Introduction
Osteitis pubis is a painful, inflammatory condition affecting the pubic symphysis, the joint located at the front of the pelvis. While often associated with athletes due to repetitive stress or trauma, this condition can also arise from non-athletic causes such as pregnancy, pelvic surgeries, or infections. The resulting pain, typically felt in the groin, lower abdomen, or pelvic region, can significantly limit mobility and quality of life, making early recognition and management crucial.
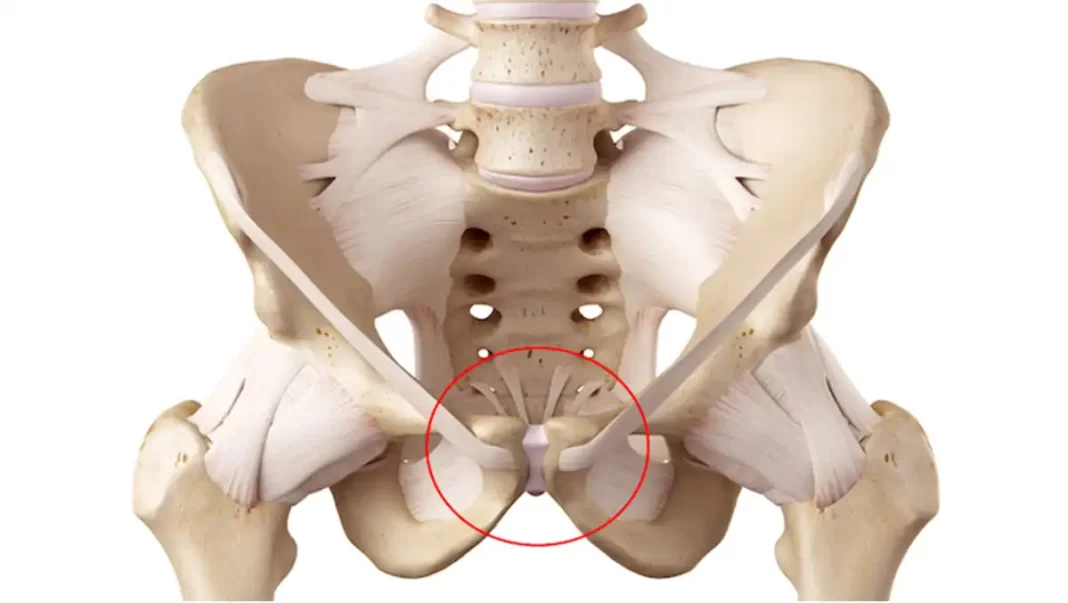
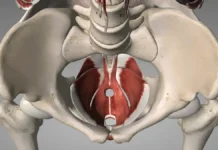
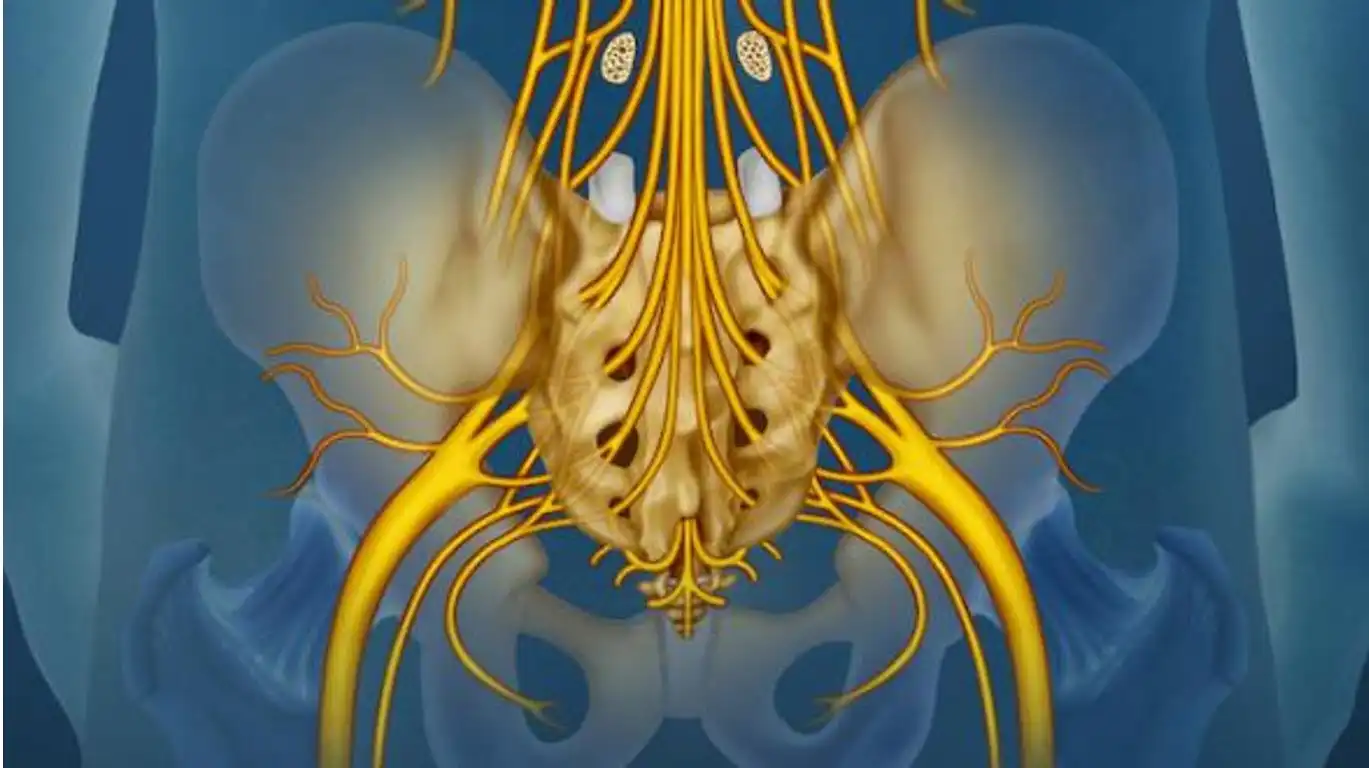
The pubic symphysis plays a vital role in maintaining pelvic stability, serving as a connection point for the left and right pubic bones. This fibrocartilaginous joint, reinforced by a network of strong ligaments, enables the pelvis to absorb and distribute forces during activities such as walking, running, and lifting. It also accommodates minor movements essential for physiological functions, including childbirth. Disruption of this intricate balance, as seen in osteitis pubis, can lead to biomechanical dysfunction, altering posture and movement patterns.
Understanding osteitis pubis begins with recognizing the complexity of the pubic symphysis and its surrounding structures. With its unique blend of stability and mobility, this joint underscores the importance of coordinated musculoskeletal and ligamentous function. The onset of osteitis pubis typically signifies an overuse injury, where excessive strain on the pubic symphysis triggers inflammation and tissue damage. In some cases, the condition can be secondary to systemic issues, such as infections or rheumatologic disorders, necessitating a multidisciplinary approach to diagnosis and treatment.
