Introduction
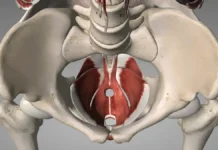
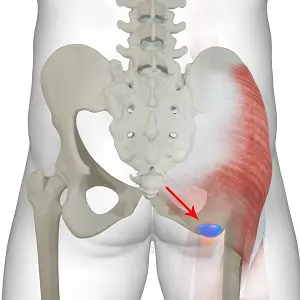
The ischial bursa, a small anatomical structure located between the gluteus maximus muscle and the ischial tuberosity bone, plays a crucial role in the harmonious functioning of the hip joint. It is essential to understand your anatomy and the factors that can influence your health.
This bursa, often overlooked, can present itself in a varied manner in different individuals. It can take the form of a single bursa or, in certain subjects, appear in the form of a multisegmental series of small localized bursae. This anatomical diversity can influence how the bursa responds to trauma and stress.
The ischial bursa is particularly prone to acute trauma and repeated microtrauma. Acute injuries often occur as a result of direct trauma to the bursa, whether from a fall on the buttocks or through overuse, such as in horseback riding or prolonged cycling. These activities can cause excessive compression of the bursa, causing acute injuries. Equestrian sports enthusiasts and cyclists, due to prolonged pressure on the ischial region, are particularly susceptible to developing acute bursa injuries.
Running, while beneficial for overall health, can also contribute to ischial bursa problems, particularly when done on uneven or soft surfaces, such as sand. The constant variation in terrain can lead to irregular movements, increasing the risk of repetitive strain injuries. These microtraumas can gradually lead to chronic inflammation of the ischial bursa, causing a series of uncomfortable symptoms.
In cases of persistent chronic inflammation, complications such as calcification of the ischial bursa may occur. Calcification often results from a process of response to chronic inflammation, where deposits of calcium salts can form in the bursa. This calcification can worsen symptoms, making hip movement more painful and limited.
It is essential to recognize the warning signs of problems with the ischial bursa. Common symptoms include local pain, increased sensitivity to pressure, and decreased hip mobility. In cases of acute injury, swelling and bruising may also be seen.
Treatment for ischial bursa problems may vary depending on the nature of the injury. For acute injuries, rest, application of ice, and taking anti-inflammatories can help reduce inflammation. For more chronic cases, physical therapy may be recommended to strengthen the surrounding muscles and improve hip stability.
Prevention also plays a key role in the health of the ischial bursa. Careful attention to warming up before exercise, proper technique when participating in risky sports, and use of appropriate protection can help minimize the risk of trauma.
In conclusion, the ischial bursa, although often overlooked, is an important anatomical structure in the hip region. A thorough understanding of its anatomy, risk factors, and associated symptoms is crucial to preventing and treating potential problems. If you experience persistent pain or worrying symptoms, it is always recommended to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Causes
- Acute trauma : Acute injuries to the ischial bursa are often caused by direct trauma, such as falls on the buttocks. These incidents can cause sudden compression of the bursa, leading to immediate inflammation and painful symptoms.
- Overuse: Activities involving prolonged pressure on the ischial region, such as horseback riding or prolonged cycling, can contribute to repetitive strain injuries. Over time, these constant stresses can lead to chronic inflammation of the bursa.
- Sports activities: Certain sports, especially those involving repetitive movements or constant pressure on the glutes, increase the risk of ischial bursa problems. Runners, cyclists and equestrians are particularly prone to these problems.
- Uneven or soft terrain: Running on uneven or soft surfaces, such as sand, can cause irregular movements and increase the risk of strain injuries. This can lead to irritation and inflammation of the bursa.
- Infections: Although less common, infections of the ischial bursa can occur. These infections can be caused by bacteria or other pathogens, leading to inflammation and painful symptoms.
- Calcification: In cases of persistent chronic inflammation, the ischial bursa can develop calcium deposits, leading to calcification. This can make the pain worse and further limit hip mobility.
- Genetic predisposition: Some individuals may have a genetic predisposition to developing ischial bursa problems. Anatomical or metabolic variations can make some people more susceptible to trauma or inflammation in this area.
- Other medical conditions: Certain medical conditions, such as arthritis or other inflammatory diseases, can contribute to ischial bursa problems. General inflammatory processes in the body can also affect the bursa.
