Introduction to Medial Epicondylitis (Golfer’s Elbow)
Medial elbow epicondylitis, also known as medial elbow tendinopathy or golfer’s elbow, is a painful condition characterized by inflammation or irritation of the tendons inside the elbow. The pain is located on the inner side of the elbow, near the medial epicondyle, the bone located on the inside of the elbow. Unlike lateral epicondylitis, also called tennis elbow, which affects the outer part of the elbow, internal epicondylitis is less common.
Although the popular term “golfer’s elbow” may suggest that this condition only affects golfers, it is crucial to understand that various repetitive activities can trigger this condition. Certainly, the golf swing motion is a common cause of medial epicondylitis, but other repetitive actions can also contribute to its development. For example, activities such as throwing objects, cutting wood with an axe, using a chainsaw, and various types of hand tools can also be risk factors.
It is essential to emphasize that any activity using the same muscles of the forearm can potentially be a trigger for internal epicondylitis. People who play sports requiring repetitive elbow movements, such as tennis, baseball, or badminton, as well as those working in industries where repetitive movements are common, such as gardening or construction, are likely to develop this condition. affection.
The pain associated with internal epicondylitis can be bothersome and limiting in daily life. To treat this condition, a well-structured rehabilitation plan is often necessary. It may include phases such as initial rest, pain and inflammation control, muscle strengthening, mobility and flexibility, functional exercises, as well as low-impact cardio activities.
It is also crucial to avoid rushing the recovery process and to follow the advice of a medical professional throughout the process. Rehabilitation after internal epicondylitis must be progressive, personalized and adapted to each individual, taking into account their level of physical condition and daily activities.
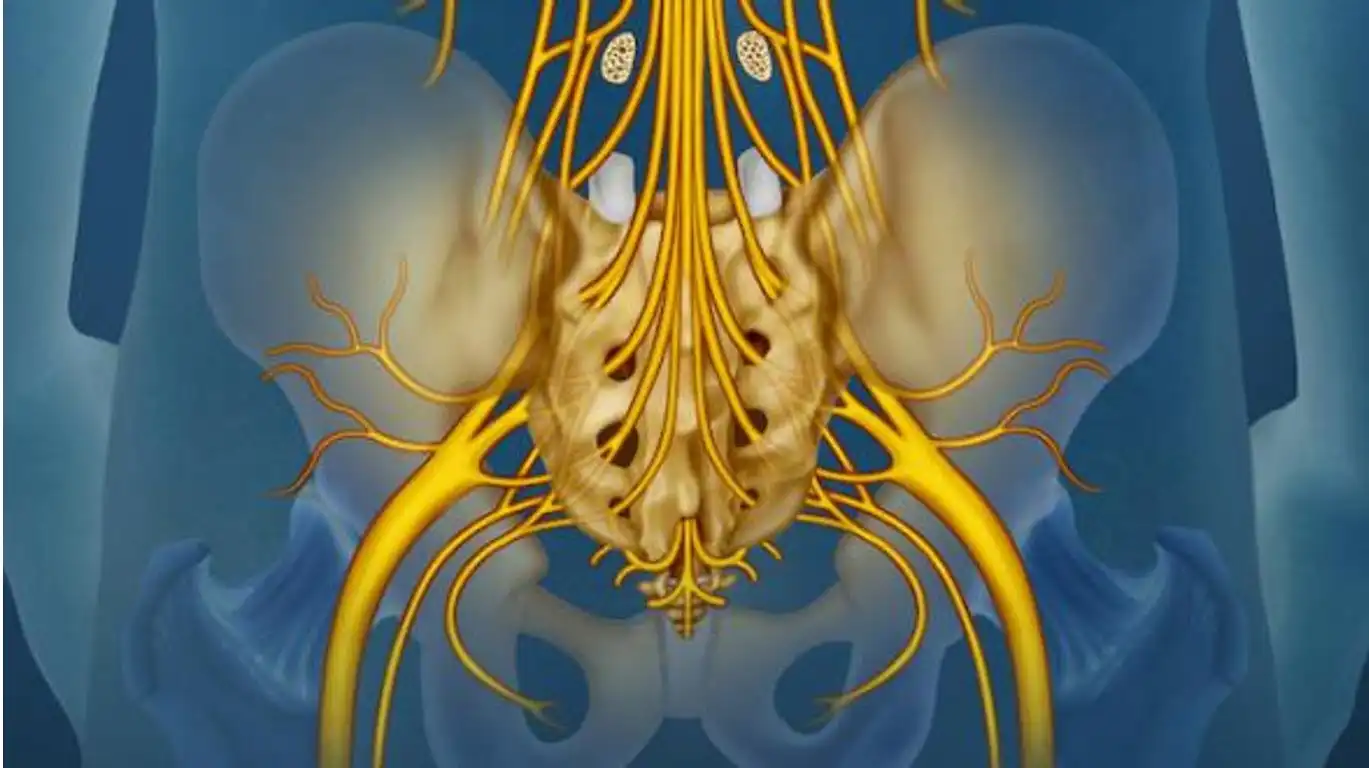
Anatomy of Medial Epicondylitis
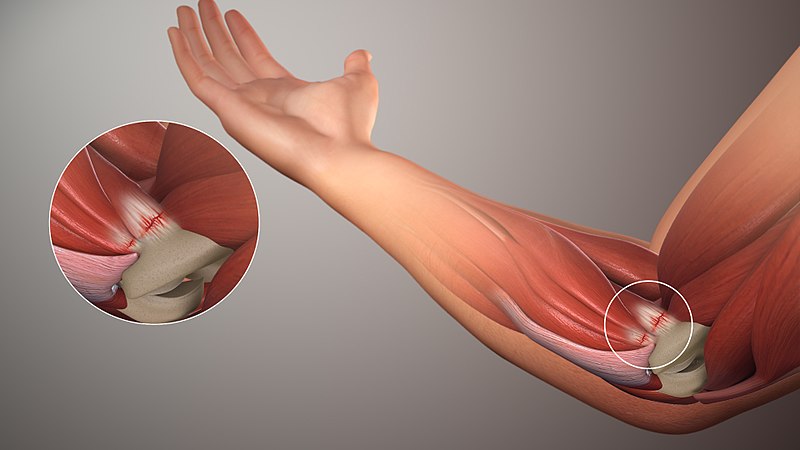