This article delves into the pathophysiology of osteitis pubis, shedding light on the factors that compromise the integrity of the pubic symphysis. By exploring the interplay between the pelvis’s structural and functional components, we aim to enhance understanding of this condition and its impact on overall musculoskeletal health. Through a deeper appreciation of the pubic symphysis’s role in pelvic stability, readers will gain insights into the importance of timely intervention and prevention strategies to maintain a healthy and functional pelvis.
Key Milestones in the Study of Osteitis Pubis
1924: Initial identification by Dr. Harris E. Beer in relation to postoperative pain after urological surgeries.
Dr. Harris E. Beer, a urologist, is credited with first describing osteitis pubis in 1924 as a postoperative complication. He observed the condition in patients who had undergone suprapubic surgery, such as prostatectomy, and characterized it as an inflammation of the pubic symphysis, leading to severe pelvic pain and mobility issues.
His initial work laid the foundation for subsequent research into this condition, both in surgical and non-surgical contexts, including its occurrence in athletes, during childbirth, and as a result of repetitive stress or trauma.
1930s-1950s: Recognition of osteitis pubis in athletes and other non-surgical cases, including during childbirth and trauma.
1970s-1980s: Broader awareness in sports medicine, particularly among soccer and hockey players, as an overuse injury.
2000s: Development of advanced imaging techniques, such as MRI and CT, improved diagnosis and management.
