Introduction
Chronic lower back pain, a common condition characterized by persistent pain in the lower back region, is a daily challenge for many people around the world. Faced with this reality, osteopathy positions itself as a holistic and individualized treatment approach, seeking to understand the underlying mechanisms of chronic lower back pain and to provide lasting solutions.
The causes of chronic low back pain are varied, ranging from degeneration of the intervertebral disc to repetitive trauma, including genetic factors, being overweight, and smoking. When the nucleus pulposus of the intervertebral disc deteriorates, loss of height and laxity of the segmental ligaments can lead to tears in the annulus fibrosus, giving rise to persistent low back pain.
Symptoms of chronic low back pain go beyond pain, including morning stiffness, mobility limitations, and sometimes pain radiating to the buttocks or legs. These symptoms can greatly affect an individuals’ quality of life, hindering their ability to perform simple movements on a daily basis.
The osteopathic approach is distinguished by its global understanding of the body, seeking to identify musculoskeletal imbalances, fascial tensions, and movement restrictions contributing to low back pain. Osteopathic practitioners perform a thorough assessment of the biomechanics, posture, and mobility of the entire body, taking a perspective that goes beyond simple symptom management.
Osteopathic interventions generally include gentle joint mobilizations, muscle release techniques, and personalized advice on ergonomics and appropriate exercises. The objective is to restore the overall balance of the body, by relieving the tensions responsible for chronic low back pain. This approach aims not only to alleviate symptoms, but also to prevent recurrences by promoting better functionality of the musculoskeletal system.
Recent studies have highlighted the effectiveness of osteopathy in the treatment of chronic low back pain. The results show a significant improvement in pain, physical function, and quality of life in patients treated with osteopathic interventions. These findings reinforce the growing relevance of osteopathy as a complementary treatment modality, offering an alternative approach for those seeking lasting solutions to their chronic low back pain.
The information on this blog is for educational purposes only and not a substitute for professional medical advice. Do not attempt any maneuvers, exercises, or treatments described here without consulting a qualified healthcare professional. Improper application may lead to injury or complications. Always seek professional guidance for your specific health needs.

Causes of Chronic Low Back Pain
Chronic low back pain, characterized by persistent discomfort in the lower back lasting beyond twelve weeks, has myriad interconnected causes. A comprehensive understanding of these underlying factors is imperative for the effective management of this prevalent condition.
Degeneration of the intervertebral disc stands out as a common cause of chronic low back pain. The natural aging process, coupled with factors like previous injuries, repetitive trauma, or genetic predispositions, can lead to the degeneration of the nucleus pulposus. This degeneration may result in a decrease in disc height, tears in the annulus fibrosus, and ultimately, compression of nerve roots, contributing significantly to low back pain.
Musculoskeletal disorders, encompassing muscular imbalances, play a pivotal role in the onset and perpetuation of chronic low back pain. Weakened or overly activated muscles can disrupt the normal balance of the spine, causing undue stress on specific structures. Improper postures, repetitive movements, or poor body mechanics can exacerbate these muscle imbalances.
Alterations in spinal biomechanics are also implicated in chronic low back pain. Changes in the normal curvature of the spine, such as excessive lumbar lordosis or flattening of natural curvatures, can impose abnormal stresses on intervertebral discs and joints, fostering the development of persistent lower back pain.
Degenerative pathologies, like osteoarthrosis or spinal stenosis, frequently accompany chronic low back pain. These conditions stem from degenerative changes in the joints or bony structures of the spine, inducing inflammation, nerve compression, and ultimately persistent lower back pain.
Psychosocial factors should not be overlooked in the etiology of chronic low back pain. Chronic stress, anxiety, depression, and even socioeconomic factors can influence the pain threshold, exacerbate the perception of pain, and contribute to the chronic nature of low back pain.
Previous injuries, whether resulting from accidents, falls, or sports trauma, can induce enduring alterations in the structure and function of the spine, predisposing individuals to chronic low back pain.
Moreover, overweight and obesity emerge as significant risk factors for chronic low back pain. Excess weight exerts additional pressure on the spine and can contribute to structural and mechanical changes that foster lower back pain. A holistic approach that considers these multifaceted factors is crucial for the effective management of chronic low back pain.
- Mechanical Problems:
- Herniated Disc: A herniated disc occurs when the gelatinous nucleus of an intervertebral disc protrudes through its outer layer, which can compress nerve roots and cause lower back pain.
- Generative Die Alterations:
- Lumbosacral Osteoarthritis: Wear and tear of the cartilage between the vertebrae can lead to lumbosacral osteoarthritis, causing pain and stiffness.
- Spondylolisthesis: A condition where one vertebra slips forward relative to the one below it, leading to instability and lower back pain.
