Trochanteric bursitis is a common source of lateral hip pain that results from inflammation of the hip bursa.
Introduction
Trochanteric bursitis, a painful problem occurring in the hip region, is increasingly recognized as a major source of discomfort and functional limitations for many people. This inflammatory condition specifically targets the bursa, a small pocket of fluid designed to minimize friction between the tendons, muscles and bones surrounding the hip. When this bursa becomes inflamed, it causes persistent pain and reduced mobility, leading to a significant influence on the quality of life of affected individuals. This introduction provides a solid foundation for examining in detail the origins, symptoms, diagnoses, and treatment options related to trochanteric bursitis.

Causes
Trochanteric bursitis can have various origins, often linked to mechanical, traumatic or inflammatory factors. Common causes include excessive pressure on the bursa from strenuous physical activity, repetitive movements, or poor posture. Traumatic injuries, such as falls to the side of the hip, can also trigger inflammation of the bursa. Additionally, underlying medical conditions such as arthritis may contribute to this condition.
- Repeated rubbing:
- One of the main causes is repeated friction between the bursa and the tendons or muscles that pass over the greater trochanter. This can result from repetitive movements, such as walking, running, or standing for long periods of time.
- Overuse or strenuous activity:
- Excessive activity or heavy use of the hip, such as frequent participation in sports such as running or hiking, can contribute to irritation of the bursa.
- Unbalanced muscle tension:
- Muscular imbalances, particularly those involving the hip and thigh muscles, can place uneven pressure on the bursa, contributing to its inflammation.
- Anatomical abnormalities:
- Certain anatomical abnormalities, such as differences in leg length or abnormal position of the hip bones, can increase the risk of trochanteric bursitis.
- Direct trauma:
- Direct trauma, such as a fall to the side of the hip, can also cause inflammation of the bursa.
- Inflammatory diseases:
- Inflammatory diseases such as rheumatoid arthritis can increase the risk of developing trochanteric bursitis.
- Other hip conditions:
- Conditions such as tendonitis of the hip muscles or conditions of the hip joint can contribute to irritation of the bursa.
It is essential to note that several factors can interact to cause trochanteric bursitis, and often, there is not one single cause. People with intensive physical activities, muscular imbalances, or particular anatomical factors may be more predisposed to developing this condition.
Symptoms
- Hip pain:
- The pain is often located on the side of the hip, above the greater trochanter. It can also radiate towards the thigh or buttock. The pain may be felt when walking, climbing stairs, or getting up after a period of rest.
- Increased pain when sitting:
- Symptoms may worsen when a person sits for long periods of time, especially on hard surfaces. This can make activities such as driving or sitting at a desk uncomfortable.
- Sensitivity to palpation:
- By gently pressing on the affected area, the practitioner may note localized tenderness or pain in the greater trochanter.
- Swelling or heat:
- There may be slight swelling or a feeling of warmth in the affected hip, indicating an inflammatory reaction.
- Stiffness:
- Some patients may experience hip stiffness, particularly after a period of inactivity.
- Night pain:
- Some individuals may experience increased pain during the night, especially when the hip is stressed during sleep.
- Difficulty lying down on the affected side:
- Some patients may have difficulty finding a comfortable position when trying to lie on the affected side.
Differential diagnosis
- Osteoarthritis of the hip:
- Osteoarthritis of the hip can cause pain similar to trochanteric bursitis. However, osteoarthritis is usually associated with wear and tear of the cartilage in the hip joint.
- Hip muscle tendinopathy:
- Tendinopathies of surrounding muscles, such as the gluteus medius tendon, can also cause pain in the trochanteric region. This condition can coexist with trochanteric bursitis.
- Piriformis syndrome:
- Piriformis syndrome can present with similar symptoms, including buttock and hip pain. It results from compression of the sciatic nerve by the piriformis muscle.
- Lumbar pathologies:
- Problems in the lumbar spine, such as herniated disc or spinal stenosis, can radiate pain to the hip area, possibly being confused with trochanteric bursitis.
- Bone tumors:
- Bone tumors in the hip area can cause similar pain. They require a thorough assessment to rule out this possibility.
- Rotator cuff tendinopathy:
- Although more commonly associated with the shoulder, rotator cuff tendinopathy can sometimes cause referred pain to the hip.
- Joint infections:
- Infections in the hip joint can cause similar pain. They require immediate attention due to their severity.
Diagnosis and treatment
Diagnosis of trochanteric bursitis
- History and clinical examination:
- The healthcare professional will begin by taking a complete medical history, asking about symptoms, history of physical activities, and any traumatic events. A physical examination will also be performed to assess sensitivity to palpation and mobility of the hip.
- Imaging tests:
- X-rays, ultrasounds, or an MRI may be recommended to rule out other possible causes of hip pain, such as fractures, joint abnormalities, or tendon injuries.
- Specific tests:
- Certain clinical tests, such as the hip abduction strength test, may be performed to assess the presence of trochanteric bursitis.
Treatment of trochanteric bursitis
- Rest and modification of activities:
- Reducing activities that exacerbate hip pain, such as prolonged walking or running, can help relieve pressure on the inflamed bursa.
- Ice application:
- Applying ice to the affected area can help reduce inflammation. It is recommended to apply ice for 15-20 minutes every 2-3 hours.
- Non-steroidal anti-inflammatory drugs (NSAIDs):
- Nonsteroidal anti-inflammatory medications, such as ibuprofen, may be prescribed to reduce pain and inflammation.
- Osteopathy:
- An osteopathy program may be recommended to strengthen surrounding muscles, improve flexibility and correct possible muscle imbalances.
- Corticosteroid injections:
- In some cases, corticosteroid injections directly into the bursa may be considered to reduce inflammation.
- Education and habit modification:
- Education about positions and movements to avoid, as well as advice on changing daily habits, can be an integral part of treatment.
- Changes in physical activities:
- Adjusting physical activities, with the incorporation of appropriate exercises, can help prevent the recurrence of trochanteric bursitis.
- Orthotics or walking aids:
- In some cases, the use of orthotics or walking aids can relieve pressure on the hip.
If symptoms do not improve despite conservative measures, surgical intervention to drain or remove the bursa (bursectomy) may be considered in severe cases resistant to treatment. However, most cases of trochanteric bursitis respond well to nonsurgical approaches.
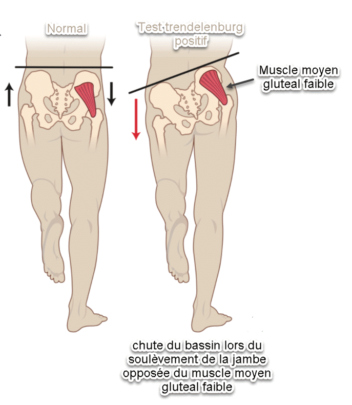
Trendelenberg test
The Trendelenburg test is often used to assess the strength of the hip muscles and to detect possible problems in this area, including trochanteric bursitis. Here is how the Trendelenburg test is generally performed:
Trendelenburg Test procedure for screening for trochanteric bursitis:
- Patient position:
- The patient is asked to stand with their feet together, facing the person performing the test.
- Instructions to the patient:
- The patient is then instructed to raise one leg off the ground by bending the knee. This may be the affected leg (the side of the hip with symptoms) or the other leg.
- Observation :
- The examiner observes the level of the patient’s hips during the leg raise phase. Normally, the hips remain level, but in cases of hip muscle weakness or a problem like trochanteric bursitis, the pelvis on the side of the raised leg may sag.
- Side Rating:
- If the hips remain level, the test is considered normal. However, if the pelvis on the side opposite the raised leg sags, this indicates a positive Trendelenburg test.
Interpretation:
- A positive Trendelenburg test may suggest weakness in the hip muscles, including the gluteus medius, which is often involved in problems such as trochanteric bursitis.
It is important to note that although the Trendelenburg test can indicate muscle weakness, it does not provide a definitive diagnosis of trochanteric bursitis. Other clinical examinations, such as specific stress tests, a complete medical history, and imaging studies, are usually necessary to confirm the presence of trochanteric bursitis. If symptoms persist, it is recommended to consult a healthcare professional for a thorough evaluation and accurate diagnosis.
Exercises and stretching
Muscle strengthening exercises
- Clamshells:
- Lie on your side with your knees bent.
- Lift your top knee while keeping your feet together.
- Hold the position for a few seconds before lowering back down.
- Repeat on the other side.
- Hip bridges:
- Lie on your back with your knees bent and your feet flat on the floor.
- Lift your hips by contracting your gluteal muscles and hold the position.
- Slowly lower your hips back toward the floor.
- Repeat the movement.
- Hip extensions:
- On all fours, lift one leg behind you while keeping your knee bent at 90 degrees.
- Hold the position by contracting your gluteal muscles.
- Slowly lower the leg and repeat the movement.
Stretching
- Gluteus medius stretch:
- Sitting on the floor, cross the affected leg over the other knee.
- Place the opposite elbow on the outside of the bent knee and gently twist the trunk.
- Hold the position for 15-30 seconds.
- Hip flexor stretch:
- Kneeling on the floor, move the affected leg forward.
- Bend your knee slightly while keeping your back straight.
- You should feel a stretch in the front of your hip.
- Hold the position for 15-30 seconds.
- Stretching the adductor muscles:
- Sitting on the floor, extend your legs out to the sides as wide as possible.
- Gently lean forward toward one leg, keeping your back straight.
- Hold the position for 15-30 seconds and repeat on the other side.
It is important to progress gradually with these exercises and stretches, always listening to the body.
Piriform