Osteitis pubis remains an area of active research, particularly in sports medicine, due to its impact on athletes’ performance and recovery times.
Symptoms of Osteitis Pubis
Osteitis pubis presents with a range of symptoms, primarily centered around pain and restricted mobility. These symptoms can significantly impact daily activities, particularly those involving movement or weight-bearing. Recognizing the hallmark signs is essential for early diagnosis and effective management.
Localized Pain in the Pubic Region
The most prominent symptom of osteitis pubis is localized pain in the pubic region, typically centered around the pubic symphysis. This pain often arises gradually and intensifies over time, particularly with physical activities that stress the pelvis. Activities such as running, jumping, or even prolonged standing can exacerbate the discomfort. The pain is usually sharp or aching in nature and may worsen when palpating the pubic symphysis. For many individuals, this localized pain serves as the first indication of the condition, prompting further investigation.
Pain Radiating to the Abdomen, Groin, or Thighs
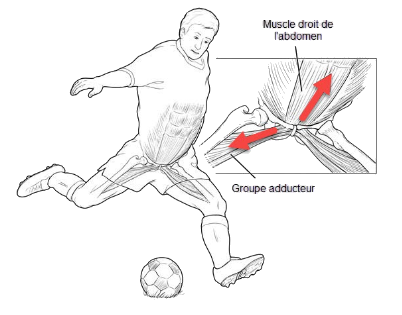
In addition to localized discomfort, osteitis pubis can cause pain that radiates to adjacent regions, including the lower abdomen, groin, or inner thighs. This radiating pain occurs because the pubic symphysis serves as a central junction for numerous muscles and ligaments, such as the adductors, rectus abdominis, and pelvic floor muscles. When inflammation or stress affects the joint, the interconnected structures may also experience tension or irritation, leading to referred pain. Athletes, in particular, often report groin pain that worsens during activities requiring sudden directional changes or repetitive motions.
Stiffness and Limited Mobility
Stiffness in the pelvic region is another hallmark symptom of osteitis pubis, particularly in the morning or after periods of inactivity. This stiffness can make it challenging to perform everyday activities, such as bending, sitting, or walking. Over time, the inflammation and resultant discomfort can lead to limited mobility, affecting both the pelvis and adjacent areas. The reduction in range of motion may also alter gait patterns, as individuals subconsciously adjust their movements to minimize pain. This compensatory mechanism can strain other parts of the body, potentially leading to secondary issues such as hip or lower back pain.
Additional Considerations
While these primary symptoms are common, the severity and combination of symptoms can vary depending on the underlying cause and the individual’s activity level. For example, athletes often experience sharper pain during high-intensity activities, while non-athletic individuals may notice a dull, persistent ache. Regardless of the presentation, early recognition and intervention are critical to preventing further complications and restoring normal function.
Causes of Osteitis Pubis
Osteitis pubis arises from various causes, ranging from mechanical stress to infections, and is influenced by several risk factors. Understanding these underlying causes and contributing elements is crucial for accurate diagnosis, prevention, and management.
Overuse and Repetitive Stress
One of the primary causes of osteitis pubis is overuse and repetitive stress on the pubic symphysis. Activities that involve frequent or intense use of the pelvic region—such as running, kicking, or jumping—can place excessive strain on the joint and surrounding tissues. This repeated stress leads to inflammation and microtrauma, disrupting the joint’s ability to function effectively. Athletes, particularly those involved in high-impact sports like soccer, rugby, and long-distance running, are especially prone to developing osteitis pubis due to the repetitive load placed on the pelvis.
Direct Trauma and Injuries
Traumatic events, such as a fall or a direct blow to the pelvis, can also cause osteitis pubis. Such injuries may disrupt the stability of the pubic symphysis or damage the surrounding soft tissues, leading to inflammation and pain. Additionally, surgical procedures involving the pelvic region—such as hernia repairs or gynecological surgeries—can sometimes lead to post-surgical complications that contribute to the condition. The disruption of tissue integrity around the pubic symphysis can impair healing and predispose individuals to chronic inflammation.