- Postural Disorders: Postural imbalances, whether acquired or resulting from underlying medical conditions, can place uneven pressure on the ischial region. Poor posture can contribute to microtrauma and inflammation of the bursa.
- Excessive physical stress: Intensive physical activities, especially without adequate progression or preparation, can create undue stress on the ischial region, increasing the risk of injury and inflammation of the bursa.
Symptoms
Symptoms associated with ischial bursa problems can vary depending on the nature of the injury or inflammation. Here is a list of common symptoms that may be associated with ischial bursa problems:
- Local pain: Pain in the ischial region is one of the most common symptoms. This pain can vary in intensity, from mild to severe, and may be felt as a burning, tingling, or dull ache.
- Increased sensitivity to pressure: The area around the ischial bursa may become more sensitive to touch. Applying pressure to the affected area may cause discomfort or pain.
- Swelling: Inflammation of the ischial bursa can lead to swelling in the affected area. Swelling may be visible or simply felt as a feeling of fullness.
- Redness and local heat: In cases of acute inflammation, the skin over the ischial region may become red and hot to the touch. These symptoms are classic signs of an inflammatory reaction.
- Limitation of hip mobility: Problems with the ischial bursa can lead to stiffness or limited movement of the hip. Mobility may be reduced due to pain or discomfort.
- Lameness: To avoid pain, some people may adopt an altered gait or limp. This lameness may be more pronounced during or after physical activity.
- Crepitation: Some individuals may feel or hear cracking or crackling sounds in the ischial bursa during hip movements. This may indicate the presence of crystals or debris.
- Pain radiating to the buttocks or thigh: Pain from the ischial bursa can radiate to the buttocks or thigh. This irradiation of pain often depends on the specific nature of the lesion or inflammation.
- Difficulty sitting or staying seated: People with ischial bursa problems may have difficulty sitting for long periods of time due to the pressure placed on the affected area.
- Muscle Fatigue: Surrounding muscles can become tired or tight due to compensating to avoid pain, especially during physical activity.
Risk factors
Several risk factors can increase the likelihood of developing ischial bursa problems. Understanding these factors can help take appropriate preventative measures. Here are some of the risk factors associated with ischial bursa problems:
- Age: The risk of joint problems, including those of the ischial bursa, generally increases with age due to the natural wear and tear of joints and tissues.
- Gender: Women are often more likely to develop ischial bursa problems, in part due to different pelvic structure and hormonal changes, particularly during pregnancy and menopause.
- Obesity: Excess weight puts additional pressure on joints, including the ischial region. Obesity is a major risk factor for joint problems.
- High-impact physical activities: Activities that involve repetitive movements, frequent impacts, or constant pressure on the ischial region, such as prolonged running or cycling, can increase the risk of bursa problems.
- Poor Posture: Improper posture, whether at work, during prolonged sitting, or during exercise, can create imbalances that increase pressure on the ischial region.
- Genetic Factors: Some individuals may have a genetic predisposition to develop joint problems, including ischial bursa problems, due to inherited anatomical structure.
- Previous trauma: Previous injuries, especially those that have not been properly treated, can increase the risk of ischial bursa problems.
- Pre-existing medical conditions: Certain medical conditions, such as arthritis, rheumatoid arthritis, or other autoimmune diseases, can increase the risk of joint problems.
- Infections: Infections in the ischial region can trigger an inflammatory response, contributing to the development of bursa problems.
- Poor diet: An unbalanced diet, high in pro-inflammatory foods and low in essential nutrients, can contribute to joint problems.
- Heredity: A family history of joint problems can increase the risk of developing ischial bursa problems.
- Metabolic Diseases: Conditions such as diabetes, hyperuricemia, and other metabolic disorders can increase the vulnerability of joints, including the ischial bursa.
- Sedentary lifestyle: Lack of physical activity can weaken surrounding muscles and contribute to joint stiffness.
- Gait Disorders: Gait problems, such as excessive supination or pronation, can place uneven pressure on the ischial region.
- Hormonal conditions in women: Hormonal fluctuations during menstruation, pregnancy and menopause can influence joint health.
