Introduction
Overview of Cervical Stenosis
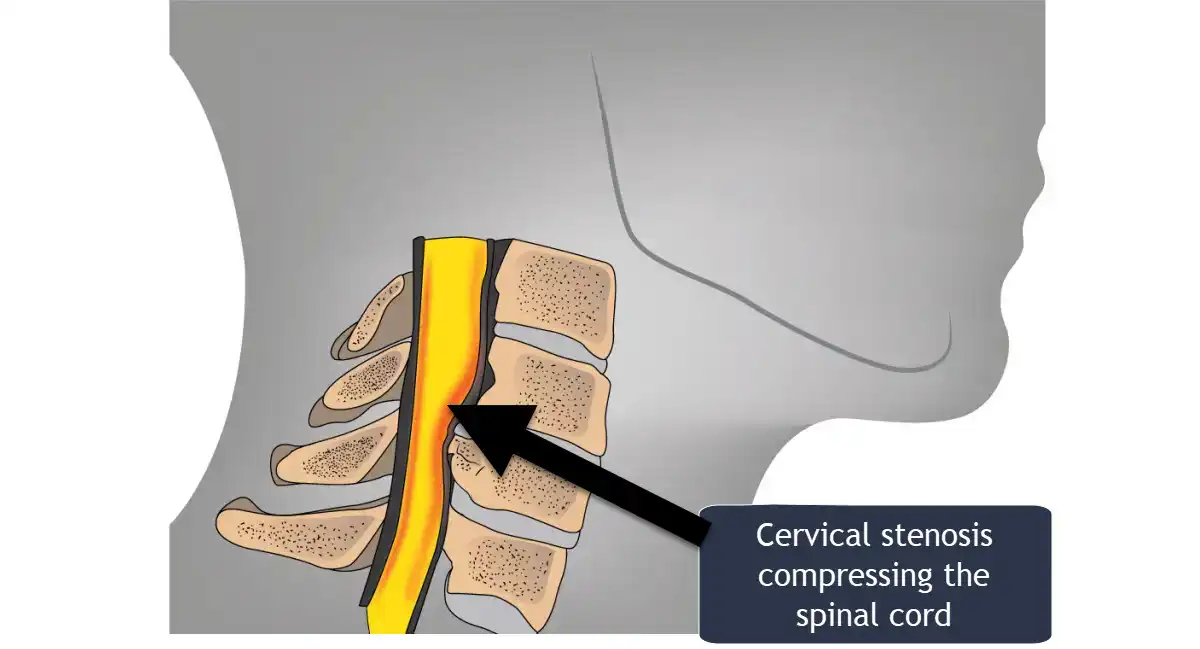
Cervical stenosis is a medical condition defined by the narrowing of the spinal canal in the cervical (neck) region of the spine. This narrowing creates pressure on the spinal cord and surrounding nerves, potentially leading to a variety of symptoms ranging from mild discomfort to debilitating neurological impairments. It is a progressive condition that typically worsens with age, though it can also arise due to congenital factors, trauma, or inflammatory conditions.
The cervical spine is composed of seven vertebrae (C1–C7) that form a vital conduit for the spinal cord, connecting the brain to the rest of the body. Within this intricate structure, elements such as intervertebral discs, ligaments, and facet joints play a role in maintaining stability, mobility, and protection for the spinal cord and nerves. In cervical stenosis, changes such as disc degeneration, ligament thickening, or bone spur formation reduce the space within the spinal canal, compressing these delicate neural structures.
The condition is particularly concerning because of its potential to disrupt the intricate communication pathways between the brain and various parts of the body. This disruption can manifest as pain, numbness, weakness, or coordination difficulties, depending on the severity and location of the compression. In some cases, advanced cervical stenosis may lead to more serious complications, such as myelopathy, characterized by impaired motor function, or radiculopathy, involving sharp nerve pain radiating to the arms or hands.
Impact on Quality of Life
The impact of cervical stenosis on an individual’s quality of life can be profound. Mild cases may only cause occasional neck discomfort or stiffness, but as the condition progresses, daily activities can become increasingly challenging. Persistent neck pain, tingling sensations in the arms or hands, and muscle weakness can interfere with tasks as simple as writing, cooking, or dressing. Over time, the loss of fine motor skills and balance may lead to difficulty walking or maintaining an active lifestyle.