Internal epicondylitis causes pain that originates inside the protuberance of the elbow. The muscles responsible for wrist flexion, located on the palm side of the forearm, are directly related to this condition, attaching firmly to a main tendon connected to the medial epicondyle. These common flexor tendons attach securely to the bone, forming a sturdy structure composed of adjacent bundles of collagen. This arrangement provides high tensile strength, allowing the tendons to withstand considerable forces exerted on both ends of the tendon.
When the muscles contract, they pull on one end of the tendon, creating bone movement. In the case of the wrist flexor muscles, their coordinated contraction is essential for actions such as flexion of the wrist, downward rotation of the forearm, or firm grasping of the hand. These contracted muscles exert traction on the flexor tendon, generating forces that can intensify, for example, when making a golf swing while holding a club tightly, or during any other similar activity that uses these muscles .
Symptoms of internal epicondylitis of the elbow
Medial elbow epicondylitis, also known as tennis elbow, is a painful condition that affects the inner part of the elbow. The symptoms of this condition can be varied and bothersome. Typically, people with medial epicondylitis of the elbow feel sharp, persistent pain on the inside of the elbow, which can radiate down the forearm and even up to the wrist. This pain may be made worse by certain activities, such as bending or rotating the wrist, as well as gripping heavy objects.
Besides pain, other symptoms may accompany medial epicondylitis of the elbow. For example, a feeling of stiffness or tension in the elbow may be present, thereby limiting the mobility of the joint. Some patients also report weakness in their wrist or hand, which can make it difficult to perform simple daily tasks.
In addition to physical symptoms, medial epicondylitis of the elbow can also impact patients’ emotional and mental well-being. Persistent pain and limitation of activities can lead to frustration, anxiety, and even depression in some people, especially if the condition interferes with their work or leisure activities.
Here are the common symptoms associated with this condition:
- Pain on the inside of the elbow: Pain is the main symptom of internal epicondylitis. It is usually located on the inside of the elbow, near the medial epicondyle (the bony protrusion on the inside of the elbow).