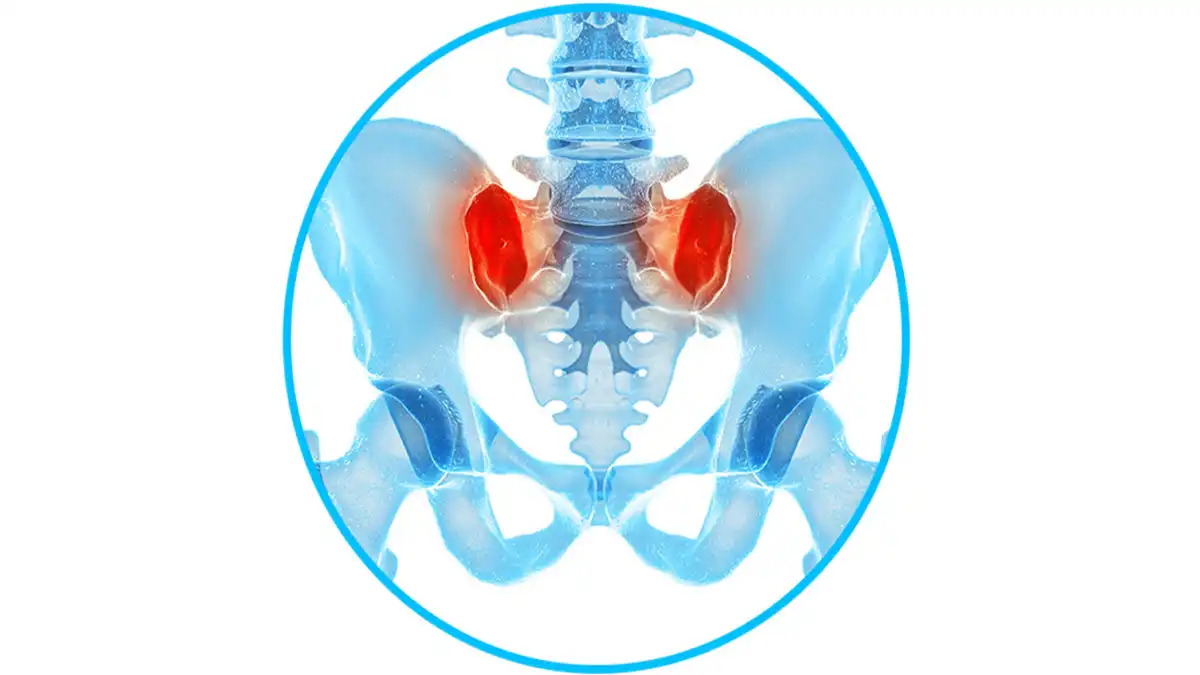
Muscle Imbalances and Poor Posture
Muscle imbalances or weaknesses in the pelvic and core musculature can contribute to abnormal forces on the pubic symphysis. For instance, tight hip flexors, weak abdominal muscles, or overactive adductor muscles can lead to uneven stress distribution across the pelvis, increasing the risk of inflammation. Similarly, poor posture—such as excessive pelvic tilt or lumbar lordosis—can alter the biomechanics of the pelvis, creating additional strain on the pubic symphysis during everyday movements or physical activities.
Anatomical Variations and Infections
Anatomical variations, such as a misaligned pelvis or leg length discrepancies, can predispose individuals to osteitis pubis by altering the natural alignment and movement of the pelvic region. In rare cases, infections can also cause osteitis pubis. Bacterial infections, often post-surgical or due to pelvic trauma, can lead to septic inflammation of the pubic symphysis, a condition known as septic osteitis pubis. This variant requires urgent medical attention to prevent complications.
Risk Factors: Sports, Gender, and Age
Participation in specific sports is one of the most significant risk factors for osteitis pubis. Athletes engaged in activities involving repetitive pelvic motion are at the highest risk. Gender and age also play a role; males, particularly in their 20s and 30s, are more commonly affected, potentially due to higher engagement in high-impact sports. Pregnant women may also develop osteitis pubis due to hormonal changes and increased stress on the pelvis during childbirth.
Pathophysiology of Osteitis Pubis
Osteitis pubis is an inflammation of the pubic bone, located at the front of the pelvis. It is often associated with athletic activities, especially those that involve repetitive movements or direct trauma to the pubic region. Here is a step-by-step explanation of the pathophysiology of osteitis pubis:
- Repetitive Stress or Trauma:
- Stage 1: Exposure to Stress – Osteitis pubis can be triggered by sports activities or repetitive movements that put excessive stress on the pubic area. This can include sports such as football, hockey, rugby, or activities that require frequent changes of direction.