In severe cases, cervical stenosis can lead to debilitating symptoms, including bladder or bowel dysfunction, which significantly diminishes independence and confidence. For those affected, the condition can foster feelings of frustration, anxiety, and isolation.
Early diagnosis and treatment are crucial to mitigating these impacts. With appropriate medical intervention—ranging from physical therapy and lifestyle modifications to surgical decompression—many individuals can find relief and regain function. Understanding cervical stenosis, its causes, and available treatments is the first step toward managing its effects and preserving quality of life.
Anatomy of the Cervical Spine
Understanding the anatomy of the cervical spine is essential for grasping the complexities of cervical stenosis. The cervical spine, located in the neck, is composed of seven vertebrae labeled C1 to C7. This intricate structure provides both support and mobility for the head while protecting the spinal cord and nerves that pass through it.
Vertebrae: C1 to C7
The cervical spine’s seven vertebrae form the uppermost portion of the spinal column, each contributing uniquely to its function.
- C1 (Atlas): The atlas is the first cervical vertebra and supports the weight of the skull. Its unique structure lacks a vertebral body and instead features a ring-like shape, enabling nodding motions such as tilting the head forward and backward.
- C2 (Axis): Positioned just below the atlas, the axis has a specialized projection called the dens, which acts as a pivot point for rotational movements of the head, such as turning side to side.
- C3 to C7: These vertebrae share a more uniform structure, including a vertebral body, which bears weight, and a vertebral arch that encases and protects the spinal cord. Their spinous processes and transverse processes serve as attachment points for muscles and ligaments, enabling stability and motion.
The interplay of these vertebrae allows for a remarkable range of motion while maintaining structural integrity.
Intervertebral Discs
Intervertebral discs are located between the vertebrae, acting as cushions to absorb shock and provide flexibility. Each disc has two primary components:
- Nucleus Pulposus: The gel-like core of the disc, which allows for flexibility and distributes pressure evenly across the disc during movement.
- Annulus Fibrosus: The tough outer layer composed of fibrous rings that encase the nucleus pulposus, providing strength and containment.
Over time, intervertebral discs may degenerate, lose hydration, or bulge, contributing to conditions like herniation, which can encroach on the spinal canal and exacerbate cervical stenosis.
Spinal Canal and Nerves
The spinal canal is a hollow, protective passage within the vertebrae that houses the spinal cord and cerebrospinal fluid. The spinal cord, a critical component of the central nervous system, carries nerve signals between the brain and the body. At each vertebral level, nerve roots branch off from the spinal cord, exiting through openings called foramina to innervate specific regions of the body.
In cervical stenosis, the narrowing of the spinal canal or foramina can compress the spinal cord or nerve roots. This compression disrupts the transmission of signals, leading to symptoms such as pain, numbness, or weakness in the neck, arms, or hands.
Ligaments and Facet Joints
The cervical spine’s stability and mobility are further supported by ligaments and facet joints:
- Ligaments: Various ligaments stabilize the cervical spine by connecting adjacent vertebrae:
- The anterior longitudinal ligament runs along the front of the vertebral bodies, preventing hyperextension.
- The posterior longitudinal ligament lines the back of the vertebral bodies, limiting hyperflexion.
- The ligamentum flavum, located within the spinal canal, maintains elasticity and stability but can thicken over time, contributing to spinal canal narrowing.
- Facet Joints: These small joints connect the vertebrae at the back of the spine, facilitating motion while maintaining alignment. Degenerative changes in these joints, such as osteoarthritis, can result in the formation of bone spurs (osteophytes), which may encroach on the spinal canal or nerve roots.
Causes of cervical stenosis
Cervical stenosis is primarily caused by conditions that lead to the narrowing of the spinal canal in the neck region. This narrowing can compress the spinal cord and nerves, leading to various symptoms. The main causes of cervical stenosis include:
Degenerative Changes
Degenerative changes represent one of the most common causes of cervical stenosis, primarily affecting adults as they age. Over time, the structures in the cervical spine—intervertebral discs, facet joints, and supporting ligaments—undergo wear and tear, resulting in alterations that can reduce the space within the spinal canal. These changes are often gradual, and symptoms may initially be mild, such as occasional neck stiffness or discomfort. However, as the degeneration progresses, the narrowing of the canal can intensify, leading to more pronounced neurological symptoms, including pain, numbness, or weakness in the arms and hands.