- Pain when flexing the wrist and hand: Pain is often exacerbated when flexing the wrist and hand inward. Activities such as gripping objects, rotating the wrist, or playing certain sports can trigger or worsen the pain.
- Pain when shaking your hand: Pain can be felt when gripping objects, handling tools, or even shaking your hand.
- Tenderness to palpation: The area near the medial epicondyle may be tender to touch. By gently pressing this area, the pain can be reproduced.
- Localized swelling: In some cases, there may be slight swelling around the affected area.
- Weakness: Some individuals may experience a feeling of weakness in the affected wrist and hand.
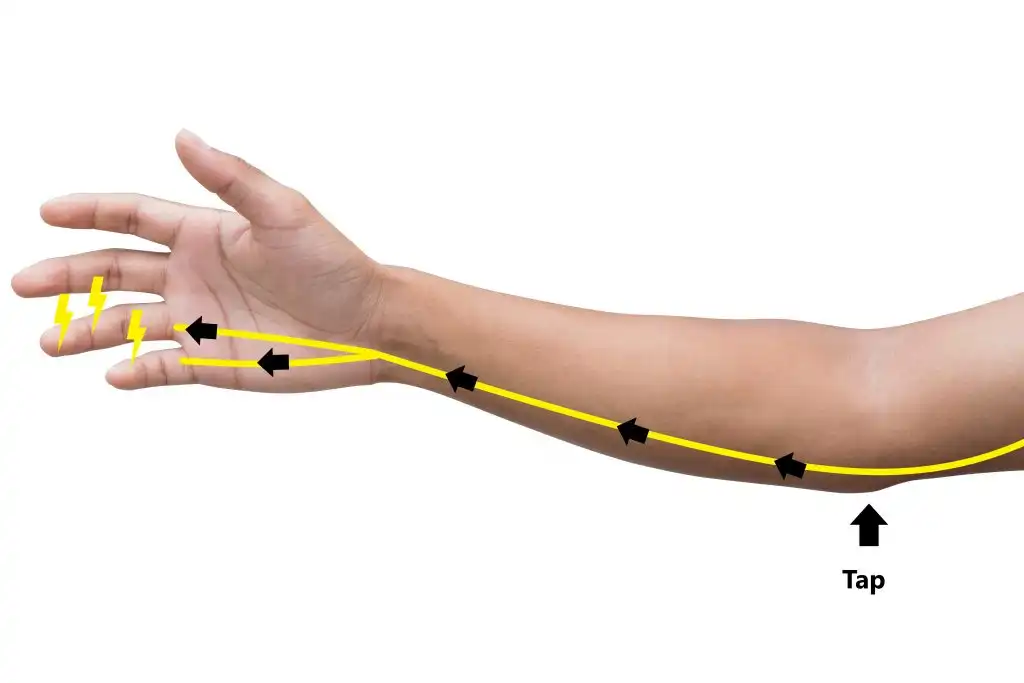
- Numbness or tingling: In some cases, abnormal sensations such as numbness or tingling may be felt along the forearm and fingers.
It is important to note that the severity of symptoms can vary from person to person. In the early stages, the pain may be mild and only present with certain activities. However, if the condition progresses, the pain may become more persistent and further affect daily activities.
Common Causes and Contributing Factors
Medial epicondylitis, also known as tennis elbow or medial epicondylitis, is a painful condition that affects the inner part of the elbow. Unlike external epicondylitis, which is more commonly associated with tennis, internal epicondylitis is usually caused by repetitive movements of the wrist and forearm, such as rotating or bending, that place excessive pressure on the the tendons and muscles attached to the medial epicondyle of the elbow.
A common cause of internal epicondylitis is repeated participation in sports or activities that strain the wrist and forearm flexor muscles, such as golf, baseball, tennis, or weightlifting. These activities can lead to repetitive strain injuries to the tendons and muscles of the medial epicondyle, causing inflammation and pain.
Apart from sporting activities, certain professions or work activities can also increase the risk of developing internal epicondylitis. Occupations involving repetitive movements of the wrist and forearm, such as painting, plumbing, computer work, or gardening, can cause overuse of the wrist flexor muscles and contribute to the development of this condition.