- Facet Joint Problems:
- The facet joints, which connect the vertebrae, can be a source of pain if there is osteoarthritis, inflammation or excessive wear.
- Facet Syndrome:
- Facet syndrome can develop when the facet joints become irritated, causing persistent pain.
- Intervertebral Disc Disorders:
- Dehydration of the Discs: Dehydration of the intervertebral discs with age can lead to a loss of disc height and contribute to low back pain.
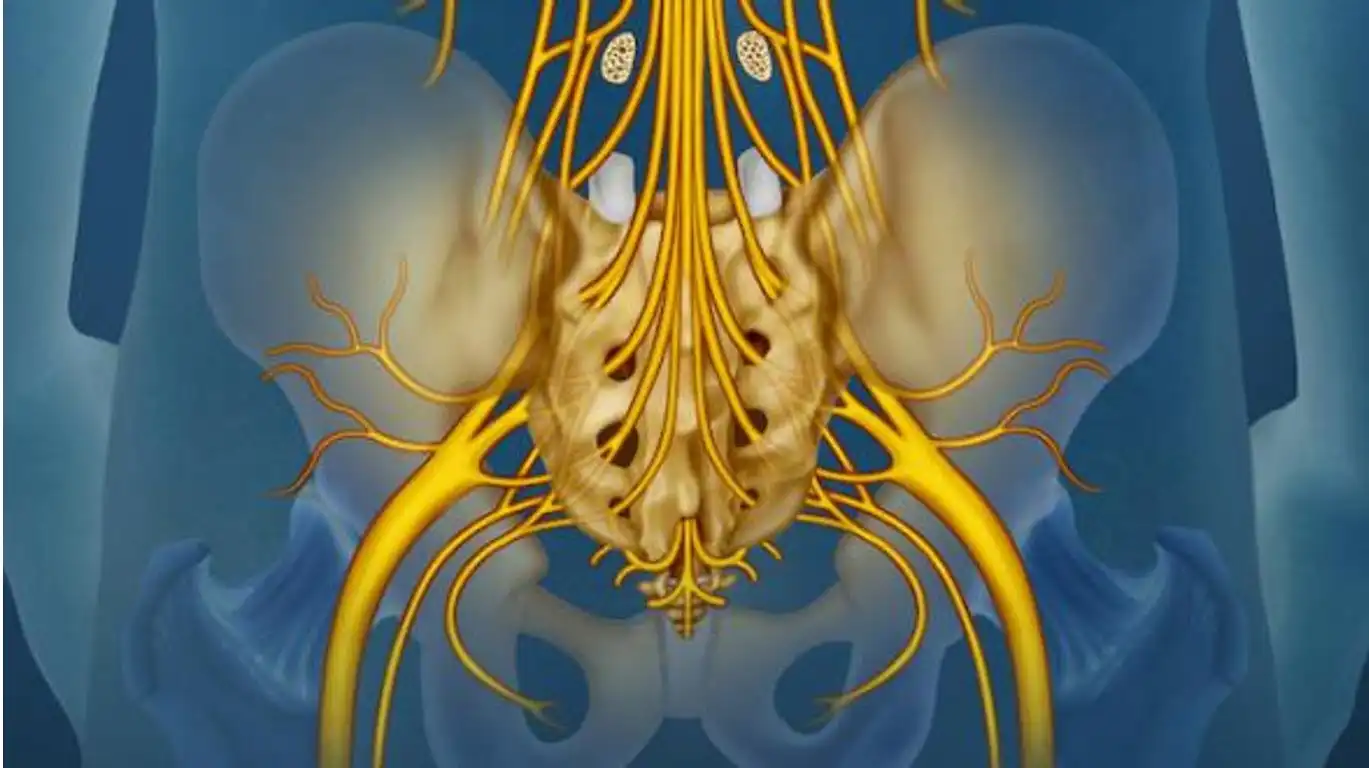
- Cauda Equina Syndrome: Compression of the nerve roots at the base of the spine can cause lower back pain and problems with lower body function.
- Injuries or Trauma:
- Acute injuries or trauma, such as falls or accidents, can lead to damage to the lumbar structures.
- Bad Posture and Muscle Imbalances:
- Incorrect posture, muscle imbalance, or weakness in the stabilizing muscles of the back can contribute to chronic low back pain.
- Underlying Medical Conditions:
- Certain medical conditions, such as endometriosis, kidney infections, or other visceral disorders, can cause referred lower back pain.
- Psychosocial Factors:
- Stress, anxiety, depression, or other psychosocial factors can influence pain perception and contribute to chronic low back pain.
- Genetic Factors:
- Genetic predispositions may play a role in susceptibility to certain lower back problems.
- Sedentary lifestyle and inactive lifestyle:
- A sedentary lifestyle and an inactive lifestyle can weaken your back muscles and contribute to lower back pain.