Among the key degenerative factors are osteoarthritis and degenerative disc disease. Osteoarthritis, or wear-and-tear arthritis, can cause the cartilage in the facet joints to deteriorate, leading to inflammation, pain, and the formation of bone spurs (osteophytes). These spurs may protrude into the spinal canal, further constricting the already limited space. In degenerative disc disease, the intervertebral discs lose hydration and elasticity. As the discs flatten or bulge outward, they can encroach on the spinal canal, exacerbating the compression of spinal nerves or the spinal cord itself.
Herniated Discs
A herniated disc, also referred to as a slipped or ruptured disc, occurs when the soft, gelatinous center of an intervertebral disc (the nucleus pulposus) pushes through a tear or crack in the tough outer layer (the annulus fibrosus). This protrusion can place direct pressure on nearby nerve roots or the spinal cord, precipitating pain that radiates from the neck down to the shoulders, arms, or even the fingers. In some instances, tingling, numbness, and muscle weakness can also be present.
Disc herniation can stem from various factors. Repeated stress on the spine, poor posture, and age-related disc degeneration are all contributing factors. Additionally, sudden trauma, such as a fall or an improper lifting technique, may cause the annulus fibrosus to rupture. Once the disc material extends beyond its normal boundaries, the risk of cervical stenosis increases significantly, as the added pressure reduces the spinal canal’s available space.
Thickened Ligaments
The ligamentum flavum and other stabilizing ligaments in the cervical spine are crucial for maintaining proper alignment and movement of the vertebrae. Over time, these ligaments may thicken or lose their natural elasticity, often due to chronic inflammation or repetitive stress. When a ligament becomes hypertrophied (thickened), it can bulge into the spinal canal, reducing the space through which the spinal cord and nerve roots pass.
This thickening is typically a gradual process. Early on, individuals might not experience significant symptoms, but as the ligament continues to thicken and encroach on the canal, signs of cervical stenosis—such as neck pain, stiffness, or radiating nerve pain—can emerge. Interventions may include physical therapy to reduce inflammation and improve neck mechanics, though advanced cases sometimes necessitate surgical decompression to remove or trim the thickened ligament.
Congenital Factors
In some cases, individuals are born with a congenitally narrow spinal canal, a condition known as congenital cervical stenosis. These people have a reduced margin for changes that might further narrow the canal, making them more susceptible to the effects of degenerative changes, herniated discs, or injuries. Even minor shifts, such as a small disc bulge, can cause disproportionately large impacts on the spinal cord or nerve roots.
Because congenital stenosis can exist without notable symptoms for many years, it often goes undiagnosed until adulthood, when degenerative processes begin to manifest. Early detection is crucial, as timely interventions—ranging from lifestyle modifications to surgical procedures—can help prevent severe complications, such as chronic pain, significant nerve compression, or myelopathy.
Spinal Injuries
Traumatic injuries to the cervical spine, including fractures, dislocations, or severe whiplash, can lead to immediate narrowing of the spinal canal. Sudden force may fracture vertebrae, displace bone fragments, or cause the discs to protrude into the canal. These acute changes raise the risk of spinal cord injury, particularly if there is significant compression of neural structures.
Beyond the initial trauma, spinal injuries can prompt secondary changes that exacerbate stenosis over time. Scar tissue may form as part of the healing process, while instability in the vertebral segments can accelerate degenerative changes. Thus, prompt and appropriate management of cervical spinal injuries is critical, often involving immobilization, surgical stabilization, or rehabilitation therapies to minimize long-term complications.
Tumors
Though less common than degenerative causes, benign or malignant tumors can also lead to cervical stenosis. These abnormal growths may develop within the spinal canal itself, originating from the meninges (the protective layers of the spinal cord), nerve sheaths, or vertebral bone. In other cases, tumors may metastasize to the spine from other parts of the body, expanding into the cervical region and compressing the spinal cord or nerve roots.
Symptoms arising from tumor-related stenosis can closely resemble those of degenerative stenosis—neck pain, radiating nerve pain, weakness, or numbness—making imaging and proper diagnosis paramount. Treatment depends on the tumor’s type and location. Surgical intervention to remove or reduce the size of the tumor may be combined with radiation therapy or chemotherapy to halt further growth and minimize neurological damage.
Inflammatory Conditions
Chronic inflammatory diseases such as ankylosing spondylitis or rheumatoid arthritis can alter the structure of the cervical spine, contributing to the development of stenosis. In rheumatoid arthritis, for instance, prolonged inflammation damages the facet joints and ligaments, potentially leading to vertebral misalignment or instability that compresses the spinal cord. Ankylosing spondylitis, on the other hand, promotes abnormal bone growth and fusion, which can significantly reduce spinal flexibility and impinge on the spinal canal.