Additionally, anatomical or biomechanical factors may predispose to internal epicondylitis. For example, muscle weakness or an imbalance between the wrist flexors and extensors can increase stress on the tendons and muscles of the medial epicondyle, increasing the risk of injury and inflammation.
Technical errors or poor posture when performing certain activities can also contribute to the development of internal epicondylitis. Poor tennis striking or golf swing technique, for example, can lead to overuse of the wrist flexor muscles and tendons attached to the medial epicondyle, leading to irritation and inflammation.
Here are some common causes of this condition:
- Repetitive movements: The most common cause of internal epicondylitis is repetitive, excessive use of the wrist and finger flexor muscles. This can occur in a variety of activities, including playing golf, hence the name “golf elbow,” as well as other sports and activities requiring rotational movements of the wrist.
- Specific sports: Certain sports, such as tennis, badminton, baseball, and other racket or throwing sports, can contribute to the development of medial epicondylitis due to repetitive motion and stress on the elbow muscles .
- Poor technique: Incorrect technique when practicing sports or weight training activities can increase stress on the elbow tendons, thus promoting the development of tendinopathy.
- Occupational factors: Certain occupations that involve repetitive wrist and hand movements, such as computer work or repetitive manual activities, may also contribute to this condition.
- Age: Internal epicondylitis can occur at any age, but is most common in middle-aged adults.
- Anatomical factors: Some individuals may have an anatomical predisposition to developing tendon problems, which may increase the risk of internal epicondylitis.
- Sudden overloads: Sudden overloads or sudden excessive exertion, even in non-repetitive activities, can also contribute to the development of this condition.
It is important to note that medial elbow tendinopathy can result from a combination of these factors, and prevention plays a crucial role. Regular breaks, using correct techniques, proper muscle strengthening, and paying attention to warning signs of overuse can help reduce the risk of developing this condition.
Pathophysiology of internal epicondylitis of the elbow
Let’s explore the pathophysiology of this condition step by step.
Step 1: Repetitive microtrauma
The first stage in the development of internal epicondylitis is often associated with repetitive microtrauma. These microtraumas occur during repetitive activities involving flexion and rotation of the wrist, such as golf swings, tennis swings, or other intensive manual activities.
Step 2: Excessive Stress on the Tendons
Repetitive movements put excessive strain on the wrist flexor tendons, which are responsible for flexion and downward rotation of the wrist. These tendons attach to the medial epicondyle, the bone located on the inside of the elbow. Excessive stress causes increased tension on these tendons, thus promoting the development of micro-lesions.
Step 3: Inflammation and Immune Response
Repetitive microtrauma and excessive strain cause inflammation of the tendons. In response to these injuries, the immune system triggers an inflammatory reaction to try to repair the damage. This results in the release of inflammatory mediators, such as cytokines, causing redness, swelling and pain.
Step 4: Scar Tissue Formation
As the inflammatory response progresses, healing processes take place. However, healing can be disrupted by continued repetitive movements, leading to the formation of irregular scar tissue. This scar tissue can alter the normal structure of tendons and compromise their flexibility.
Step 5: Chronic Pain and Reduced Function
At this stage, the presence of scar tissue, combined with persistent inflammation, contributes to chronic pain. The pain may worsen with activity and lead to reduced elbow function. Patients may experience discomfort with simple wrist movements or when grasping objects.
Step 6: Risk of Long-Term Complications
Without adequate treatment, internal epicondylitis can progress to long-term complications, such as tendon degeneration or the formation of calcifications in the tendons. These complications can lead to a significant decrease in quality of life and require more invasive interventions.
Logical Pathway to Medial Epicondylitis Diagnosis
Diagnosing medial epicondylitis, or golfer’s elbow, involves a structured approach to identify the root cause of pain, assess the severity of the condition, and rule out other potential diagnoses. Below is the logical pathway typically followed to arrive at an accurate diagnosis:
1. Patient History and Symptom Inquiry
The diagnostic process begins with a thorough review of the patient’s medical history and a detailed discussion of symptoms. The healthcare provider will ask about:
- Pain location: Patients typically report pain on the inner side of the elbow, which may radiate down the forearm.
- Activity level: Questions about any repetitive movements involving the wrist, forearm, or elbow, such as playing golf, racket sports, or engaging in manual labor, are essential. These activities often contribute to the overuse injury.
