Introduction
Metatarsal fractures are a frequent problem in the field of trauma and medical emergencies. These fractures, which usually occur as a result of direct trauma to the forefoot, represent one of the most common foot injuries. To better understand this medical condition, let us explore in detail the etiological, clinical, diagnostic aspects, and available treatment options.
Etiology of Metatarsal Fractures
Metatarsal fractures can result from various traumatic mechanisms, whether direct or indirect. Direct trauma often occurs following heavy objects falling on the foot, which is frequently observed in industrial workers. Conversely, indirect trauma occurs when there is a twisting movement of the hindfoot and leg, while the forefoot remains fixed. Supination injuries of the foot can lead to avulsion fractures of the base of the fifth metatarsal due to the tension generated on the peroneus brevis tendon and the lateral cord of the plantar aponeurosis.
Additionally, metatarsal fractures can also be caused by stress fractures, resulting from a small amount of repeated force. These stress fractures are commonly seen in ballet dancers, athletes, and soldiers, sometimes earning them the term “walking fractures.” Other associated risk factors include overload syndrome, Morton’s foot, anorexia nervosa, amenorrhea, and prolonged hypoestrogenism.
Metatarsal fractures can also manifest as insufficiency fractures, which occur due to normal loading on a weakened bone. These injuries are commonly seen in patients with osteoporosis and postmenopausal women.
The etiology of metatarsal fractures, which are common foot injuries, is diverse and often linked to traumatic mechanisms. Understanding the underlying causes of these fractures is essential to guide treatment and prevent future injuries. Here is a detailed exploration of the etiology of metatarsal fractures:
List of causes
- Direct Trauma: Metatarsal fractures frequently occur following direct trauma, mainly impacts or falls of heavy objects on the foot. This form of trauma is often seen in industrial environments where accidents can occur, resulting in isolated or multiple metatarsal fractures.
- Indirect Trauma: Twisting movements of the hindfoot and leg, combined with a fixed forefoot, can cause metatarsal fractures through indirect trauma. This especially occurs during inappropriate movements or twisting of the foot, causing excessive stress on the metatarsal bones.
- Supination Fractures: Supination injuries of the foot can lead to avulsion fractures of the base of the fifth metatarsal. This is often due to the tension generated on the peroneus brevis tendon and the lateral cord of the plantar aponeurosis during this type of movement.
- Stress Fractures: Stress fractures result from continuous repetition of low force on the metatarsals. They are commonly seen in specific populations, including ballet dancers, athletes, and military personnel. These stress fractures may be associated with activities involving repetitive loading on the foot.
- Insufficiency Fractures: Insufficiency fractures occur due to normal loading on an already weakened bone. They are more common in people with osteoporosis or in postmenopausal women, where bone density is reduced.
- Lisfranc Fractures: Lisfranc fractures, involving the tarsometatarsal joints, can occur when falling from a height or down stairs. These fractures often result from longitudinal compressive forces or rotations around a fixed forefoot.
- Walking Fractures: Walking fractures, a variety of stress fractures, are associated with a low amount of repetitive force. They are commonly seen in individuals exposed to activities requiring prolonged walking, such as marching soldiers.
- Insufficiency Fractures in the Elderly: Older adults, particularly those with osteoporosis, may experience metatarsal insufficiency fractures due to normal loading on a weakened bone.
- Additional Risk Factors: Certain risk factors, such as overload syndrome, Morton foot, anorexia nervosa, amenorrhea, and prolonged hypoestrogenism, may contribute to the development of metatarsal fractures.
- Metatarsal Fractures in Children: In children, metatarsal fractures are often linked to play activities, games or falls during play. The distribution of metatarsal fractures in children may differ from that in adults, with a higher prevalence at the fifth metatarsal.
- Crush Fractures: Metatarsal fractures can also result from crush injuries, where significant force is applied to the foot. This can happen in road accidents, industrial accidents or incidents of a traumatic nature.
- Iatrogenic Fractures: In some cases, metatarsal fractures can be induced by medical interventions, such as inappropriate manipulation, surgical procedures, or orthopedic procedures. These iatrogenic fractures can occur as a complication of previous treatments.
- Genetic Factors: Although less common, some cases of metatarsal fractures may be linked to predisposing genetic factors. Genetic conditions that affect bone density or bone strength may contribute to fractures occurring more easily.
- Concomitant Injuries: Metatarsal fractures can often coexist with other foot injuries, such as sprains, ankle fractures, or soft tissue injuries. These concomitant lesions can complicate the diagnosis and management.