- Microtrauma and Inflammation:
- Step 2: Microtrauma – Repetitive movements or direct trauma can cause microtrauma to the pubic area. These microtraumas can cause damage to the pubic bone.
- Inflammatory Response:
- Stage 3: Inflammatory Response – Microtrauma triggers a local inflammatory response in the affected area of the pubic bone. This inflammation is a natural reaction of the body to heal damaged tissue.
- Pain and Swelling:
- Stage 4: Pain – Inflammation causes localized pain in the pubic area. Pain may be felt during physical activity, movement, or even at rest.
- Stage 5: Swelling – In response to inflammation, there may be some degree of swelling in the affected area.
- Formation of Lesions and Calluses:
- Step 6: Lesion Formation – Repetitive microtrauma can lead to lesion formation in the pubic bone. These lesions may involve cracks or areas of fragility.
- Stage 7: Callus Formation – In response to injury, the body may form a bone callus in the affected area, in an attempt to strengthen the bone.
- Alteration of Bone Architecture:
- Step 8: Bone Structure Alteration – Over time, repeated injury and callus formation can lead to alteration of the bony architecture of the pubis. This can affect the strength of the bone.
- Persistent Symptoms:
- Stage 9: Persistence of Symptoms – Symptoms such as pain and swelling may persist, even after the activity that initially triggered the osteitis pubis has ceased.
Diagnosis
Accurate diagnosis of osteitis pubis is essential to ensure appropriate treatment and recovery. It involves a combination of patient history, physical examination, and imaging techniques to confirm the condition and assess its severity.
Patient History and Physical Examination
Taking a detailed patient history is the first step in diagnosing osteitis pubis. Key aspects include:
- Symptoms: Patients often report localized pain in the pubic region, which may radiate to the lower abdomen, groin, or inner thighs. Pain is typically exacerbated by activities that stress the pelvic area, such as running, kicking, or prolonged sitting.
- Onset and Duration: Understanding when the symptoms began and whether they are related to specific activities or injuries helps identify potential triggers, such as overuse or direct trauma.
- Activity History: Inquiring about sports participation, training intensity, or any sudden increase in physical activity can provide clues about the cause.
- Associated Factors: Any history of previous pelvic injuries, infections, or underlying conditions like arthritis should be considered.
A thorough physical examination involves:
- Palpation: The pubic symphysis is palpated to identify tenderness or swelling. Pain on palpation is a hallmark sign of osteitis pubis.
- Mobility Tests: Assessing the range of motion of the pelvic joint and surrounding areas helps evaluate stiffness or mobility limitations.
- Functional Tests: Tests involving resisted movements or weight-bearing activities can reproduce symptoms and indicate functional impairments.
Imaging Techniques
Imaging plays a crucial role in confirming the diagnosis of osteitis pubis and excluding other conditions. Common modalities include:
X-rays:
- X-rays are often the initial imaging choice. They can reveal:
- Widening of the pubic symphysis: Indicates joint instability.
- Erosion or sclerosis: Reflects inflammation or degenerative changes.
- Fracture lines or cracks: Seen in cases of severe stress on the pubic joint.
MRI (Magnetic Resonance Imaging):
- MRI is more sensitive than X-rays and is particularly useful for detecting early-stage inflammation and soft tissue involvement.
- It provides detailed visualization of:
- Bone marrow edema.
- Inflammatory changes in the surrounding muscles and ligaments.
- Subtle structural damage not visible on X-rays.
CT Scans (Computed Tomography):
- CT scans may be used for detailed evaluation of bone abnormalities.
- They are helpful in detecting small fractures, joint misalignments, or chronic changes in the bone structure.
Treatment Approaches for Osteitis Pubis: Emphasis on Osteopathy
Managing osteitis pubis requires a comprehensive and individualized treatment approach. Osteopathy plays a crucial role in addressing the underlying biomechanical issues, reducing pain, and promoting recovery. Here’s an overview of effective treatment strategies:
Rest and Activity Modification
- Rest: Resting the affected area is critical to allow inflammation to subside. Patients should avoid activities that exacerbate pain, such as running, kicking, or heavy lifting.
