Introduction
Knee sprains represent a common category of injuries that affect the musculoskeletal system, often leading to significant consequences on individuals’ mobility and quality of life. The anatomical complexity of the knee, made up of ligaments, tendons, cartilage and bone, makes it particularly vulnerable to sprains, defined as overstretching or tearing of the ligaments.
Ligaments, fibro-cartilaginous structures crucial for joint stability, are often the main players in knee sprains. Sprain can occur when a force applied to the knee exceeds the ability of the ligaments to maintain the integrity of the joint. Sports involving sudden changes of direction, abrupt stops, or direct impacts to the knee, such as football and basketball, are contexts prone to these injuries.
The severity of knee sprains can vary, generally classified into three degrees. First-degree sprains involve overstretching the ligaments, causing a slight tear without significant loss of function. Second-degree sprains present partial tears of the ligaments, leading to moderate instability and more pronounced symptoms. Finally, third-degree sprains represent complete tears of the ligaments, resulting in major instability and often requiring immediate medical intervention.
Symptoms of knee sprains are often immediate, with sharp pain, swelling, and sometimes an inability to bear body weight. Mild sprains can often be treated with conservative measures such as rest, icing, compression, and elevation (RICE), as well as anti-inflammatories. However, more serious sprains may require medical intervention, including physical therapy, rehabilitation, or even surgery to restore joint stability.
Preventing knee sprains is of critical importance, especially for individuals engaged in demanding physical activities. Warming up before exercise, targeted muscle strengthening, and appropriate use of protective equipment can help minimize the risk of injury. Correct landing techniques during sports activities, as well as strengthening the stabilizing muscles of the knee, are also key elements of prevention.
Beyond the physical aspects, knee sprains can have a significant psychological impact, sometimes leading to fear of recurrence and excessive caution in daily activities. The overall management of these injuries must therefore include a psychosocial component to promote complete recovery and resumption of an active life.
In conclusion, knee sprains represent a common challenge in the trauma field. Understanding the mechanisms of these injuries, coupled with effective preventive measures, can help minimize their incidence. Appropriate treatment and a holistic approach taking into account physical and psychosocial aspects are essential for optimal recovery and long-term preservation of knee health.
Anatomy
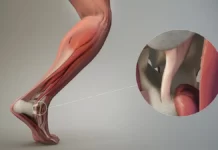
The knee is a complex joint made up of different structures, with ligaments playing a crucial role in the stability and overall function of the joint. Among these ligaments, those located on the outside of the knee, also called lateral ligaments, contribute significantly to the lateral stability of the joint.
1. Lateral Collateral Ligament (LCL): The lateral collateral ligament, or LCL, is one of the main external ligaments of the knee. It extends from the lower end of the femur (thigh bone) to the head of the fibula (leg bone). The LCL plays a crucial role in lateral stability by preventing the knee from excessively flexing outward.
2. Lateral Fibular Ligament (LLF): The lateral fibular ligament, or LLF, is an intrinsic ligament that reinforces the joint capsule of the knee on the lateral side. It works in tandem with the LCL to provide maximum lateral stability, particularly during pivoting movements.
3. Biceps Femoris Tendon: Although the biceps femoris tendon is primarily associated with the thigh muscles, its long tendon runs along the outer side of the knee and contributes to lateral stability. It is often involved in stabilizing the knee during certain movements, acting synergistically with the lateral ligaments.
4. Joint Capsule: The joint capsule surrounds the knee and houses the ligaments. It strengthens the stability of the joint by providing structural support. The outer part of the joint capsule is reinforced by the lateral ligaments, contributing to resistance against lateral forces.
In terms of function, the external ligaments of the knee act as essential stabilizers during lateral movements, preventing the knee from moving excessively outward. These structures are particularly important in preventing injuries related to lateral forces or twisting of the knee.

Causes
Knee sprains can occur for a variety of reasons, often related to excessive force or unnatural movements. The most common causes of knee sprains include:
- Physical Trauma:
- Sudden Twist: Knee sprains can result from sudden twisting, often seen during sporting activities, sudden movements, or rapid changes in direction.
- Direct Impact: A direct impact on the knee, such as a collision during a sporting accident or a fall, can cause sprains.
- Poor Body Mechanics:
- Poor Alignment: Poor body mechanics, such as poor posture or muscle imbalance, can increase the risk of knee sprains during simple movements.
- Intense Sports Activities:
- Risky Sports: Certain sports, such as football, basketball and skiing, which involve rapid movements and frequent changes of direction, can increase the risk of knee sprains.
- Tearing or Excessive Stretching of Ligaments:
- Poor Sports Practice: Poor sports technique, such as landing incorrectly after a jump, can lead to overstretching or tearing ligaments.
