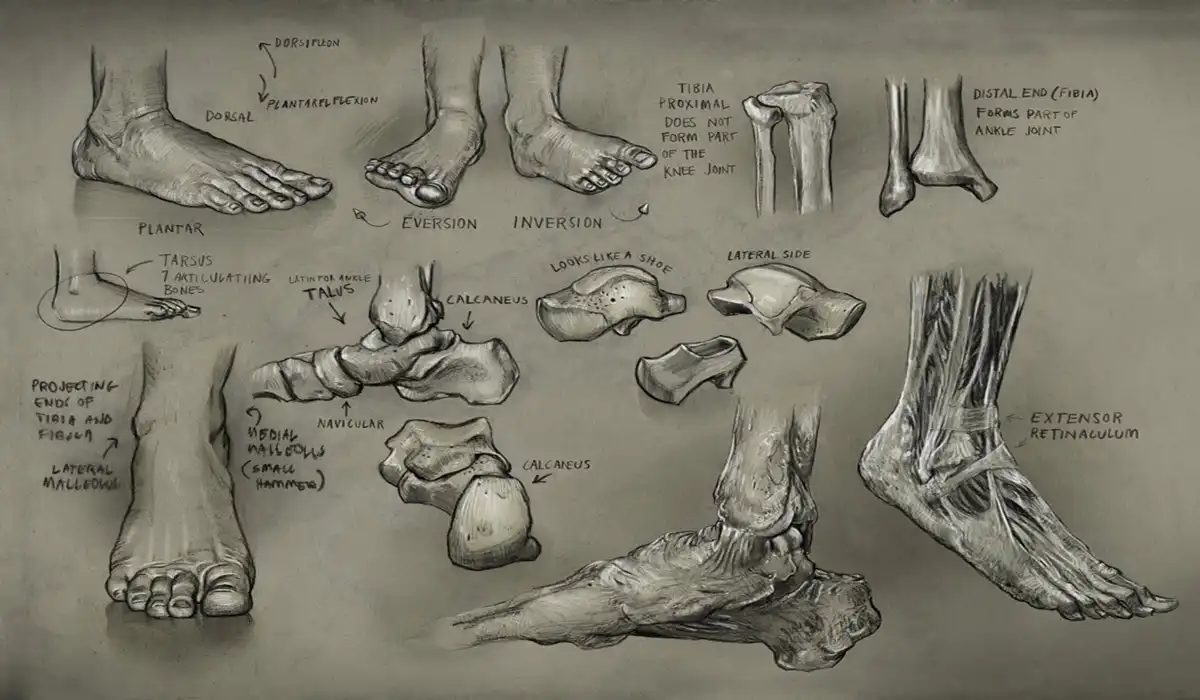
Anatomy of the Lumbar Spine
The lumbar spine is composed of five vertebrae (L1 to L5), located between the thoracic spine and the sacrum. Each of these vertebrae is separated by an intervertebral disc, which plays a crucial role in shock absorption and load distribution. The discs are composed of a gelatinous nucleus pulposus surrounded by a solid fibrous ring. The articular facets, for their part, are small joints located at the back of the vertebrae that allow the flexion, extension and rotation movements of the spine.
The primary role of the lumbar spine is to support the weight of the upper body while allowing some mobility and flexibility. However, this region is subjected to significant mechanical stress, making it vulnerable to wear and degenerative injuries.
Degenerative Changes and Pathophysiology
Lumbar spondylosis occurs when degenerative changes begin to affect the supporting structures of the lumbar spine. The degenerative process often begins with a progressive degradation of the intervertebral discs. With age, the discs lose their hydration and elasticity, leading to a decrease in their ability to absorb shock and a loss of height. This phenomenon of disc degeneration increases the compressive forces on the facet joints and neighboring vertebrae.
In response to this mechanical overload, the zygapophyseal joints can develop osteoarthritis, characterized by degradation of articular cartilage, local inflammation, and formation of bony growths (osteophytes). These osteophytes can grow along the edges of the vertebrae, contributing to stiffness and decreased mobility. When they become too large, osteophytes can also put pressure on nerve roots, leading to radiating pain and neurological symptoms.
The ligaments of the lumbar spine, such as the ligamentum flavum and interspinous ligaments, can also be affected by lumbar spondylosis. Over time, these ligaments lose their elasticity and become calcified, further limiting the movement of the spine and worsening stiffness.
Functional Consequences
The degenerative changes seen in lumbar spondylosis lead to impaired mobility and stability of the spine. The decreased thickness of the intervertebral discs reduces the space between the vertebrae, increasing pressure on the joints and nerve roots. This compression can cause chronic low back pain, radiating to the lower limbs (sciatica), and neurological disorders such as numbness and tingling.
Arthritis of the facet joints, which often accompanies disc degeneration, also contributes to spinal stiffness and decreased flexibility. Patients with lumbar spondylosis frequently complain of lower back pain that is aggravated by prolonged standing, walking, or flexion and extension movements.
In addition, degeneration of the lumbar structures leads to compensatory phenomena in the rest of the body. For example, a decrease in lumbar mobility can be compensated by an increase in the stress on the hips and knees, which can lead to pain and dysfunction in these regions. In addition, patients may adopt an inappropriate posture to relieve pain, which can lead to postural imbalances and additional muscle tension.
Causes and Risk Factors
Aging and Mechanical Wear
One of the main causes of lumbar spondylosis is the natural aging process. With age, the intervertebral discs gradually lose their ability to retain water, leading to a decrease in their thickness and elasticity. This dehydration of the discs makes the spine less able to withstand daily mechanical stresses. As a result, the vertebral segments become stiffer and the flexibility of the spine is reduced, creating a breeding ground for the development of facet joint osteoarthritis and osteophytes.
In addition to aging, mechanical wear and tear from daily activities plays a major role in the development of lumbar spondylosis. Repetitive movements, excessive lifting efforts, or prolonged poor posture increase the stress on the spinal structures. This mechanical overload leads to progressive wear and tear of the intervertebral discs and zygapophyseal joints.
Bad Posture and Intense Physical Activities
Posture plays a crucial role in the development of lumbar spondylosis. People with poor posture, such as lumbar hyperlordosis or anterior pelvic tilt, put excessive pressure on certain areas of their spine. In the long term, this mechanical overload can accelerate the wear of the intervertebral discs and promote the appearance of osteophytes.
In addition, intense physical activities, including contact sports, bodybuilding, or professions requiring repetitive physical effort, increase the risk of accumulated microtraumas. These microtraumas accelerate the degeneration process and promote arthritic changes in the joint facets.