- Anatomical Defects: Some individuals may have pre-existing anatomical abnormalities, such as accessory bones (os vesalianum, os peroneum) or anatomical variations. These anatomical defects may increase susceptibility to metatarsal fractures.
- Repetitive Fractures in Athletes: Athletes playing high-impact sports, such as basketball or soccer, may be prone to repetitive fractures of the metatarsals. Repetition of movements can cause excessive strain on the bones, increasing the risk of fractures.
- Hormonal Factors in Women: In women, hormonal changes related to menstruation, pregnancy or menopause can influence bone density and bone strength. These hormonal variations may contribute to the predisposition to metatarsal fractures.
- Poor Environmental Conditions: Environmental conditions, such as uneven surfaces, inappropriate footwear, or uneven terrain, can increase the risk of falls and trauma, contributing to metatarsal fractures.
- Crush Fractures: Metatarsal fractures can also result from crush injuries, where significant force is applied to the foot. This can happen in road accidents, industrial accidents or incidents of a traumatic nature.
- Iatrogenic Fractures: In some cases, metatarsal fractures can be induced by medical interventions, such as inappropriate manipulation, surgical procedures, or orthopedic procedures. These iatrogenic fractures can occur as a complication of previous treatments.
- Genetic Factors: Although less common, some cases of metatarsal fractures may be linked to predisposing genetic factors. Genetic conditions that affect bone density or bone strength may contribute to fractures occurring more easily.
- Concomitant Injuries: Metatarsal fractures can often coexist with other foot injuries, such as sprains, ankle fractures, or soft tissue injuries. These concomitant lesions can complicate the diagnosis and management.
- Anatomical Defects: Some individuals may have pre-existing anatomical abnormalities, such as accessory bones (os vesalianum, os peroneum) or anatomical variations. These anatomical defects may increase susceptibility to metatarsal fractures.
- Repetitive Fractures in Athletes: Athletes playing high-impact sports, such as basketball or soccer, may be prone to repetitive fractures of the metatarsals. Repetition of movements can cause excessive strain on the bones, increasing the risk of fractures.
- Hormonal Factors in Women: In women, hormonal changes related to menstruation, pregnancy or menopause can influence bone density and bone strength. These hormonal variations may contribute to the predisposition to metatarsal fractures.
- Poor Environmental Conditions: Environmental conditions, such as uneven surfaces, inappropriate footwear, or uneven terrain, can increase the risk of falls and trauma, contributing to metatarsal fractures.
- Pathological Metatarsal Fractures: Certain pre-existing medical conditions, such as metabolic bone disorders, bone tumors or bone infections, can contribute to pathological metatarsal fractures. These fractures can result from bone fragility induced by underlying diseases.
- Metatarsal Fractures in Professional Athletes: Professional athletes, due to the intensive nature of their training and participation in high-level competitions, are more likely to develop metatarsal fractures. Repetitive stress on the foot can lead to cumulative microtrauma.
- Fall-Related Metatarsal Fractures: Accidental falls, whether at home, on slippery surfaces, or in outdoor environments, can cause metatarsal fractures. The force of impact during the fall can cause injury to the bones of the foot.
- Metatarsal Fractures in the Elderly: Older people, due to bone fragility linked to aging, may be more prone to metatarsal fractures. Falls from short heights can cause fractures due to reduced bone density in this population.
- Metatarsal Fractures Induced by Osteopathic Stress: Biomechanical imbalances or gait abnormalities can induce metatarsal fractures by osteopathic stress. Excessive stresses placed on the metatarsals can cause repetitive strain injuries, eventually leading to fractures.
- Psychosomatic Metatarsal Fractures: In some cases, psychological or emotional factors may contribute to metatarsal fractures. Studies suggest that emotional stress can influence bone density, increasing the risk of fractures.
- Metatarsal Fractures In Overweight People: Excess weight puts additional pressure on the bones of the foot, increasing the risk of metatarsal fractures. Overweight people may be more likely to develop fractures from increased load on the lower extremities.
- Metatarsal Fractures Associated with Recreational Activities: Recreational activities such as jumping, running, or other high-impact sports may be associated with metatarsal fractures. Sudden, repetitive movements during these activities can cause excessive stress on the bones of the foot.
- Metatarsal Fractures in Construction Workers: Construction workers, exposed to the risk of falling heavy objects and demanding working conditions, may be more prone to metatarsal fractures. Accidents in the workplace are a common source of injuries.