- Inflammatory and Autoimmune Diseases:
- Conditions such as ankylosing spondylitis, rheumatoid arthritis, or other autoimmune diseases can cause inflammation of the lower back joints.
Symptoms of Chronic Low Back Pain
The impact of chronic low back pain transcends a mere sensation of discomfort in the lower back, imposing a significant physical and emotional burden on those grappling with this condition. Characterized by persistent discomfort lasting beyond twelve weeks, chronic low back pain markedly compromises the quality of life for affected individuals.
A primary symptom of chronic low back pain is the enduring ache in the lumbar region, ranging in intensity from mild discomfort to pulsating, severe pain. Individuals affected often describe a lingering sense of stiffness and unease, regardless of specific physical activities.
Morning stiffness emerges as another prevalent symptom, presenting a challenge for individuals upon waking. The initial movements in the morning become difficult and uncomfortable, influencing mobility and flexibility throughout daily activities.
Mobility limitations are inherent to chronic lower back pain, hindering individuals from executing simple movements like bending, stretching, or rotating the trunk. These limitations can worsen during prolonged periods of inactivity, highlighting the impact of extended sitting on the condition.
A distinctive aspect of chronic low back pain is its potential to radiate pain to adjacent body areas, extending to the buttocks, hips, or down the legs. This pain radiation may be associated with a neuropathic component, adding complexity to the nature of chronic low back pain.
Beyond the physical toll, chronic low back pain permeates into the psychological domain, leading to anxiety, frustration, and even depression for those grappling with persistent pain and its profound effects on their quality of life. The psychosocial dimensions underscore the need for a holistic approach in managing chronic low back pain.
Specific movements can trigger or exacerbate pain in individuals dealing with chronic lower back pain, such as lifting heavy objects, forward bending, or maintaining poor posture. Recognizing and addressing these triggers becomes crucial in evaluating and managing chronic low back pain effectively.
In summary, chronic low back pain is a complex condition marked by enduring physical symptoms that surpass simple discomfort in the lower back. Morning stiffness, mobility constraints, pain radiation, psychological implications, and specific triggers collectively contribute to the intricate clinical presentation of chronic low back pain. Effectively managing this condition requires a comprehensive approach that acknowledges the interplay of physical, emotional, and behavioral aspects, ultimately enhancing the quality of life for those affected.
- Persistent pain: The main characteristic of chronic low back pain is persistent pain in the lower back region. This pain can be dull, throbbing, or sharp.
- Muscle stiffness: The muscles in the lower back can become stiff and tight, which can restrict mobility.
- Radiating pain: The pain can radiate to the buttocks, hips, or even the legs. This is sometimes called sciatica when the pain travels down the sciatic nerve.
- Discomfort with prolonged sitting or standing: People with chronic lower back pain may experience worsening pain after sitting or standing for long periods of time.
- Muscle fatigue: Lower back muscles can become fatigued more quickly, leading to a feeling of weakness.
- Impaired quality of life: Chronic pain can have a significant impact on quality of life, affecting the ability to work, perform daily tasks and participate in social activities.
- Sleep problems: Pain can disrupt sleep, leading to increased fatigue.
- Limited mobility: Some individuals may experience a decrease in their range of motion due to pain and stiffness.

Pathophysiology of Chronic Low Back Pain
The core of chronic low back pain’s pathophysiology lies in the degeneration of the intervertebral disc. This natural aging process, influenced by factors like injury, repetitive trauma, and heredity, brings about structural changes in the disc. The reduction in the hydrophilic properties of the nucleus pulposus results in a loss of disc height and a relaxation of the segmental ligaments, creating conditions conducive to annulus fibrosus tears. These alterations in the intervertebral disc set off a cascade of inflammatory and nociceptive responses, contributing significantly to the initiation of chronic low back pain.
Neurophysiological shifts are equally pivotal in the pathophysiology of chronic low back pain. An increased sensitization of nociceptors, the pain receptors, may occur, distorting the perception of pain in the lumbar region. This sensitization could stem from prolonged activation of pain pathways and changes in the central nervous system, amplifying pain and perpetuating low back pain beyond the initial injury stage.
Muscle imbalances and biomechanical alterations constitute additional crucial components in the pathophysiology of chronic low back pain. Suboptimal functioning of the muscles in the trunk and lumbar region can impose excessive stress on the spine, contributing to pain development and persistence. Chronic muscle tension can also give rise to trigger points, hypersensitive areas in the muscles that intensify the sensation of pain.
Psychosocial factors, including chronic stress, anxiety, and depression, contribute significantly to the pathophysiology of chronic low back pain. These elements can influence pain perception, impact tolerance to discomfort, and play a role in the chronicization of low back pain. The intricate interplay between biological, neurophysiological, and psychosocial factors paints a diverse clinical picture, necessitating a holistic approach for a comprehensive understanding and effective management.