Genetic Factors and Family Predispositions
Genetic predispositions may also play a role in the development of lumbar spondylosis. Studies have shown that some people are genetically more likely to develop early disc degeneration. These predispositions may include structural weakness of the intervertebral discs, congenital anomalies of the spine, or an inherited tendency to develop osteophytes.
Heredity can also influence posture and spinal alignment, which indirectly contributes to the development of lumbar spondylosis. Therefore, people with a family history of degenerative spinal pathologies should pay particular attention to their posture and lifestyle to prevent worsening of symptoms.
Obesity and Overweight
Excess weight is a major risk factor for lumbar spondylosis. Obesity puts additional pressure on the spine, especially on the intervertebral discs and facet joints. This overload increases mechanical stress, thereby accelerating the degeneration process. In addition, obesity is often associated with muscle weakness and poor posture, which further aggravates spinal dysfunction.
Overweight people are also more likely to develop other degenerative conditions, such as osteoarthritis of the knees and hips, which can change their gait and posture, and therefore have a negative impact on the lumbar spine.
Trauma and Repeated Microtrauma
Acute trauma, such as car accidents, falls or severe impacts, can cause significant damage to the lumbar structures, thus promoting the development of lumbar spondylosis. Direct trauma can cause cracks in the intervertebral discs, damage the facet joints or cause vertebral fractures, which can trigger early degenerative processes.
At the same time, repeated microtraumas resulting from professional or sporting activities, such as frequent lifting, prolonged vibrations or repetitive bending, contribute to the progressive wear of the structures of the spinal column. These microtraumas create cumulative lesions over time, promoting the degeneration of discs and joints.
By identifying the causes and risk factors of lumbar spondylosis, it becomes possible to develop effective preventive and management strategies to limit the progression of this degenerative pathology and reduce the impact of symptoms on quality of life.
Symptoms and Clinical Manifestations
Lower Back Pain and Stiffness
One of the most common symptoms of lumbar spondylosis is lower back pain, which can vary in intensity and location. The pain is often described as a feeling of stiffness, heaviness, or tension in the lower back. It tends to worsen with prolonged physical activity, flexion or extension movements of the spine, or after prolonged sitting. This pain is caused by wear and tear of the supporting structures, such as the intervertebral discs and facet joints, as well as inflammatory reactions and irritation of local nerves.
Stiffness of the spine, especially in the morning upon waking, is another common symptom. This stiffness is the result of reduced disc thickness and osteoarthritis of the facet joints. With the loss of flexibility, the mobility of the lumbar spine becomes increasingly limited, leading to difficulty in performing certain movements or maintaining prolonged positions.
Associated Neurological Symptoms
Lumbar spondylosis can also cause neurological symptoms due to compression of the nerve roots or narrowing of the spinal canal. Osteophytes, or bony growths, as well as decreased space between the vertebrae, can cause compression of the nerve roots exiting the lumbar spine. This nerve compression can cause pain radiating into the lower extremities, often described as sciatic pain or radicular pain.
In addition to pain, patients may also experience numbness, tingling, or weakness in the legs. These symptoms are often made worse by certain positions, such as prolonged standing or walking. In more severe cases, nerve compression can lead to loss of sensation or significant muscle weakness, limiting mobility and daily activities.
Alteration of Mobility and Quality of Life
Lumbar spondylosis has a direct impact on the mobility and quality of life of those affected. Stiffness and lower back pain limit the movements of the spine, making certain daily activities, such as bending to pick up an object or climbing stairs, difficult or even painful. The reduced flexibility of the spine can also change the patient’s gait and posture, leading to compensations in other areas of the body.
Because of these limitations, people with lumbar spondylosis may restrict their physical activities, leading to a decrease in overall fitness and eventual weight gain. This vicious cycle further increases the pressure on the spine, increasing pain and functional limitations.
Postural Disorders and Muscle Imbalances
Pain and stiffness caused by lumbar spondylosis often lead to postural changes and muscle imbalances. Patients may adopt inappropriate postures to avoid pain, such as leaning forward or excessive arching of the lumbar spine. These postural adaptations can cause additional muscle tension, particularly in the paraspinal muscles, glutes, and hamstrings.
Muscle imbalances created by lumbar spondylosis can worsen pain and functional limitations. For example, decreased lumbar mobility can lead to overuse of the hip and knee muscles, increasing the risk of developing joint pain in these areas. In addition, muscle tension and imbalances can promote the development of myofascial trigger points, which further exacerbate pain and stiffness.
Sleep Disturbances and Chronic Fatigue
Nighttime pain caused by lumbar spondylosis often disrupts patients’ sleep, leading to chronic fatigue and decreased energy. Lack of restorative sleep impairs the body’s ability to regenerate and recover, further exacerbating pain perception and morning stiffness. In addition, chronic fatigue can reduce patients’ motivation to stay active and exercise, increasing functional limitations and the risk of weight gain.
Psychological impact
Chronic pain and functional limitations associated with lumbar spondylosis often impact patients’ mental health. The inability to perform daily activities or participate in leisure activities can lead to feelings of frustration, depression, or anxiety. Fear of causing pain can also limit patients’ engagement in physical activities, leading to a decreased quality of life.
By addressing these symptoms and clinical manifestations holistically, it becomes possible to better understand the impact of lumbar spondylosis on patients and to develop tailored management strategies to reduce pain and improve function.
Diagnosis and Imaging
Clinical Assessment and Physical Examination
The diagnosis of lumbar spondylosis is based primarily on a thorough clinical assessment and physical examination by a qualified healthcare professional, such as an osteopath, general practitioner, or spine specialist. During the physical examination, the practitioner seeks to identify signs of degeneration and assess the extent of the symptoms experienced by the patient. This assessment usually begins with a detailed history, in which the patient describes the history of their symptoms, their duration, location, intensity, and aggravating or relieving factors.
The physical examination includes several tests to assess spinal mobility, stiffness, pain, and nerve function. The practitioner analyzes the flexion, extension, and rotation movements of the lumbar spine to detect possible mobility limitations or specific pain. Neurological tests are also performed to assess the presence of radicular symptoms, such as numbness or tingling in the lower extremities. These tests include assessments of skin sensation, muscle strength, and deep tendon reflexes.
At the same time, the healthcare professional examines the patient’s posture and seeks to detect imbalances or bodily compensations that may be related to lumbar spondylosis. Areas of muscle tension and painful trigger points are also palpated to determine potentially affected structures.
Clinical Criteria for Diagnosis
Based on clinical evaluation, several criteria can be used to confirm the diagnosis of lumbar spondylosis. These include:
- Chronic persistent or recurring low back pain , often aggravated by prolonged standing or flexion-extension movements.
- Morning stiffness that usually goes away after some time of movement.
- Decreased lumbar flexibility , measured by a reduction in the range of motion of the spine.
