Introduction
Diffuse idiopathic skeletal hyperostosis (DISH), also known as Forestier’s disease or ankylosing spinal hyperostosis, is a disease characterized by excessive bone formation (hyperostosis) along the spine, joints, and tendons. . This extra bone growth can lead to spinal stiffness and associated symptoms.
Although the exact cause of DISH is not completely understood, it is known that it is not related to inflammation, which sets it apart from some other bone conditions such as ankylosing spondylitis. DISH is often associated with aging, and it is more common in older people. However, it can also affect younger individuals.
The main sites of hyperostosis in DISH include the ligaments along the spine, particularly in the thoracic region. This bone growth can also occur in joints and tendons, which can lead to decreased mobility and flexibility. Common symptoms of DISH include spinal stiffness, limited neck movement, and back pain. These symptoms can vary in intensity from person to person.
An accurate diagnosis of DISH is usually based on medical imaging, such as x-rays. Images may reveal the presence of characteristic bone formations along the spine and in other affected areas. Healthcare professionals may also consider the patient’s clinical symptoms and medical history to confirm the diagnosis.
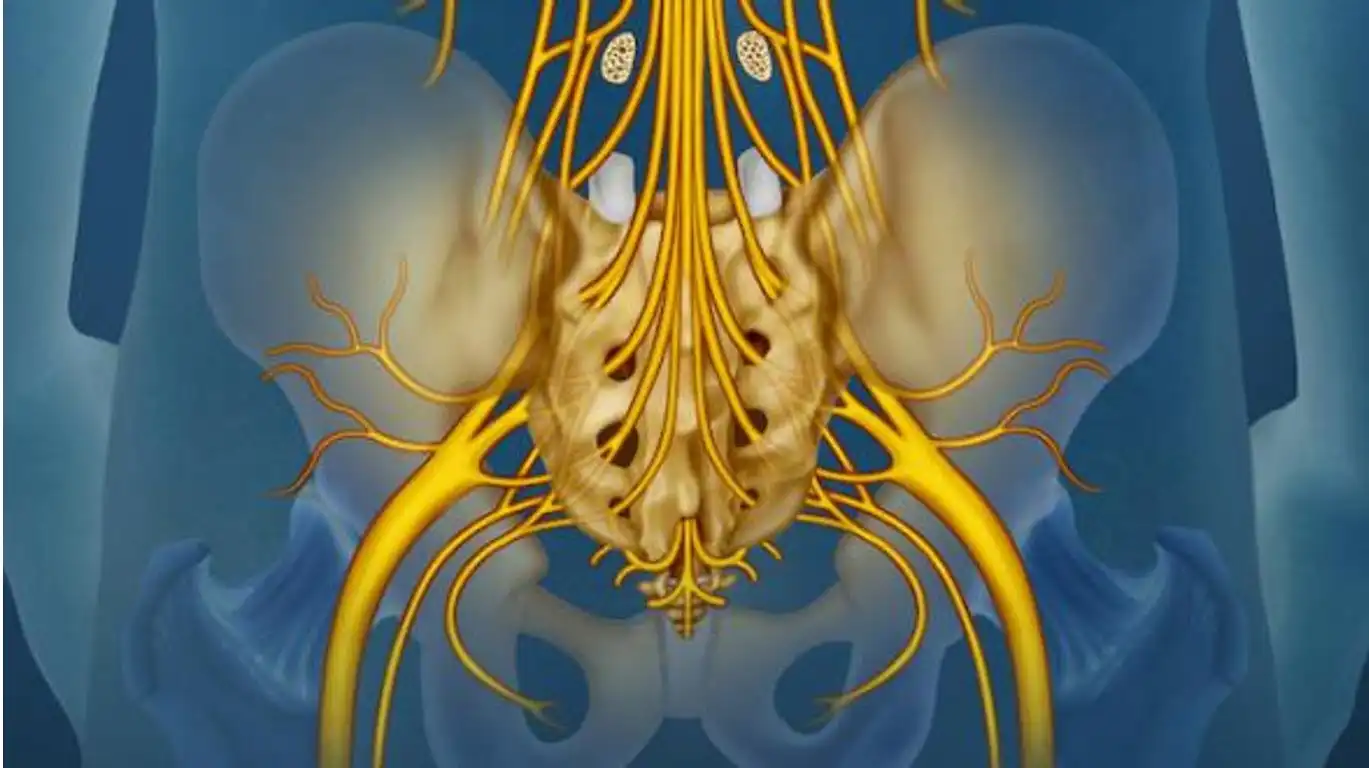
Although DISH is generally considered a benign condition, it can lead to complications in some cases. Compression of adjacent structures, such as the trachea, esophagus or nerves, can cause more serious symptoms. For example, compression of the windpipe can cause breathing problems, while compression of the nerves can lead to pain and impaired nerve function.
