Introduction to Lumbosacral Facet Syndrome
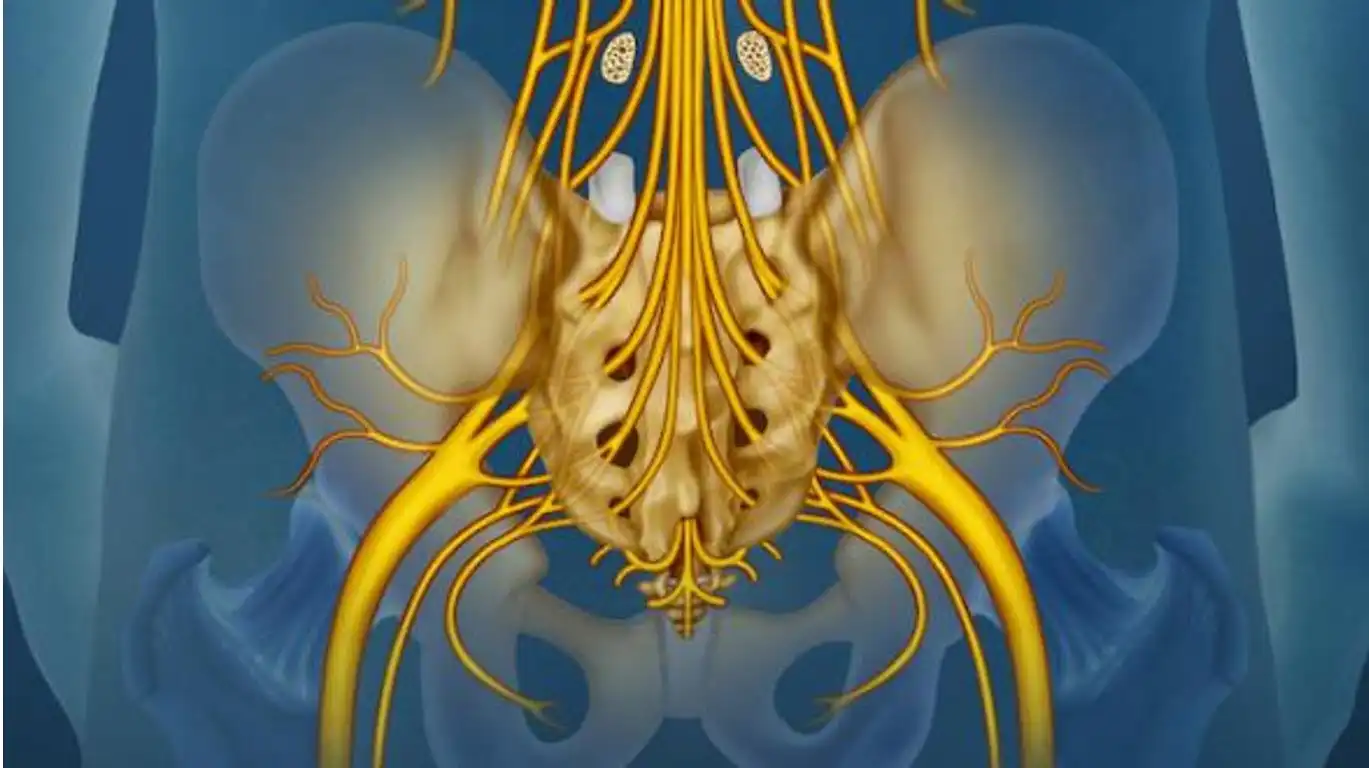
Lumbosacral facet syndrome, often referred to as facet low back pain, is a medical condition affecting the small joints located between the lumbar vertebrae, which make up the lower part of the spine, and the sacrum. These joints, known as the lumbosacral facets, play a vital role in maintaining mobility and stability of the spine.
Anatomically, the lumbosacral facets are synovial joints that lie on either side of the spine, forming connections between the lumbar vertebrae and the upper part of the sacrum. They are covered in cartilage and surrounded by a joint capsule that contains synovial fluid, thus promoting fluidity of movement. These small joints allow a variety of movements, including flexion, extension, and rotation of the lumbar spine.
When lumbosacral facet syndrome occurs, these joints can become inflamed or degenerate, leading to painful symptoms. Pain, the predominant symptom of this condition, is usually located in the lower back region, highlighting the direct impact on the functionality of this part of the spine.
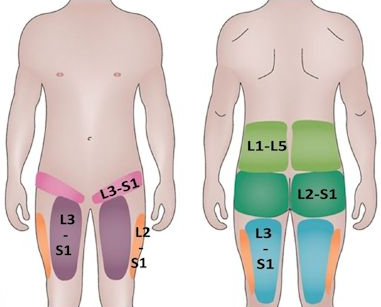
Pain associated with lumbosacral facet syndrome may also radiate to other areas, such as the buttocks, hips, or thighs, depending on the specific location of the affected facets and adjacent nerves. Stiffness in the spine, resulting from inflammation, can limit mobility and make movement in the lower back more difficult.
