Introduction
Surfer’s myelopathy is a rare but notable condition that can develop in surfing enthusiasts due to repetitive movements of the neck and cervical spine. This condition is primarily attributed to excessive neck flexion and spinal cord compression while surfing.
From an etiological point of view, surfer’s myelopathy is linked to repeated mechanical stresses suffered by the spine during surfing activities. These stresses can cause damage to spinal cord structures, leading to symptoms such as numbness, muscle weakness and coordination problems.
The pathogenesis of this condition involves progressive impairment of the spinal cord due to repetitive movements. Injuries can vary in severity, from mild to severe, and require a thorough clinical evaluation to determine the nature and extent of the damage.
In terms of assessment, medical imaging techniques, such as magnetic resonance imaging (MRI), are often used to visualize the structures of the spinal cord and identify any abnormalities. Complete clinical evaluation, including analysis of symptoms and medical history, is also crucial for an accurate diagnosis.
The management of surfer’s myelopathy is based on a multidisciplinary approach. Specific osteopathic interventions, physiotherapy and counseling on behavioral modifications while surfing can help alleviate symptoms. Awareness of proper posture and appropriate movements is essential to prevent possible relapses.
Cause of Surfer’s Myelopathy
Surfer’s myelopathy has its roots in the repetitive mechanical stresses experienced by the spine, particularly the neck and cervical spine, while surfing. Constant flexion of the neck and compression of the spinal cord can lead to damage and progressive impairment of this crucial structure.
Excessive flexion of the neck while paddling, sudden changes in position on the board, as well as falls and impacts related to surfing contribute to the occurrence of this condition. These repeated actions generate significant forces and pressures on the spinal cord, which can lead to tissue damage and neurological disruption.
Mechanical stress on the spine can cause compression of the intervertebral discs and surrounding structures, leading to inflammation and symptoms characteristic of surfer’s myelopathy, such as numbness, muscle weakness and coordination problems.
It is essential to understand that surfer’s myelopathy is often the result of a combination of factors, including frequency and intensity of surfing sessions, individual technique, and genetic predisposition to spinal problems. Recognition of these risk factors can guide the prevention and management of this specific condition in surfing enthusiasts.
Symptoms of Surfer’s Myelopathy
Surfer’s myelopathy is characterized by a range of symptoms related to spinal cord injury, resulting from the repetitive mechanical stresses associated with surfing. The clinical manifestations of this condition can vary in intensity and combination, but several symptoms are commonly observed.
One of the predominant signs of surfer’s myelopathy is numbness and tingling. Affected people may experience abnormal sensations, often described as tingling or tingling, in the upper or lower limbs. These symptoms are indicative of sensory disturbances resulting from alterations in the transmission of nerve signals along the spinal cord.
Muscle weakness is also commonly observed. Muscles in the upper or lower limbs may lose strength, leading to a decreased ability to perform precise, sustained movements. These symptoms of muscle weakness can affect the quality of daily life and participation in sports activities, including surfing.
Coordination problems are another significant aspect of surfer’s myelopathy. Alterations in the transmission of nerve signals can lead to difficulties in coordinating movements, affecting balance and the ability to perform complex motor actions, which can directly impact surfing performance.
Neck and back pain are commonly reported symptoms. The stresses placed on the spine during surfing can lead to persistent pain, requiring special attention in the assessment and management of the condition.
Gait disturbances may occur, with individuals experiencing difficulty walking in a stable and coordinated manner. These gait alterations may be associated with muscle weakness and coordination problems, impacting overall mobility.
Finally, bladder and bowel control problems may be seen in some individuals with surfer’s myelopathy. These sphincter disorders result from damage to the spinal cord, affecting the normal regulation of bladder and intestinal functions.
Pathophysiology
The pathophysiology of surfer’s myelopathy lies in the repetitive mechanical stresses placed on the spine, particularly the neck and cervical spine, during surfing. These constant and specific movements associated with surfing, such as excessive neck flexion, rotation, and impact during falls, can lead to progressive damage to the spinal cord.
Excessive neck flexion is a key component of the pathophysiology. While paddling, surfers frequently adopt a neck flexion position to paddle and maintain balance on the board. This repeated action, combined with impacts during falls or waves, exposes the spinal cord to considerable mechanical forces, leading to repetitive microtrauma.