- Presence of neurological symptoms , such as radiating pain, numbness or weakness in the legs, indicating possible nerve compression.
However, clinical diagnosis alone may not be sufficient to differentiate lumbar spondylosis from other spinal pathologies, such as disc herniations, spinal stenosis or spondylolisthesis. In this context, imaging examinations become essential to confirm the presence of degenerative changes and to assess the extent of the lesions.
Imaging: X-rays, MRI and CT scans
Imaging tests are commonly used to establish an accurate diagnosis of lumbar spondylosis and to assess degenerative changes in spinal structures. The most commonly used imaging techniques include X-rays, magnetic resonance imaging (MRI), and computed tomography (CT) scans.
- X-rays : Plain X-rays are often the first step in visualizing the spine and identifying signs of spondylosis. They can detect bony changes such as osteophyte formation, decreased intervertebral space, and the presence of ligamentous calcifications. X-rays are useful in assessing the curvature of the spine and in detecting postural imbalances.
- Magnetic Resonance Imaging (MRI) : MRI is particularly useful for evaluating the soft tissues of the spine, including the intervertebral discs, ligaments, and nerves. It can detect disc degeneration, herniated discs, facet joint inflammation, and nerve compression. MRI is often indicated in patients with neurological symptoms, such as radicular pain or muscle weakness, to determine the severity of nerve damage.
- CT scan (computed tomography) : CT scan is a more detailed imaging technique than X-rays, allowing for precise visualization of bony structures and detection of small fractures or facet joint abnormalities. It is often used to evaluate spinal stenosis or complex bony changes associated with spondylosis.
Importance of Differential Diagnosis
When evaluating a patient with symptoms of lumbar spondylosis, it is crucial to perform a differential diagnosis to exclude other pathologies with similar manifestations. Conditions such as herniated discs, vertebral fractures, spinal infections, or tumors should be excluded by a combination of clinical examination and imaging studies.
The healthcare professional should also take into account the patient’s medical history, including past trauma, surgical procedures, and pre-existing diseases. This helps to better understand the origin of the symptoms and adapt the management accordingly.
Using a combination of clinical and imaging criteria, the diagnosis of lumbar spondylosis can be made accurately and comprehensively, allowing an appropriate treatment plan to be developed to reduce pain and improve spinal function.
Potential Complications
Spinal Stenosis and Nerve Compression
One of the most common complications of lumbar spondylosis is spinal stenosis, which occurs when the spinal canal narrows due to degenerative changes. This narrowing of the canal can be caused by bony growths (osteophytes), thickened ligaments, or associated herniated discs. Spinal stenosis causes compression of the nerve roots or spinal cord, causing pain that radiates down the legs, often described as sciatica. Patients with lumbar stenosis may also experience numbness, tingling, or muscle weakness, especially after walking a distance or standing for a prolonged period. This complication can seriously affect patients’ mobility and quality of life.
In the most severe cases, nerve compression can lead to loss of bladder or bowel control, a symptom called cauda equina syndrome. This condition requires emergency medical intervention to prevent permanent nerve damage and paralysis.
Advanced Lumbar Osteoarthritis
Progression of lumbar spondylosis can also lead to advanced lumbar osteoarthritis, characterized by significant degradation of the zygapophyseal (facet) joints and chronic inflammation. Advanced facet joint osteoarthritis not only causes significant stiffness and pain in the lower back, but it can also lead to loss of mobility and flexibility. This loss of mobility increases patients’ dependence on other spinal segments and neighboring joints, promoting postural imbalances and additional tension in the paravertebral muscles.
When lumbar osteoarthritis is advanced, conservative treatments may be ineffective in relieving pain, sometimes requiring surgery to stabilize the spine or release compressed nerves.
Vertebral Instability and Spondylolisthesis
Due to degenerative changes in the intervertebral discs and facet joints, spinal instability can occur. This instability manifests as the vertebrae slipping relative to each other, a phenomenon known as degenerative spondylolisthesis. This condition can exacerbate low back pain and cause compression of nerve roots, leading to radiating pain and neurological symptoms similar to those seen in spinal stenosis.
Spinal instability may be aggravated by repetitive movements, strenuous physical activities, or weakness of the trunk stabilizing muscles. In patients with severe instability, surgery may be recommended to fuse the affected spinal segments and stabilize the spine.
Postural Imbalances and Muscular Disorders
Chronic pain associated with lumbar spondylosis and limitations in spinal mobility often lead to postural changes and muscle imbalances. Patients may adopt compensatory postures to avoid pain, such as anterior trunk flexion or excessive arching of the lumbar spine. These postural adaptations create additional muscle imbalances and tension, promoting the development of myofascial trigger points in the paraspinal muscles, glutes, and hamstrings.
These postural imbalances can also affect other areas of the body, particularly the hips, knees and feet. For example, impaired lumbar mobility can lead to an abnormal gait, increasing stress on the joints of the lower limbs and promoting the onset of secondary joint and muscle pain.
Decreased Quality of Life
Complications of lumbar spondylosis are not limited to physical pain and functional limitations. Chronic symptoms of the disease, such as stiffness, pain, neurological disorders, and postural imbalances, can lead to a significant decrease in patients’ quality of life. Functional limitations, combined with the fear of worsening symptoms, can restrict patients’ physical activities and hobbies, making them more sedentary and less active. This inactivity can in turn worsen overall physical condition, lead to weight gain, and increase pain.
In addition, patients with lumbar spondylosis often experience sleep disturbances due to nighttime pain, which leads to chronic fatigue and low energy. This fatigue not only affects patients’ ability to perform their daily tasks, but also their mental and emotional state.
Psychological and Emotional Impact
Chronic pain and functional limitations associated with lumbar spondylosis can impact patients’ mental health. Frustration at not being able to perform tasks or having to limit daily activities can lead to anxiety, depression, and decreased self-esteem. The psychological impact of chronic pain and loss of mobility should not be underestimated, as it can further aggravate pain perception and lead to a vicious cycle of inactivity and deconditioning.
Patients with lumbar spondylosis may also experience a sense of dependency, due to their inability to perform certain tasks without assistance. This feeling of loss of autonomy can impair their psychological and emotional well-being, increasing the perception of the limitations imposed by their condition.
Osteopathic Approach to Lumbar Spondylosis
Myofascial Release Techniques
One of the fundamental approaches of osteopathy to treat lumbar spondylosis is the use of myofascial release techniques. These techniques aim to release tension in the soft tissues surrounding the spine, including the paraspinal muscles, gluteal muscles and fascia. Myofascial tension can be exacerbated by chronic pain and movement limitations, leading to painful trigger points and reduced flexibility.