Diagnosis of this syndrome typically involves a thorough clinical evaluation, taking into account the patient’s medical history, detailed physical examinations, and sometimes medical imaging procedures such as X-rays or MRIs to confirm the presence of lesions at the lumbosacral facets.
In terms of management, therapeutic approaches often aim to reduce inflammation and relieve pain. Conservative treatments may include osteopathy, the use of anti-inflammatory medications, corticosteroid injections, as well as muscle strengthening exercises to stabilize the lumbar region.
Understanding the anatomical and clinical nuances of lumbosacral facet syndrome is crucial for early identification, accurate diagnosis, and effective management of this condition that can significantly impact the quality of life of affected individuals.
Mechanisms and causes
Lumbosacral facet syndrome is a painful lower back condition that results from irritation or degeneration of the facet joints, the small joints at the back of each vertebra that allow and limit movement of the spine. To understand the potential causes of this syndrome, it is essential to examine the mechanisms and factors that can affect these joints and lead to the development of chronic pain.
Repetitive movements and mechanical overload
One of the main mechanisms of lumbosacral facet syndrome is repetitive movements, especially those involving flexion, twisting, or extension of the spine. These movements, when performed excessively or under poor conditions, can lead to mechanical overload on the facet joints. For example, manual workers, athletes, or even people who adopt awkward positions in their daily lives, such as frequent bending, are more likely to develop microtraumas at the facet level. These microtraumas, over time, can cause premature wear of the articular cartilage, leading to irritation and pain.
Bad postures
Posture also plays a crucial role in the development of lumbosacral facet syndrome. Poor posture, such as prolonged sitting with a hunched back or adopting asymmetrical positions, can place excessive stress on the facet joints. When the spine is misaligned, the facets have to bear more load than they are designed to, which accelerates their wear. In addition, prolonged poor posture can lead to muscle imbalance, with muscles tight on one side and weak on the other, further increasing the stress on the facet joints.
Aging and degeneration
Aging is another key factor in the development of lumbosacral facet syndrome. As we age, the cartilage in the facet joints naturally wears down, and the intervertebral discs lose height and elasticity. This disc degeneration can increase the pressure on the facets as they have to compensate for the lack of support from the discs. In addition, the wear of the cartilage exposes the facet bones to direct contact, which can lead to the formation of osteophytes (bony growths), making movement painful and limited. This progressive degradation can be exacerbated by genetic factors, a sedentary lifestyle, or a history of back injuries.
Trauma and injuries
Trauma, whether acute or repeated, is a common cause of lumbosacral facet disorders. Acute trauma, such as a fall, car accident, or sudden misalignment, can cause displacement or microfracture of the facets. These injuries can then progress to chronic pain if not properly treated. Repeated injuries, even minor ones, can also accumulate damage over time, leading to chronic inflammation of the facets and weakening of their structure.
Impact of repeated microtraumas
Repetitive strain injuries are a common cause of lumbosacral facet degeneration. These strain injuries occur when even small, everyday movements are performed repeatedly without adequate recovery time. Activities such as heavy lifting, repeated twisting of the trunk, or even poor posture over time can cause minor facet injuries. Although individual injuries are often too small to cause immediate symptoms, accumulating over time can lead to progressive degradation of the facets. This process of continued wear and tear can make the facets more susceptible to injury and inflammation, contributing to chronic pain. Preventing strain injuries includes improving posture, adopting proper lifting techniques, and incorporating adequate rest periods into physical activities.
Muscle imbalances
Muscle imbalances play a significant role in the development of lumbosacral facet syndrome. When certain muscles in the lumbar region are too tight or too weak, they can alter the alignment of the spine, causing overload on the facet joints. For example, overly tight hip flexor muscles can pull the spine forward, accentuating lumbar lordosis and increasing pressure on the facets. Similarly, weak lumbar extensor muscles may not provide adequate support, leading to spinal instability. This muscle imbalance can be the result of poor posture, lack of exercise, or poor movement habits. Over the long term, these tensions and weaknesses can cause microtrauma to the facets, contributing to their degeneration and the development of chronic pain.
Degeneration of intervertebral discs
Intervertebral disc degeneration is a key mechanism in the development of lumbosacral facet syndrome. The discs, located between the vertebrae, act as shock absorbers, absorbing shock and facilitating movement. With age, the discs lose their elasticity and height, reducing their ability to support spinal load. As a result, more pressure is transferred to the facet joints, which must compensate for this loss of support. This overload can accelerate the wear of the facet cartilage, causing pain and inflammation. Disc degeneration can also lead to a decrease in the intervertebral space, which can lead to compression of adjacent nerves and exacerbate symptoms. This mechanism underscores the importance of maintaining intervertebral disc health to prevent facet-related pain.
Risk Factors
- Age: The risk of developing lumbosacral facet syndrome generally increases with age due to the natural degeneration of the joints.