- Onset of symptoms: The physician will inquire whether the pain began gradually or was triggered by a specific activity or trauma.
- Duration and intensity of pain: Information on how long the patient has experienced symptoms and whether the pain worsens during specific activities (e.g., gripping, twisting, or lifting).
- Previous treatments: Any home treatments or medications used and their effectiveness.
This history helps to form an initial impression of medial epicondylitis and sets the stage for further evaluation.
2. Physical Examination
A physical exam helps assess pain, movement limitations, and any visible signs of injury. The physician will perform a series of tests to evaluate the function of the elbow and surrounding areas. This typically includes:
- Palpation: The doctor will press on the medial epicondyle (the bony bump on the inside of the elbow) to assess for tenderness, which is a key indicator of medial epicondylitis.
- Range of motion tests: The patient may be asked to bend and extend the elbow, wrist, and fingers to determine if these movements trigger pain.
- Grip strength: The doctor may assess the strength of the patient’s grip by asking them to squeeze an object. Weakness in the grip, combined with pain, is a common finding in medial epicondylitis.
- Resisted wrist flexion and pronation tests: The patient will be asked to flex their wrist against resistance while the elbow is extended. Pain during this test suggests inflammation of the wrist flexor tendons, which is characteristic of medial epicondylitis.
3. Differential Diagnosis
Before confirming medial epicondylitis, it is important to rule out other conditions that may cause similar symptoms. Differential diagnoses may include:
- Cubital tunnel syndrome: This condition involves compression of the ulnar nerve, causing pain along the inner elbow and forearm. However, it often presents with numbness and tingling in the ring and little fingers, which is not typical of medial epicondylitis.
- Elbow arthritis: Inflammatory or degenerative joint disease can cause pain and stiffness in the elbow, but arthritis-related pain is usually diffuse rather than concentrated around the medial epicondyle.
- Ulnar collateral ligament (UCL) injury: Common in athletes, a UCL injury presents with elbow pain, but usually with instability and a history of acute trauma.
- Bursitis or tendinitis in other areas: Inflammation of the bursae or other tendons around the elbow joint can cause pain but may involve different locations and patterns of movement restriction.
Osteopathy for the treatment of internal epicondylitis of the elbow
Medial epicondylitis, commonly referred to as “golfer’s elbow,” is a painful condition caused by overuse or strain on the tendons that attach to the medial epicondyle, the bony prominence on the inside of the elbow. This condition is not limited to golfers; it can affect anyone engaging in repetitive motions that stress the forearm muscles and tendons, such as tennis players, manual laborers, or office workers who perform frequent wrist and finger movements.
While conventional treatments like rest, ice, anti-inflammatory medications, and physiotherapy are commonly recommended, osteopathy provides a holistic, non-invasive approach to managing and treating medial epicondylitis. Osteopathy focuses on restoring balance within the body by addressing the musculoskeletal structures involved, including muscles, tendons, and joints, not just at the site of pain but throughout the entire upper body. This integrative approach allows osteopaths to treat the root cause of the condition, rather than just alleviating symptoms.
Understanding Medial Epicondylitis
Before delving into how osteopathy can treat medial epicondylitis, it’s important to understand the condition itself. Medial epicondylitis is characterized by inflammation and micro-tears in the tendons of the forearm muscles responsible for wrist flexion and finger movements. These tendons attach to the medial epicondyle, a small bony structure on the inner side of the elbow. Repetitive strain, overuse, or improper technique during physical activities can lead to the gradual breakdown of these tendons, resulting in pain, weakness, and reduced functionality.
People suffering from medial epicondylitis may experience:
- Pain on the inside of the elbow, often radiating down the forearm.
- Weakness in grip strength, particularly when attempting to lift objects or perform tasks like turning a doorknob.
- Stiffness or reduced range of motion in the elbow and wrist.
- Tenderness when touching or applying pressure to the medial epicondyle.
- Discomfort during activities that involve repetitive hand or wrist movements, such as gripping or flexing the wrist.
The condition can be aggravated by activities that involve wrist flexion, pronation of the forearm, or gripping motions, which are common in various sports and occupations. If left untreated, medial epicondylitis can become chronic and lead to prolonged pain and disability.