- Activity Modification: Low-impact exercises like swimming or cycling can maintain fitness without stressing the pubic symphysis. Gradual reintroduction of activities is essential as symptoms improve.
Osteopathic Insight:
An osteopath evaluates the patient’s activity patterns to identify and address movements that may overload the pelvic region. They provide tailored advice on safe exercises and modifications.
Pain Management: Medications and Injections
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to reduce inflammation and alleviate pain.
- Corticosteroid Injections: In severe cases, localized injections may be used to manage persistent inflammation and provide temporary relief.
Osteopathic Insight:
While osteopaths do not prescribe medications, they focus on manual techniques to reduce reliance on pharmaceuticals by improving biomechanics and easing pain naturally.
Physical Therapy and Rehabilitation Exercises
- Strengthening: Exercises targeting the core muscles, including the transverse abdominis and pelvic stabilizers, are crucial for restoring stability and function.
- Flexibility: Stretching tight muscle groups, such as the adductors and hip flexors, helps reduce tension on the pubic symphysis.
- Progressive Rehabilitation: Gradual progression in intensity ensures the pelvic region adapts safely to increased demands.
Osteopathic Insight:
Osteopaths integrate rehabilitation exercises with manual therapy to enhance muscle function and promote balanced force distribution across the pelvis. They may also address muscle imbalances contributing to the condition.
Osteopathic Interventions for Pelvic Alignment
Osteopathy offers a holistic approach to treating osteitis pubis by focusing on the structural and functional relationships within the body. Key osteopathic techniques include:
- Joint Mobilization: Gentle mobilization of the pubic symphysis and adjacent joints restores optimal movement and alignment.
- Myofascial Release: Targeted techniques relieve tension in the soft tissues surrounding the pelvis, reducing strain on the pubic symphysis.
- Pelvic Balancing: Addressing imbalances in the pelvic girdle, sacroiliac joint, and lumbar spine helps normalize force distribution and relieve stress on the pubic joint.
- Postural Assessment and Correction: Osteopaths analyze and correct postural deviations that contribute to excessive pelvic strain.
- Whole-Body Approach: Osteopathy considers the entire kinetic chain, addressing compensatory patterns in the legs, spine, and upper body that may exacerbate symptoms.
Incidence of Osteitis Pubis
It is a disease that occurs between the ages of 20 and 40, women are more frequently affected than men.
Risk factors for osteitis pubis
Certain risk factors can increase the likelihood of developing osteitis pubis. These factors are often related to specific physical activities, anatomical features, or other medical conditions. Here are some of the risk factors associated with osteitis pubis:
- Participation in specific sports: Athletes involved in sports requiring repetitive movements, frequent changes of direction, impacts or intense efforts, such as football, soccer, hockey, rugby, are at greater risk of osteitis pubis.
- Overuse: Intense physical activity or excessive training can increase the risk of overloading the pubic joint, leading to inflammation.
- Muscle Imbalances: Imbalances in the strength of the muscles surrounding the pubic joint can increase uneven pressure on this area, promoting the development of inflammation.
- Poor training technique: Incorrect training technique, including improper movements or sudden overload, can contribute to the risk of osteitis pubis.
- Anatomical conditions: Certain anatomical variations, such as abnormalities in the structure of the pelvis or lower limbs, may increase susceptibility to osteitis pubis.
- Postural problems: Postural problems or pelvic misalignments can increase pressure on the pubic symphysis.
- History of pelvic injuries: People with prior pelvic injuries or trauma may be more likely to develop osteitis pubis.
- Gender: Osteitis pubis is more common in men, especially male athletes.
- Age: Although it can affect individuals of any age, osteitis pubis is often seen in young adults and active athletes.
It is important to note that the presence of these risk factors does not guarantee the development of osteitis pubis, and some people can develop the condition without having these factors.
Exercise
A structured exercise program plays a vital role in recovering from osteitis pubis by reducing pain, restoring function, and preventing recurrence. Exercises should focus on strengthening the core and pelvic stabilizers, improving flexibility, and addressing imbalances in the surrounding muscles. Here’s a detailed look at effective exercises, including osteopathic insights to optimize recovery.