- Genetics: Genetic predispositions may make some people more prone to joint conditions, increasing their vulnerability to lumbosacral facet syndrome.
- Sedentary lifestyle: A sedentary lifestyle can contribute to poor posture and weakened supporting muscles, thereby promoting the development of the condition.
- Obesity: Excess weight can increase the pressure on the lumbosacral facets, increasing the risk of inflammation and pain.
- Intense Physical Activities: Certain physical activities, particularly those involving repetitive movements or significant loading on the spine, can increase the risk of facet injuries.
- Structural Disorders: Anatomical abnormalities or pre-existing medical conditions, such as spinal malformations, may contribute to the development of lumbosacral facet syndrome.
Understanding these mechanical causes and risk factors allows healthcare professionals to design personalized treatment and prevention approaches. By identifying and mitigating these elements, it is possible to reduce the frequency and severity of lumbosacral facet syndrome, thereby improving the quality of life of affected individuals.
Symptoms
Symptoms of lumbosacral facet syndrome, also known as facet back pain, can vary from person to person. This condition affects the small joints between the lumbar vertebrae and the sacrum, called the lumbosacral facets. Common symptoms associated with this syndrome include:
- Lower Back Pain: Pain in the lower back region is the main symptom. It can be described as a deep, stabbing pain, usually located on the side or in the middle of the lower back.
- Pain Radiation: Pain may radiate to the buttocks, hips, or even thighs. The exact area often depends on the specific location of the affected facets.
- Muscle Stiffness: A feeling of stiffness in the spine, especially after prolonged periods of inactivity, may be felt.
- Decreased Mobility: People with the condition may experience decreased mobility in the spine, making movement difficult or uncomfortable.
- Pain Aggravated by Movement: Pain may be exacerbated by certain movements, such as bending back, rotating the trunk, or even simple daily activities.
- Pain Improved at Rest: Rest may temporarily relieve pain, but it may return with activity.
- Occasional Blockages: Some patients report feelings of blocking or jamming, associated with increased discomfort during movement.
- Response to Changes in Position: Pain may vary depending on body position, with worsening with prolonged sitting or standing.
- Targeted Pain on Palpation: On physical examination, palpation of the lumbosacral facets may elicit local pain.
Pathophysiology
The pathophysiology of lumbosacral facet syndrome involves the facet joints, which are located at the back of the spine. These joints are formed by the articular surfaces of adjacent vertebrae and are responsible for the mobility and stability of the spine.
Lumbosacral facet syndrome is characterized by irritation or inflammation of the facet joints, usually in the lumbar or sacral region of the spine. Here are some aspects of the pathophysiology associated with this condition:
- Joint wear: Over time, facet joints can experience wear due to repetitive motions, overload, abnormal positions, or other factors. This wear can lead to increased friction between the joint surfaces, causing irritation.
- Joint hypertrophy: In response to wear and tear or repeated stress, the facet joints can develop hypertrophy, which means abnormal growth of bone tissue. This hypertrophy can lead to compression of surrounding structures, including nerves.
- Inflammation: Constant irritation of the facet joints can trigger an inflammatory response. Inflammation can lead to thickening of the structures surrounding the joints, exacerbating nerve compression and causing pain.
- Nerve compression: Irritation and inflammation of the facet joints can lead to compression of adjacent nerve roots. This can cause local pain in the lumbar region, as well as pain radiating along the compressed nerve, often into the buttocks, thighs, or legs.
- Muscle spasms: In response to pain and irritation, surrounding muscles may reflexively contract, causing muscle spasms. These spasms can contribute to pain and limited mobility.
- Development of synovial cysts: In some cases, irritation of the facet joints can lead to the formation of synovial cysts, which are sacs filled with synovial fluid. These cysts can put additional pressure on nearby structures, worsening symptoms.
The pathophysiology of lumbosacral facet syndrome is complex and can vary from person to person. Genetics, aging, trauma, excess weight, and other factors may contribute to the development of this condition. Understanding these mechanisms allows healthcare professionals to implement targeted treatment approaches to relieve symptoms and improve the quality of life of those affected.
Possible complications
Lumbosacral facet syndrome, if not properly managed, can lead to various complications that affect the patient’s quality of life and overall health. Understanding these complications is essential to emphasize the importance of early diagnosis and appropriate management.
Chronicity of pain
One of the most common complications of untreated lumbosacral facet syndrome is chronic pain. Over time, the initial acute pain can progress to persistent pain, which can become increasingly difficult to manage. Chronic pain is not limited to physical discomfort; it can also have significant psychological impacts, such as anxiety, depression, and decreased quality of life. Patients with chronic pain may also develop central sensitization, a phenomenon in which the nervous system becomes hyperreactive to painful stimuli. This can make even normal daily activities painful and lead to a progressive increase in pain perception, making its treatment even more complex.