These mechanical stresses can cause compression of the intervertebral discs, herniated discs and damage to the surrounding tissues. These structural alterations of the spine can result in direct compression of the spinal cord, disrupting the normal transmission of nerve signals.
The resulting lesions can affect the sensory and motor pathways of the spinal cord. Symptoms, such as numbness, tingling, muscle weakness, and coordination problems, reflect this disruption in nerve communication. Damage to nerve fibers can lead to decreased muscle sensitivity and strength, impacting the ability to perform precise, coordinated movements.
The pathophysiology of surfer’s myelopathy may also involve inflammatory processes in response to repetitive microtrauma. Inflammation can make damage worse and contribute to the painful symptoms associated with the condition.
Medical imaging, particularly magnetic resonance imaging (MRI), is often used to visualize structural abnormalities of the spinal cord and confirm the diagnosis. A thorough clinical assessment, combined with radiological studies, is essential to understand the nature and extent of damage, which then guides the appropriate management for each patient.
Surfing and Physical Health: Posture, Strengthening and Preventative Advice
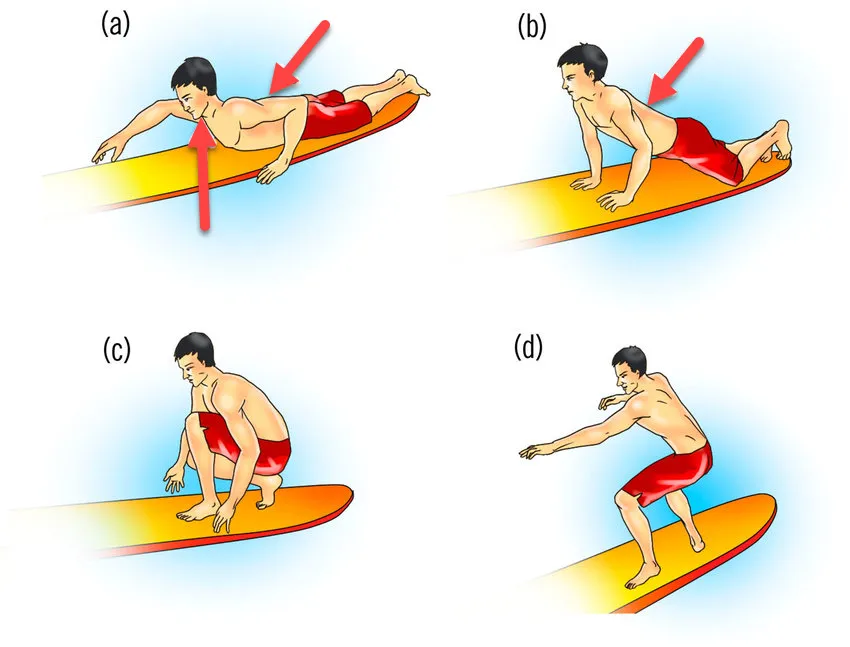
Correct posture when swimming in a prone position requires extension of the lumbar and thoracic spine to lift the upper chest off the deck of the surfboard and enable ergonomic swimming. Muscle strains at the cervical and lumbar level are relatively common, probably due to the sustained isometric contraction of these muscles during swimming. For example, surfing after long periods of inactivity often leads to burning muscle pain in the trapezius and rhomboid muscles. Likewise, hyperextending the neck, to compensate for insufficient lumbar extension while surfing, can worsen neck pain. Fortunately, most neck and back spasms due to overuse resolve spontaneously, but physical therapy can also improve acute symptoms. A proper warm-up before surfing (especially in cold water) and regular stretching of your lower back, hamstrings and hip flexors can help prevent this common problem.
Active activation of the core musculature during swimming creates a solid swimming platform, unloading the muscles of the lower back. Therefore, land-based exercises aimed at improving core strength in surfers are essential. Previous observations suggest that although surfers have more powerful shoulder flexion and extension than other athletes, they often have weaker core strength. Persistent neck pain despite conservative treatment may be due to cervical disc injury, degenerative arthritis in older surfers, or thoracic outlet syndrome. Symptoms are exacerbated by movements that severely stretch the lower back, such as diving under approaching waves or standing up (going from lying to standing) on a surfboard. Stress fractures of the pars interarticularis usually heal with conservative therapy but often require 4 to 6 months off from sports, although some may require spinal fusion later in life.
