Introduction
The incidence of tuberculosis (TB) is on the rise globally, presenting a significant public health challenge. Several factors contribute to this increase, including the growing number of immunocompromised individuals, the emergence of drug-resistant strains of Mycobacterium tuberculosis, and an aging population. Among these factors, HIV stands out as the primary risk factor for the reactivation of latent TB infections, as it severely weakens the immune system, making individuals more susceptible to the disease.
According to the World Health Organization, approximately one-third of the world’s population is infected with Mycobacterium tuberculosis. It is considered one of the leading causes of death and disability worldwide. Alarmingly, about one-fifth of newly diagnosed TB cases are extrapulmonary, meaning the infection occurs outside the lungs, and the spine is involved in 50% of bone and joint TB cases. This spinal involvement can lead to severe complications, including deformities and neurological deficits.
Tuberculosis has been recognized as a disease since antiquity, with descriptions found in ancient texts and evidence found in skeletal remains. In 1779, Sir Percival Pott made significant contributions to the understanding of spinal TB by describing its clinical presentation, which includes kyphotic deformity and neurological deficits in European patients. His observations laid the foundation for future research and treatment of spinal tuberculosis.
The 20th century marked a turning point in the fight against tuberculosis. The discovery of Mycobacterium tuberculosis as the causative pathogen led to significant advancements in TB management. The development of the Bacillus Calmette-Guérin (BCG) vaccine provided a crucial tool for preventing TB, especially in children. Additionally, advances in diagnostic modalities, chemotherapeutic agents, and surgical procedures revolutionized the treatment of spinal tuberculosis, offering hope for recovery and improved quality of life for affected individuals.
Despite these advances, tuberculosis has experienced a resurgence in recent years, particularly in developed countries. This resurgence is largely attributed to the increase in global migration, which has led to the spread of TB across borders and into new populations. This “global migration phenomenon” has posed a significant challenge to the international community, as TB cases are often complicated by drug resistance and the presence of co-infections like HIV.
Addressing the resurgence of tuberculosis requires a multifaceted approach. Public health initiatives must focus on early detection and diagnosis, effective treatment regimens, and robust vaccination programs to prevent the spread of TB. Additionally, addressing the social determinants of health, such as poverty and access to healthcare, is crucial for controlling the disease. Research efforts continue to explore new diagnostic tools, treatments, and vaccines to combat the evolving threat of tuberculosis.
Epidemiology of Tuberculosis
Global Burden of Tuberculosis
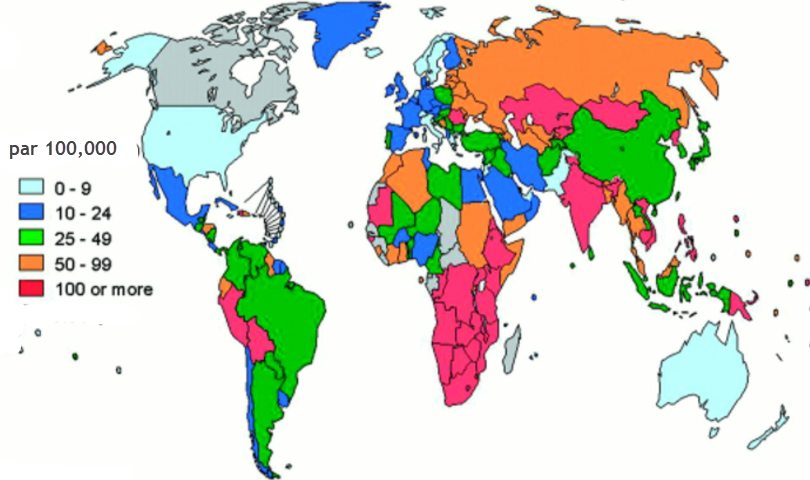
Tuberculosis (TB) remains one of the world’s most significant public health challenges, with a profound impact on global health. According to the World Health Organization (WHO), TB is one of the top 10 causes of death worldwide and the leading cause of death from a single infectious agent, surpassing even HIV/AIDS. In 2022, it was estimated that around 10.6 million people fell ill with TB, and 1.6 million people died from the disease. These numbers underscore the enduring threat TB poses, particularly in low- and middle-income countries.