Reduced mobility
Another major complication is reduced mobility. The facet joints play a key role in stabilizing and providing flexibility to the spine. When these joints are damaged or inflamed, spinal movement becomes limited and painful. Patients may have difficulty bending, twisting, or performing movements that require flexion or extension of the lumbar spine. This reduced mobility can lead to muscle stiffness and weakening of the back muscles, further exacerbating functional limitations. Over time, loss of mobility can also lead to muscle atrophy, worsening symptoms and making recovery even more difficult.
Development of other spinal pathologies
Failure to treat lumbosacral facet syndrome can also promote the development of other spinal pathologies. For example, in response to pain and limited mobility, patients may adopt compensatory postures or abnormal movement patterns to avoid worsening their symptoms. These adjustments can, in turn, lead to overloading other parts of the spine, hips, or knees, causing pain and impairment in these areas. In addition, continued wear and tear on the facet joints can lead to the formation of osteophytes (bony growths), which can cause additional pain and further limit mobility. In severe cases, these osteophytes can even lead to spinal stenosis, a condition in which the spinal canal narrows, compressing spinal nerves and causing neurological symptoms such as radiating pain, numbness, or weakness in the lower extremities.
Impact on quality of life
Together, these complications can have a significant impact on quality of life. Chronic pain, reduced mobility, and the development of secondary pathologies can make daily activities difficult or impossible to perform. Patients may have difficulty walking, sitting, or standing for long periods of time, limiting their ability to work, engage in hobbies, or interact socially. Social isolation, loss of independence, and frustration associated with not being able to perform normal activities can lead to psychological problems, exacerbating the cycle of pain and health decline.
Global postural dysregulation
Failure to treat lumbosacral facet syndrome can result in global postural dysregulation, which manifests as a change in the natural curvatures of the spine. This dysregulation is often a consequence of subconscious bodily adjustments that patients make to avoid pain. For example, to reduce pressure on the lumbar facets, a patient may exaggerate the lordotic (hollow) curve of the lumbar region or, conversely, adopt a more flexed posture to temporarily relieve discomfort.
These posture changes are not limited to the lumbar region. They can affect the entire spine, causing compensations in the thoracic and cervical regions. For example, lumbar hyperlordosis can cause thoracic hyperkyphosis, where the upper back becomes more rounded. These changes can in turn cause pain in other parts of the body, such as the shoulders, neck, and even the head, due to the excessive strain on the muscles and ligaments that are trying to stabilize these new postures.
Global postural imbalance can also lead to lower limb inequality, where one side of the pelvis is higher than the other, creating an asymmetry in leg length. This condition can exacerbate lower back pain and create new problems, such as pain in the hips, knees, and ankles.
Neurological complications
If left untreated, lumbosacral facet syndrome can progress to serious neurological complications. One of the most concerning complications is spinal stenosis, a condition in which the narrowing of the spinal canal puts pressure on the spinal cord and spinal nerves. This stenosis can be caused by the formation of osteophytes (bony growths) around the facet joints, which invade the space of the spinal canal.
Symptoms of spinal stenosis may include radiating pain, tingling, numbness, and weakness in the lower extremities. In advanced cases, patients may experience difficulty walking, loss of bladder or bowel control, or even partial paralysis. These neurological symptoms require immediate medical attention and, in some cases, surgery to decompress the affected nerves.
Another neurological risk is cauda equina syndrome , a medical emergency where compression of the nerves at the base of the spinal cord causes severe pain in the lower back and legs, as well as loss of sensation in the areas around the genitals and anus. This syndrome requires prompt surgery to prevent permanent nerve damage.
Psychosomatic disorders
Psychosomatic disorders are another potential complication of untreated lumbosacral facet syndrome. When pain becomes chronic, it can negatively influence the patient’s psychological state, creating a close connection between body and mind. Stress and anxiety caused by persistent pain can amplify painful sensations, creating a vicious cycle where physical discomfort feeds mental anguish, and vice versa.
This interaction can lead to psychosomatic disorders, where patients begin to experience physical symptoms that have no apparent medical cause, but are actually a result of their emotional state. For example, a patient with chronic lower back pain may develop chest pain, headaches, or gastrointestinal disturbances, all of which are aggravated by anxiety or depression.
These psychosomatic disorders can make diagnosis and treatment more complex, as they require a multidisciplinary approach that includes both physical care and psychological support. Ignoring the psychological impact of chronic pain can prolong the patient’s suffering and decrease the effectiveness of treatments.
Finally, the deterioration of mental and emotional status can impact the patient’s social and professional relationships. Irritability, fatigue, and decreased quality of life can lead to social isolation, decreased productivity at work, and loss of interest in activities once enjoyed, further exacerbating the consequences of the untreated syndrome.
Osteopathic Approaches to Treatment
Osteopaths take a holistic approach to treating lumbosacral facet syndrome, with a focus on restoring musculoskeletal balance, reducing pain, and improving joint function. Here are some of the specific methods and techniques osteopaths use in treating this condition:
- Joint Mobilizations: Mobilizations involve gentle, controlled movements of the joints to gradually improve their range of motion. This can help reduce stiffness associated with lumbosacral facet syndrome.