- Metatarsal Fractures in Professional Dancers: Professional dancers, due to the complex movements and physical demands of their profession, can develop metatarsal fractures. Repetitive loading on the feet during dancing can contribute to these injuries.
- Metatarsal Fractures Related to Sports Equipment: Inappropriate athletic shoes, faulty equipment or inadequate playing surfaces can increase the risk of metatarsal fractures in sports enthusiasts. Unsuitable environmental conditions and equipment can contribute to injuries.
- Metatarsal Fractures Related to Outdoor Activities: Outdoor activities, such as hiking or climbing, can expose individuals to difficult terrain and the risk of falls, leading to metatarsal fractures. Exposure to outdoor environments may be a contributing factor.
Clinical Presentation
Let’s take a closer look at the clinical presentation of metatarsal fractures, a common injury that can cause significant symptoms. These fractures, often caused by direct trauma such as falls, impacts, or excessive forces to the foot, have distinct clinical features.
Pain is one of the most predominant symptoms of metatarsal fractures. Affected individuals usually experience sharp pain at the time of the traumatic incident, localized to the affected foot region. This pain can be exacerbated when walking or any activity that involves pressure on the foot. The nature of the pain may vary depending on the severity of the fracture and whether there is bone displacement.
Another key component of the clinical presentation is swelling. In response to the injury, an inflammatory reaction occurs, leading to edema around the fractured area. This swelling, combined with local redness, contributes to the characteristic appearance of inflammation and can be observed visually.
Foot deformity is also a potential sign of metatarsal fracture. If the fracture causes the bones to shift, an abnormal protrusion or noticeable change in the shape of the foot may occur. This may be particularly evident upon visual inspection and is an important indicator of the severity of the fracture.
The appearance of a hematoma is also common. The rupture of small blood vessels can cause a collection of blood to form around the fractured area, contributing to skin discoloration. This reddish or bluish coloration, associated with the hematoma, is often visible and constitutes an additional element of the clinical presentation.
Difficulty walking is a major functional symptom of metatarsal fractures. Due to severe pain, swelling, and possibly displacement of bones, affected individuals may have difficulty bearing weight on the affected foot. This frequently leads to a characteristic limp and may require the use of crutches to relieve pressure on the injured area.
Sensitivity to touch is also a notable aspect of the clinical presentation. The area of the metatarsal fracture may be particularly tender to touch, which can be assessed by a healthcare professional during the physical exam. This sensitivity can help precisely locate the area of injury.
List of clinical présentation
- Foot Pain: Pain is often the predominant symptom in patients with a metatarsal fracture. The location of the pain depends on which metatarsal is affected, but it is usually felt in the forefoot. The pain may be sharp, stabbing, or aching, made worse by pressure or weight bearing on the foot.
- Swelling and Edema: Significant swelling and edema in the affected area is commonly observed. This may be the result of an inflammatory response to the injury. The foot may appear swollen, warm to the touch, and have a noticeable change in volume.
- Difficulty Walking or Pressing Foot: Due to severe pain and swelling, patients may experience difficulty walking or putting weight on the affected foot. Weight bearing on the fractured metatarsal can increase pain, leading to lameness or an inability to walk normally.
- Tenderness and Tenderness on Palpation: During physical examination, local tenderness and tenderness on palpation may be noted at the site of the metatarsal fracture. The specific areas of tenderness will depend on the metatarsal affected and the nature of the fracture.
- Visible Deformation (in Severe Cases): In cases of severe fractures, visible deformation may be observed, including deviations or deformities of the toes. This may indicate a complex fracture or associated dislocation requiring further evaluation.
- Bruising (in Some Cases): Bruising may develop around the area of the metatarsal fracture due to the rupture of small blood vessels during the injury. The presence of bruising may vary depending on the severity of the injury.
- Crepitation (in Some Cases): Crepitation, a rubbing or grinding sensation under the skin, can sometimes be noticeable when bone fragments move. This can be detected by a healthcare professional during the clinical examination.
- Gait Alterations: Due to pain and functional limitations, patients may experience gait alterations, such as lameness or reluctance to weight-bear the foot. These alterations can be observed when observing the patient’s gait.
- Symptoms Associated with Complications: In cases of complications such as infections, poor healing, or nerve damage, additional symptoms such as fever, drainage of pus, or numbness may occur.
- Difficulty Putting On Shoes: Patients may report difficulty putting on shoes due to pain and swelling. Some may notice that their regular shoes become uncomfortable due to the associated deformation.