Treatment for DISH often aims to relieve symptoms and improve the patient’s quality of life. Non-drug approaches include physiotherapy to maintain flexibility and mobility, as well as weight management to reduce pressure on the spine. Medications such as nonsteroidal anti-inflammatory drugs may be prescribed to relieve the pain and inflammation associated with the condition.
In more serious cases or if complications are present, surgical intervention may be considered. However, the decision to opt for surgery will depend on various factors, such as the severity of symptoms and response to other forms of treatment.
Synonym: Diffuse idiopathic skeletal hyperostosis, Dorsal ensheathing hyperostosis, Ankylosing vertebral hyperostosis, Vertebral ensheathing hyperostosis, Senile vertebral hyperostosis, Forestier’s disease, Forestier and Rotès-Quérol disease, Forestier’s hyperostosing disease, Vertebral melorheostosis
DISH Vs Ankylosing Spondylitis
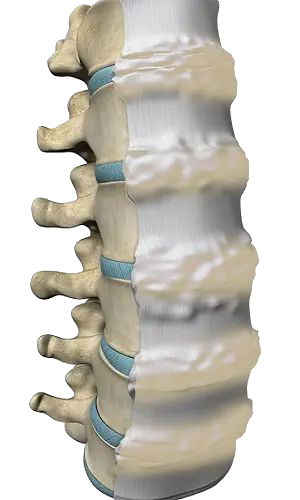
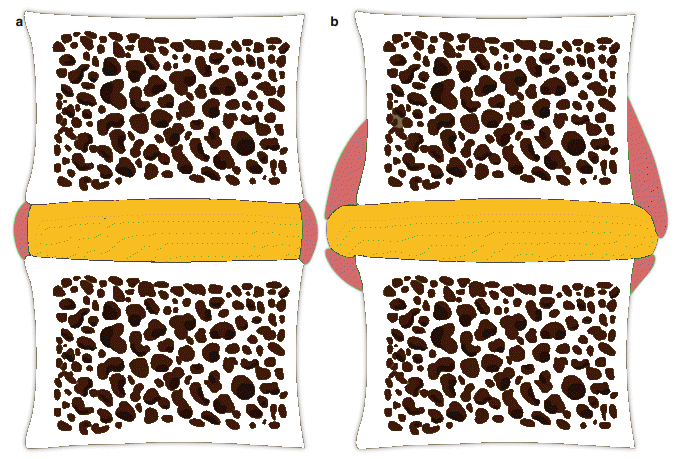
This relatively benign condition is sometimes confused with ankylosing spondylitis. It is characterized and diagnosed by the presence of flowing calcifications and ossification along the anterolateral borders of at least four adjacent vertebral bodies. Disc spaces are, however, preserved (unlike ankylosing spondylitis), without loss of height or other changes. degenerative, and the sacroiliac and facet joints do not become ankylosed. Most cases are asymptomatic, or have mild or moderate restriction of movement in the affected parts of the spine. No treatment is effective.
Diffuse idiopathic skeletal hyperostosis (DISH) is a disease of the back or spine. Unlike other types of arthritis, it does not involve inflammation, but a buildup of calcium salts in the tendons and ligaments (non-marginal syndesmophyte) and abnormal new bone growth (ossification) of the ligaments and connective tissues most commonly in the spine, resulting in “bony bridges” between the vertebrae. This calcification can also be seen in the tissues around other joints in the body (like the elbows, knees, and Achilles tendons) causing bony growths (spurs) where the tendons and ligaments attach to the bone.
Undulating ossification of the anterior longitudinal ligament (OALL)
Undulating ossification of the anterior longitudinal ligament (OALL) can affect both the cervical and dorsal regions of the spine, although its incidence is less common in the latter. This rare condition is characterized by the formation of calcium deposits along the anterior longitudinal ligament, which can lead to a variety of symptoms and requires thorough evaluation for accurate diagnosis and appropriate management.
OALL in the cervical region, corresponding to the cervical spine, can cause symptoms such as neck pain, stiffness, difficulty turning the head, headaches and sometimes neurological symptoms. In the thoracic spine, it can result in back pain, stiffness, limitations of movement and neurological symptoms if the calcification puts pressure on surrounding nerve structures.
The diagnosis of OALL is based on imaging examinations such as x-rays, CT scans or MRIs, making it possible to visualize the ossification of the anterior longitudinal ligament and to assess the extent of the damage. It is essential to note that OALL can be asymptomatic in some individuals and be discovered incidentally during examinations carried out for other reasons.