- Myofascial Release Techniques: Osteopaths use myofascial release techniques to relax the muscles and connective tissues around the lumbosacral facets. This can help reduce tension and improve flexibility.
- Therapeutic Exercises: Osteopaths often recommend specific exercises to strengthen the supporting muscles of the spine. This can help stabilize the lumbar region and prevent relapses.
- Lifestyle and Ergonomics Advice: Osteopaths provide lifestyle advice, including ergonomic adjustments at work and at home, to reduce pressure on the lumbosacral facets in everyday life.
- Patient Education: Osteopaths provide in-depth patient education about the condition, explaining contributing factors, pain mechanisms, and self-care techniques. This may include advice on posture, physical activity, and stress management.
- Relaxation Techniques: Stress reduction can help ease muscle tension and promote relaxation. Osteopaths may recommend relaxation techniques such as deep breathing and meditation.
- Incorporating Whole Body Exercise: Some osteopaths encourage forms of whole body exercise such as yoga or tai chi, which can promote flexibility, strength and body awareness.
Exercises and Rehabilitation
Osteopathic exercises and rehabilitation approaches aim to strengthen supporting muscles, improve stability, and promote better joint function in the lumbosacral region. It is crucial to personalize exercises to each individual’s specific needs. Before beginning any exercise program, it is recommended to consult a health professional for personalized advice. Here are some exercises and approaches commonly recommended in osteopathy:
- Strengthening the Abdominal Muscles:
- Transverse Abdominal Exercise: Lie on your back, bend your knees and gently engage the transverse abdominis muscle by pulling your belly button towards your spine. Hold the contraction for a few seconds and release. Repeat several times.
- Strengthening Back Muscles:
- Quadruped Lumbar Extension: On your knees and with your hands on the floor, perform a back extension by lifting one arm and the opposite leg simultaneously. Hold the position for a few seconds and alternate sides.
- Spinal Stabilization:
- Plank: Assume a plank position by supporting yourself on your forearms and toes, maintaining a straight body line. This position engages your deep stabilizer muscles.
- Spinal Mobility:
- Seated Spine Rotation: Sitting in a chair, rotate your upper body to one side, using your abdominal muscles and lower back to perform the rotation. Repeat on the other side.
- Stretching and Flexibility:
- Seated Knee-Elbow Curl: Sitting on the floor, bend one knee toward your chest while rotating your upper body toward that knee. Hold the position to stretch the muscles in your lower back.
- Pelvic Stabilization:
- Bridge Pelvic Raises: Lie on your back, bend your knees and slowly lift your pelvis by contracting your glutes. Hold the position at the top for a few seconds and then lower back down.
- Breathing Exercises:
- Diaphragmatic Breathing: Practice deep breathing using the diaphragm. Inhale deeply through the nose, expanding the belly, then exhale slowly through the mouth.
- Coordination and Balance Exercises:
- Heel-toe Walk: Walk with alternating heel-toe contact with each step to improve coordination and balance.
It is important to progress gradually in these exercises, adapting them according to individual tolerance.
Pain Management
Osteopathic pain management for lumbosacral facet syndrome involves an integrated approach that combines manual techniques, lifestyle advice, and specific exercises. The goal is to reduce pain, improve joint function, and prevent relapses. Here are some common osteopathic strategies for pain management associated with this syndrome:
- Myofascial Release:
- Myofascial release techniques are used to relax the muscles and connective tissues around the affected facets, helping to reduce tension and pain.
- Stabilization Exercises:
- Specific exercises aimed at strengthening the supporting muscles of the spine are recommended. This can help stabilize the lumbosacral region and reduce pressure on the facets.
- Targeted Stretches:
- Appropriate stretches may be prescribed to improve the flexibility of the surrounding muscles, which can relieve pressure on the lumbosacral facets.
- Lifestyle and Ergonomics Tips:
- Osteopaths provide advice on ergonomic adjustments at work and at home, as well as recommendations for maintaining healthy posture in everyday life.
- Stress Management:
- Stress management is often incorporated, as stress can contribute to increased muscle tension. Osteopaths may recommend relaxation techniques such as deep breathing and meditation.
- Heat or Cold Therapy:
- Application of hot or cold compresses may be recommended to relieve pain and inflammation in the lower back region.
- Breathing and Relaxation Techniques:
- Learning deep breathing and relaxation techniques can help reduce muscle tension and promote an overall state of well-being.
- Incorporation of Physical Activity:
- Advice on appropriate physical activity levels and recommendations for low-impact exercises can be provided to maintain mobility without worsening symptoms.
Differential Diagnosis
- Herniated disc: A herniated disc occurs when the jelly-like core of an intervertebral disc protrudes from its socket. This can cause compression of nerve roots and cause lower back pain.