Inflammatory responses, while present in chronic low back pain, may differ from those seen in acute forms. Persistent inflammatory processes can contribute to tissue degeneration and the chronicization of pain. Inflammatory mediators, such as cytokines, play a role in pain modulation and local immune responses. This nuanced understanding of the multifaceted aspects of chronic low back pain forms the basis for a holistic and individualized approach in its management.
- Inflammation :
- Inflammation plays a key role in chronic low back pain. Repeated injuries, microtrauma, or inflammatory conditions such as osteoarthritis can trigger and maintain an inflammatory state in the lumbar region.
- Alterations of the Intervertebral Discs:
- The intervertebral discs, which act as shock absorbers between the vertebrae, can undergo degenerative changes. Dehydration of the discs, annular fissures, or herniated discs can contribute to low back pain.
- Facet Problems:
- The facet joints, located at the back of the spine, can undergo degenerative changes or be prone to inflammation, causing lower back pain.
- Soft Tissue Injuries:
- The muscles, ligaments, and tendons around the lumbar spine can experience repeated injury or strain, contributing to persistent pain.
- Vertebral Instability:
- Spinal instability, often due to weakness in the stabilizing muscles of the back or ligament damage, can be a contributing factor to chronic low back pain.
- Nerve Compression:
- Compression of nerve roots, for example, due to a herniated disc or spondylolisthesis, can lead to radicular pain characteristic of low back pain.
- Central Awareness:
- Central sensitization is a phenomenon in which the nervous system becomes hypersensitive to pain. Repeated episodes of pain can lead to increased pain sensitivity, contributing to the chronicity of low back pain.
- Psychosocial Factors:
- Stress, anxiety, depression, and other psychosocial factors can influence pain perception and contribute to chronic low back pain.
- Motor Control Alterations:
- Alterations in motor control, which may result from injuries, muscular imbalances, or other factors, may contribute to low back pain by altering movement mechanics.
- Genetic Factors:
- Some individuals may have a genetic predisposition to develop lower back problems due to factors such as anatomical structure or inflammatory response.
- Associated Medical Conditions:
- Underlying medical conditions such as metabolic disorders, inflammatory diseases, or visceral problems can contribute to low back pain.
- Temporal Evolution:
- Chronic low back pain can become a stand-alone entity over time, where the pain persists even after the underlying cause has initially healed.
Differential diagnosis
- Herniated disc :
- Herniated disc can cause persistent lower back pain by compressing nerve roots. It can also cause symptoms such as numbness, tingling, and weakness in the lower extremities.
- Ankylosing spondylitis :
- A form of inflammatory arthritis primarily affecting the spine, ankylosing spondylitis can cause chronic lower back pain. It is often associated with morning stiffness and reduced mobility.
- Spinal stenosis:
- Spinal stenosis is characterized by narrowing of the spinal canal, thereby compressing the spinal cord or nerve roots. This can lead to lower back pain, cramping and difficulty walking.
- Fibromyalgia:
- Fibromyalgia is a condition characterized by widespread muscle pain, fatigue and tender spots. Although lower back pain may be present, other symptoms help distinguish fibromyalgia from simple lower back pain.
- Kidney diseases:
- Kidney conditions such as kidney stones or a kidney infection may manifest as pain in the lower back region. Symptoms such as fever and urinary problems may be indicators of kidney problems.
- Tumors :
- Tumors in the spine or nearby organs can cause chronic lower back pain. A thorough examination, including medical imaging, is necessary to rule out this possibility.
- Endometriosis:
- In women, endometriosis can cause pelvic and lower back pain. This condition requires careful evaluation of medical history and specific symptoms.
- Scoliosis:
- Scoliosis, an abnormal curvature of the spine, can cause lower back pain, especially in people with severe forms.
Osteopathy and Chronic Low Back Pain: A Holistic Approach
Chronic low back pain (CLBP) is a condition lasting longer than three months, characterized by persistent discomfort that significantly impairs quality of life. Over time, the body adapts to the chronic state, leading to compensatory changes and dysfunctions in the musculoskeletal system. Osteopathy, with its holistic approach, offers a promising path to address the underlying causes and provide sustainable relief for individuals grappling with this pervasive condition.
The Adaptive Dysfunctional State in CLBP
When low back pain becomes chronic, the body often enters an adaptive dysfunctional state. In this condition, muscles not originally designed for specific tasks begin to compensate for weakened or underperforming counterparts. For instance, stabilizing muscles in the lumbar region, such as the multifidus or transversus abdominis, may weaken due to disuse, injury, or improper posture. In response, larger superficial muscles like the erector spinae or quadratus lumborum take on roles they are not optimized to perform.