- Anatomical Factors:
- Structural Abnormalities: Some individuals may have anatomical abnormalities that increase their predisposition to knee sprains, such as congenital ligamentous laxity.
- Environmental Conditions:
- Playing Surface: Playing conditions, such as the nature of the surface on which physical activity is performed, can contribute to knee sprains.
- Inadequate Training:
- Lack of Muscle Strengthening: A lack of muscle strengthening, particularly around the knee, can make the joint more vulnerable to injury.
- Muscle fatigue :
- Overfeeding or Overuse: Muscle fatigue from overuse or excessive loading can decrease the muscles’ ability to stabilize the joint, increasing the risk of sprains.
- Genetic Predisposition:
- Family History: A family history of frequent sprains may indicate a genetic predisposition to these injuries.
Symptoms
Knee sprains can manifest with a variety of symptoms, which vary depending on the severity of the injury. Common symptoms of knee sprains include:
- Pain :
- Sharp pain at the time of injury.
- Persistent pain around the knee joint.
- A burning or tingling sensation in the affected area.
- Swelling (Oedema):
- Swelling that is immediate or develops over time.
- An increase in knee circumference due to fluid accumulation.
- Hematoma (Bruises):
- Bruises or contusions around the knee.
- Bluish or purple discoloration of the skin due to internal bleeding.
- Difficulty moving the knee:
- A limitation of full flexion or extension of the knee.
- A feeling of joint stiffness.
- Feeling of Instability:
- A feeling of weakness or instability in the knee.
- Difficulty supporting body weight on the affected knee.
- Crepitation:
- A cracking, clicking, or crackling sensation when moving the knee.
- Local Heat:
- An increase in heat around the affected joint.
- Inability to Walk Normally:
- Difficulty walking without limping or using the injured knee.
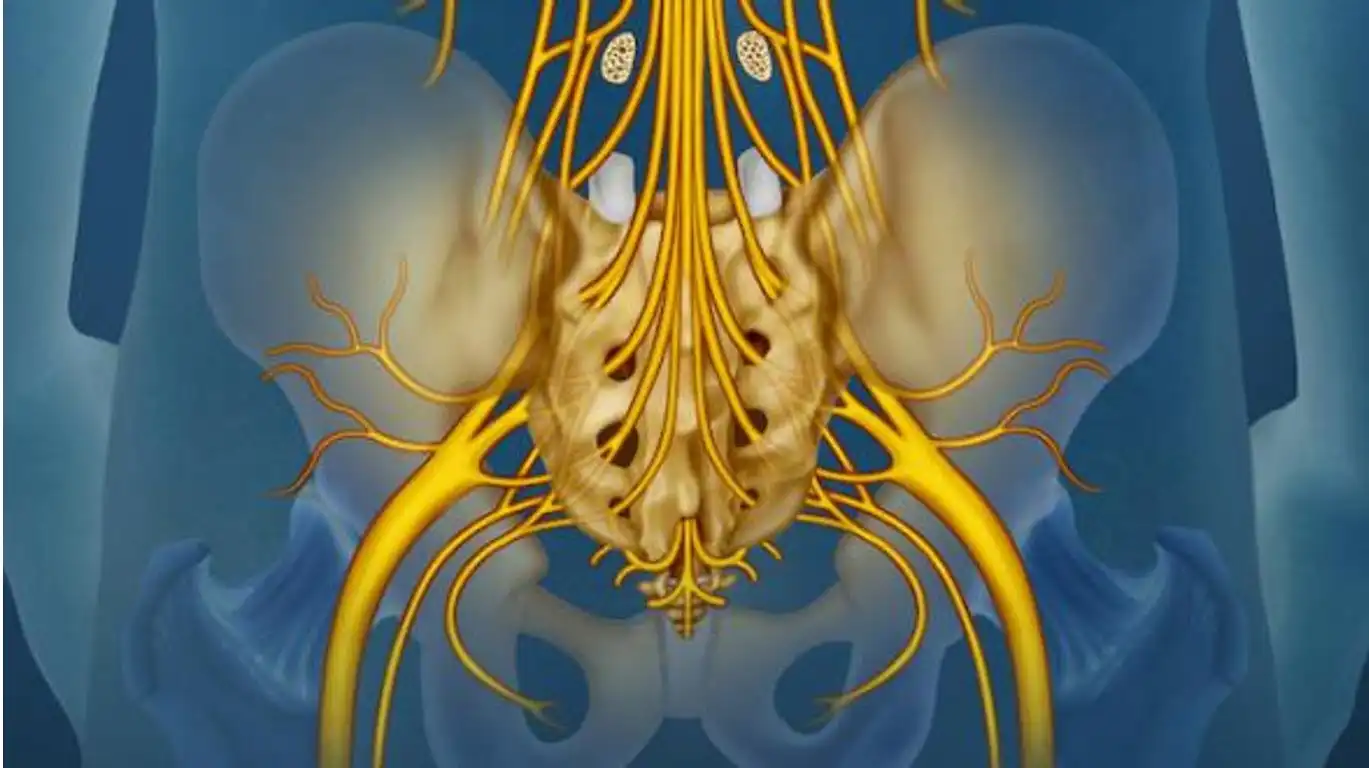
Pathophysiology
The pathophysiology of knee sprains is essential to understanding how these injuries occur and progress. A knee sprain usually involves damage to the ligaments, which are sturdy connective tissues responsible for stabilizing the knee joint. These ligaments may be stretched, partially torn, or completely ruptured depending on the severity of the sprain.