- Foot Pain: Pain is often the predominant symptom in patients with a metatarsal fracture. The location of the pain depends on which metatarsal is affected, but it is usually felt in the forefoot. The pain may be sharp, stabbing, or aching, made worse by pressure or weight bearing on the foot.
- Swelling and Edema: Significant swelling and edema in the affected area is commonly observed. This may be the result of an inflammatory response to the injury. The foot may appear swollen, warm to the touch, and have a noticeable change in volume.
- Difficulty Walking or Pressing Foot: Due to severe pain and swelling, patients may experience difficulty walking or putting weight on the affected foot. Weight bearing on the fractured metatarsal can increase pain, leading to lameness or an inability to walk normally.
- Tenderness and Tenderness on Palpation: During physical examination, local tenderness and tenderness on palpation may be noted at the site of the metatarsal fracture. The specific areas of tenderness will depend on the metatarsal affected and the nature of the fracture.
- Visible Deformation (in Severe Cases): In cases of severe fractures, visible deformation may be observed, including deviations or deformities of the toes. This may indicate a complex fracture or associated dislocation requiring further evaluation.
- Bruising (in Some Cases): Bruising may develop around the area of the metatarsal fracture due to the rupture of small blood vessels during the injury. The presence of bruising may vary depending on the severity of the injury.
- Crepitation (in Some Cases): Crepitation, a rubbing or grinding sensation under the skin, can sometimes be noticeable when bone fragments move. This can be detected by a healthcare professional during the clinical examination.
- Gait Alterations: Due to pain and functional limitations, patients may experience gait alterations, such as lameness or reluctance to weight-bear the foot. These alterations can be observed when observing the patient’s gait.
- Symptoms Associated with Complications: In cases of complications such as infections, poor healing, or nerve damage, additional symptoms such as fever, drainage of pus, or numbness may occur.
- Difficulty Putting On Shoes: Patients may report difficulty putting on shoes due to pain and swelling. Some may notice that their regular shoes become uncomfortable due to the associated deformation.
- Neurological Symptoms: In some cases, neurological symptoms may accompany metatarsal fractures, particularly when nerve damage is involved. This may manifest as tingling, numbness, or decreased sensitivity in the affected area.
- Worsening Pressure Pain: Pain may be exacerbated when putting pressure on the fracture area, whether by walking, standing, or applying direct pressure to the affected metatarsal. This can help differentiate pain from a fracture from other conditions.
- Pain Reference: Pain can sometimes radiate to other parts of the foot or even to the leg. This can complicate the diagnosis because the source of the pain may be felt distant from the fracture. Careful assessment is necessary to precisely locate the source of the pain.
- Joint Stiffness: Joint stiffness may develop around the fractured area, limiting the range of motion in the foot. This may be especially noticeable in the morning or after prolonged periods of rest.
- Functional Disability: In cases of severe or complex fractures, significant functional disability may be present. Patients may have difficulty performing simple foot movements, such as flexion, extension, or rotation.
- Continuous Inflammation: Persistent inflammation at the fractured area may be observed, even after a few days of injury. This may indicate an ongoing inflammatory response and highlight the need for appropriate management.
- Sensation of Local Warmth: A sensation of local warmth around the fracture may be felt due to the associated inflammation. This can be assessed during physical examination by palpation of the temperature of the skin over the fracture.
- Foot Instability: Metatarsal fractures, especially those involving adjacent joints, can cause some instability of the foot. This may manifest as feeling weak or unsteady while walking.
- Psychological Reactions: The presence of a metatarsal fracture can cause psychological reactions such as anxiety, frustration or even depression, due to the limitations imposed on daily activities and mobility.
- Change in Arch of the Foot: In cases of severe metatarsal fractures, a change in the normal arch of the foot may be observed. This may be noticeable visually and may require radiological evaluation to determine the extent of the deformity.
- Impact on Quality of Life: Metatarsal fractures can have a significant impact on the patient’s quality of life, affecting their ability to work, participate in social activities and maintain an active lifestyle. These aspects must be taken into account in the overall management of the injury.
- Response to Mobilization: When trying to mobilize the foot, patients may report increased pain or discomfort. This can help assess fracture stability and determine the best treatment approaches.