Geographic Distribution
TB is a disease of global reach but is disproportionately concentrated in certain regions. The highest burden is found in South-East Asia and Africa, accounting for nearly 70% of all TB cases. India, China, Indonesia, the Philippines, Pakistan, Nigeria, and South Africa are among the countries with the highest TB burdens, collectively accounting for two-thirds of the global total. This uneven distribution reflects the socioeconomic disparities, healthcare access challenges, and varying levels of healthcare infrastructure that influence TB transmission and treatment outcomes.
Pathophysiology of spinal tuberculosis
The pathophysiology of spinal tuberculosis involves several steps and responses of the immune system to Mycobacterium tuberculosis infection. The following is a general description of the pathophysiology of this condition:
- Initial Infection: Spinal tuberculosis often begins with an initial infection of the respiratory tract, where Mycobacterium tuberculosis bacteria are inhaled. Once in the lungs, the bacteria can invade lung cells and escape destruction by the immune system.
- Hematogenous Spread: When bacteria manage to evade the immune response in the lungs, they can enter the bloodstream. Hematogenous spread allows the bacteria to reach other organs and tissues, including the spine.
- Granulomas Formation: Mycobacterium tuberculosis has the ability to resist clearance by immune cells. Cells of the immune system surround the bacteria, forming structures called granulomas. These granulomas are clumps of immune cells that attempt to isolate and contain the infection.
- Inflammatory Response: Granuloma formation triggers an inflammatory response in the spine. This can cause tissue damage, including bone destruction.
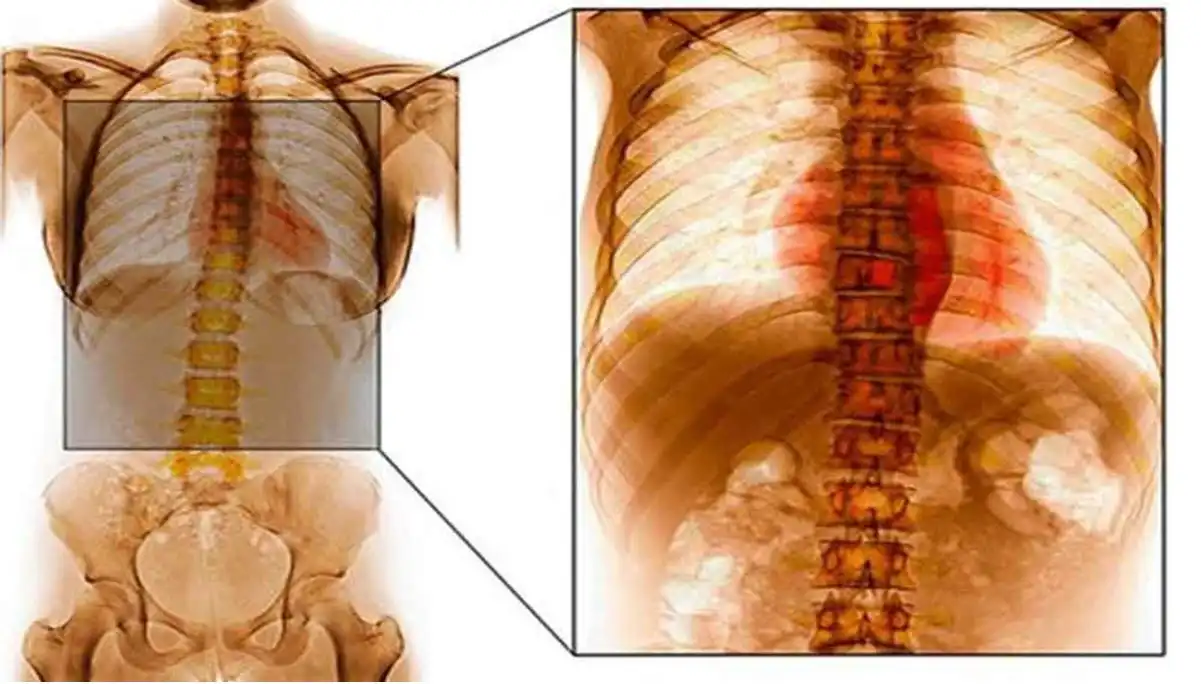
- Abscess Formation: In response to infection, abscesses may form around the spine. These pockets of pus are the body’s attempt to contain the infection and can be seen on medical images.