These conditions often have systemic effects, meaning patients may experience symptoms beyond the neck, including fatigue or inflammation in other joints. Consequently, treatment approaches may involve medications to control inflammation, physical therapy to maintain range of motion, and targeted interventions for any neural compression identified through imaging.
Ossification of the Posterior Longitudinal Ligament (OPLL)
OPLL is a distinct pathological process in which the posterior longitudinal ligament, running along the back of the vertebral bodies, undergoes calcification or ossification. As this ligament transforms into a rigid structure of bone-like tissue, it can significantly narrow the spinal canal. This condition is more prevalent in certain populations, particularly in East Asian countries, suggesting potential genetic or environmental factors.
Because OPLL can progress gradually, early symptoms may be mild, such as occasional neck pain or stiffness. However, as the ossification advances, it can lead to marked spinal cord compression, manifesting as numbness, weakness, or coordination problems in the limbs. In severe cases, surgical decompression is often considered to remove or reduce the ossified ligament, relieving pressure on the spinal cord and preventing irreversible neurological deficits.
Risk Factors
Several factors can increase the risk of developing cervical stenosis:
- Age: The risk increases with age, as degenerative changes become more common.
- Genetics: A family history of spinal conditions can increase susceptibility.
- Occupation: Jobs that involve repetitive neck movements or heavy lifting can contribute to wear and tear on the cervical spine.
- Lifestyle: Poor posture, smoking, and obesity can contribute to spinal degeneration.
Understanding the causes and risk factors of cervical stenosis is essential for early diagnosis, prevention, and effective management of the condition. Early intervention can help mitigate symptoms and improve quality of life for those a
Symptoms of cervical stenosis
Symptoms of Cervical Stenosis
Cervical stenosis, a condition characterized by the narrowing of the spinal canal in the neck, can lead to a range of symptoms that vary in severity depending on the degree of compression on the spinal cord and nerve roots. These symptoms often develop gradually but can significantly impact an individual’s quality of life if left untreated. Below is a detailed exploration of the common symptoms associated with cervical stenosis.
Neck Pain
Neck pain is one of the hallmark symptoms of cervical stenosis. This discomfort can range from mild, intermittent aching to severe, persistent pain that radiates down into the shoulders or upper back. The pain is often caused by irritation or inflammation in the surrounding structures, such as ligaments, joints, or muscles, due to increased pressure on the cervical spine. Movements such as looking up, turning the head, or prolonged periods of poor posture can exacerbate the discomfort.
Numbness and Tingling
Numbness and tingling sensations, also known as paresthesia, are common in cervical stenosis, typically affecting the arms, hands, and sometimes the shoulders. These sensations result from the compression of nerve roots as they exit the narrowed spinal canal. The distribution of these symptoms often corresponds to the specific nerve roots affected. For example, compression at the C6 or C7 level may lead to numbness or tingling in the thumb, index, or middle fingers. These symptoms are often more pronounced during activities that involve neck extension or prolonged positioning.
Weakness and Loss of Coordination
Cervical stenosis can also cause muscle weakness and difficulty with coordination, particularly in the arms and hands. This weakness may manifest as difficulty grasping objects, writing, or performing fine motor tasks such as buttoning a shirt. As the condition progresses, leg weakness can also occur, affecting walking and balance. These symptoms arise from the disruption of nerve signals to the muscles due to spinal cord or nerve root compression, which can impair motor function.
Radiculopathy and Myelopathy
Radiculopathy and myelopathy are two distinct but related conditions that may arise from cervical stenosis:
- Radiculopathy: This occurs when specific nerve roots are compressed, leading to radiating pain, numbness, or tingling along the pathway of the affected nerve. It is often described as a sharp or burning sensation and may affect one or both arms.
- Myelopathy: This occurs when the spinal cord itself is compressed. Symptoms include weakness, difficulty with balance, and a sense of clumsiness, especially in the hands. Myelopathy is a serious condition requiring immediate medical attention to prevent permanent neurological damage.
Sensory Loss and Stiffness
As cervical stenosis progresses, sensory deficits may develop, causing reduced sensitivity to touch, temperature, or vibration in the hands or feet. These sensory changes can significantly affect daily activities and increase the risk of injuries. Stiffness in the neck is another common symptom, often accompanied by a reduced range of motion. This stiffness can be due to chronic inflammation, degenerative changes, or muscle guarding in response to the narrowing of the spinal canal.