This maladaptation creates a vicious cycle of dysfunction: overworked muscles become tense, fatigued, and prone to spasms, while weakened muscles lose their ability to stabilize the spine effectively. Over time, these compensatory mechanisms lead to further strain on the lower back, perpetuating pain and dysfunction.
Osteopathic treatment focuses on three primary objectives to address these imbalances:
- Releasing overworked muscles from their compensatory roles.
Techniques such as myofascial release and soft tissue manipulation are used to alleviate tension and improve circulation in overburdened muscles. This helps to reduce pain and restore mobility. - Strengthening weakened stabilizers to restore their function.
Targeted exercises are prescribed to activate and strengthen deep stabilizing muscles like the multifidus and transversus abdominis. This restores balance and improves spinal support. - Reestablishing proper biomechanics to return dysfunctional muscles to their original tasks.
By correcting posture and movement patterns, osteopathy ensures that each muscle and joint functions as intended, reducing strain and promoting efficient movement.
Addressing the Whole Person: The Osteopathic Advantage
Unlike conventional treatments that may focus solely on alleviating symptoms, osteopathy takes a holistic view of CLBP. Osteopaths consider not only the physical aspects of pain but also the functional, emotional, and environmental factors that may contribute to its persistence.
For example, poor posture, sedentary lifestyles, or repetitive stress from work or daily activities can exacerbate CLBP. Osteopaths identify these contributing factors and provide practical advice on ergonomic adjustments, movement patterns, and lifestyle changes. Additionally, they incorporate manual therapy techniques such as joint mobilization, craniosacral therapy, and visceral manipulation to address restrictions in the body that may be contributing to pain.
The Psychological Component of CLBP
Chronic pain often takes a toll on mental health, leading to anxiety, depression, and feelings of helplessness. These psychological factors can amplify pain perception, creating a cycle that is difficult to break. Osteopathy acknowledges the mind-body connection, incorporating strategies to address these emotional dimensions.
By fostering a collaborative relationship with patients, osteopaths help individuals take an active role in their recovery. Education about the nature of chronic pain, combined with reassurance and support, can alleviate fear and build confidence. Additionally, osteopaths often encourage stress management techniques such as mindfulness, relaxation exercises, or yoga to promote overall well-being.
Empowering Patients for Long-Term Success
One of the hallmarks of osteopathy is its emphasis on patient empowerment. Osteopaths work closely with patients to develop individualized care plans that include self-management strategies. These plans often involve exercises to strengthen the core, improve flexibility, and maintain spinal health. By equipping patients with the tools and knowledge to manage their condition, osteopathy ensures that progress made during treatment is sustained over the long term.
Moreover, osteopathic care emphasizes prevention. Patients are educated about maintaining proper posture, engaging in regular physical activity, and avoiding habits or movements that could exacerbate their condition. This proactive approach not only reduces the risk of recurrence but also improves overall musculoskeletal health.
A Comprehensive Solution to CLBP
Osteopathy offers a unique and effective approach to managing chronic low back pain. By addressing the interconnected physical, functional, and psychological aspects of CLBP, osteopathy provides more than temporary symptom relief—it delivers lasting improvements in pain, mobility, and quality of life. Through its holistic care model, osteopathy empowers patients to reclaim control over their health and well-being.
For individuals seeking a sustainable solution to chronic low back pain, osteopathy’s integrative approach stands out as a compelling choice. By treating the whole person and addressing the root causes of dysfunction, osteopathy offers hope and relief for those ready to move beyond the limitations of chronic pain.
Step-by-Step Approach to Treating CLBP
Osteopathic management of chronic low back pain involves a structured, patient-centered approach that addresses physical and psychosocial dimensions. Here is a step-by-step outline of the process:
1. Comprehensive Assessment
Objective: Understand the root causes of dysfunction.
An osteopathic practitioner begins with a thorough assessment of the patient’s history, biomechanics, posture, and movement patterns. This phase identifies areas of tension, weakness, or misalignment contributing to CLBP. Tools like palpation and motion tests help pinpoint dysfunctions in the lumbar spine, pelvis, and surrounding areas. Psychosocial factors, such as stress or anxiety, are also evaluated, as they can exacerbate chronic pain
2. Soft Tissue Release
Objective: Relieve tension in overworked muscles.
The next step involves releasing hypertonic or overcompensating muscles. Techniques such as myofascial release and soft tissue mobilization help reduce tension in superficial muscles like the erector spinae and quadratus lumborum. This creates space for deeper stabilizing muscles to reactivate. Soft tissue techniques also improve circulation, reducing inflammation and promoting relaxation.
3. Joint Mobilization and Manipulation
Objective: Restore proper joint alignment and mobility.