The Physiological Issues of the Surfer: Postural Impact and Vascular Risks
Novice surfers tend to spend more time in hyperlordosis compared to experienced surfers. The vulnerability of this posture, combined with the time spent in it, can significantly predispose them to the development of spinal cord disease following an event such as venous thrombosis. The persistent pressure of the surfboard on the surfer’s trunk can impede the flow of the inferior vena cava, worsening complications related to weakened venous blood flow. Suddenly moving from a pronated hyperextension position of the lumbar spine to a plank squat position and the associated Valsalva maneuver may contribute to increased spinal pressure and ischemia. This rapid transition from lying on the board in a hyperextended position to squatting to perform the Valsalva maneuver represents a significant change in stress on the spine. Less experienced surfers may be more prone to this abrupt transition, exposing their spine to additional pressures and increased risk of ischemia.
The balance between these different positions is crucial, because the occurrence of complications, notably venous thrombosis, can be exacerbated by impaired blood circulation. Surfers should be aware of the potential impacts of these postural changes on their spinal and vascular health. Knowledge of these risks can encourage safer practices when transitioning between these positions, thereby minimizing stress on the spine and improving blood circulation.
In sum, the progression of surfer posture, from lying on the board to crouching to execute specific maneuvers, represents a physiological challenge and can have significant implications for the health of the spine and blood circulation. venous. Understanding these mechanisms by surfers, especially beginners, is essential to minimize potential risks and promote safer and healthier surfing.
Preventative measure to prevent surfer’s myelopathy
In the specific context of preventing surfer’s myelopathy, preventive measures can be implemented to mitigate the risks associated with surfing and reduce mechanical stress on the spine. These measures aim to promote a proactive approach to minimizing risk factors and promoting the spinal health of surfers. Here are some recommendations to prevent surfer’s myelopathy:
Education on Technique and Posture:
Educating surfers on proper technique and posture is fundamental. By emphasizing the importance of maintaining a natural curvature of the neck and back when paddling and standing up on the board, mechanical stress on the spine can be reduced. Surfers should be aware of movements that can cause excessive neck flexion, preventing potential injuries.
Muscle Strengthening and Flexibility:
An exercise program focused on muscle strengthening, with emphasis on the muscles of the neck, back and core, can help stabilize the spine and reduce stress on the spinal cord. Flexibility exercises to maintain appropriate range of motion can also be beneficial in preventing stiffness and tightness.
Use of Protective Equipment:
Using protective equipment, such as properly fitted flotation vests, can help minimize the impact of falls and keep surfers safe. Specific equipment designed to reduce pressure on the neck and spine may also be considered for surfers particularly prone to back problems.
Limitation of Practice Time and Adequate Rest:
Excessive surfing, especially in extreme conditions, can increase the risk of injury. Encouraging surfers to take regular breaks and respect their body’s limits can help prevent excessive fatigue and reduce strain on the spine.