Symptoms Based on Severity
Symptoms of Cervical Stenosis Based on Severity
Cervical stenosis, the narrowing of the spinal canal in the neck, can lead to a spectrum of symptoms ranging from mild discomfort to severe neurological impairment. Understanding the progression of symptoms based on their severity helps in recognizing the condition early and seeking timely treatment.
Mild Symptoms
In the early stages of cervical stenosis, symptoms may be subtle and easily overlooked. These include:
- Intermittent Neck Pain:
Mild to moderate neck discomfort is often the first sign. This pain may be dull or achy and can worsen after prolonged activity or poor posture. - Occasional Stiffness:
Mild stiffness in the neck, particularly after waking up or sitting in one position for extended periods, can occur. - Tingling or Numbness:
A slight tingling sensation in the arms, hands, or fingers may develop. These symptoms are often intermittent and occur during certain activities, such as holding a phone or typing.
Moderate Symptoms
As the condition progresses, the symptoms become more persistent and noticeable, affecting daily activities:
- Persistent Neck Pain and Stiffness:
Pain becomes more frequent and is often accompanied by reduced range of motion in the neck, making it difficult to turn or tilt the head. - Numbness and Tingling in Extremities:
Paresthesia (numbness or tingling) becomes more prominent, affecting the arms, hands, and occasionally the legs. These sensations are typically related to specific nerve root compressions. - Muscle Weakness:
Weakness in the arms or hands may develop, leading to difficulty with tasks requiring fine motor skills, such as writing, gripping objects, or buttoning clothes. - Radiculopathy:
Pain may radiate from the neck into the shoulders and arms, often described as sharp, shooting, or burning. The pain follows the pathway of the compressed nerve roots.
Severe Symptoms
In advanced stages, cervical stenosis can cause serious neurological impairment and significantly reduce quality of life. These severe symptoms may include:
- Myelopathy (Spinal Cord Compression):
- Loss of Coordination: Difficulty with hand movements, such as typing or holding utensils.
- Impaired Walking and Balance: Gait may become unsteady, with frequent tripping or stumbling.
- Spasticity: Stiffness and involuntary muscle spasms in the arms or legs.
- Severe Weakness:
Marked weakness in the arms, hands, or legs can make everyday tasks, such as lifting objects or walking, challenging. - Sensory Loss:
Reduced sensation in the hands and feet, leading to difficulty feeling textures, temperatures, or vibrations. - Bladder and Bowel Dysfunction:
In rare but serious cases, severe compression of the spinal cord can affect autonomic nerves, leading to issues with bladder or bowel control. - Chronic Pain:
Severe, constant pain that limits mobility and interferes with daily activities.
Recognizing the Progression
Cervical stenosis symptoms can worsen over time if the underlying cause, such as degenerative changes or herniated discs, is not addressed. Early recognition of mild to moderate symptoms allows for conservative management, while severe symptoms often require surgical intervention to prevent permanent neurological damage.
If you notice any symptoms, especially those related to weakness, coordination issues, or myelopathy, consult a healthcare professional promptly. Early diagnosis and appropriate treatment are key to managing cervical stenosis effectively.
Pathophysiology
Here is a step-by-step and clear explanation of the pathophysiology of spinal stenosis:
- Onset of Spinal Stenosis: Spinal stenosis can be caused by several factors, including aging, osteoarthritis, birth defects, tumors, or trauma. In most cases, it is related to a combination of these factors.
- Osteoarthritis and Osteophyte Formation: Osteoarthritis, a process of joint degeneration, can lead to the formation of osteophytes, bony growths. These osteophytes can grow into the spinal canal, contributing to narrowing.
- Thickening of Ligaments: In response to wear and tear and osteoarthritis, the ligaments surrounding the spinal canal may thicken. This can contribute to compression of the spinal cord and nerve roots.
- Herniated Disc: The intervertebral discs between the vertebrae can undergo degenerative changes. A herniated disc, where the gelatinous core of the disc extends beyond its normal limit, can occur. This can also contribute to narrowing of the spinal canal.
- Disc Space Reduction: As we age, the space between the vertebrae may become smaller due to the decreased height of the intervertebral discs. This can also contribute to spinal stenosis.