Myofascial release techniques used by the osteopath restore tissue mobility and reduce pain by applying gentle, prolonged pressure to tense areas. The goal is to improve local blood circulation, release adhesions, and promote better muscle and fascia function. This approach also helps reduce postural imbalances created by body compensations, by improving force balance and movement symmetry.
Joint Mobilization and Mobility Techniques
In addition to myofascial techniques, the osteopath uses joint mobilization techniques to restore mobility to the vertebral segments affected by lumbar spondylosis. These techniques include gentle, progressive movements that aim to improve the flexibility of the zygapophyseal joints (facet joints) and reduce stiffness caused by osteoarthritis. Mobilization techniques are adapted to the patient’s specific needs and the state of the degenerative structures, in order to avoid excessive stress or additional pain.
The osteopath may also use gentle traction techniques to stretch the spine and reduce pressure on the intervertebral discs. Spinal traction helps reduce nerve compressions and relieve radicular symptoms, such as radiating pain and numbness in the lower limbs.
Postural Correction and Muscle Rebalancing
A key aspect of the osteopathic approach in the management of lumbar spondylosis is to correct postural imbalances and strengthen the stabilizing muscles of the trunk. Loss of spinal flexibility and chronic pain can lead to postural alterations, such as lumbar hyperlordosis or anterior pelvic tilt. These postural adaptations increase mechanical stress on the lumbar structures and aggravate pain.
The osteopath assesses postural imbalances and suggests specific exercises to strengthen the stabilizing muscles, such as the abdominal muscles, deep paravertebral muscles and pelvic floor muscles. Muscle rebalancing helps restore spinal alignment and reduce mechanical stress on degenerative segments. At the same time, stretching is recommended to improve the flexibility of tight muscles, particularly the hamstrings and gluteal muscles.
Trigger Point Release Techniques
Myofascial trigger points are hyperalgesic areas located in tight muscles that cause local and referred pain. Patients with lumbar spondylosis often develop trigger points in the paravertebral muscles, gluteal muscles, and thigh muscles. These trigger points worsen low back pain and movement limitations, making management of the condition difficult.
The osteopath uses specific techniques to release these trigger points, such as ischemic pressure or muscle release techniques. Ischemic pressure involves applying progressive pressure to the trigger point until the pain decreases and the muscle relaxes. These techniques help reduce muscle tension and improve flexibility, thus contributing to better management of lower back pain.
Fascia and Ligament Mobilization Techniques
Ligaments and fascia play a vital role in the stability and mobility of the spine. Lumbar spondylosis can cause tension and adhesions in these structures, limiting movement and increasing pain. Osteopathy offers specific techniques for mobilizing fascia and ligaments, aimed at restoring their flexibility and function.
Fascial mobilization techniques include gentle traction movements and deep fascial stretching. These techniques help reduce adhesions and restore fluid circulation in the tissues, thereby promoting better regeneration of degenerative structures. Ligament mobilization techniques aim to improve the flexibility of calcified ligaments and reduce stiffness in the lumbar segments.
Patient Support and Education
Finally, a fundamental aspect of the osteopathic approach is to support the patient in managing their pathology and provide them with personalized advice on their lifestyle and physical activities. The osteopath helps the patient understand the origin of their pain and offers them specific exercises to strengthen their spine and improve their posture. They also give advice on ergonomics at work, good practices for lifting loads, and the importance of regular physical activity.
Osteopathic support also includes the management of psychological and emotional aspects related to chronic pain. The osteopath encourages the patient to stay active, maintain a positive attitude and practice relaxation techniques to reduce stress and anxiety.
Prevention and Healthy Living
Strategies to Prevent Worsening of Lumbar Spondylosis
Prevention plays a crucial role in the management of lumbar spondylosis and in mitigating the risks of disease progression. The main goal is to reduce stress on the spine and maintain good mobility. An effective preventive approach involves adopting specific measures and lifestyle changes to limit wear and tear on spinal structures and strengthen supporting muscles.
One of the most important prevention strategies is to maintain regular and appropriate physical activity. Low-impact exercises, such as walking, swimming or cycling, help to preserve flexibility and strengthen muscles without putting excessive stress on the spine. Regular exercise also contributes to weight management, a crucial factor in avoiding overloading of the intervertebral discs and zygapophyseal joints.
Importance of Ergonomics and Posture
Adopting good posture in everyday life is essential to prevent the worsening of lumbar spondylosis. Proper posture helps to distribute the loads on the spinal structures in a balanced manner, thus reducing stress on the discs and facet joints. At work, it is crucial to ensure the ergonomics of the work environment, including adjusting the height of the chair and computer screen, and using a lumbar support if necessary. Prolonged positions should be avoided, and it is recommended to take regular breaks to stand up, stretch and release muscle tension.
When performing daily activities, it is essential to adopt proper techniques for lifting heavy objects. It is better to bend your knees and use leg strength rather than overstrain your back. Similarly, it is recommended to avoid sudden twisting or bending movements of the spine.
Strengthening and Stretching Exercises
A specific exercise program is essential to strengthen the stabilizing muscles of the lumbar spine and maintain good flexibility. Strengthening exercises targeting the abdominal, paraspinal and gluteal muscles help create solid muscular support around the spine, thus reducing mechanical constraints. Planking, for example, is an effective exercise to strengthen the deep core muscles and improve lumbar stability.
In addition, stretching exercises help maintain muscle flexibility and reduce joint stiffness. Stretching the hamstrings, glutes, and paraspinal muscles is particularly beneficial for preventing excessive muscle tension and postural imbalances.
Weight Management and Nutrition
Being overweight is a major risk factor for the development and worsening of lumbar spondylosis. Excess weight puts additional pressure on the intervertebral discs and joints, increasing the risk of degeneration. Therefore, it is essential to maintain a healthy body weight through a balanced diet and regular physical activity.
A diet rich in essential nutrients, such as vitamins D and C, calcium, and omega-3 fatty acids, is beneficial for bone and joint health. Antioxidants found in fruits and vegetables can also help reduce inflammation and protect spinal tissues from oxidative damage.
Prevention of Repeated Microtraumas
Repetitive microtrauma resulting from professional or sports activities can accelerate the degeneration process of the spinal structures. To prevent these microtraumas, it is important to take precautionary measures during risky activities. Professionals who perform jobs that require intense physical effort, such as handlers, construction workers or athletes, must be trained in good lifting techniques and safe postures. In addition, it is recommended to vary tasks and avoid repetitive movements that excessively stress the same segments of the spine.
Stress Management and Relaxation
Chronic stress can worsen the symptoms of lumbar spondylosis by increasing muscle tension and heightening the perception of pain. Stress management is therefore a key aspect of preventing and managing this condition. Relaxation techniques, such as deep breathing, meditation or yoga practice, help reduce stress and release muscle tension. These techniques also help improve the general well-being of patients and reduce the emotional impact of chronic pain.