- Ligament Stretching:
- Mild sprains typically occur when the knee ligaments are stretched beyond their normal range without experiencing significant tearing.
- This can result from sudden twisting of the knee, excessive flexion, or lateral force applied to the joint.
- Partial Ligament Tear:
- Moderate sprains may involve a partial tear of the ligaments, leading to an alteration in their structure.
- This can occur during sudden movements, direct impacts to the knee, or situations where the force applied exceeds the load capacity of the ligaments.
- Complete Ligament Rupture:
- Severe sprains are characterized by a complete rupture of one or more ligaments.
- This can occur in sporting accidents, significant falls, or violent trauma.
- Inflammatory Response:
- Immediately after the sprain, an inflammatory response is triggered to help stabilize the injured area.
- Inflammation causes swelling, redness, and local heat.
- Hematoma Formation:
- If the blood vessels tear, a hematoma may form, causing bruising and increased pressure in the area.
- Alteration of Joint Stability:
- Due to the ligament injury, joint stability may be compromised, which can lead to feelings of instability and difficulty supporting body weight on the knee.
Diagnostic
The diagnosis of knee sprains is crucial to determine the precise nature of the injury and guide the treatment plan. Healthcare professionals use different methods to assess the severity of the sprain and make an accurate diagnosis.
- Clinical Evaluation:
- The doctor will begin by taking a detailed medical history, including the nature of the event that caused the injury, symptoms experienced, and history of knee problems.
- A physical examination is performed to assess knee stability, joint mobility, and the presence of swelling, bruising, or other visible signs of a sprain.
- Imaging Exams:
- X-rays may be taken to rule out bone fractures or to assess bone alignment.
- Magnetic resonance imaging (MRI) is often used to obtain detailed images of the ligaments, tendons, and other structures of the knee. This allows you to visualize tears or ruptures of the ligaments.
- Functional Tests:
- Functional tests, such as the anterior drawer test, may be performed to assess knee stability and identify affected ligaments.
- Severity Classification:
- Knee sprains are often classified into three grades based on severity:
- Grade I: Mild stretching of the ligaments.
- Grade II: Partial tear of ligaments with moderate loss of function.
- Grade III: Complete rupture of ligaments with significant loss of function.
- Knee sprains are often classified into three grades based on severity:
- Elimination of other Conditions:
- Sometimes other conditions such as meniscal damage or cartilage damage can coexist with a knee sprain. The diagnosis must therefore exclude these possibilities.
- Specialized Consultation:
- In complex or severe cases, a consultation with an orthopedic specialist may be recommended to discuss treatment options, including surgery if necessary.
Treatment
- Conservative Treatment:
- Rest and Immobilization: For mild sprains, rest and immobilization of the knee using a splint or bandage can promote healing.
- Application of Ice: Using ice reduces inflammation and relieves pain. This is often recommended for the first 48 hours after the injury.
- Compression and Elevation: Wearing a compression bandage and elevating the knee helps reduce swelling.
- Rehabilitation and Physiotherapy:
- Muscle Strengthening Exercises: Osteopathy includes targeted exercises to strengthen the muscles around the knee, improving joint stability and function.
- Stretching: Stretching exercises help regain flexibility and prevent stiffness.
- Drugs :
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications such as ibuprofen may be prescribed to reduce pain and inflammation.
- Splint or Orthosis:
- In some cases, wearing a brace or orthosis may be recommended to stabilize the knee while it heals.
- Surgery :
- Ligament Repair: Severe sprains, especially complete ligament tears, may require surgery to repair damaged ligaments.
- Arthroscopy: In some cases, an arthroscopy may be performed to evaluate and treat internal knee injuries.
- Rehabilitation:
- After surgery or in the event of a severe sprain, a period of supervised rehabilitation is often necessary to regain strength and mobility in the knee.