- Nerve Compression: As the spinal canal narrows due to these various factors, the nerve structures within it, including the spinal cord and nerve roots, can become compressed. This can lead to symptoms such as pain, numbness, weakness, and coordination problems.
- Clinical Symptoms: Symptoms of spinal stenosis can vary depending on the location and severity of nerve compression. Patients may experience pain in the back, buttocks, or legs, tingling sensations, numbness, muscle weakness, and difficulty walking.
It is important to note that spinal stenosis may be asymptomatic in some people and the severity of symptoms may vary from individual to individual.
When to Seek Medical Attention
It’s important to seek medical attention if you experience:
- Sudden or severe neck pain
- Progressive weakness or numbness in the arms or legs
- Loss of coordination or balance
- Bladder or bowel dysfunction
Early diagnosis and treatment are crucial to managing cervical stenosis and preventing further complications. If you experience any of these symptoms, consult a healthcare professional for a thorough evaluation and appropriate intervention.
Differential diagnoses
Cervical stenosis can present with symptoms similar to other medical conditions. Here are some differential diagnoses to consider when evaluating cervical stenosis symptoms:
- Cervical osteoarthritis (cervical osteoarthritis):
- Degeneration of the cervical joints can cause similar symptoms, such as neck pain and stiffness.
- Cervical disc herniation:
- A herniated disc in the cervical region can compress nerves and cause symptoms such as pain, numbness or weakness in the arms.
- Myélopathie cervicale :
- It involves compression of the spinal cord in the cervical region, causing coordination problems, muscle weakness and difficulty walking.
- Spondylose cervicale :
- Cervical spondylosis involves wear and tear of the intervertebral discs and can cause symptoms similar to cervical stenosis.
- Migraines cervicales :
- Some migraines can be triggered by neck problems, causing headaches and associated symptoms.
- Arnold’s neuralgia:
- This is a nerve condition that can cause severe headaches and pain along the occipital nerve, which can be confused with symptoms of cervical stenosis.
- Cervical tumors:
- Tumors in the cervical region can compress the spinal cord or nerve roots, causing symptoms similar to those of cervical stenosis.
- Cervical foraminal stenosis:
- This specific narrowing of the holes through which nerve roots exit the spine can cause symptoms similar to those of cervical stenosis.
- Infections cervicales :
- Infections in the cervical region can cause inflammation and symptoms similar to stenosis.
- Lyme disease :
- In some areas where Lyme disease is prevalent, it can cause neurological symptoms that resemble those of cervical stenosis.
Diagnosis
Cervical stenosis refers to the narrowing of the spinal canal in the cervical region of the spine, which can put pressure on the spinal cord or nerve roots. Symptoms may include neck pain, numbness, weakness, or balance problems. Here is some general information about the diagnosis and treatment of cervical stenosis:
Diagnostic
- Medical exams: A healthcare professional may perform a physical exam to assess symptoms, test muscle strength and reflexes, and observe neck mobility.
- Medical imaging: Imaging tests such as X-rays, MRI (magnetic resonance imaging), or CT scans may be done to visualize the spine and identify narrowing of the spinal canal.
- Electromyography (EMG): This test can be used to assess the electrical activity of muscles and identify areas of nerve compression.
- Myelography: This is a special X-ray where a dye is injected into the spinal canal to better visualize the spinal cord.
Treatment
- Drugs :
- Nonsteroidal anti-inflammatory drugs (NSAIDs) can relieve pain and inflammation.
- Analgesics may be prescribed for pain relief.
- Muscle relaxants can help relax neck muscles.
- Physical therapy:
- Specific exercises can strengthen neck muscles, improve flexibility, and relieve pressure on the spinal cord.
- Injection therapy:
- Corticosteroid injections can reduce inflammation around the nerves and relieve pain.
- Cervical orthoses:
- Wearing a neck brace or cervical orthosis can help limit neck movement, reducing pressure on the spinal cord.
- Lifestyle changes:
- Maintaining a healthy weight and adopting good posture can help reduce symptoms.
- Surgery :
- In cases of severe symptoms that do not respond to conservative treatments, surgery may be considered. Procedures may include surgical decompression to widen the spinal canal.
- Pain management:
- Complementary approaches such as acupuncture, osteopathy can be considered to help manage pain.
Conclusion
In conclusion, cervical stenosis represents a significant medical challenge due to its impact on the spinal canal and spinal cord in the cervical region of the spine. Associated symptoms, such as pain, weakness, tingling, and numbness in the arms, hands, and even legs, can significantly impair the quality of life of affected individuals.
