Introduction
Quervain’s tenosynovitis, first described in 1895 by the Swiss surgeon Fritz de Quervain, is the most common tendonitis of the wrist. It is characterized by a thickening of the tendon sheaths surrounding the abductor pollicis longus and the extensor pollicis brevis, where the tendons pass into the fibro-osseous tunnel along the radial styloid at the distal wrist. Patients with this condition typically experience pain that spans the radial aspect of the wrist, and this pain is exacerbated by ulnar deviation of the hand. The main cause of this condition is overuse of the thumb muscles.

Tendons play a crucial role in connecting muscles to bones. However, repetitive activities and overuse can lead to damage to the tendons, causing pain and impairing their function. This type of problem is generally classified as a tendinopathy. Although some people use the term biceps tendinitis to describe this condition, the more accurate term is tendinopathy, as most affected individuals do not have inflammation. The suffix “-pathy” means pain, while “-itis” means inflammation.
It is important to recognize and treat de Quervain tenosynovitis promptly, as continued overuse can worsen the condition and lead to long-term deterioration in wrist function. Treatment approaches may include rest, ice application, physical therapy, and in some cases anti-inflammatory medications. If symptoms persist, surgical intervention may be considered to release the tendons from the fibro-osseous tunnel.
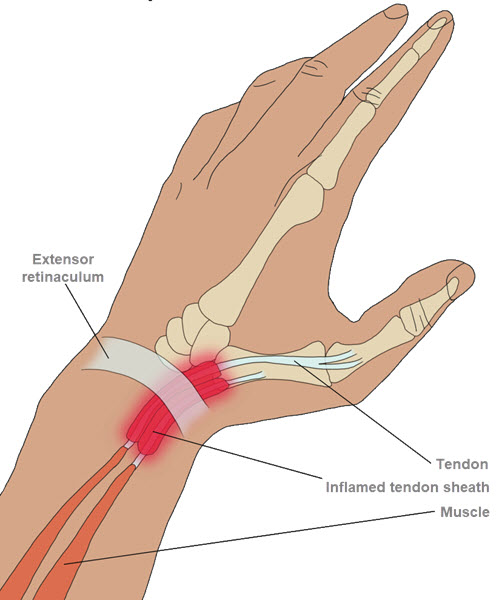
The image illustrates the anatomy of the wrist and thumb, highlighting De Quervain’s tenosynovitis. This condition involves inflammation of the tendon sheath surrounding the extensor pollicis brevis and abductor pollicis longus tendons, leading to pain and swelling on the thumb side of the wrist. The inflamed tendon sheath and extensor retinaculum are shown, emphasizing the areas affected by this common repetitive stress injury. Contributed by Chelsea Row
Mechanisms of tendon irritation
- The 2 tendons around the base of the thumb swell.
- The swelling causes inflammation of the synovial sheaths covering the tendons.
- The inflammation thickens the tenosynovitis tendon sheath and tightens the tendon as it slips through the sheath.
- This puts pressure on nearby nerves, causing pain and numbness.
- Causing the tendon to become blocked when the patient moves the thumb.
Causes of de Quervain tenosynovitis
De Quervain tenosynovitis is a painful condition that affects the tendons of the thumb, often caused by inflammation of the synovial sheath that surrounds these tendons. The main causes of de Quervain tenosynovitis are usually related to activities that involve repetitive movements of the thumb and wrist, as well as certain underlying medical conditions.
A common cause of de Quervain tenosynovitis is excessive use of the thumb and wrist in repetitive twisting or pinching movements, such as knitting, gardening, sewing, prolonged use of a smartphone or a computer mouse, or even everyday activities such as lifting a child. These repetitive movements can lead to irritation and inflammation of the thumb tendons, worsening the synovial sheath around them.
Additionally, anatomical factors such as a genetic predisposition to having a narrower synovial sheath or anatomical variations of the thumb tendons may also increase the risk of developing de Quervain tenosynovitis. For example, some people may have a natural tendency to develop tendon inflammations due to their specific anatomical structure.
Traumatic injuries to the thumb or wrist, such as a sprain or fracture, may also be associated with the development of de Quervain tenosynovitis. These injuries can lead to acute inflammation of the tendons and synovial sheath, thereby triggering the condition.
Additionally, certain underlying medical conditions, such as rheumatoid arthritis or chronic inflammatory diseases, may increase the risk of developing de Quervain tenosynovitis. These conditions can lead to widespread inflammation throughout the body, including the tendons of the thumb, which may contribute to the development of de Quervain tenosynovitis.