- Lumbar Arthritis: Arthritis can affect the joints of the spine, causing pain, stiffness, and inflammation. Lumbar arthritis can be a cause of pain similar to that associated with lumbosacral facet syndrome.
- Spinal stenosis: Spinal stenosis occurs when the space in the spinal canal narrows, putting pressure on the spinal cord or nerve roots. This can cause lower back pain and associated symptoms, such as numbness or weakness in the legs.
- Spondylolisthesis: This condition occurs when vertebrae slip relative to each other, often in the lumbar region, causing pain and instability.
- Spinal infection: Spinal infections can cause symptoms such as low back pain, fever, and neurological deficits.
- Kidney disease: Certain kidney problems, such as kidney stones or kidney infections, can cause pain in the lower back.
- Tumors: Tumors of the spine can compress surrounding structures and cause lower back pain.
- Fibromyalgia: A condition characterized by widespread muscle pain, tender points, and fatigue.
Practical Patient Cases
Patient: Mrs. X, aged 45, residing on the South Shore of Montreal, presents with persistent lower back pain and associated stiffness. Symptoms are exacerbated by flexion and rotation of the trunk.
Initial Evaluation: After a thorough evaluation, including medical history and physical examination, the osteopath diagnoses lumbosacral facet syndrome. X-rays and imaging tests are performed to confirm the diagnosis.
Osteopathic Treatment Plan:
- Myofascial Release Techniques: Specific massages and stretches are used to relax the surrounding muscles.
- Stabilization Exercises: A personalized exercise program is prescribed to strengthen the supporting muscles.
- Lifestyle Advice: Ergonomic recommendations and advice on daily posture are provided.
- Pain Management: Pain management approaches, including advice on heat therapy, are integrated.
Follow-up and Results: After several sessions, Mrs. X reports a significant reduction in pain, improved mobility and a better quality of daily life. She continues to follow the treatment plan and to integrate the osteopath’s advice into her lifestyle.
Prevention of Lumbosacral Facet Syndrome
Lumbosacral facet syndrome is a condition that can be influenced by a variety of factors, including lifestyle. While it is not always possible to completely prevent this condition, certain healthy lifestyle habits can help reduce the risk of developing lumbosacral facet syndrome and alleviate symptoms. Here are some tips and recommendations:
- Maintain a healthy weight: Excess weight puts extra pressure on the spine and can increase the risk of lumbosacral facet problems. Maintaining a healthy weight through a balanced diet and exercise can help reduce this pressure.
- Get regular physical activity: Regular exercise strengthens the muscles that support the spine, which can help prevent facet problems. Activities such as swimming, walking, yoga, and strength training can be beneficial.
- Adopt good posture: Maintaining proper posture, whether sitting or standing, is essential to reduce pressure on the lumbosacral facets. Avoid remaining in the same position for long periods of time and take regular breaks if you work while sitting.
- Practice regular stretching: Gentle stretching can help maintain flexibility in the spine and surrounding muscles. Targeted stretching may be recommended by a healthcare professional or osteopath.
- Avoid sudden movements and heavy lifting: Jerky movements or lifting heavy loads can put excessive pressure on the lumbosacral facets. Use proper lifting techniques and seek assistance when handling heavy objects.
- Maintain adequate hydration: Water is essential for healthy spinal discs. Make sure you stay well hydrated to maintain the flexibility of spinal tissues.
- Consult a healthcare professional: If you experience persistent symptoms or lower back pain, consult a healthcare professional, such as a physician or osteopath. Early diagnosis and an appropriate treatment plan can help prevent the progression of lumbosacral facet syndrome.
Myofascial compression technique
Myofascial release therapy is a widely used therapeutic approach to treat a variety of musculoskeletal conditions, including lumbosacral facet syndrome. The technique aims to release tension built up in myofascial tissues, which include muscles and fascia, a dense connective tissue that surrounds and supports muscles, bones, and other body structures. Tension in these tissues can restrict movement, cause pain, and contribute to postural imbalances.
Principles of the myofascial technique
Myofascial Release Therapy is based on the principle that restrictions and adhesions in the myofascial tissues can disrupt the body’s normal function, leading to pain and dysfunction. These restrictions can be caused by a variety of factors, such as trauma, overuse, chronic stress, or poor posture. By applying sustained, precise pressure to these tight areas, the goal is to release the adhesions, restore tissue mobility, and relieve pain.
Muscles often affected
Certain muscle areas are more likely to accumulate myofascial tension, especially in patients with chronic pain. Commonly affected muscles include:
- Erector spinae : This group of muscles supports the spine and plays a crucial role in maintaining posture. Tension in these muscles can cause lower back pain and stiffness.
- The latissimus dorsi muscle : Involved in shoulder and trunk movements, the latissimus dorsi can accumulate tension due to poor posture or repetitive movements.
- Quadratus Lumborum Muscle : Located in the lumbar region, this muscle is often responsible for lower back pain, especially when bending or extending the trunk.