Assessment and Diagnosis
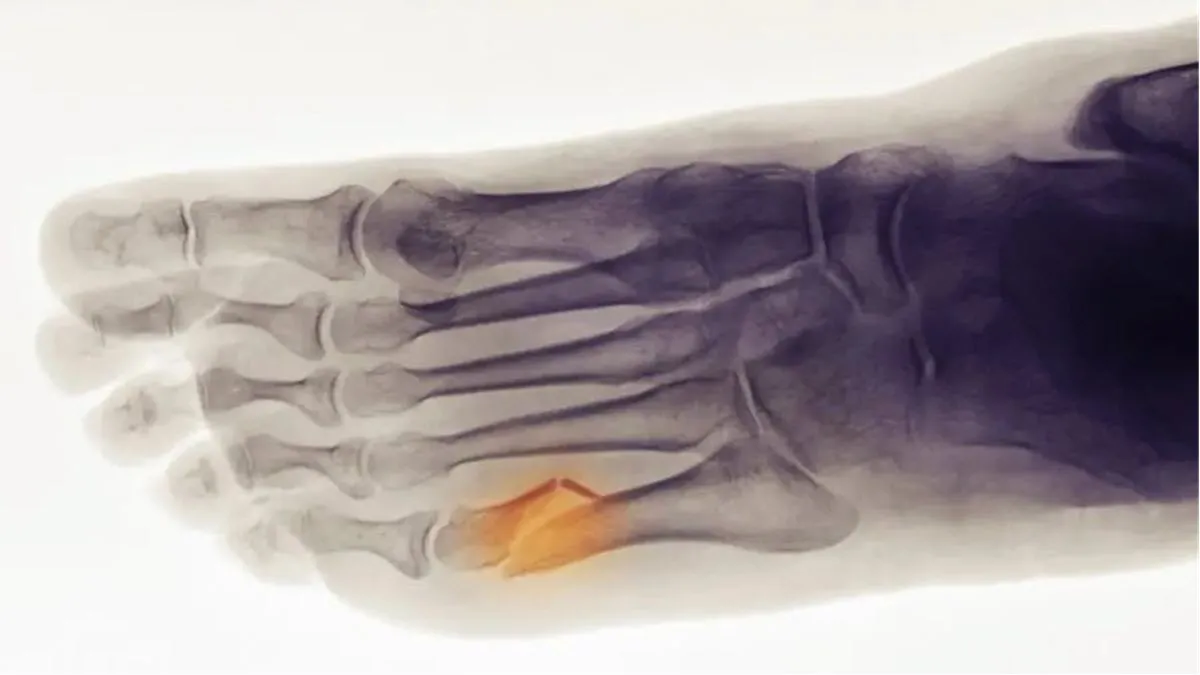
Radiographic evaluation plays a crucial role in the diagnosis of metatarsal fractures. Standard views of the foot, including an anteroposterior view, a 45-degree oblique view, and a lateral projection, are usually performed. To diagnose stress fractures, weight-bearing radiographs, including a lateral view of the foot and a tangential view of the metatarsal heads, may be helpful.
In some cases, acute stress fractures are not detected with a standard x-ray. To confirm the diagnosis, x-rays may be repeated after 10 to 14 days from the start of symptoms. Advanced imaging techniques such as MRI and technetium scans can also be used due to their high sensitivity to detect such fractures.
List of assessment
- In-Depth Questioning:
- Take a detailed history to understand the circumstances of the injury, mechanism of trauma and initial symptoms.
- Explore the patient’s medical history, including pre-existing bone problems, metabolic diseases, and lifestyle habits.
- Physical examination :
- Assess pain by palpating the affected metatarsal region and observing the patient’s reactions during mobilization.
- Look for signs of inflammation, bruising, visible deformity, and gait alterations.
- Test joint stability and assess range of motion of the foot.
- Neurovasc
- Check blood circulation by assessing distal pulses and skin color.
- Assess nerve sensitivity and reflexes to identify possible associated nerve damage.
- Radiological examinations:
- Radiographs, including anteroposterior, 45-degree oblique, and lateral views, are essential to confirm the diagnosis, locate the fracture, and assess its severity.
- Additional studies, such as CT scans or MRIs, may be needed for complex cases or when complications are suspected.
- Fracture Classification:
- Classify the fracture according to its location (head, neck, diaphysis, base) and its severity (simple, comminuted, open).
- Identify fractures associated with adjacent joints, such as Lisfranc fracture.
- Assessment of Complications:
- Look for signs of infections, displaced bone fragments, nerve damage, and other potential complications.
- Assess the stability of joints and bone fragments to determine the need for surgical intervention.