- Lie on your side with the affected hip on top. Cradle your head in your arm and bend your lower leg for support.
- Slowly move the top leg up and back 45°, keeping the knee straight. Hold this position for 5 seconds
- Slowly lower the leg for a count of 5 and relax it for 2 seconds.
- Ankle weights should be used, starting with weights light enough to allow 2 sets of 8 repetitions and progressing to 3 sets of 15 repetitions.
- Then return to 2 sets of 8 repetitions and add weight in 2-3 pound increments, working your way up. to 3 pounds, progressing each time up to 3 sets of 15 repetitions.
- Perform the exercise 3 times a week, continuing for 2 to 3 weeks.
Iliotibial band

- Stand about 2 feet from a wall with the affected side toward the wall
- Fully extend your arm and place your hand on the wall for support.
- Cross the injured leg (the leg farthest from the wall) over the opposite leg.
- Lean your hips toward the wall until you feel a stretch on the outside of the injured leg.
- Hold the maximum stretch for 30 seconds, then relax for 10 seconds.
- Repeat the sequence 4 times on each side.
- Perform 2 to 3 sets of 4 repetitions 5 to 7 days per week, continuing for 2 to 3 weeks.
- Perform the stretch on both sides.
abduction

Stretching the iliotibial fascia (iliotibial band)

Stand with your affected hip against a wall. For additional support, you can use a chair or counter. Shift your weight to your affected hip and cross the other leg in front of it. Raise your arm on the same side as your affected hip above your head. Lean away from the wall, letting your affected hip press against the wall, until you feel a gentle stretch in the side of your hip. Hold the stretch for 15 to 30 seconds. Repeat 2 to 4 times.
References
- Segal NA, Felson DT, Torner JC, Zhu Y, Curtis JR, Niu J, Nevitt MC., Multicenter Osteoarthritis Study Group. Greater trochanteric pain syndrome: epidemiology and associated factors. Arch Phys Med Rehabil. 2007 Aug;88(8):988-92. [ PMC free article ] [ PubMed ]
- Bird PA, Oakley SP, Shnier R, Kirkham BW. Prospective evaluation of magnetic resonance imaging and physical examination findings in patients with greater trochanteric pain syndrome. Arthritis Rheum. 2001 Sep;44(9):2138-45. [ PubMed ]
- Fearon AM, Cook JL, Scarvell JM, Neeman T, Cormick W, Smith PN. Greater trochanteric pain syndrome negatively affects work, physical activity and quality of life: a case control study. J Arthroplasty. 2014 Feb;29(2):383-6. [ PubMed ]
- Steinert L, Zanetti M, Hodler J, Pfirrmann CW, Dora C, Saupe N. Are radiographic trochanteric surface irregularities associated with abductor tendon abnormalities? Radiology. 2010 Dec;257(3):754-63. [ PubMed ]
- Ganderton C, Semciw A, Cook J, Moreira E, Pizzari T. Gluteal Loading Versus Sham Exercises to Improve Pain and Dysfunction in Postmenopausal Women with Greater Trochanteric Pain Syndrome: A Randomized Controlled Trial. J Womens Health (Larchmt). 2018 Jun;27(6):815-829. [ PubMed ]
- Attum B, Varacallo M. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Dec 18, 2021. Anatomy, Bony Pelvis and Lower Limb, Thigh Muscles. [ PubMed ]
- Mellor R, Bennell K, Grimaldi A, Nicolson P, Kasza J, Hodges P, Wajswelner H, Vicenzino B. Education plus exercise versus corticosteroid injection use versus a wait and see approach on global outcome and pain from gluteal tendinopathy: prospective, single blinded , randomized clinical trial. Br J Sports Med. 2018 Nov;52(22):1464-1472. [ PubMed ]
- Mathew J, Sankar P, Varacallo M. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Apr 28, 2021. Physiology, Blood Plasma. [ PubMed ]
- credit in part: Aaron J. Seidman; Matthew Varacallo.


