Here are some common causes of de Quervain tenosynovitis:
- Overuse of the Thumb: Frequent use of the thumb in grasping or pinching movements, such as prolonged use of a cell phone, repeated grasping of objects, or knitting activity, can lead to overuse of the tendons and promote the development of Quervain tenosynovitis.
- Repetitive Movements: Occupations or activities involving repetitive movements of the thumb and wrist, such as sewing, computer work, carpentry, may increase the risk of de Quervain tenosynovitis.
- Pregnancy: Some pregnant women may develop this condition due to hormonal changes and fluid retention, which can increase pressure on the tendons.
- General Inflammation: General inflammatory conditions such as rheumatoid arthritis may increase the risk of de Quervain tenosynovitis.
- Trauma: Direct trauma or injury to the wrist, although less common, can also contribute to the development of this condition.
Symptoms of de Quervain tenosynovitis
Quervain tenosynovitis is characterized by specific symptoms that mainly affect the thumb and wrist region. The most common symptoms of this condition usually include pain and tenderness at the base of the thumb, as well as along the side of the wrist. This pain may be described as dull, stabbing, or burning, and it may worsen with certain movements of the thumb or wrist, including gripping objects, twisting the wrist, or stretching the thumb.
Another common feature of de Quervain tenosynovitis is the presence of a swelling or bump at the base of the thumb, caused by inflammation of the synovial sheath that surrounds the tendons. This swelling may be associated with a feeling of warmth or stiffness in the thumb and wrist.
Patients with de Quervain tenosynovitis may also experience a crackling or cracking sensation in the thumb or wrist during certain movements, which may indicate abnormal friction of the inflamed tendons against the synovial sheath.
Additionally, some patients may experience weakness or difficulty using their thumb and wrist habitually due to the pain and discomfort associated with de Quervain tenosynovitis. This weakness may be especially noticeable when performing tasks that require precise gripping or manipulation with the thumb.
Symptoms of de Quervain tenosynovitis can vary in intensity from one individual to another, and they can be exacerbated by certain activities or positions, such as gripping heavy objects, twisting the wrist, or even just resting. thumb and wrist in a prolonged position.
- Wrist and Thumb Pain: The pain is usually felt on the side of the thumb and wrist. It may be described as a shooting pain or burning feeling.
- Swelling: Swelling, often visible at the base of the thumb, may accompany de Quervain tenosynovitis. This can make the area more tense and sensitive to touch.
- Sensitivity to Touch: The affected area may be sensitive to touch. Squeezing or feeling the area around inflamed tendons can make the pain worse.
- Difficulty Grasping Objects: Due to pain and limitation of movement, people with de Quervain tenosynovitis may have difficulty grasping objects, especially those requiring gripping with the thumb.
- Crepitation or Grinding: Some individuals may feel or hear a crackle or grinding sound when they move their thumb or wrist. This may be due to friction of inflamed tendons.
- Radiating Pain in the Forearm: The pain can sometimes radiate down the forearm on the thumb side, worsened by movements involving the thumb and wrist.
- Difficulty Performing Specific Movements: Certain activities, such as twisting the wrist, pinching, or grasping, may be particularly painful and difficult to perform.
- Worsened with Activity: The pain and discomfort associated with de Quervain tenosynovitis is often exacerbated by activities that involve repetitive movements of the thumb and wrist.
Pathophysiology
The pathophysiology of de Quervain tenosynovitis primarily involves inflammation of the tendons located at the base of the thumb, particularly the abductor pollicis longus (APL) and extensor pollicis brevis (EPB) tendons. This inflammation occurs in the fibro-osseous tunnel next to the radial styloid at the distal wrist.
The tendons in question slide through a synovial sheath that holds them in place while allowing fluid movement. When this synovial sheath becomes inflamed, it can lead to thickening and narrowing of the tendon passageway, causing friction and increased irritation during thumb movements.
Several factors can contribute to the pathophysiology of Quervain tenosynovitis:
- Overuse or Repetitive Motions: Activities that involve repetitive movements of the thumb, such as frequent grabbing or pinching, can contribute to tendon irritation.
- Anatomy: Some individuals may have particular anatomy that predisposes to this condition, such as a narrower synovial sheath, which increases the risk of inflammation.
- Hormonal Factors: De Quervain tenosynovitis may be more common in women, and certain hormonal factors may play a role in the development of inflammation.