Regular Monitoring and Follow-up
Finally, it is important to have regular follow-up with a healthcare professional to monitor the progress of lumbar spondylosis and adjust prevention strategies according to the patient’s needs. The osteopath can regularly assess posture, mobility and muscle imbalances to detect any signs of progression of the pathology. Follow-up also helps to strengthen the patient’s motivation to adopt preventive measures and maintain appropriate physical activity.
By applying these preventive strategies and adopting a healthy lifestyle, it is possible to slow the progression of lumbar spondylosis and maintain a good quality of life. Prevention, combined with regular osteopathic care, constitutes an essential pillar in the overall management of this degenerative pathology.
Radiographic or Imaging Signs
Use of X-rays for Diagnosis
Radiographs remain one of the most commonly used tests to assess signs of lumbar spondylosis. They provide a simple and rapid visualization of bony structures, allowing the detection of characteristic changes such as decreased intervertebral space, the presence of osteophytes, and alterations of the facet joints. Standard radiography is particularly useful for identifying the alignment of the vertebrae and for assessing the overall curvature of the spine.
On lumbar spine X-ray, typical signs of spondylosis include loss of intervertebral disc height, signs of subchondral sclerosis (hardening of the bone beneath the cartilage), and irregular vertebral edges due to osteophyte formation. These bony growths, although often asymptomatic, may indicate a progressive adaptation of the spinal structures to increased mechanical stresses.
Magnetic Resonance Imaging (MRI): Visualization of Soft Tissues
MRI is the preferred imaging tool for evaluating soft tissues and intervertebral structures. Unlike X-rays, which focus primarily on bones, MRI can visualize intervertebral discs, nerves, ligaments, and muscles. It is particularly indicated in patients with radicular pain (sciatica) or neurological symptoms, to determine the severity of nerve damage and identify the underlying cause.
MRI scans reveal important details such as disc degeneration, herniated discs, and thickened ligamentum flavum (ligamentum flavum) that can contribute to spinal stenosis. Disc signal loss on MRI usually indicates dehydration and reduced elasticity, common features of lumbar spondylosis. In addition, MRI can identify nerve compression caused by osteophytes or spinal canal narrowing.
CT Scan (Computerized Tomography): Accurate Assessment of Bone Structures
CT scanning, or computed tomography, is an imaging technique that uses X-rays to produce detailed cross-sectional images of spinal structures. It is particularly useful for evaluating complex bony changes and facet joint abnormalities. CT scanning allows for precise visualization of osteophytes, stress fractures, ligamentous calcifications, and vertebral deformities.
In spinal stenosis, CT is often used in addition to MRI to assess spinal canal narrowing and to precisely localize sites of nerve compression. This technique is also indicated in patients with spinal instability or a history of spinal surgery, to assess the integrity of spinal implants or fusions.
Role of Dynamic Imaging
Standard X-rays and CT scans provide static information about spinal structures, but dynamic imaging studies may be necessary to assess spinal motion. Dynamic X-rays are taken in flexion and extension positions to detect signs of spinal instability, such as slipping of the vertebrae (spondylolisthesis) or excessive displacement during movement.
These dynamic examinations help determine whether surgical intervention is necessary to stabilize the spine, particularly in patients with advanced degenerative instability or persistent mechanical pain.
Identification of Anatomical Changes
Different imaging techniques can identify a variety of anatomic changes associated with lumbar spondylosis. Typical radiographic findings include:
- Osteophytes : Bony growths formed along the edges of the vertebrae, which are signs of chronic degeneration and bony compensation.
- Narrowing of the Intervertebral Space : A sign of advanced disc degeneration, indicating a loss of disc height.
- Subchondral Sclerosis : Thickening of the bone beneath the cartilage, a common feature of facet joint osteoarthritis.
- Herniated Discs : The protrusion or extrusion of a portion of the intervertebral disc, visible primarily on MRI.
- Spinal Stenosis : Narrowing of the spinal canal seen on MRI or CT scan, caused by osteophytes, herniated discs, or thickening of the ligaments.
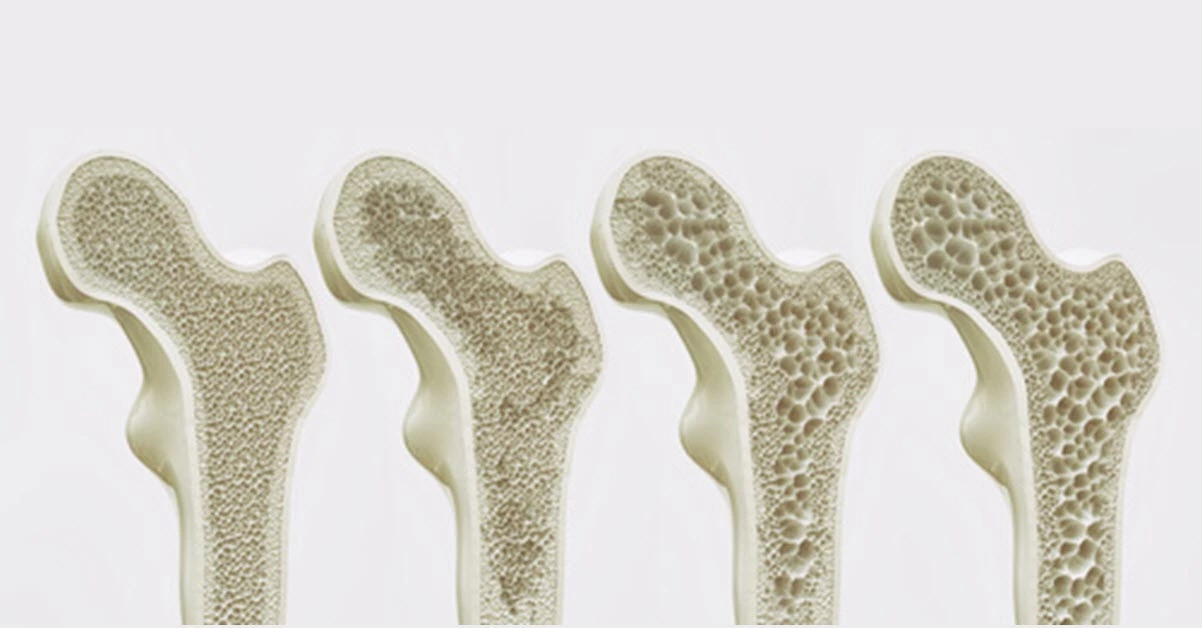
Kellgren-Lawrence (KL) grading system
The Kellgren-Lawrence (KL) grading system is a commonly used method to classify the severity of osteoarthritis, including spinal spondylosis. Developed by Dr. Kellgren and Dr. Lawrence, this system assesses the presence and progression of osteoarthritic changes through radiographic imaging. The grading system has five grades (0 to 4), based on the presence of osteophytes, joint space narrowing, sclerosis, and other degenerative changes:
- Grade 0: No radiographic features of osteoarthritis are visible.