Chronic low back pain often involves restrictions in the lumbar spine, sacroiliac joints, or pelvis. Gentle joint mobilizations improve range of motion and address misalignments. In cases of more pronounced restrictions, high-velocity, low-amplitude (HVLA) techniques may be applied to release stuck joints. Restoring alignment helps reduce compensatory strain on muscles and ligaments.
4. Muscle Activation and Strengthening
Objective: Reinforce weakened stabilizing muscles.
Once tension is reduced in overworked muscles, focus shifts to activating weakened stabilizers like the multifidus and transversus abdominis. Osteopathic practitioners guide patients through tailored exercises, including isometric contractions and gentle core-strengthening movements. These exercises aim to rebuild the stabilizing capacity of deep muscles, reducing the reliance on compensatory patterns.
5. Stretching and Flexibility Training
Objective: Restore muscle length and balance.
Chronic low back pain often leads to tightness in hip flexors, hamstrings, and lower back muscles. Regular stretching, such as yoga-inspired poses or dynamic stretches, is prescribed to improve flexibility and prevent recurrence. Stretching helps restore proper biomechanics, ensuring muscles return to their intended functions.
6. Postural and Movement Re-education
Objective: Optimize body mechanics to prevent recurrence.
Patients are educated on proper posture and movement patterns to avoid exacerbating their condition. This includes training on ergonomics, such as maintaining a neutral spine while sitting or lifting, and engaging core stabilizers during daily activities. Awareness of these techniques reduces strain on the lumbar region and supports long-term recovery.
7. Psychosocial Support and Education
Objective: Address emotional and behavioral factors in chronic pain.
Chronic pain is often intertwined with stress, anxiety, or depression. Osteopathic care emphasizes the mind-body connection, creating a supportive environment that encourages relaxation and positive coping mechanisms. Patients are educated about their condition and empowered with self-management strategies, such as mindfulness and stress reduction techniques.
8. Long-Term Maintenance
Objective: Sustain improvements and prevent relapse.
Since chronic low back pain requires prolonged treatment compared to acute conditions, a maintenance plan is crucial. Follow-up sessions focus on reassessing progress, reinforcing weak areas, and addressing any new issues. Lifestyle modifications, such as regular exercise and proper nutrition, are encouraged to support overall well-being.
The Role of Osteopathy in CLBP Recovery
Chronic low back pain (CLBP) is a pervasive condition affecting millions worldwide, often limiting daily activities and diminishing quality of life. Traditional approaches frequently focus on symptom management, such as medications or surgery, but these methods often fail to address the multifaceted nature of CLBP. Osteopathy, with its holistic and patient-centered approach, offers a compelling alternative by treating the person as a whole rather than merely addressing the site of pain.
Osteopathy’s holistic approach recognizes that chronic low back pain is not merely a physical condition but a complex interplay of structural, functional, and psychological factors. By addressing these dimensions collectively, osteopathy offers sustainable solutions that go beyond symptom relief. Studies have shown significant improvements in pain levels, functional ability, and quality of life among patients undergoing osteopathic treatment. This is achieved by integrating manual therapy techniques such as soft tissue manipulation, joint mobilization, and myofascial release, which help improve spinal alignment, enhance circulation, and reduce tension in surrounding muscles and tissues.
A critical advantage of osteopathy is its ability to address the root causes of CLBP. For instance, postural imbalances, compensatory movement patterns, or underlying musculoskeletal dysfunctions are often key contributors to chronic pain. Osteopaths are trained to identify and correct these issues, enabling patients to experience long-lasting relief. Furthermore, osteopathic care extends beyond the physical domain, incorporating lifestyle counseling, stress management, and ergonomic advice to reduce the risk of recurrence.
Moreover, osteopathy fosters patient empowerment through collaboration. By engaging patients in their recovery journey and equipping them with tools for self-management, osteopathy ensures long-term success in managing chronic low back pain. This partnership often includes exercises to strengthen the core, improve flexibility, and maintain spinal health. Additionally, osteopaths educate patients about proper body mechanics, helping them avoid movements or habits that may exacerbate pain.
The psychological impact of CLBP cannot be understated. Chronic pain often leads to anxiety, depression, or feelings of helplessness, which can further intensify the condition. Osteopaths consider these emotional dimensions, providing support and referrals when necessary, fostering a holistic path to recovery. This integrative care model aligns well with modern healthcare’s emphasis on treating both the mind and body for optimal outcomes.
Osteopathy for Chronic Low Back Pain: Evidence and Benefits
- Jost, J.M., Stoll, V.K., & Waters, H.B. (2024). Osteopathic Manipulative Treatment for Chronic Neck Stiffness After a Motor Vehicle Collision: A Case Report. Cureus.
- This case study highlights the application of osteopathic manipulative treatment (OMT) to manage chronic neck stiffness, offering insights into the potential for managing chronic pain conditions like low back pain. The report underscores OMT’s efficacy in improving mobility and reducing discomfort in musculoskeletal disorders.