- Genetic Factors: Genetic predispositions may also influence susceptibility to this condition.
Inflammation of the synovial sheath leads to the production of excess synovial fluid, which worsens swelling and pain. The repetitive movement of the thumb can then become painful and restricted, affecting daily activities.
By understanding these underlying mechanisms, healthcare professionals can tailor treatment approaches to relieve inflammation, reduce pain, and restore normal thumb function.
Differential diagnoses of de Quervain tenosynovitis
The diagnosis of de Quervain tenosynovitis is generally based on clinical examination, the patient’s medical history and specific tests. However, it is also important to rule out other conditions that may present similar symptoms. Here are some differential diagnoses of Quervain tenosynovitis:
- Rheumatoid Arthritis: Rheumatoid arthritis can cause inflammation of the joints, including those in the wrist. Symptoms such as pain and swelling may be similar to those of de Quervain tenosynovitis.
- Osteoarthritis of the Thumb: Osteoarthritis of the thumb, also called rhizarthrosis, is a degeneration of the cartilage at the base of the thumb. It can cause pain and decreased function similar to those of de Quervain tenosynovitis.
- Cystic Ganglion: A synovial cyst or ganglion can form near the tendons of the wrist, causing a lump and pain similar to that of Quervain’s tenosynovitis.
- Carpal Tunnel Syndrome: This condition is characterized by compression of the median nerve at the wrist, causing symptoms such as pain, numbness and weakness in the hand. These symptoms can sometimes be confused with those of Quervain tenosynovitis.
- Tendonitis of Another Tendon: Other tendons in the wrist may also be prone to tendinitis, causing symptoms similar to de Quervain tenosynovitis.
- Infection: An infection of the soft tissues of the wrist can also cause pain and swelling similar to that of de Quervain tenosynovitis.
Finkelstein’s test
The Finkelstein test is a clinical test used to assess the presence of de Quervain tenosynovitis. This test is simple and can be performed in a clinic by a healthcare professional. Here is how it is generally performed:
- Patient Positioning: The patient is asked to place their affected hand with the wrist flexed towards the opposite side of the palm (ulnar). This means that the thumb is folded towards the palm, and the other fingers are closed over the thumb.
- Wrist Movement: The healthcare professional then asks the patient to move the wrist radially, i.e. outwards, while keeping the thumb folded in the palm.
- Interpretation: If this movement causes pain at the base of the thumb (on the wrist side), it is a positive sign of the Finkelstein test. The pain is usually located along the radial edge of the wrist, where the inflamed tendons of de Quervain tenosynovitis pass through a synovial sheath.
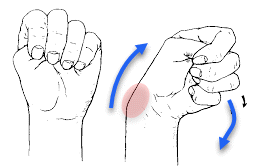
A positive Finkelstein test suggests the possibility of de Quervain tenosynovitis. However, the final diagnosis must be made by a healthcare professional who can take into account other clinical elements, the patient’s history and, if necessary, additional examinations such as x-rays or ultrasounds.
Recommendation
- Rest: Avoid activities that make symptoms worse and give your thumb and wrist time to recover. Rest is often essential to allow healing.
- Application of Ice: Apply ice to the painful area to reduce inflammation. Be sure to wrap the ice in a cloth to avoid direct contact with the skin.
- Elevation: Keep the hand and wrist elevated as much as possible to reduce swelling.
- Splint: A thumb splint or splint can help immobilize the area, reducing pressure on the tendons.
- Anti-inflammatory Medications: Nonsteroidal anti-inflammatory medications (NSAIDs), such as ibuprofen, can help reduce pain and inflammation. However, consult a healthcare professional before taking medications, as they may have side effects.
- Physical Therapy: A physical therapist can recommend specific exercises to strengthen muscles, improve mobility and promote healing.
- Corticosteroid Injections: In some cases, corticosteroid injections may be recommended to reduce inflammation.
- Activity Changes: If specific activities are identified as triggers, consider modifying or limiting those activities to avoid overuse.
Diagnoses of Quervain tenosynovitis
The diagnosis of de Quervain tenosynovitis is generally based on clinical examination, the patient’s medical history and specific tests. Here are some elements commonly used in the diagnosis of de Quervain tenosynovitis:
- Clinical Examination: The healthcare professional will examine the patient’s hand, wrist and thumb to assess the presence of pain, swelling, warmth or redness. Specific tests can be done to reproduce the symptoms.