- Grade 1: Doubtful narrowing of joint space and possible presence of minute osteophytes.
- Grade 2: Definite osteophytes and possible narrowing of the joint space.
- Grade 3: Multiple moderate osteophytes, definite narrowing of the joint space, some sclerosis, and possible deformity of bone contour.
- Grade 4: Large osteophytes, marked narrowing of joint space, severe sclerosis, and definite deformity of bone contour.
In lumbar spondylosis, the Kellgren-Lawrence system helps assess the progression of degenerative changes in the spine, such as osteophyte formation, disc space narrowing, and bony sclerosis. This grading aids clinicians in diagnosing the severity of the condition and planning treatment strategies. It is widely recognized and utilized in clinical and research settings for various forms of osteoarthritis and spinal degeneration.
4o
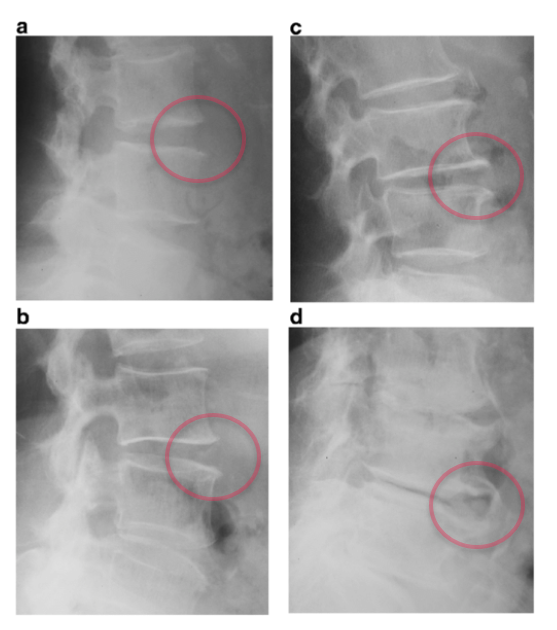
Image A represents KL Grade 1, indicating the presence of slight osteophytes with minimal or no narrowing of the intervertebral disc space. Osteophytes, or small bony projections, begin to form along the edges of the vertebral bodies.
Image B corresponds to KL Grade 2, showing the development of more defined osteophytes without significant disc space narrowing, which suggests a moderate degree of spondylosis.
Image C depicts KL Grade 3, characterized by notable narrowing of the intervertebral disc space along with the presence of osteophytes. This indicates advancing degeneration, affecting both the bony and disc structures.
Image D illustrates KL Grade 4, which is the most severe grade. It features substantial disc space narrowing, large osteophytes, and bone sclerosis, indicating extensive degeneration in the lumbar spine.
The KL grading system is commonly used to assess and quantify the severity of degenerative changes in the lumbar spine, helping to guide clinical decisions regarding patient management and treatment options.
Limitations of Imaging Techniques
Although imaging is essential for the diagnosis of lumbar spondylosis, it is important to note that visible degenerative changes do not always correlate with the severity of symptoms. For example, many patients have osteophytes or disc space narrowing without significant pain. Conversely, patients with chronic low back pain may have only minimal signs of spondylosis on imaging studies.
Thus, imaging should be used as a complement to clinical assessment, and not as an isolated diagnostic method. The healthcare professional should interpret imaging results in the context of the patient’s symptoms and medical history, in order to provide personalized and appropriate management.
By combining different imaging modalities, it is possible to obtain a complete view of the structures affected by lumbar spondylosis and to develop an effective treatment plan. Imaging techniques not only allow to confirm the diagnosis, but also to monitor the evolution of the pathology and to adjust interventions according to the patient’s needs.
Complications and Prognosis
Complications without Appropriate Management
The progression of lumbar spondylosis without adequate treatment can lead to several significant complications, which affect not only the spine, but also the overall quality of life of patients. One of the most common complications is the progressive worsening of stiffness and lower back pain, leading to a loss of mobility and flexibility of the spine. The decrease in intervertebral space and the formation of osteophytes can limit the normal movements of the spine, causing difficulty in bending, sitting, or performing simple tasks of daily living.
Another major complication is the development of chronic nerve compressions due to the narrowness of the spinal canal (spinal stenosis). These compressions cause radiating pain in the legs (sciatica), as well as neurological symptoms such as numbness, tingling or muscle weakness. Prolonged compression of the nerve roots can also lead to more severe sensory or motor dysfunctions, compromising the autonomy and functional capacities of patients.
In severe cases, untreated progression of lumbar spondylosis can also lead to cauda equina syndrome, a medical emergency characterized by loss of control of urinary and bowel functions. This condition requires immediate surgery to prevent permanent nerve damage.
Long-Term Consequences on Musculoskeletal Health
Beyond pain and movement limitations, complications of lumbar spondylosis affect the entire musculoskeletal system. Patients often develop postural imbalances and body compensations, such as trunk tilt or excessive arching of the lumbar spine. These postural changes increase stress on the paraspinal muscles, gluteal muscles, and lower extremity muscles, which can cause secondary pain in the hips, knees, and feet.
Muscle imbalances can also lead to weakness in the core stabilizing muscles, increasing the risk of injuries and falls. Patients with lumbar spondylosis often have an altered gait due to stiffness and pain, compromising their balance and coordination.
Psychological and Emotional Impact
Chronic pain and functional limitations associated with lumbar spondylosis have a significant impact on patients’ mental and emotional health. The inability to perform daily tasks or participate in social and recreational activities can lead to feelings of frustration, depression, and social isolation. Persistent pain and movement limitations can also cause anxiety related to fear of worsening symptoms or loss of independence.
The psychological repercussions of lumbar spondylosis often require comprehensive management, including psychological support or relaxation techniques to help patients manage their pain and maintain a positive attitude.
Prognosis and Evolution of Lumbar Spondylosis
The prognosis of lumbar spondylosis depends on several factors, such as the severity of degenerative changes, the patient’s age, level of physical activity, and early management. In many cases, the progression of spondylosis is slow and symptoms can be well managed with conservative interventions such as osteopathy, physiotherapy, and an appropriate lifestyle.
However, for patients with advanced forms of spondylosis with severe nerve compression or pain resistant to conservative treatments, surgery may be necessary. Surgical procedures, such as laminectomy (removal of part of the bone to free the nerves) or spinal fusion (stabilization of unstable segments), can significantly improve patients’ symptoms and quality of life.