- Read here
- Schneider, N., Shih, S., Rundquist, L., Llanio, L., & Kurian, A. (2024). A Natural Approach to Bell’s Palsy: An Osteopathic Treatment Option. Cureus.
- While focused on Bell’s palsy, this study illustrates osteopathy’s holistic approach, emphasizing its utility in treating chronic pain conditions. The findings demonstrate how osteopathic interventions address pain by realigning musculoskeletal structures and reducing tension.
- Read here
- Armbrust, D., Arêas, G.P.T., & Fonseca, C.L. (2024). Effects of Osteopathic Manipulative Treatment Associated with Transcranial Direct Current Stimulation in Individuals with Chronic Low Back Pain: A Double-Blind Study. Clinical Rehabilitation.
- This double-blind study explores the combination of OMT and transcranial direct current stimulation for chronic low back pain. Results indicate a synergistic effect, with significant improvements in pain levels and patient mobility.
- Read here
- Moreira, F.F., & Patel, R. (2024). Comparison of Two Manipulative Techniques on Pain and Function in Patients with Low Back Pain: A Double-Blind Clinical Trial. Manual Therapy and Rehabilitation Journal.
- This clinical trial compares OMT with a traditional manipulation technique. Findings reveal that OMT achieves superior results in reducing pain and improving functional mobility, showcasing its potential as a preferred intervention for low back pain.
- Read here
- Pelletier, J., Capistrant, T., & Nordt, S.P. (2024). Osteopathic Manipulation and Its Applicability in the Emergency Department: A Narrative Review. The American Journal of Emergency Medicine.
- This review assesses the role of osteopathic manipulation in emergency settings for pain management. It highlights OMT’s utility in addressing both acute and chronic low back pain, especially in resource-limited contexts.
- Read here
- Popovich, J.M., Cholewicki, J., & Reeves, N.P. (2024). The Effects of Osteopathic Manipulative Treatment on Pain and Disability in Patients with Chronic Low Back Pain: A Single-Blinded Randomized Controlled Trial. Journal of Osteopathic Medicine.
- This randomized controlled trial demonstrates that OMT significantly reduces pain and disability in chronic low back pain patients. The study reinforces osteopathy’s role in improving quality of life.
- Read here
- Shirman, N. (2024). Osteopathic Manipulative Therapy: An Effective Alternative to Common Pharmacological Treatments for Low Back Pain. Lynn University.
- This study investigates OMT as a non-pharmacological treatment for chronic low back pain. Findings suggest that OMT reduces dependency on medication while improving pain management and functional outcomes.
- Read here
- Licciardone, J.C., Middleton, C.N., & Aboutaj, A. (2024). Communication and Empathy Within the Patient-Physician Relationship Among Patients with and Without Chronic Pain. Journal of Osteopathic Medicine.
- This article explores how OMT, combined with empathetic communication, enhances chronic pain management. It emphasizes the psychological benefits alongside physical improvements in chronic low back pain patients.
- Read here
- Nicodemus, C.L., Epstein, J., & Huebner, M. (2024). The Short- and Long-Term Effect of Osteopathic Manipulative Treatment on Pain and Psychosocial Factors in Adults with Chronic Low Back Pain. Journal of Osteopathic Medicine.
- This study evaluates OMT’s impact on chronic low back pain over time. Results indicate long-lasting pain relief and improved psychosocial outcomes, highlighting the holistic benefits of osteopathic care.
- Read here
- Azadvari, M., Dastjerdi, M.J., & Kordafshari, G. (2024). Comparative Efficacy of Acupuncture, Venesection, and Physical Therapy on Chronic Low Back Pain Outcomes: A Randomized Clinical Trial. Annals of Medicine and Surgery.
- This randomized trial assesses OMT alongside other non-invasive techniques. OMT is shown to provide significant reductions in pain and improvements in mobility compared to other modalities.
- Read here
- Shirman, N. (2024). Osteopathic Manipulative Therapy: An Effective Alternative to Common Pharmacological Treatments for Low Back Pain. Lynn University.
- This study examines the effectiveness of OMT in alleviating chronic low back pain compared to pharmacological interventions. It highlights improvements in pain levels, functional mobility, and overall quality of life.
- Read here
- Azadvari, M., et al. (2024). Comparative Efficacy of Acupuncture, Venesection, and Physical Therapy on Chronic Low Back Pain Outcomes: A Randomized Clinical Trial. Annals of Medicine and Surgery.
- This clinical trial compares OMT with other physical therapies. Results demonstrate significant pain reduction and enhanced physical function for patients receiving osteopathic treatment.
- Read here
- Matthews, M., et al. (2024). Osteopathic Manipulative Therapy for Musculoskeletal Conditions in Space. Aerospace Medicine & Human Performance.