The Osteopathic Approach to Medial Epicondylitis
Osteopathy takes a whole-body approach to the treatment of medial epicondylitis, addressing not only the local symptoms in the elbow but also the underlying causes and compensatory patterns in other parts of the body. The goal of osteopathic treatment is to improve the body’s ability to heal itself by restoring balance, mobility, and function throughout the musculoskeletal system.
An osteopath considers the following factors when treating medial epicondylitis:
- Muscle Imbalances and Tension The osteopath assesses muscle imbalances in the forearm, upper arm, shoulder, and back that may be contributing to the strain on the tendons attached to the medial epicondyle. Muscle tightness or weakness in these areas can lead to poor mechanics during repetitive activities, increasing the likelihood of injury. Through manual techniques such as soft tissue manipulation, muscle energy techniques, and stretching, the osteopath works to release tension and restore normal muscle function.
- Joint Mobility Restricted joint mobility, particularly in the elbow, wrist, shoulder, or cervical spine, can affect the mechanics of the entire upper limb, leading to compensatory movements that increase stress on the elbow tendons. Osteopathic joint mobilization techniques are used to improve the range of motion in these areas, ensuring that the elbow is not overloaded during activities. This helps distribute the physical load more evenly across the arm, reducing strain on the medial epicondyle.
- Postural Alignment Poor posture, particularly in the shoulders and upper back, can contribute to the development and persistence of medial epicondylitis. For example, forward-rolled shoulders or a slouched upper back can alter the alignment of the entire upper extremity, increasing strain on the forearm muscles and tendons. Osteopathic treatment may involve postural corrections, with the aim of improving shoulder and spine alignment to reduce the stress placed on the elbow.
- Neural Considerations Osteopaths also consider the role of nerve impingement or irritation in contributing to symptoms of medial epicondylitis. The ulnar nerve, which runs along the inside of the elbow, may become irritated due to inflammation or poor biomechanics. Techniques such as nerve mobilization or gentle manipulations can help reduce nerve tension and improve the overall function of the arm.
- Circulation and Healing Osteopathic techniques also aim to enhance blood flow and lymphatic drainage to the affected area. Improved circulation supports the healing process by delivering oxygen and nutrients to the injured tissues and removing waste products that accumulate as a result of inflammation. Techniques like soft tissue massage and rhythmic joint mobilization promote circulation and reduce swelling, speeding up recovery.
Osteopathic Techniques for Medial Epicondylitis
An osteopath uses various techniques, tailored to the patient’s specific needs, to treat medial epicondylitis. The following osteopathic techniques are commonly employed:
- Soft Tissue Manipulation This technique involves the application of pressure to muscles and tendons to release tension and improve circulation. By addressing tightness in the forearm, shoulder, and upper back, soft tissue manipulation helps reduce strain on the tendons attached to the medial epicondyle.
- Joint Mobilization Gentle manipulation of the elbow, wrist, shoulder, and even the spine can improve joint mobility and ensure that movement patterns are more balanced. By increasing the range of motion in these joints, the osteopath helps reduce compensatory movements that exacerbate medial epicondylitis.
- Muscle Energy Techniques (MET) MET involves the patient actively contracting specific muscles against a controlled resistance provided by the osteopath. This technique helps to lengthen tight muscles and strengthen weak ones, promoting balanced muscle function and reducing tension on the elbow tendons.
- Stretching and Rehabilitation Exercises In addition to hands-on treatment, osteopaths often prescribe specific stretching and strengthening exercises for the forearm, wrist, and shoulder. These exercises help restore flexibility and strength, aiding in the long-term prevention of medial epicondylitis recurrence. Stretching exercises, such as wrist flexor and extensor stretches, are particularly important for maintaining flexibility in the forearm muscles.
- Postural and Ergonomic Advice Osteopaths provide advice on proper posture and ergonomics, particularly for patients whose work or daily activities contribute to their condition. Adjusting the workspace, using proper lifting techniques, and modifying repetitive movements can all help reduce the risk of re-injury.
Benefits of Osteopathy for Medial Epicondylitis
Osteopathy offers several key benefits for individuals suffering from medial epicondylitis:
- Holistic Approach: Osteopaths treat the body as a whole, addressing not only the local site of pain but also other factors such as muscle imbalances, posture, and joint mobility, which may be contributing to the condition.