- Hamstrings : These muscles located at the back of the thigh are often tight in people who sit for long periods of time, which can affect posture and mobility.
- Piriformis Muscle : Located in the gluteal region, the piriformis can cause pain that radiates down the leg due to compression of the sciatic nerve.
- Iliopsoas muscle : This hip flexor muscle can accumulate tension in people who spend a lot of time sitting, contributing to lower back pain and postural imbalances.
- Trapezius and Rhomboid Muscles : Located in the upper back, these muscles can build up tension due to stress or poor posture, causing neck and shoulder pain.
Procedure and application
Myofascial treatment begins with a careful assessment of the patient to identify areas of tension and restriction, particularly in the muscles mentioned above. The therapist palpates the tissues to locate areas of tightness, often felt as knots or cords in the muscles and fascia. Once these areas are identified, the therapist applies firm but controlled manual pressure directly to the affected areas.
Pressure is maintained for a period of time, often several minutes, to allow the tissues to gradually soften. Unlike conventional massage techniques that focus on superficial muscles, myofascial release targets the deeper layers of connective tissue. This slow, sustained pressure encourages the release of myofascial adhesions, improves local blood circulation, and stimulates the body’s natural healing response.
Benefits of Pressure Myofascial Release Technique
Myofascial release offers many benefits, especially for patients with chronic pain and movement restrictions. By releasing tension in the myofascial tissues, this technique can:
- Reduce Pain : By releasing adhesions and decompressing tissues, myofascial release can relieve pain associated with muscle tension, tight fascia, and trigger points.
- Improve Mobility : By restoring tissue flexibility, myofascial release allows for greater range of motion, making daily activities easier and reducing the risk of further injury.
- Correct postural imbalances : Myofascial tensions can contribute to postural imbalances that affect body alignment. By working on these tensions, the technique helps restore correct posture and prevent associated pain.
- Stimulate circulation : Improving blood circulation in the treated tissues helps nourish muscles and fascia, promoting their healing and regeneration.
Integration into a comprehensive treatment plan
Although pressure myofascial release is effective for treating muscle pain and restrictions, it is often integrated into an overall treatment plan. This may include strengthening and stretching exercises, postural adjustments, and lifestyle modifications to address the underlying causes of myofascial tension.
Patients are also encouraged to take an active role in their recovery by practicing gentle mobilization exercises at home and becoming aware of factors that can contribute to the reoccurrence of tension, such as stress or poor postural habits.
Frequently Asked Questions (FAQ) about Lumbosacral Facet Syndrome
Lumbosacral facet syndrome is a common source of lower back pain, but it can be difficult for those who suffer from it to understand. Here is a list of frequently asked questions to help patients understand the condition, treatment expectations, and precautions to take.
1. What is lumbosacral facet syndrome?
Lumbosacral facet syndrome is a condition in which the facet joints of the lumbar vertebrae become damaged or irritated, causing lower back pain. These facet joints are small joints located at the back of each vertebra that allow for flexion, extension, and rotation of the spine. When these joints become worn out or inflamed, they can cause pain, stiffness, and reduced mobility.
2. What are the common symptoms?
Symptoms include deep pain in the lower back, often made worse by movements such as bending over or twisting the torso. The pain may also extend to the buttocks and thighs, but it usually does not extend lower than the knee. Some patients may also experience stiffness and loss of flexibility, especially after sitting or standing for long periods of time.
3. How long does it take to heal?
The length of time it takes to heal varies depending on the severity of the condition and the treatment that is followed. For mild to moderate cases, pain may improve within a few weeks to a few months with appropriate treatment, such as anti-inflammatory medications, manual therapies, and rehabilitation exercises. However, for more severe cases, or if treatment is delayed, healing may take several months or even become a chronic condition requiring long-term management.
4. What treatments are available?
Treatment for lumbosacral facet syndrome may include anti-inflammatory medications, corticosteroid injections, physical therapy, and manual techniques such as osteopathy. In some cases, more invasive procedures, such as nerve blocks or radiofrequency, may be recommended. Surgery is rarely necessary, but it may be considered if other treatments fail to relieve symptoms.
5. What activities should I avoid?
It is recommended to avoid activities that put excessive strain on the lower back, such as heavy lifting, repeated twisting of the trunk, and high-impact exercises such as running or jumping. It is also advisable to avoid prolonged positions, such as sitting or standing for too long without moving. However, it is important to stay active with gentle, tailored exercises, such as walking, swimming, or specific stretches, to maintain mobility and muscle strength.
6. Can I continue to work with this syndrome?
It depends on the nature of your job. If your job involves intense physical effort or repetitive movements, you may need to take extra precautions or temporarily adjust your tasks. If you have a sedentary job, be sure to take regular breaks to move around and adopt an ergonomic posture. In all cases, it is important to consult a healthcare professional for recommendations tailored to your situation.