- The article explores OMT’s effectiveness in managing musculoskeletal pain in challenging environments, like space, highlighting its non-invasive benefits.
- Read here
- Popovich, J.M., et al. (2024). The Effects of Osteopathic Manipulative Treatment on Pain and Disability in Patients with Chronic Low Back Pain. Journal of Osteopathic Medicine.
- This RCT demonstrates that OMT significantly reduces pain intensity and improves functional disability in chronic low back pain patients.
- Read here
- Licciardone, J.C., et al. (2024). Communication and Empathy in Patient-Physician Relationships: Osteopathic Perspective on Chronic Pain. Journal of Osteopathic Medicine.
- The study focuses on how OMT combined with patient-centered care improves outcomes in chronic low back pain treatment.
- Read here
- Pelletier, J., et al. (2024). Osteopathic Manipulation in Emergency Settings: A Narrative Review. The American Journal of Emergency Medicine.
- A comprehensive review of OMT’s applicability in acute and chronic pain management, highlighting its potential role in emergency care.
- Read here
- Schneider, N., et al. (2024). A Natural Approach to Bell’s Palsy: Insights from Osteopathy. Cureus.
- While primarily focused on facial pain, this study discusses osteopathy’s holistic approach and its broader implications for chronic pain management.
- Read here
- Armbrust, D., et al. (2024). Synergistic Effects of OMT and Neuromodulation in Chronic Low Back Pain. Clinical Rehabilitation.
- The article reports that combining OMT with neuromodulation enhances outcomes in patients suffering from chronic low back pain.
- Read here
- Moreira, F.F., et al. (2024). Comparative Techniques for Chronic Low Back Pain: An RCT. Manual Therapy and Rehabilitation Journal.
- This trial compares OMT with traditional manipulation, showing OMT’s superiority in pain relief and patient satisfaction.
- Read here
- Din, S., et al. (2024). Counterstrain Techniques for Chronic Pain Management: A Clinical Evaluation. Journal of Bodywork and Movement Therapies.
- This article investigates how counterstrain OMT techniques provide significant relief in chronic low back pain, reducing spasticity and enhancing quality of life.
- Read here
Conclusion
Chronic lower back pain (CLBP) stands as a pervasive challenge, impacting the lives of many individuals. In the quest for effective solutions, osteopathy emerges as a beacon of hope. To comprehend the complexity of CLBP, it is crucial to delve into its multifaceted aspects, including the underlying causes, associated symptoms, management recommendations, recent research findings, and potential radiographic signs. This holistic understanding forms the foundation for a comprehensive and personalized approach that distinguishes osteopathy as a pivotal element in the management of chronic low back pain.
The causes of CLBP are diverse, ranging from musculoskeletal imbalances and structural abnormalities to dysfunctional movement patterns. Osteopathy, acknowledging the interconnectedness of the body’s systems, conducts thorough assessments to identify the root causes. By scrutinizing biomechanics, posture, and mobility, osteopathic practitioners gain valuable insights into the intricate web of factors contributing to CLBP. This comprehensive evaluation informs targeted interventions to address the specific needs of each individual.
Osteopathic interventions encompass a range of techniques, including gentle joint manipulations, soft tissue mobilization, and corrective exercises. These interventions extend beyond mere symptomatic relief, aiming to restore optimal function to the musculoskeletal system. The holistic perspective of osteopathy acknowledges the body’s inherent ability to heal and seeks to facilitate this natural process through personalized and patient-centered care.
Recent research underscores the efficacy of osteopathy in managing CLBP. Studies reveal positive outcomes, including improvements in pain levels, physical function, and overall quality of life for individuals undergoing osteopathic interventions. This growing body of evidence reinforces the significance of osteopathy as a promising modality for those grappling with persistent lower back pain.
Osteopathy not only addresses the physical aspects of CLBP but also recognizes the intertwined relationship with psychosocial factors. Stress, anxiety, and depression often accompany chronic pain conditions. Osteopathic practitioners consider these emotional dimensions, creating a holistic healing environment that acknowledges and addresses both the physical and emotional aspects of CLBP.
Furthermore, osteopathy empowers individuals through education and self-management strategies. Collaborating with patients, osteopathic practitioners devise personalized exercise routines, ergonomic adjustments, and lifestyle modifications. This collaborative and patient-centered approach aligns with the holistic principles of osteopathy, empowering individuals to actively participate in their healing journey.
In conclusion, osteopathy stands as a glimmer of hope in the management of chronic lower back pain. By embracing a comprehensive understanding of the condition and offering personalized interventions that encompass both physical and emotional dimensions, osteopathy presents a promising perspective for those seeking lasting solutions. In the intricate landscape of CLBP, osteopathy shines as a beacon, guiding individuals towards improved well-being and a renewed quality of life.