Prevention
Preventing knee sprains involves several measures aimed at strengthening the stability of the joint and minimizing the risk of injury. Here are some tips and prevention strategies:
- Muscle Strengthening: A regular exercise program focused on strengthening the muscles surrounding the knee, including the quadriceps, hamstrings and calf muscles, helps stabilize the joint.
- Flexibility and Stretching: Regular stretching exercises improve the flexibility of muscles and tendons, thereby reducing the risk of injury during physical activities.
- Proper Warm-Up: Before any physical activity, it is essential to warm up properly to prepare the muscles and joints for exercise. Dynamic stretches and specific movements can be included in the warm-up routine.
- Correct Technique: Learning and maintaining proper technique during sports activities or physical exercise can help avoid undue stress on the knee.
- Use of Protective Equipment: In some sports, wearing protective equipment such as knee pads can reduce the risk of injury by providing additional support.
- Suitable Terrain: When practicing physical activities, it is recommended to choose suitable surfaces and monitor the terrain conditions to avoid the risk of slipping or impact.
- Prevention Program: Certain sports, particularly those with a high risk of knee sprains, may benefit from specific injury prevention programs. These programs often include strengthening, balance and coordination exercises.
- Maintaining a Healthy Weight: Maintaining a healthy body weight helps reduce the load on joints, including the knee, thereby reducing the risk of injury.
- Rest and Recovery: Allowing the body time to recover between training sessions is crucial to avoiding excessive muscle fatigue and reducing the risk of injury.
- Education: Awareness of risk factors, prevention techniques and injury management is important for active people, athletes and healthcare professionals.
Knee pad
Knee braces are orthopedic devices designed to provide additional support and protection to the knee joint. They are commonly used in the prevention and treatment of knee injuries, including ligament sprains. Here is some information about knee pads:
Types of Knee Pads
- Supportive Knee Pads: These knee pads provide overall support to the knee joint, helping to prevent injuries and stabilize the joint. They are often used during sports or physical activities.
- Soft Knee Pads: Made of elastic materials, these knee pads provide light compression and support. They are commonly used to relieve mild knee pain.
- Rigid Knee Pads: These knee pads feature rigid braces or hinges to provide maximum support. They are often prescribed after a knee injury or after surgery to immobilize the joint.
- Patella Knee Braces: Designed specifically to support the patella, these knee braces are used to treat problems related to the patella, such as patellofemoral syndrome.
- Therapeutic Knee Pads: Prescribed by health professionals, these knee pads are adapted to specific needs, such as the correction of certain anatomical anomalies or post-surgical support.
Use of Knee Pads
- Injury Prevention: Athletes, especially in high-risk knee sports, can wear knee braces to prevent sprains and other injuries.
- Post-Injury Support: After a sprain or ligament injury, knee sleeves can be used during recovery to provide support and prevent further trauma.
- Chronic Pain: People with chronic knee pain, whether due to osteoarthritis or other conditions, may benefit from using knee braces to relieve symptoms.
- Rehabilitation: Knee pads can be used during rehabilitation sessions to provide support during exercises and physical activities.
- Sports Activities: Many athletes wear knee pads during competitions or intensive training to reduce the risk of injury.
Precautions
Although knee braces can be beneficial in many situations, it is important to consult a healthcare professional to determine the appropriate type of knee brace and its specific use, as incorrect use can sometimes make problems worse.
Conclusion
In conclusion, knee sprains represent a frequent problem, often linked to sports injuries or everyday accidents. The complex anatomy of the knee joint, including the external ligaments, makes this area particularly prone to sprains.
The causes of knee sprains are diverse, ranging from sudden movements to direct trauma, and can lead to damage to the ligaments. Symptoms, such as pain, swelling, and limitation of movement, are common signs of a sprain.
The pathophysiology of sprains typically involves overstrain or partial rupture of ligaments, which can compromise joint stability. Diagnosis is based on clinical examination, medical imaging and assessment of symptoms.
Treatment for sprains varies depending on the severity of the injury, ranging from conservative measures like rest and physical therapy to more invasive interventions like surgery. Prevention plays a crucial role, involving muscle strengthening exercises, proper warm-up techniques and, in some cases, the use of support devices such as knee pads.
Knee braces, in particular, are commonly used tools in the management of sprains. They provide additional support, compression and stability, whether to prevent injury, aid recovery or relieve chronic symptoms. However, it is essential to consult a healthcare professional to determine the appropriate type of knee brace for each situation.
In summary, a thorough understanding of the anatomy, causes, symptoms, pathophysiology, diagnosis, treatment, and prevention of knee sprains contributes to effective management of these common injuries. By combining appropriate medical approaches with preventive measures, it is possible to improve the quality of life of people affected by knee sprains.