References
- Thompson TP, Pearce J, Chang G, Madamba J. Surfer’s myelopathy. Spine (Phila Pa 1976) . 2004;29(16):E353–6. doi: 10.1097/01.BRS.0000134689.84162.E7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nathanson A, Bird S, Dao L, Tam-Sing K.. Competitive surfing injuries: a prospective study of surfing-related injuries among contest surfers. Am J Sports Med . 2007;35(1):113–7. doi: 10.1177/0363546506293702 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nathanson A, Haynes P, Galanis D.. Surfing injuries. Am J Emerg Med . 2002;20(3):155–60. doi: 10.1053/ajem.2002.32650 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wadia S, Padmanabhan P, Moeller K, Rominger A.. Pediatric surfer’s myelopathy. J Emerg Med . 2015;49(5):e143–5. doi: 10.1016/j.jemermed.2015.06.065 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Conidi F. Some unusual sports-related neurologic conditions. Continuum (Minneap Minn) . 2014;20(6 Sports Neurology):1645–56. [ PubMed ] [ Google Scholar ]
- Maharaj MM, Phan K, Hariswamy S, Rao PJ.. Surfer’s myelopathy: a rare presentation in a non-surfing setting and review of the literature. J Spine Surg . 2016;2(3):222–6. doi: 10.21037/jss.2016.09.07 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Freedman BA, Malone DG, Rasmussen PA, Cage JM, Benzel EC.. Surfer’s myelopathy: a rare form of spinal cord infarction in novice surfers: a systematic review. Neurosurgery . 2016;78(5):602–11. doi: 10.1227/NEU.0000000000001089 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nakamoto BK, Siu AM, Hashiba KA, Sinclair BT, Baker BJ, Gerber MS, et al. Surfer’s myelopathy: a radiologic study of 23 cases. AJNR Am J Neuroradiol . 2013;34(12):2393–8. doi: 10.3174/ajnr.A3599 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Robles LA. Letter: surfer’s myelopathy: a rare form of spinal cord infarction in novice surfers: a systematic review. Neurosurgery . 2017;80(6):E266. doi: 10.1093/neuros/nyx044 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Takakura T, Yokoyama O, Sakuma F, Itoh R, Romero RR.. Complete paraplegia resulting from surfer’s myelopathy. Am J Phys Med Rehabil . 2013;92(9):833–7. doi:10.1097/PHM.0b013e3182411f58 [ PubMed ] [ Crossword ] [ Google Scholar ]
- Nathanson AT. Surfing injuries. In: Mei-Dan O, Carmont MR, (eds.) Adventure and Extreme Sports Injuries: Epidemiology, Treatment, Rehabilitation and Prevention . London: Springer; 2013. p. 143–72. [ Google Scholar ]
- Aoki M, Moriizumi S, Toki M, Murakami T, Ishiai S.. Rehabilitation and long-term course of nontraumatic myelopathy associated with surfing. Am J Phys Med Rehabil . 2013;92(9):828–32. doi: 10.1097/PHM.0b013e318238a1d0 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sunshine S. Surfing injuries. Curr Sports Med Rep . 2003;2(3):136–41. doi: 10.1249/00149619-200306000-00005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Renneker M. Surfing: the sport and the lifestyle. Phys Sportsmed . 1987;15(10):156–62. doi: 10.1080/00913847.1987.11702109 [ CrossRef ] [ Google Scholar ]
- Moeller JL, Rifat SF.. Spondylolysis in active adolescents: expediting return to play. Phys Sportsmed . 2001;29(12):27–32. doi: 10.3810/psm.2001.12.1074 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Aviles-Hernandez I, Garcia-Zozaya I, DeVillasante JM.. Nontraumatic myelopathy associated with surfing. J Spinal Cord Med . 2007;30(3):288–93. doi: 10.1080/10790268.2007.11753939 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chung HY, Sun SF, Wang JL, Lai PH, Hwang CW.. Non-traumatic anterior spinal cord infarction in a novice surfer: a case report. J Neurol Sci . 2011;302(1–2):118–20. doi: 10.1016/j.jns.2010.11.026 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Albuja AC, Qaiser S, Lightner DD, Raslau FD, Zafar MS, Bernard PA, et al.. Surfer’s myelopathy without surfing: a report of two pediatric patients. Spinal Cord Ser Cases . 2017;3:17008. doi: 10.1038/scsandc.2017.8 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- eixeira S, Moser F, Kotton RH.. Imaging features and differentials in surfers’ myelopathy: a case report. Emerg Radiol . 2016;23(1):89–92. doi:10.1007/s10140-015-1346-1 [ PubMed ] [ Crossword ] [ Google Scholar ]
- Choi J, Seok HY, Kim Y, Kim BJ.. Surfer’s myelopathy mimicking infectious myelitis. J Clin Neurol . 2017;13(2):207–8. doi: 10.3988/jcn.2017.13.2.207 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Scatchard R, Alves Rosa J, Bowen P, Mortimer A, Sharples PM, Lux AL.. A case report: pediatric surfer’s myelopathy. Eur J Paediatr Neurol . 2018;22(1):199–202. doi: 10.1016/j.ejpn.2017.09.011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sugiyama N, Yokoyama JI, Ikegami M, Matsuda S, Miyashita Y.. A child case of surfer’s myelopathy. No To Hattatsu . 2016;48(1):41–4. [ PubMed ] [ Google Scholar ]