- Specialized Consultation:
- In case of neurovascular complications, complex fractures, or injuries requiring specific management, consult specialists such as orthopedic surgeons, neurologists or interventional radiologists.
- Functional Assessment:
- Assess the functional impact of the fracture on the patient’s ability to perform daily activities.
- Observe mobility limitations and gait alterations.
- Psychosocial Assessment:
- Consider the emotional and psychological impact of the fracture on the patient.
- Identify psychosocial support needs and refer to mental health professionals if necessary.
- Assessment of Bone Healing:
- Monitor the progress of bone healing using follow-up x-rays.
- Adapt the treatment plan according to the progress of healing.
- Assessment of
- Monitor the patient’s tolerance to the prescribed treatment, whether conservative or surgical.
- Adjust medications and treatment modalities based on patient responses.
Classification and Epidemiology
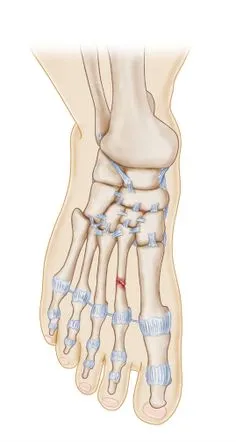
Metatarsal fractures are classified according to their topographical location, including head fractures, subcapital fractures, shaft fractures, and base fractures. The frequency of metatarsal fractures is approximately ten times higher than that of Lisfranc fracture-dislocations.
Children also have a significant prevalence of metatarsal fractures, accounting for 61% of all foot fractures in this population. The fifth metatarsal is most commonly fractured, followed by the third metatarsal in industrial injuries.
The classification and epidemiology of metatarsal fractures provide crucial information for understanding the prevalence, severity, and specific characteristics of these injuries. Here is a detailed analysis of the classification and epidemiology associated with metatarsal fractures:
Classification of Metatarsal Fractures
Metatarsal fractures can be classified based on their specific location and the nature of the injury. Here is a general classification based on these criteria:
Emplacement
- Metatarsal Head: Fractures at the most distal parts of the metatarsal bones.
- Metatarsal Neck: Fractures located in the middle part of the metatarsals, often associated with stress injuries.
- Metatarsal Shaft: Fractures involving the long, straight part of the metatarsal bones.
- Base Metatarsal: Fractures at the proximal parts of the metatarsal bones.
Nature of the Fracture
- Simple: Fracture without significant displacement of bone fragments.
- Comminuted: Fracture with several bone fragments.
- Open: Fracture with a skin wound, increasing the risk of infection.
- Stress: Fracture resulting from repeated stress on the bone, often seen in athletes.
Associations with Adjacent Joints
- Lisfranc fracture: Involvement of the tarsometatarsal joints, often associated with serious injuries.
- Classification de Lisfranc :
- Homolateral: Lateral displacement of the metatarsals without alteration of the first metatarsophalangeal joint.
- Divergent: Lateral displacement of the metatarsals with alteration of the first metatarsophalangeal joint.
Epidemiology of Metatarsal Fractures
The epidemiology of metatarsal fractures provides data on the frequency, demographic distribution and risk factors associated with these injuries:
- High Prevalence:
- Metatarsal fractures represent one of the most common foot injuries, with a high incidence in the general population.
- Pediatric Population:
- Children and adolescents: Metatarsal fractures represent approximately 61% of all foot fractures in children, with a predominance at the fifth metatarsal.
- Adults Youth and Athletes:
- Athletes, particularly dancers, ballet athletes, and military personnel, are at increased risk of metatarsal fractures, particularly stress fractures.
- Older Adults:
- Metatarsal fractures in older adults are sometimes associated with osteoporosis, with an increased risk of insufficiency fractures.
- Lateral Distribution of Fractures:
- The fifth metatarsal is most commonly affected, accounting for approximately 23% of all metatarsal fractures. The first metatarsal is also often involved.
- Gender:
- Some studies suggest a slight female predominance in the incidence of metatarsal fractures.
- Traumatic Events and Risk Factors:
- Common causes include direct trauma, falling heavy objects, twisting movements of the foot, and repeated sports injuries.
- Stress Injuries:
- Metatarsal stress fractures are common among athletes involved in high-impact activities, such as running.
- Lisfranc Fractures:
- Less common than isolated metatarsal fractures, Lisfranc fractures are often associated with serious trauma and falls from height.
Analysis of the classification and epidemiology of metatarsal fractures provides an essential basis for the management and prevention of these common foot injuries. Understanding risk factors and demographic characteristics helps tailor treatment approaches and implement appropriate preventive measures.