- Non-Invasive: Osteopathy is a non-invasive treatment option, making it suitable for individuals seeking alternatives to medications or surgery.
- Pain Relief: By releasing muscle tension and improving joint function, osteopathy can provide immediate relief from pain and discomfort associated with medial epicondylitis.
- Improved Mobility: Osteopathic treatment helps restore mobility in the affected joints and muscles, allowing patients to return to their daily activities without pain.
- Preventative Care: Osteopaths not only treat the symptoms but also provide guidance on how to prevent future episodes of medial epicondylitis through proper posture, ergonomics, and exercise.
Recommendations for Managing Medial Epicondylitis (Golfer’s Elbow)
Below are practical recommendations to help alleviate symptoms and promote recovery.
1. Rest the Arm
One of the most important steps in recovering from medial epicondylitis is allowing the affected arm to rest. Repeated use of the injured arm, especially engaging in the same repetitive motions that caused the injury, can delay the healing process and worsen the pain. It is critical to stop these repetitive activities until the pain has completely subsided.
- Tip: During this rest period, avoid lifting heavy objects, repetitive wrist motions, or any activity that strains the elbow. Once the pain has significantly reduced, gradually reintroduce activities to ensure the tendons have recovered and strengthened.
2. Apply Ice or Cold Compresses
Ice or a cold compress is an effective way to reduce pain, swelling, and inflammation in the elbow. Cold therapy numbs the affected area, reducing discomfort and preventing further tissue damage.
- How to Apply: Wrap an ice pack or a cold compress in a towel and apply it to the painful area for up to 20 minutes. Repeat this process three to four times a day. Be careful not to apply the ice directly to the skin to avoid frostbite.
3. Wear a Splint

A splint can provide support to the injured arm, minimizing unnecessary movement and reducing strain on the affected tendons. It helps immobilize the elbow, allowing the tendons to heal properly without excessive motion that could worsen the condition.
- When to Use: Wear the splint during daily activities where your arm may be used or strained. It is especially useful when engaging in tasks that involve repetitive wrist movements or gripping objects.
4. Stretching Exercises
Incorporating stretching exercises can help improve flexibility, relieve tension in the tendons, and strengthen the muscles around the elbow. These exercises should be done gently and consistently to support long-term recovery. Below are some effective stretches:
- Wrist Extension Stretch:
- Extend the affected arm in front of you with the palm facing down.
- Use your other hand to apply light downward pressure on your fingers and wrist.
- Hold the stretch for 15 to 30 seconds.
- Repeat on the other side.
- Wrist Flexor Stretch:
- Extend the affected arm in front of you with the palm facing up.
- Gently pull your fingers down with the opposite hand.
- Hold the position for 15 to 30 seconds.
- Repeat on the other arm.
- Forearm Stretch with Opposite Hand:
- Extend the affected arm in front of you with the palm up.
- Use your other hand to grasp your fingers and gently pull them down.
- Hold the stretch for 15 to 30 seconds.
- Repeat on the opposite side.
- Triceps Stretch:
- Raise the affected arm above your head.
- Bend your elbow and let your hand slide down your back.
- Use your opposite hand to apply light pressure to your elbow.
- Hold for 15 to 30 seconds and repeat on the other side.
- Shoulder Muscle Stretch:
- Extend the affected arm in front of you.
- Cross the arm over your chest and use the other hand to apply light pressure toward your body.
- Hold the stretch for 15 to 30 seconds, then switch to the other arm.
Performing these stretches regularly can improve range of motion and prevent stiffness in the elbow, wrist, and shoulder. However, it is essential to listen to your body—if pain worsens or persists, it may be necessary to consult a healthcare professional for further guidance.
5. Listen to Your Body
While rest, ice, and stretching are effective strategies for recovery, every person’s condition is unique. If you experience increasing pain during these exercises or daily activities, seek professional medical advice. A healthcare provider can offer a personalized treatment plan that may include physical therapy, specific exercise routines, or other interventions tailored to your specific needs.