Although surgery can provide relief of symptoms, it also carries risks and potential complications, such as infections, postoperative pain, or residual stiffness. Therefore, the decision to undergo surgery should be made after a thorough evaluation and discussion with the patient about the benefits and risks.
Prevention of Complications and Improvement of Prognosis
To avoid complications of lumbar spondylosis, it is essential to adopt a preventive approach by maintaining regular physical activity, adopting proper posture and following the recommendations of a healthcare professional. Muscle strengthening and flexibility exercises help reduce stress on the spine and maintain good mobility. Patients should also monitor their weight and avoid repetitive movements or risky activities to prevent wear and tear on the spinal structures.
Regular osteopathic care can also help prevent complications by reducing myofascial tension, improving postural balance and maintaining joint mobility. Osteopathic support, in collaboration with other health professionals, provides a comprehensive and individualized approach for each patient.
In conclusion, although lumbar spondylosis is a common degenerative pathology, its complications can be avoided or limited through early and multidisciplinary management. By understanding the mechanisms of the disease and adopting a proactive approach, it is possible to improve the prognosis and preserve the quality of life of patients.
Clinical Cases or Testimonials
Presentation of Real Cases to Illustrate Successful Osteopathic Treatments
The osteopathic approach to the management of lumbar spondylosis is distinguished by its comprehensive and personalized nature. The following clinical cases illustrate the effectiveness of this approach in the management of chronic low back pain and functional limitations. Each case highlights the specific strategies used by the osteopath to address the unique needs of the patients, and demonstrates the importance of individualized management.
Clinical Case 1: Pain Reduction and Mobility Restoration
Mrs. X, 65 years old, consulted for chronic lower back pain that had persisted for several years. This pain was aggravated by flexion movements and prolonged positions. During the initial assessment, the osteopath noted marked stiffness of the lumbar spine, as well as significant muscle tension in the paravertebral muscles and gluteal muscles. The patient also had slight spinal instability due to a reduction in the intervertebral space.
The osteopath first used myofascial release techniques to release muscle tension and improve local circulation. Then, gentle facet joint mobilization techniques were applied to restore spinal flexibility and reduce mechanical pain. Specific exercises to strengthen the stabilizing muscles of the trunk were proposed to the patient, in order to support the spine and prevent recurrences.
After several sessions, Mrs. X noticed a significant reduction in her pain and an improvement in her mobility. She also reported better quality of sleep and an increase in her energy level. Thanks to osteopathic support, she was able to resume moderate physical activities, such as walking, without experiencing significant pain.
Clinical Case 2: Management of Neurological Symptoms and Improvement of Posture
Mr. Y, 58 years old, presented to the clinic with low back pain radiating to the legs, associated with numbness and tingling. Physical examination and imaging studies revealed spinal stenosis due to osteophyte formation and advanced disc degeneration. The patient also had excessive arching of the lumbar spine, aggravating nerve compressions.
The osteopath implemented a treatment strategy focused on reducing compressions and improving posture. Spinal traction techniques were applied to stretch the spine and release compressed nerve roots. Gentle joint mobilizations were also used to release the vertebral segments and improve the flexibility of the facet joints. In parallel, the osteopath worked on postural imbalances by proposing corrective exercises to correct excessive lumbar arching.
After a series of sessions, Mr. Y reported a decrease in radiating pain and improved sensation in his legs. His posture also improved, and he was able to resume some activities that he had had to stop due to pain, such as gardening. This case illustrates the importance of comprehensive care that includes postural correction and spinal mobilization.
Patient Testimonials
Testimonials from patients with lumbar spondylosis often show the positive impact of osteopathy on their physical and emotional well-being. Mrs. Z, 72, describes her experience: “I had constant lower back pain that prevented me from walking for more than a few minutes without having to stop. After trying several treatments, it was osteopathy that really brought me relief. My osteopath worked on my tight muscles and restored flexibility to my spine. Today, I can walk for an hour without feeling pain, and I feel more confident and active.”
Mr. W, 63, also talks about his journey: “I felt as stiff as a board, and every movement caused me pain. The osteopath explained the origin of my pain and showed me how to improve my posture on a daily basis. Thanks to the sessions and exercises he recommended, I have regained better mobility and I no longer need to take painkillers every day.”
Recent Research on Lumbar Spondylosis and Osteopathy
Research into the effectiveness of osteopathic treatments for lumbar spondylosis shows promising results, particularly in reducing chronic pain and improving function. Here is a summary of relevant studies in this area:
Effectiveness of Myofascial Release Techniques
A study by Arguisuelas et al. evaluated the effect of myofascial release (MFR) on patients with chronic low back pain. In this randomized, controlled study, patients received four 40-minute MFR sessions targeting the paravertebral muscles, thoracolumbar fascia, and psoas muscle. Results showed a significant decrease in pain as measured by the SF-MPQ and the Roland-Morris questionnaire, as well as a reduction in fear-avoidance beliefs. Compared with the placebo group, participants treated with MFR showed improved range of motion and decreased functional disability after 12 weeks of follow-up【40†source】.
Osteopathic Manipulations and Pain Reduction
Another study published in the Journal of the American Medical Association explored the effect of osteopathic manipulation on patients with subacute and chronic low back pain. The results revealed that multimodal osteopathic treatments, including spinal manipulation techniques and myofascial releases, resulted in a significant reduction in activity limitations compared to a placebo group. The study highlighted an average decrease of 4.7 points on the Quebec Pain Disability Index (QBPDI) scale, demonstrating the clinical effectiveness of these techniques in reducing functional limitations【39†source】.
Comparison with Other Therapeutic Approaches
Research shows that osteopathic myofascial release and gentle mobilisation techniques are often more effective at improving flexibility and reducing pain than more targeted soft tissue interventions, such as deep tissue massage or physiotherapy alone. A systematic review demonstrated that osteopathy combined with a core strengthening exercise programme could reduce pain and improve mobility more effectively than isolated exercises, highlighting the importance of an integrated approach【40†source】.
These results support the use of osteopathic treatments for lumbar spondylosis and show that myofascial release and manipulation techniques can play a crucial role in the management of this degenerative pathology. To strengthen these conclusions, it is essential to continue to conduct rigorous clinical studies to clarify the effects and mechanisms of different osteopathic interventions.
Conclusion
Lumbar spondylosis is a common degenerative pathology that affects a large part of the aging population and has a significant impact on the quality of life of those affected. Although the degenerative changes associated with this condition are inevitable with age, it is possible to prevent their worsening and to effectively manage the symptoms through appropriate management.