People who engage in the following activities have a higher risk of developing ischial bursitis:
- Cyclists who ride frequently
- The runners
- People who exercise incorrectly
- People who jump or kick repeatedly
Recommendations
- Rest and Avoid Aggravating Activities:
- Give the affected area time to heal by avoiding activities that may make the pain worse, such as sitting for long periods of time or activities that put pressure on the buttocks.
- Ice Application:
- Applying ice to the affected area can help reduce inflammation. Use an ice pack wrapped in a thin cloth and apply it to the affected area for about 15 to 20 minutes each time, several times a day.
- Anti-inflammatory medications:
- Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can help reduce pain and inflammation. However, consult a healthcare professional before taking any medication.
- Cushioning and Support:
- Use a cushion or pillow when sitting to reduce pressure on the affected area. This can be especially helpful if your job or lifestyle requires prolonged sitting.
- Avoid prolonged sitting:
- If possible, take breaks from standing or walking to avoid prolonged periods of sitting.
- Warm-up Before Activities:
- Gentle stretches and warm-up exercises before participating in physical activities can help prevent symptoms from getting worse.
- Edit Activities:
- Change activities that may make the condition worse. This may include avoiding activities that involve repetitive hip movements or prolonged pressure on the buttocks.
Remember, this is general advice and may not be suitable for everyone. It is crucial to consult a healthcare professional for advice tailored to your specific situation. If symptoms persist or worsen, seek the advice of a healthcare professional promptly.
Osteopathy
Osteopathy can be used as a complementary approach to relieve the symptoms of ischial bursitis. Osteopaths are practitioners who use manual techniques to assess, diagnose and treat various musculoskeletal disorders.
Here are some osteopathic approaches that can be used in the case of ischial bursitis:
- Joint manipulation: The osteopath may use gentle joint manipulation techniques to improve mobility of the hip joint and reduce tension in the ischial region.
- Muscle stretching: Specific exercises and stretches may be recommended to relieve muscle tension around the affected area, thereby promoting healing.
- Myofascial release techniques: The osteopath may use myofascial release techniques to release tension in the soft tissues, including the muscles and the affected bursa.
- Correction of postural imbalances: Osteopathy can help identify and correct postural imbalances that may contribute to ischial bursitis. This may involve postural adjustments and advice on how to improve posture in everyday life.
- Advice on ergonomics: The osteopath can provide advice on ergonomics to minimize pressure on the affected area during daily activities.
It is important to emphasize that osteopathy does not replace conventional medical recommendations. If you suspect ischial bursitis, it is essential to consult a healthcare professional for an accurate diagnosis. A comprehensive treatment plan may include medical, physiotherapeutic and osteopathic approaches for comprehensive management of the condition.
References
- Kubota K, Yamashita H, Mimori A. Clinical Value of FDG-PET/CT for the Evaluation of Rheumatic Diseases: Rheumatoid Arthritis, Polymyalgia Rheumatica, and Relapsing Polychondritis. Semin Nucl Med. 2017 Jul;47(4):408-424. [ PubMed ]
- Chen B, Rispoli L, Stitik T, Leong M. Successful Treatment of Gluteal Pain from Obturator Internus Tendinitis and Bursitis with Ultrasound-Guided Injection. Am J Phys Med Rehabil. 2017 Oct;96(10):e181-e184. [ PubMed ]
- kiz T, Biçici V, Hatioglu C, Yalçın S, Cingöz K. Ischial Pain and Sitting Disability Due to Ischiogluteal Bursitis: Visual Vignette. Pain Physician. 2015 Jul-Aug;18(4):E657-8. [ PubMed ]
- Navarro-Zarza JE, Villaseñor-Ovies P, Vargas A, Canoso JJ, Chiapas-Gasca K, Hernández-Díaz C, Saavedra MÁ, Kalish RA. Clinical anatomy of the pelvis and hip. Reumatol Clin. 2012 Dec-2013 Jan;8 Suppl 2:33-8. [ PubMed ]
- Guanche CA. Hamstring injuries. J Hip Preserv Surg. 2015 Jul;2(2):116-22. [ PMC free article ] [ PubMed ]
- Paluska SA. An overview of hip injuries in running. Sports Med. 2005;35(11):991-1014. [ PubMed ]
- Bard H. [Periarticular pathology of the hip]. Rev Pr