Transverse Abdominis Rehabilitation
The transverse abdominis (TrA) is a deep core muscle essential for pelvic stability. Strengthening it helps alleviate strain on the pubic symphysis and supports recovery.
Exercise: Abdominal Draw-In Maneuver
- Lie on your back with your knees bent and feet flat on the floor.
- Gently draw your belly button toward your spine, engaging your deep abdominal muscles without lifting your ribcage.
- Hold the contraction for 5–10 seconds while breathing normally.
- Relax and repeat for 10–15 repetitions, 3–4 times daily.
Osteopathic Insight:
An osteopath can guide proper activation of the TrA and ensure that other muscle groups are not compensating during the exercise.
Strengthening Exercises
Targeting muscles around the pelvis helps improve stability and reduce uneven forces on the pubic symphysis. Key strengthening exercises include:
- Clamshells: Strengthens the gluteus medius to improve pelvic alignment.
- Lie on your side with knees bent and feet together.
- Lift your top knee while keeping your feet in contact, then lower.
- Perform 10–15 repetitions per side, 2–3 sets.
- Bridges: Activates the glutes and core.
- Lie on your back with knees bent and feet hip-width apart.
- Lift your hips toward the ceiling, engaging your glutes and core.
- Hold for 3–5 seconds and lower slowly. Repeat for 10–12 reps.
Flexibility Exercises
Tight muscles can place additional stress on the pubic symphysis. Stretching these muscles helps reduce tension and restore balance.
- Adductor Stretch:
- Sit with the soles of your feet together and knees apart.
- Gently press your knees toward the floor while keeping your back straight.
- Hold for 20–30 seconds and repeat 2–3 times.
- Hip Flexor Stretch:
- Kneel on one knee with the other foot in front, forming a 90-degree angle.
- Shift your weight forward slightly to stretch the hip flexors.
- Hold for 20–30 seconds per side.
Other Recovery Exercises
To address full-body mechanics, include exercises that enhance coordination and overall stability.
- Pelvic Tilts: Improves pelvic mobility and strengthens core muscles.
- Lie on your back with knees bent.
- Flatten your lower back against the floor by tilting your pelvis upward.
- Hold for a few seconds, then release. Repeat for 10–15 reps.
- Single-Leg Balance:
- Stand on one leg and maintain balance for 20–30 seconds.
- To increase difficulty, add slight movements with the opposite leg or close your eyes.
Progressive Rehabilitation
As pain decreases, gradually introduce functional exercises like squats, lunges, and low-impact activities (e.g., swimming or cycling) to rebuild strength and endurance. Always prioritize form and avoid movements that exacerbate pain.
Osteopathic Support During Recovery
Osteopathy complements exercise programs by addressing muscle imbalances, improving joint mobility, and optimizing alignment. Osteopaths may:
- Assess and correct pelvic misalignments.
- Guide safe progression of exercises tailored to the patient’s condition.
- Provide manual therapy to reduce tension in overactive muscles and improve flexibility.
Key Considerations
- Begin exercises under the supervision of a healthcare provider or osteopath.
- Focus on pain-free movements; stop any exercise that causes discomfort.
- Consistency is key—perform exercises regularly for the best results.
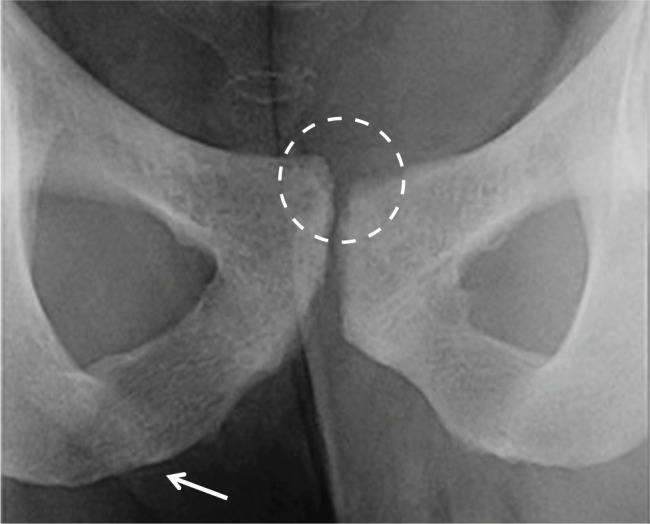
Osteitis Pubis X-ray
Radiographic signs of osteitis pubis can vary and can sometimes be subtle. It is important to note that in many cases, changes may not be evident on plain radiographs, and more advanced imaging techniques, such as MRI (magnetic resonance imaging) or CT scans, may be necessary for a more detailed evaluation. However, here are some possible radiographic signs that may be seen in advanced or chronic cases:
- Widening of the pubic symphysis: Osteitis pubis can sometimes cause widening of the pubic joint, which may be visible on x-rays.