- Spinal Deformity and Complications: Inflammation and tissue destruction can lead to spinal deformities, vertebral compressions, and other complications. The injuries can affect the stability of the spine and, in some cases, compress nerve structures, leading to neurological symptoms.
- Chronic Immune Response: In cases where the infection is not cleared, a chronic immune response may persist. This can lead to scarring, permanent changes in bone structure, and long-term complications.
Causes of spinal tuberculosis
Spinal tuberculosis is primarily caused by infection of the spine with the bacteria Mycobacterium tuberculosis. This infection can occur in a number of ways, and several factors can contribute to its development. Here are some causes of spinal tuberculosis:
- Primary Lung Infection: Spinal tuberculosis is often the result of a primary lung infection with Mycobacterium tuberculosis. When a person inhales droplets containing the bacteria, they can develop a lung infection that, in some cases, spreads to other parts of the body, including the spine.
- Reactivation of Latent Infection: In some cases, spinal TB can result from reactivation of a latent TB infection. People who have been infected with the bacteria but have not developed symptoms may have the infection reactivate later in life, sometimes affecting the spine.
- Bloodborne Contamination: Spinal infection can occur through bloodborne transmission, meaning that bacteria reach the spine through the bloodstream. This can occur when the bacteria enter the bloodstream from another part of the body.
- Weakened Immune System: Individuals with weakened immune systems, either due to diseases such as HIV/AIDS or due to immunosuppressive medications, are more likely to develop spinal tuberculosis.
- Migration of Extravertebral Infection: In some cases, tuberculous infection may spread to the spine from extravertebral sites, such as adjacent lymph nodes.
- Genetic Factors: Some studies suggest that there may be genetic predispositions to tuberculosis, although the precise genetic contribution is not fully understood.
Symptoms of spinal tuberculosis
- Lower Back Pain: Pain in the lower back is one of the most common symptoms. The pain can be localized to the spine and worsen over time.
- Spine Stiffness: Stiffness of the spine may be present, limiting mobility and making movement painful.
- Vertebral Compression Disorders: Bone destruction resulting from infection can lead to vertebral compression disorders, where the vertebrae lose their normal height.
- Spinal Deformities: Untreated spinal tuberculosis can cause spinal deformities, such as kyphosis or scoliosis, giving the spine a curved appearance.
- Fever: Some patients may present with fever, often associated with a systemic inflammatory response to the infection.
- Fatigue: Fatigue can result from chronic infection and the body’s immune response.
- Weight Loss: Unexplained weight loss may occur, often due to malnutrition related to illness.
- Neurological Symptoms: In advanced cases, when the spine compresses nerve structures, neurological symptoms such as numbness, tingling, muscle weakness, and impaired bowel or bladder function may occur.
- Paravertebral Abscesses: The formation of paravertebral abscesses can cause painful swellings in the affected area.
Types of tuberculous lesions in the spine
Tuberculous lesions in the spine can present in different forms. Here are four common types of tuberculous lesions seen in the spine:
- Granulomas and Tubercles: Tubercles, also called tuberculous nodules, are small nodular lesions that form as a result of infection with Mycobacterium tuberculosis. These granulomas can develop in the vertebrae and cause bone destruction, eventually leading to spinal deformities.
- Paravertebral Abscess: Tuberculous infections in the spine can result in the formation of paravertebral abscesses. These abscesses are pockets of pus that form in the surrounding soft tissues, usually in response to bone infection. They can be seen on X-ray images.
- Tuberculous Spondylodiscitis: Tuberculous spondylodiscitis is an inflammation of the intervertebral discs and adjacent vertebrae. It can cause changes in the height of the intervertebral discs, vertebral compressions and angular deformities, contributing to kyphosis.
- Spinal Fusion: In advanced cases of untreated spinal tuberculosis, there may be fusion of the affected vertebrae. This fusion often results from the progressive destruction of bone tissue and scarring reaction, leading to loss of mobility in the spine.
It is important to note that spinal tuberculosis can affect multiple vertebrae, leading to more extensive lesions and severe complications. Accurate diagnosis of tuberculous lesions in the spine usually requires advanced imaging tests such as magnetic resonance imaging (MRI) and, in some cases, biopsies to confirm the presence of Mycobacterium tuberculosis.