Conclusion
Medial epicondylitis, commonly known as “golfer’s elbow,” is a painful condition that can significantly affect the quality of life of those who suffer from it. The pain is usually localized on the inner side of the elbow and can radiate down the forearm, making it difficult to perform everyday tasks such as lifting objects, gripping tools, or even simple activities like turning a doorknob. Although often associated with repetitive activities or mechanical overload, it is essential to adopt a comprehensive and personalized treatment approach for each patient.
Osteopathy provides a natural, non-invasive solution for treating medial epicondylitis. With its holistic approach, osteopathy aims to restore balance to the musculoskeletal system by reducing excessive tension and promoting better tissue mobility. By addressing the entire upper limb, from the shoulder to the wrist, as well as the neck and back, osteopathy helps improve circulation and supports faster healing of affected tissues.
In addition to treating the elbow directly, osteopathy also targets postural imbalances and accumulated tension in other parts of the body that may contribute to overuse of the elbow. Through gentle manipulation techniques, mobilization, and specific stretches, an osteopath can help alleviate pain, reduce inflammation, and restore normal function to the joint.
It is important to note that osteopathic treatment for medial epicondylitis is tailored to the individual, depending on the severity of symptoms and the underlying causes. Preventive care can also be implemented, with advice on ergonomics, posture, and exercises to strengthen and stretch the relevant muscles, helping to prevent future recurrence of the condition.
In summary, osteopathy offers an effective, natural alternative for treating medial epicondylitis, promoting long-lasting recovery and helping to prevent the condition from returning through a comprehensive and preventive approach.
References
- Shiri R, Viikari-Juntura E, Varonen H, Heliövaara M. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol. 2006 Dec 01;164(11):1065-74. [PubMed]
- Floor KD, Halbrecht J, Lourie GM. Medial and lateral epicondylitis in the athlete. Clin Sports Med. 1996 Apr;15(2):283-305. [PubMed]
- Wolf JM, Mountcastle S, Burks R, Sturdivant RX, Owens BD. Epidemiology of lateral and medial epicondylitis in a military population. Mil Med. 2010 May;175(5):336-9. [PubMed]
- Descatha A, Leclerc A, Chastang JF, Roquelaure Y., Study Group on Repetitive Work. Medial epicondylitis in occupational settings: prevalence, incidence and associated risk factors. J Occup Environ Med. 2003 Sep;45(9):993-1001. [PMC free article] [PubMed]
- Budoff JE, Hicks JM, Ayala G, Kraushaar BS. The reliability of the “Scratch test”. J Hand Surg Eur Vol. 2008 Apr;33(2):166-9. [PubMed]
- Polkinghorn BS. A novel method for assessing elbow pain resulting from epicondylitis. J Chiropr Med. 2002 Summer;1(3):117-21. [PMC free article] [PubMed]
- Amin NH, Kumar NS, Schickendantz MS. Medial epicondylitis: assessment and management. J Am Acad Orthop Surg. 2015 Jun;23(6):348-55. [PubMed]
- Kane SF, Lynch JH, Taylor JC. Evaluation of elbow pain in adults. Am Fam Physician. 2014 Apr 15;89(8):649-57. [PubMed]
- Sims SE, Miller K, Elfar JC, Hammert WC. Non-surgical treatment of lateral epicondylitis: a systematic review of randomized controlled trials. Hand (NY). 2014 Dec;9(4):419-46. [PMC free article] [PubMed]
- Hoogvliet P, Randsdorp MS, Dingemanse R, Koes BW, Huisstede BM. Does effectiveness of exercise therapy and mobilization techniques offer guidance for the treatment of lateral and medial epicondylitis? A systematic review. Br J Sports Med. 2013 Nov;47(17):1112-9. [PubMed]
- Degen RM, Cancien JM, Camp CL, Altchek DW, Dines JS, Werner BC. Patient-related risk factors for requiring surgical intervention following a failed injection for the treatment of medial and lateral epicondylitis. Phys Sportsmed. 2017 Nov;45(4):433-437. [PubMed]
- Vinod AV, Ross G. An effective approach to diagnosis and surgical repair of refractory medial epicondylitis. J Shoulder Elbow Surg. 2015 Aug;24(8):1172-7. [PubMed]
- Epicondylitis and corticosteroid injection: fewer cures at one year. Prescribe Int. 2015 Jun;24(161):160-1. [PubMed]