- Erosion or degenerative changes: Signs of bone erosion or degenerative changes may be seen at the pubic symphysis.
- Bone sclerosis: Thickening or densification of the bone around the pubic symphysis may be a sign of a reaction to inflammation.
- Fracture line or cracks: In some cases, fracture lines or cracks may be visible, reflecting a response to excessive stress on the pubic joint.
It is important to note that radiographic changes may not be evident early in the condition. MRI is often more sensitive for detecting early signs of inflammation and soft tissue changes around the pubic joint.
X-rays show erosion, sclerosis and widening of the pubic symphysis.
References
- Via AG, Frizziero A, Finotti P, Oliva F, Randelli F, Maffulli N. Management of osteitis pubis in athletes: rehabilitation and return to training – a review of the most recent literature. Open Access J Sports Med. 2019;10:1-10. [ PMC free article ] [ PubMed ]
- Lynch TS, Bedi A, Larson CM. Athletic Hip Injuries. J Am Acad Orthop Surg. 2017 Apr;25(4):269-279. [ PubMed ]
- Weber MA, Rehnitz C, Ott H, Streich N. Groin Pain in Athletes. Rofo. 2013 Aug 23; [ PubMed ]
- Johnson R. Osteitis pubis . Curr Sports Med Rep. 2003 Apr;2(2):98-102. [ PubMed ]
- Hiti CJ, Stevens KJ, Jamati MK, Garza D, Matheson GO. Athletic osteitispubis . Sports Med. 2011 May 01;41(5):361-76. [ PubMed ]
- Akgün AS, Agirman M. Association between cam-type femoroacetabular impingement and osteitispubis in non-athletic population on magnetic resonance imaging. J Orthop Surg Res. 2019 Oct 22;14(1):329. [ PMC free article ] [ PubMed ]
- Phillips E, Khoury V, Wilmot A, Kelly JD. Correlation Between Cam-Type Femoroacetabular Impingement and Radiographic Osteitis Pubis . Orthopedics. 2016 May 01;39(3):e417-22. [ PubMed ]
- Birmingham PM, Kelly BT, Jacobs R, McGrady L, Wang M. The effect of dynamic femoroacetabular impingement on pubic symphysis motion: a cadaveric study. Am J Sports Med. 2012 May;40(5):1113-8. [ PubMed ]
- Gomella P, Mufarrij P. Osteitis pubis : A rare cause of suprapubic pain. Rev Urol. 2017;19(3):156-163. [ PMC free article ] [ PubMed ]
- Lentz SS. Osteitis pubis : a review. Obstet Gynecol Surv. 1995 Apr;50(4):310-5. [ PubMed ]
- Economopoulos KJ, Milewski MD, Hanks JB, Hart JM, Diduch DR. Radiographic evidence of femoroacetabular impingement in athletes with athletic pubalgia. Sports Health. 2014 Mar;6(2):171-7. [ PMC free article ] [ PubMed ]
- Verrall GM, Hamilton IA, Slavotinek JP, Oakeshott RD, Spriggins AJ, Barnes PG, Fon GT. Hip joint range of motion reduction in sports-related chronic groin injury diagnosed as pubic bone stress injury. J Sci Med Sports. 2005 Mar;8(1):77-84. [ PubMed ]
- Saito M, Utsunomiya H, Hatakeyama A, Nakashima H, Nishimura H, Matsuda DK, Sakai A, Uchida S. Hip Arthroscopic Management Can Improve Osteitis Pubis and Bone Marrow Edema in Competitive Soccer Players With Femoroacetabular Impingement. Am J Sports Med. 2019 Feb;47(2):408-419. [ PubMed ]