- Finkelstein test: This test is often used to diagnose de Quervain tenosynovitis. The patient folds the thumb in the palm of the hand and closes the fingers around the thumb. Then he tilts his wrist towards the little finger side. If this causes significant pain at the base of the thumb, it may indicate de Quervain tenosynovitis.
- Imaging Exams:
- Ultrasound: Ultrasound can be used to visualize the tendons and synovial sheath, helping to detect any inflammation or thickening.
- MRI (Magnetic Resonance Imaging): MRI can provide detailed images of soft tissues, helping to confirm the diagnosis.
- Laboratory Tests: Although less common, blood tests can sometimes be done to rule out other conditions, such as inflammatory forms of arthritis.
- History Assessment: The healthcare professional will ask about the patient’s medical history, including daily and work activities, and specific symptoms.
Stretching and exercise
When it comes to de Quervain tenosynovitis, it is crucial to take gentle approaches to reduce pressure on the inflamed tendons. However, it is important to note that exercises and stretches should be performed with caution, and it is recommended to consult a healthcare professional before beginning any exercise program. Here are some stretches and exercises that can be considered under the supervision of a qualified professional:
- Wrist Stretch:
- Extend the affected arm in front of you, palm down.
- With the other hand, apply gentle downward pressure on the fingers to stretch the wrist.
- Hold for 15 to 30 seconds, then release.
- Repeat several times throughout the day.
- Thumb Stretch:
- Extend the affected arm in front of you, palm facing up.
- Bend your thumb inward, toward your little finger.
- Use the other hand to apply light pressure to the thumb.
- Hold for 15 to 30 seconds, then release.
- Repeat several times.
- Forearm Stretch:
- Extend the affected arm in front of you, palm down.
- Use the other hand to gently pull the fingers back.
- Hold for 15 to 30 seconds, then release.
- Repeat several times.
- Wrist Rotation:
- Extend your arm in front of you, palm down.
- Make circular movements with the wrist in both directions.
- Perform this movement slowly and smoothly.
- Muscle Strengthening (under supervision):
- A healthcare professional can recommend specific strengthening exercises for the muscles surrounding the thumb and wrist.
It is essential not to force movements and to respect comfort limits. If pain persists or worsens, it is important to consult a healthcare professional to adjust the treatment plan.
Conclusion
In conclusion, de Quervain tenosynovitis is a painful condition that affects the tendons of the thumb, usually caused by overuse or repetitive movements. The diagnosis of this condition is based on a thorough clinical examination, specific tests and sometimes imaging examinations. It is crucial to consult a healthcare professional to get an accurate diagnosis and put an appropriate treatment plan in place.
Treatment for de Quervain tenosynovitis often aims to reduce inflammation and relieve pain. Approaches such as rest, use of supportive devices, anti-inflammatory medications and physiotherapy may be recommended. In some cases, corticosteroid injections may be considered to reduce inflammation.
Specific exercises and stretches can also be incorporated into the treatment plan to improve flexibility and strengthen surrounding muscles. However, these activities should be undertaken under the supervision of a healthcare professional to avoid worsening the condition.
In summary, early diagnosis and appropriate management of de Quervain tenosynovitis can help relieve symptoms and restore function to the thumb and wrist. People experiencing thumb and wrist pain are encouraged to consult a healthcare professional for treatment tailored to their individual situation.
References
- De Quervain’s tenosynovitis. Mayo Clinic . June 13, 2015; http://www.mayoclinic.org/diseases-conditions/de-quervains-tenosynovitis/basics/definition/con-20027238.
- Meals RA. De Quervain Tenosynovitis. MedscapeReference . July 7, 2016; http://emedicine.medscape.com/article/1243387-overview.
- Aggarwal R, Ring D. de Quervain tendinopathy. UpToDate . Waltham, MA: UpToDate; June 10, 2015; https://www.uptodate.com/contents/de-quervain-tendinopathy .
- Focus PM. Physical Medicine and Rehabilitation for De Quervain Tenosynovitis. MedscapeReference . April 27, 2016; http://emedicine.medscape.com/article/327453-overview#a6.
- Ilyas AM, Ast M, Schaffer AA, Thoder J. De quervain tenosynovitis of the wrist. J Am Acad Orthop Surg . December, 2007; 15(12):757-764. https://www.ncbi.nlm.nih.gov/pubmed/18063716.
- Wikipedia
- Credit in part: Ellen Satteson; Shruti C. Tannan.
