Jones fracture
A Jones fracture generally refers to a “fifth metatarsal fracture.” The fifth metatarsal is the bone on the outside of the foot, connected to the little toe. This fracture is often called a Jones fracture after Sir Robert Jones, an early 20th century orthopedic surgeon who described this injury.
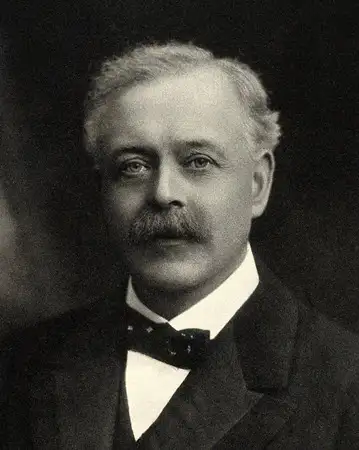
Jones fracture can occur due to excessive strain on the fifth metatarsal, often as a result of sudden twisting of the foot. It can also result from a stress fracture due to overuse or repetition of activities, such as running.
Treatment for Jones fracture depends on the severity of the injury. It may include rest, immobilization with a splint or boot, and sometimes surgery, particularly if the fracture is not healing properly.
It is important to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan if you suspect a Jones fracture or experience persistent pain in your foot.
Radiographic signs
Radiographic signs of metatarsal fractures play a crucial role in diagnosis, classification and treatment planning. Radiographic imaging allows detailed visualization of the metatarsal bones, fractured fragments and possible complications. Here are the main radiographic signs to consider when evaluating metatarsal fractures:
- Visible Fractures:
- Anteroposterior, 45-degree oblique, and lateral radiographs provide a complete view of the metatarsal bones, allowing detection of obvious fractures.
- Movement of Bone Fragments:
- X-rays reveal the degree of displacement of the bone fragments. Significant displacement may require surgery to restore alignment.
- Comminution :
- Comminution, characterized by the presence of several bone fragments, is clearly visible on x-rays. Comminution may influence the choice of treatment.
- Skin Opening (Open Fracture):
- X-rays may show a skin opening associated with a compound fracture, indicating the need for special attention due to the risk of infection.
- Fracture Line:
- The fracture line is often visible on x-rays and can indicate the direction of the traumatic force. It is crucial for the classification of the fracture.
- Stress Fractures:
- Stress fractures may not be immediately visible on standard x-rays. Radiographic signs of stress fractures include fine fracture lines and areas of bone resorption.
- Assessment of Adjacent Joints:
- Radiographs are used to assess the involvement of adjacent joints, particularly in the case of Lisfranc fractures, which may require a specific surgical approach.
- Assessment of Bone Healing:
- Follow-up x-rays help monitor bone healing. Proper consolidation is essential to avoid long-term complications.
- Advanced Imaging (CT, MRI):
- In some cases, advanced imaging, such as computed tomography (CT) or magnetic resonance imaging (MRI), may be necessary for more detailed evaluation, particularly for complex fractures or when tissue damage is suspected. soft.
- Anatomical Anomalies:
- X-rays can also reveal pre-existing anatomical abnormalities, such as accessory bones, which can influence the treatment plan.


Conclusion
In conclusion, metatarsal fractures represent frequent injuries, mainly affecting the foot, and can have significant consequences on the mobility and quality of life of individuals. Their appropriate assessment, classification and management are essential to ensure optimal patient recovery. Here are some key points to remember:
- Diversity of Fractures: Metatarsal fractures can vary in location, nature and severity. Their precise classification guides medical management, whether for isolated fractures, stress fractures in athletes, or complex fractures involving adjacent joints, such as the Lisfranc fracture.
- Varied Epidemiology: These fractures have a high prevalence, affecting diverse populations, from children to the elderly, with increased risks in athletes and individuals exposed to repeated trauma. Understanding the epidemiology helps target preventive measures and appropriate interventions.
- Multidisciplinary Management: Management of metatarsal fractures requires a multidisciplinary approach, involving orthopedists, radiologists, physiotherapists and, in some cases, sports medicine specialists. A comprehensive evaluation, including thorough clinical examinations and radiological analyses, is crucial for an accurate diagnosis.
- Varied Treatment Options: Treatment may vary from conservative management with immobilization to surgery depending on the nature of the fracture, its location and the presence of complications. Continued monitoring of bone healing, symptoms, and functionality guides adjustment of treatment modalities.