The diversity of causes, ranging from natural aging to underlying medical conditions, underscores the complexity of this condition. Early diagnosis, often using imaging tests, is essential to allow appropriate intervention.
Treatment for cervical stenosis varies depending on the severity of symptoms. Conservative approaches, such as drug pain management, osteopathy, and lifestyle adjustments, are often considered first. However, in more severe cases or when nerve function is compromised, surgical options may be considered.
The decision between conservative and surgical treatments depends on many factors, and it is crucial to closely involve healthcare professionals in the decision-making process. Continuing advances in surgical techniques provide safer and more effective options to relieve pressure on the spinal cord.
Ultimately, cervical stenosis highlights the importance of a holistic approach in managing this condition. Awareness of risk factors, early diagnosis and appropriate treatment are essential to minimise the debilitating effects of cervical stenosis and improve the quality of life of those affected.
Questions and answers
Question 1: What is cervical stenosis?
A) Inflammation of the intervertebral discs
B) Narrowing of the spinal canal in the cervical region
C) Degeneration of the cervical joints
D) Compression of the nerves in the lumbar region
Question 2: What are the common symptoms of cervical stenosis?
A) Lower back pain and numbness in the legs
B) Neck pain, weakness, tingling or numbness in the arms, hands and sometimes legs
C) Headache and neck stiffness
D) Chest pain and difficulty breathing
Question 3: What are the factors that can cause cervical stenosis?
A) Cervical infections
B) Lyme disease
C) Osteoarthritis, bone spurs, herniated discs and trauma
D) Ankylosing spondylitis
Question 4: How can cervical stenosis be diagnosed?
A) By obvious symptoms without the need for medical tests
B) By X-rays only
C) By physical examination, imaging tests such as MRI and a detailed medical history
D) By ultrasound of the spine
Question 5: What is the pathophysiology of cervical stenosis?
A) Thickened ligaments have no connection with cervical stenosis
B) Herniated disc is the only cause of cervical stenosis
C) Cervical stenosis can result from aging, osteoarthritis, bone spurs, thickened ligaments, and herniated disc
D) Cervical stenosis is exclusively caused by trauma
Question 6: What are the symptoms that may be associated with cervical stenosis?
A) Chest pain and tingling in the hands
B) Muscle weakness, difficulty walking, and bladder control problems
C) Neck stiffness and headaches only
D) Lower back pain and numbness in the feet
Question 7: What are the possible treatments for cervical stenosis?
A) Medications, physical therapy, injection therapy, cervical orthotics, lifestyle changes, and surgery
B) Medications only
C) Surgery only
D) Physical therapy and acupuncture only
Question 8: What are the differential diagnoses of cervical stenosis?
A) Cervical tumors only
B) Cervical osteoarthritis, cervical disc herniation, cervical myelopathy and cervical spondylosis
C) Cervical migraines only
D) Cervical infections only
Question 9: What is the role of bone spurs in the pathophysiology of cervical stenosis?
A) They contribute to widening the spinal canal
B) They have no connection with cervical stenosis
C) They can grow in the spinal canal, contributing to narrowing
D) They cause herniated discs
Question 10: How can cervical stenosis be asymptomatic?
A) It can never be asymptomatic
B) Symptoms are always severe
C) In some people it may not cause symptoms
D) Only in young people
Answers to questions :
- B) A narrowing of the spinal canal in the cervical region
- B) Neck pain, weakness, tingling or numbness in the arms, hands and sometimes legs
- C) Osteoarthritis, bone spurs, herniated discs and trauma
- C) Through a physical examination, imaging tests such as MRI, and a detailed medical history
- C) Cervical stenosis can result from aging, osteoarthritis, bone spurs, thickening of ligaments, and herniated discs
- B) Muscle weakness, difficulty walking and bladder control problems
- A) Medications, physical therapy, injection therapy, cervical orthoses, lifestyle changes and surgery
- B) Cervical osteoarthritis, cervical disc herniation, cervical myelopathy and cervical spondylosis
- C) They can grow into the spinal canal, contributing to narrowing
- C) In some people it may not cause symptoms
References
- Tang C, Moser FG, Reveille J, Bruckel J, Weisman MH. Cauda Equina Syndrome in Ankylosing Spondylitis: Challenges in Diagnosis, Management, and Pathogenesis. J Rheumatol. 2019 Dec;46(12):1582-1588. [PubMed]2.