7. Can lumbosacral facet syndrome become chronic?
Yes, without proper treatment, lumbosacral facet syndrome can become chronic, leading to persistent pain and reduced quality of life. It is essential to treat the condition promptly to prevent it from becoming a long-term problem. Regular follow-up with a healthcare professional is also recommended to manage symptoms and prevent recurrences.
8. What can I do to prevent recurrences?
To prevent recurrence, it is crucial to maintain good posture, strengthen the core muscles, and avoid movements that put excessive pressure on the lower back. Regular exercise, stretching, and a healthy lifestyle can also help prevent it. It is also advisable to regularly consult a healthcare professional for personalized check-ups and advice.
Conclusion
In conclusion, Lumbosacral Facet Syndrome reveals the complexity of anatomical interactions and mechanical factors that can lead to uncomfortable symptoms. Through a holistic approach to osteopathy, we have explored precise diagnostic methods and therapeutic interventions aimed at relieving pain and restoring function. However, prevention remains an essential component, emphasizing the importance of adopting healthy lifestyles and attention to posture. With this knowledge and a close collaboration between patients and osteopaths, we can approach Lumbosacral Facet Syndrome in a comprehensive manner, improving quality of life and promoting long-term well-being.
References
- Bogduk N. Degenerative joint disease of the spine. Radiol Clin North Am. 2012 Jul;50(4):613-28. [PubMed]2.
- Manchikanti L, Singh V, Pampati V, Damron KS, Barnhill RC, Beyer C, Cash KA. Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician. 2001 Oct;4(4):308-16. [PubMed]3.
- Grgić V. [Lumbosacral facet syndrome: functional and organic disorders of lumbosacral facet joints]. Lijec Vjesn. 2011 Sep-Oct;133(9-10):330-6. [PubMed]4.
- Perolat R, Kastler A, Nicot B, Pellat JM, Tahon F, Attye A, Heck O, Boubagra K, Grand S, Krainik A. Facet joint syndrome: from diagnosis to interventional management. Insights Imaging. 2018 Oct;9(5):773-789. [PMC free article] [PubMed]5.
- Marcia S, Masala S, Marini S, Piras E, Marras M, Mallarini G, Mathieu A, Cauli A. Osteoarthritis of the zygapophysial joints: efficacy of percutaneous radiofrequency neurotomy in the treatment of lumbar facet joint syndrome. Clin Exp Rheumatol. 2012 Mar-Apr;30(2):314. [PubMed]6.
- Kalichman L, Li L, Kim DH, Guermazi A, Berkin V, O’Donnell CJ, Hoffmann U, Cole R, Hunter DJ. Facet joint osteoarthritis and low back pain in the community-based population. Spine (Phila Pa 1976). 2008 Nov 01;33(23):2560-5. [PMC free article] [PubMed]7.
- Chazen JL, Leeman K, Singh JR, Schweitzer A. Percutaneous CT-guided facet joint synovial cyst rupture: Success with refractory cases and technical considerations. Clin Imaging. 2018 May-Jun;49:7-11. [PubMed]8.
- Cavanaugh JM, Ozaktay AC, Yamashita HT, King AI. Lumbar facet pain: biomechanics, neuroanatomy and neurophysiology. J Biomech. 1996 Sep;29(9):1117-29. [PubMed]9.
- Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022 Jan 19;92(6):e2021313. [PMC free article] [PubMed]10.
- Rajeev A, Choudhry N, Shaikh M, Newby M. Lumbar facet joint septic arthritis presenting atypically as acute abdomen – A case report and review of the literature. Int J Surg Case Rep. 2016;25:243-5. [PMC free article] [PubMed]11.
- Manchikanti L, Boswell MV, Singh V, Pampati V, Damron KS, Beyer CD. Prevalence of facet joint pain in chronic spinal pain of cervical, thoracic, and lumbar regions. BMC Musculoskelet Disord. 2004 May 28;5:15. [PMC free article] [PubMed]12.
- Datta S, Lee M, Falco FJ, Bryce DA, Hayek SM. Systematic assessment of diagnostic accuracy and therapeutic utility of lumbar facet joint interventions. Pain Physician. 2009 Mar-Apr;12(2):437-60. [PubMed]13.
- Kozera K, Ciszek B, Szaro P. Posterior Branches of Lumbar Spinal Nerves – part II: Lumbar Facet Syndrome – Pathomechanism, Symptomatology and Diagnostic Work-up. Ortop Traumatol Rehabil. 2017 Apr 12;19(2):101-109. [PubMed]14.
- Bogduk N. Functional anatomy of the spine. Handb Clin Neurol. 2016;136:675-88. [PubMed]15.
- Ening G, Kowoll A, Stricker I, Schmieder K, Brenke C. Lumbar juxta-facet joint cysts in association with facet joint orientation, -tropism and -arthritis: A case-control study. Clin Neurol Neurosurg. 2015 Dec;139:278-81. [PubMed]