Predisposing factors
- Malnutrition
- Poor sanitation
- Overcrowding
- Close contact with a tuberculosis patient
- Multiple pregnancy
- Immunodeficiency state
Regional distribution of spinal tuberculosis
- Cervical – 12%
- Cervicodorsal – 5%
- Dorsal – 42%
- Dorsolumbar – 12%
- Lumbar – 26%
- Lumbosacral – 3%
Radiographic signs of spinal tuberculosis
Tuberculosis of the spine, also called Pott’s disease when it affects the vertebrae, has specific radiographic findings. These findings may vary depending on the stage of the disease and the severity of the disease. Some of the commonly observed radiographic findings include:
- Bone Lesions: X-rays may reveal characteristic bone lesions, such as areas of bone destruction, geodes, bone sequestra, and sometimes changes in bone density.
- Spinal Deformity: A spinal deformity may be present, often manifesting as vertebral compressions or angular deformities. This can result in curvature of the spine, including kyphosis, sometimes giving the appearance of a “game hump.”
- Widening of Intervertebral Spaces: Infection can cause widening of the intervertebral spaces, resulting in increased separation between the affected vertebrae.
- Abscess Formation: Abscesses may form around infected vertebrae. These abscesses, sometimes called paravertebral abscesses, may be visible on X-rays as opaque areas.
- Soft Tissue Reaction: A reaction of the surrounding soft tissues, such as enlargement of the tissues, may be seen on X-rays. This may be due to inflammation and the immune response to the infection.
- Spinal Fusion: In some advanced cases, there may be fusion of the affected vertebrae, resulting in loss of mobility in the spine.
- Intervertebral Disc Erosion: Infection can cause erosion of the intervertebral disc, changing the height of the disc and contributing to spinal deformities.
Reference
- Tuli SM. Historical aspects of Pott’s disease (spinal tuberculosis) management. Eur Spine J. 2013 Jun; 22 Suppl 4 :529-38. [ PMC free article ] [ PubMed ]
- Dobson J. Percivall Pott. Ann R Coll Surg Engl. 1972 Jan; 50 (1):54-65. [ PMC free article ] [ PubMed ]
- Oettinger T, Jørgensen M, Ladefoged A, Hasløv K, Andersen P. Development of the Mycobacterium bovis BCG vaccine: review of the historical and biochemical evidence for a genealogical tree. Tuber Lung Dis. 1999; 79 (4):243-50. [ PubMed ]
- McLain RF, Isada C. Spinal tuberculosis deserves a place on the radar screen. Cleve Clin J Med. 2004 Jul; 71 (7):537-9, 543-9. [ PubMed ]
- Arockiaraj J, Karthik R, Michael JS, Amritanand R, David KS, Krishnan V, Sundararaj GD. ‘Need of the Hour’: Early Diagnosis and Management of Multidrug Resistant Tuberculosis of the Spine: An Analysis of 30 Patients from a “High Multidrug Resistant Tuberculosis Burden” Country. Asian Spine J. 2019 Apr; 13 (2):265-271. [ PMC free article ] [ PubMed ]
- Rajasekaran S, Soundararajan DCR, Shetty AP, Kanna RM. Spinal Tuberculosis: Current Concepts. Global Spine J. 2018 Dec; 8 (4 Suppl):96S-108S. [ PMC free article ] [ PubMed ]
- Shetty AP, Viswanathan VK, Kanna RM, Shanmuganathan R. Tubercular spondylodiscitis in elderly is a more severe disease: a report of 66 consecutive patients. Eur Spine J. 2017 Dec; 26 (12):3178-3186. [ PubMed ]
- Jain AK, Dhammi IK. Tuberculosis of the spine: a review. Clin Orthop Relat Res. 2007 Jul; 460 :39-49. [ PubMed ]
- Rasouli MR, Mirkoohi M, Vaccaro AR, Yarandi KK, Rahimi-Movaghar V. Spinal tuberculosis: diagnosis and management. Asian Spine J. 2012 Dec; 6 (4):294-308. [ PMC free article ] [ PubMed ]
- Jain AK. Tuberculosis of spine: Research evidence to treatment guidelines. Indian J Orthop. 2016 Jan-Feb; 50 (1):3-9. [ PMC free article ] [ PubMed ]