- Psychosocial Impact: Metatarsal fractures can have significant psychological repercussions due to mobility limitations and disruptions to daily life. Taking these aspects into account contributes to a holistic approach to the patient.
Questionnaire 1
Questions :
- What is the most common mechanism of trauma associated with metatarsal fractures?
a) Hindfoot twist
b) Foot compression
c) Fall on toes
d) Plantar flexion movement
e) Direct strike by a heavy object - What term is sometimes used to describe metatarsal fractures in ballet dancers and military personnel?
a) Walking fractures
b) Dancing fractures
c) Sprinting fractures
d) Loading fractures
e) Rotation fractures - What risk factor is associated with metatarsal fractures in people with osteoporosis?
a) High blood pressure
b) Overload syndrome
c) Anorexia nervosa
d) Estrogen excess
e) Vitamin D deficiency - How can metatarsal stress fractures that are not immediately visible on standard x-rays be diagnosed?
a) Ultrasound
b) MRI
c) Computed tomography (CT)
d) Weighted x-rays
e) Blood tests - Which characteristic is associated with a serious metatarsal fracture requiring further evaluation?
a) Acute pain
b) Moderate swelling
c) Visible deformity
d) Mild tenderness
e) Minor bruising - Which metatarsal is most commonly affected by fractures in children?
a) First metatarsal
b) Second metatarsal
c) Third metatarsal
d) Fourth metatarsal
e) Fifth metatarsal - What is the most appropriate imaging method to evaluate complex metatarsal fractures?
a) Standard X-ray
b) MRI
c) Ultrasound
d) Computed tomography (CT)
e) Weighted X-ray - Which symptom may be associated with complications such as infections or nerve damage in the context of metatarsal fractures?
a) Fever
b) Fatigue
c) Chills
d) Night sweats
e) Persistent cough - What is the prevalence of metatarsal fractures in children compared to all foot fractures?
a) About 10%
b) About 25%
c) About 50%
d) About 61%
e) About 75% - What is the main psychosocial consequence of metatarsal fractures?
a) Anxiety
b) Depression
c) Social isolation
d) Reduction in mobility
e) Impact on quality of life
Answers:
- e) Direct strike by a heavy object
- a) Walking fractures
- c) Anorexia nervosa
- d) X-rays with weights
- c) Visible deformation
- e) Fifth metatarsal
- b) IRM
- a) Fever
- d) About 61%
- e) Impact on quality of life
Questionnaire 2
Questions :
- What is the most common mechanism leading to metatarsal fractures?
a) Compression
b) Twist
c) Extension
d) Flexion
e) Rotation - Which category of people are at increased risk of metatarsal fractures due to high-impact activities?
a) Swimmers
b) Cyclists
c) Dancers
d) Walkers
e) Gardeners - Which metatarsal is most commonly affected by stress fractures?
a) First metatarsal
b) Second metatarsal
c) Third metatarsal
d) Fourth metatarsal
e) Fifth metatarsal - What type of metatarsal fracture is often associated with falling heavy objects on the foot?
a) Open fracture
b) Comminuated fracture
c) Stress fracture
d) Insufficiency fracture
e) Simple fracture - Which imaging method is particularly useful for assessing bone healing over time?
a) Standard X-ray
b) MRI
c) Computed tomography (CT)
d) Ultrasound
e) Weighted X-ray - What risk factor is specifically associated with metatarsal fractures in older adults?
a) Excessive exercise
b) Osteoporosis
c) Intense sports practice
d) Unbalanced diet
e) Smoking - What potential complication of metatarsal fractures may require surgery?
a) Swelling
b) Simple fracture
c) Infection
d) Stress fracture
e) Minor deformity - What is the main clinical feature associated with metatarsal fractures?
a) Fever
b) Swelling
c) Poor vision
d) Abdominal pain
e) Hearing loss - What is the anatomical area most frequently affected by metatarsal fractures?
a) Metatarsal head
b) Metatarsal neck
c) Metatarsal shaft
d) Metatarsal base
e) Metatarsophalangeal joint - Which metatarsal is often involved in Lisfranc fractures?
a) First metatarsal
b) Second metatarsal
c) Third metatarsal
d) Fourth metatarsal
e) Fifth metatarsal
Answers:
- a) Compression
- c) Dancers
- e) Fifth metatarsal
- e) Fracture simple
- a) Standard radiography
- b) Osteoporosis
- c) Infection
- b) Swelling
- a) Metatarsal head
- b) Second metatarsal