- Glassman DM, Magnusson E, Agel J, Bellabarba C, Bransford RJ. The impact of stenosis and translation on spinal cord injuries in traumatic cervical facet dislocations. Spine J. 2019 Apr;19(4):687-694. [PubMed]3.
- Bindal S, Bindal SK, Bindal M, Bindal AK. Noninstrumented Lumbar Fusion with Bone Morphogenetic Proteins for Spinal Stenosis with Spondylolisthesis in the Elderly. World Neurosurg. 2019 Jun;126:e1427-e1435. [PubMed]4.
- Messiah S, Tharian AR, Candido KD, Knezevic NN. Neurogenic Claudication: a Review of Current Understanding and Treatment Options. Curr Pain Headache Rep. 2019 Mar 19;23(5):32. [PubMed]5.
- Urits I, Burshtein A, Sharma M, Testa L, Gold PA, Orhurhu V, Viswanath O, Jones MR, Sidransky MA, Spektor B, Kaye AD. Low Back Pain, a Comprehensive Review: Pathophysiology, Diagnosis, and Treatment. Curr Pain Headache Rep. 2019 Mar 11;23(3):23. [PubMed]6.
- Bagley C, MacAllister M, Dosselman L, Moreno J, Aoun SG, El Ahmadieh TY. Current concepts and recent advances in understanding and managing lumbar spine stenosis. F1000Res. 2019;8 [PMC free article] [PubMed]7.
- Melancia JL, Francisco AF, Antunes JL. Spinal stenosis. Handb Clin Neurol. 2014;119:541-9. [PubMed]8.
- Akar E, Somay H. Comparative morphometric analysis of congenital and acquired lumbar spinal stenosis. J Clin Neurosci. 2019 Oct;68:256-261. [PubMed]9.
- Schroeder GD, Kurd MF, Vaccaro AR. Lumbar Spinal Stenosis: How Is It Classified? J Am Acad Orthop Surg. 2016 Dec;24(12):843-852. [PubMed]10.
- Shim DM, Kim TG, Koo JS, Kwon YH, Kim CS. Is It Radiculopathy or Referred Pain? Buttock Pain in Spinal Stenosis Patients. Clin Orthop Surg. 2019 Mar;11(1):89-94. [PMC free article] [PubMed]11.
- Stienen MN, Ho AL, Staartjes VE, Maldaner N, Veeravagu A, Desai A, Gautschi OP, Bellut D, Regli L, Ratliff JK, Park J. Objective measures of functional impairment for degenerative diseases of the lumbar spine: a systematic review of the literature. Spine J. 2019 Jul;19(7):1276-1293. [PubMed]12.
- Kaye AD, Manchikanti L, Novitch MB, Mungrue IN, Anwar M, Jones MR, Helander EM, Cornett EM, Eng MR, Grider JS, Harned ME, Benyamin RM, Swicegood JR, Simopoulos TT, Abdi S, Urman RD, Deer TR, Bakhit C, Sanapati M, Atluri S, Pasupuleti R, Soin A, Diwan S, Vallejo R, Candido KD, Knezevic NN, Beall D, Albers SL, Latchaw RE, Prabhakar H, Hirsch JA. Responsible, Safe, and Effective Use of Antithrombotics and Anticoagulants in Patients Undergoing Interventional Techniques: American Society of Interventional Pain Physicians (ASIPP) Guidelines. Pain Physician. 2019 Jan;22(1S):S75-S128. [PubMed]13.
- Lavi ES, Pal A, Bleicher D, Kang K, Sidani C. MR Imaging of the Spine: Urgent and Emergent Indications. Semin Ultrasound CT MR. 2018 Dec;39(6):551-569. [PubMed]14.
- Deer TR, Grider JS, Pope JE, Falowski S, Lamer TJ, Calodney A, Provenzano DA, Sayed D, Lee E, Wahezi SE, Kim C, Hunter C, Gupta M, Benyamin R, Chopko B, Demesmin D, Diwan S, Gharibo C, Kapural L, Kloth D, Klagges BD, Harned M, Simopoulos T, McJunkin T, Carlson JD, Rosenquist RW, Lubenow TR, Mekhail N. The MIST Guidelines: The Lumbar Spinal Stenosis Consensus Group Guidelines for Minimally Invasive Spine Treatment. Pain Pract. 2019 Mar;19(3):250-274. [PubMed]