Osteopathy offers a holistic and non-invasive approach to treating lower back pain and movement limitations caused by lumbar spondylosis. Using gentle techniques of myofascial release, joint mobilization and postural correction, osteopathy helps restore flexibility to the spinal segments, reduce muscle tension and improve body balance. In addition, osteopathic support includes patient education on ergonomic practices, healthy lifestyle, and specific exercises to strengthen the spine and prevent recurrence.
Clinical studies and real cases demonstrate the effectiveness of osteopathy in reducing chronic lower back pain, improving mobility and preventing long-term complications. The complementarity of osteopathic treatments with other therapeutic approaches, such as physiotherapy, acupuncture and physical exercises, reinforces the effectiveness of interventions and allows for comprehensive management of lumbar spondylosis.
References
- Frymoyer JW. Back pain and sciatica. N Engl J Med. 1988;318:291–300. [PubMed] [Google Scholar]
- van Geen J, Edelaar M, Janssen M, et al. The long-term effect of multidisciplinary back training: a systematic review. Spine. 2007;32(2):249–55. doi: 10.1097/01.brs.0000251745.00674.08. [PubMed] [CrossRef] [Google Scholar]
- Andersson GB. Epidemiological features of chronic low pain. Lancet. 1999;354:581–5. doi: 10.1016/S0140-6736(99)01312-4. [PubMed] [CrossRef] [Google Scholar]
- Dillane J, Fry J, Kalton G. Acute back syndrome—a study from general practice. Br Med J. 1966;2:82–4. doi: 10.1136/bmj.2.5505.82. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Andersson HI, Ejlertsson G, Leden I, et al. Chronic pain in a geographically defined general population: studies of differences in age, gender, social class and pain localization. Clin J Pain. 1993;9:174–82. [PubMed] [Google Scholar]
- Andersson GB. The epidemiology of spinal disorders. In: Frymoyer JW, editor. The adult spine: principles and practice. 2. Philadelphia, PA: Lippincott-Raven; 1997. [Google Scholar]
- van Tulder MW, Koes BW, Bouter LM. A cost-of-illness study of back pain in The Netherlands. Pain. 1995;62:233–40. doi: 10.1016/0304-3959(94)00272-G. [PubMed] [CrossRef] [Google Scholar]
- Deyo R, Cherkin D, Conrad D. Cost, controversy, crisis: low back pain and the health of the public. Annu Rev Publ Health. 1991;12:141–56. doi: 10.1146/annurev.pu.12.050191.001041. [PubMed] [CrossRef] [Google Scholar]
- Bogduk N. The innervation of the lumbar spine. Spine. 1983;8:286–93. doi: 10.1097/00007632-198304000-00009. [PubMed] [CrossRef] [Google Scholar]
- Williams ME, Hadler NM. The illness as the focus of geriatric medicine. N Engl J Med. 1983;308:1357–60. [PubMed] [Google Scholar]
- Boden SD, Davis DO, Diniesel SW, Tsourmas N, Feffer HL, et al. A study of computer-assisted tomography. The incidence of positive CAT scans in an asymptomatic group of patients. Spine. 1984;9:549. doi: 10.1097/00007632-198409000-00003. [PubMed] [CrossRef] [Google Scholar]
- Pye SR, Reid DM, Lunt M, et al. Lumbar disc degeneration: association between osteophytes, end-plate sclerosis and disc space narrowing. Ann Rheum Dis. 2007;66(3):330–3. doi: 10.1136/ard.2006.052522. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Osteophytes: relevance and biology. Osteoarthritis cartilage. 2007;15(3):237–44. doi: 10.1016/j.joca.2006.11.006. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rothschild B. Lumbar spondylosis. In: Emedicine publication. 2008. Available via WebMD. http://emedicine.medscape.com/article/249036-overview.
- Fardon DF, Milette PC. Nomenclature and classification of lumbar disc pathology. Spine. 2001;26(5):E93–113. doi: 10.1097/00007632-200103010-00006. [PubMed] [CrossRef] [Google Scholar]
- Schneck CD. The anatomy of lumbar spondylosis. Clin Orthop Relat Res. 1985;193:20–36. [PubMed] [Google Scholar]
- Gibson JNA, Waddell G. Surgery for degenerative lumbar spondylosis. Spine. 2005;20:2312–20. doi: 10.1097/01.brs.0000182315.88558.9c. [PubMed] [CrossRef] [Google Scholar]
- Symmons DPM, van Hemert AM, Vandenbrouke JP, et al. A longitudinal study of back pain and radiological changes in the lumbar spines of middle aged women: radiographic findings. Ann Rheum Dis. 1991;50:162–6. doi: 10.1136/ard.50.3.162. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- O’Neill TW, McCloskey EV, Kanis JA, et al. The distribution, determinants, and clinical correlates of vertebral osteophytosis: a population based survey. J Rheumatol. 1999;26:842–8. [PubMed] [Google Scholar]
- Jensen MC, Brant-Zawadzki MN, Obuchowski N, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331(2):69–73. doi: 10.1056/NEJM199407143310201. [PubMed] [CrossRef] [Google Scholar]
- Frymoyer JW, Newberg A, Pope MH, et al. Spine radiographs in patients with low-back pain. An epidemiological study in men. J Bone Joint Surg Am. 1984;66(7):1048–55. [PubMed] [Google Scholar]
- Lawrence JS. Disc degeneration. Its frequency and relationship to symptoms. Ann Rheum Dis. 1969;28:121–38. doi: 10.1136/ard.28.2.121. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Kirkaldy-Willis W, Bernard T. Managing low back pain. New York: Churchill livingstone; 1983. [Google Scholar]
- Boswell MV, Trescot AM, Datta S, et al. Interventional techniques: evidence-based practice guidelines in the management of chronic spinal pain. Pain Physician. 2007;10(1):7–111. [PubMed] [Google Scholar]
- Kirkaldy-Willis WH, Wedge JH, Yong-Hing K, et al. Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine. 1978;3:319–28. doi: 10.1097/00007632-197812000-00004. [PubMed] [CrossRef] [Google Scholar]
- Menkes CJ, Lane NE. Are osteophytes good or bad? Osteoarthritis Cartilage. 2004;12(Suppl A):S53–4. doi: 10.1016/j.joca.2003.09.003. [PubMed] [CrossRef] [Google Scholar]
- Peng B, Hou S, Shi Q, et al. Experimental study on mechanism of vertebral osteophyte formation. Chin J Traumatol. 2000;3(4):202–5. [PubMed] [Google Scholar]
- Blom AB, van Lent PL, Holfhuysen AE, et al. Synovial lining macrophages mediate osteophyte formation during experimental osteoarthritis. Osteoarthritis Cartilage. 2004;12(8):627–35. doi: 10.1016/j.joca.2004.03.003. [PubMed] [CrossRef] [Google Scholar]