Management of OALLdepends on the severity of symptoms and the impact on the patient’s quality of life. Conservative approaches such as physiotherapy, anti-inflammatory medications and pain management may be considered. In some cases that are more serious or resistant to conservative treatment, surgery may be recommended to remove the calcification and stabilize the spine.
It is imperative to tailor the management of OALL based on specific symptoms, location of the ossification, and response to different treatment modalities. Close collaboration with healthcare professionals specializing in spinal disorders is essential to ensure thorough assessment and optimal management of this condition, whether it affects the cervical or dorsal region.
- Undulating Ossification of the Anterior Longitudinal Ligament (OALL):
- OALL is a condition characterized by the formation of calcified deposits or ossifications in the anterior longitudinal ligament of the spine. These calcifications may appear wavy on medical imaging images.
- Symptoms may include back pain, stiffness, and sometimes impaired mobility of the spine.
- Diagnosis is usually made using imaging tests, such as x-rays or CT scans.
- Diffuse Idiopathic Skeletal Hyperostosis (DISH):
- DISH, also known as Forestier-Certonciny disease, is a disease characterized by the excessive formation of bone tissue (osteophytes) along ligaments and tendons, primarily in the vertebrae.
- Symptoms often include back pain, stiffness, mobility difficulties and, in some cases, neurological complications.
- Diagnosis is usually based on imaging tests, such as x-rays, showing ossification of ligamentous structures.
Although both conditions involve calcifications or ossifications in the spinal region, they have different clinical features and are often diagnosed by specific imaging tests.
- The space between two vertebrae is also called a non-marginal sydesmophyte
- To confirm the presence of DISH of the spine , there must be presence of calcification of the anterior longitudinal ligament on three successive levels (involving 4 contiguous vertebrae).

Epidemiology of Diffuse Idiopathic Skeletal Hyperostosis (DISH)
DISH is considered a relatively common but underdiagnosed condition. While its exact cause is unknown, it is thought to be related to metabolic disorders, such as obesity, diabetes, and hyperinsulinemia. Below is an overview of the epidemiology of DISH, including its prevalence, demographics, and associated risk factors.
1. Prevalence
The prevalence of DISH varies widely depending on the population studied and the criteria used for diagnosis. Estimates from radiographic studies suggest that the prevalence ranges from 3% to 28% in the general population, depending on age and geographic location.
- General Population: In large population studies, the prevalence of DISH is estimated to be between 10% and 15% in older adults. This wide range is due to differing diagnostic criteria, with some studies requiring stricter evidence of ligamentous ossification and others using broader definitions.
- Elderly Population: DISH is particularly common among the elderly, with prevalence increasing significantly after the age of 50. Studies show that it affects between 15% and 25% of individuals over the age of 65.
- Gender Differences: DISH is more commonly diagnosed in men than in women, with a male-to-female ratio of approximately 2:1 to 3:1. This gender difference is consistent across most studies, though the reasons for it are not entirely understood.
2. Geographic Variation
The prevalence of DISH appears to vary across different regions, though it is found globally. Some of the reported geographic variations may be due to differences in diagnostic practices or the populations studied.
- Western Countries: In the United States and Europe, prevalence rates are similar, ranging from 10% to 20% in older adults.
- Asian Populations: Some studies have shown lower prevalence rates in Asian populations compared to Western populations, although this may be influenced by diagnostic criteria or underreporting.
- Indigenous Populations: Some studies of Indigenous populations and non-Western regions suggest lower rates of DISH, but research in these areas is limited.
3. Age Distribution
DISH is primarily a disease of older adults, and its prevalence increases significantly with age.
- Age 40-50: DISH is rarely diagnosed in individuals under the age of 40, and its prevalence in this age group is low (around 5%).
- Age 50-70: Between the ages of 50 and 70, the prevalence of DISH increases significantly, affecting 10% to 20% of individuals.
- Age 70 and Older: In individuals over the age of 70, the prevalence rises to between 20% and 30%, making it a common condition among elderly populations.
4. Risk Factors
Several risk factors are strongly associated with the development of DISH. These factors include both metabolic conditions and lifestyle factors, suggesting a potential link between DISH and systemic metabolic dysfunctions.
- Obesity: Obesity is one of the most strongly associated risk factors for DISH. Studies indicate that individuals with higher body mass index (BMI) are at a significantly greater risk for developing DISH.
- Type 2 Diabetes Mellitus: There is a well-documented association between type 2 diabetes and DISH. Up to 40% of patients with DISH may have diabetes, and individuals with diabetes are more likely to develop the condition earlier in life.
- Hyperinsulinemia: Elevated insulin levels, often related to insulin resistance, are also strongly linked to DISH. It is thought that hyperinsulinemia may promote abnormal bone growth by stimulating osteoblast activity.
- Metabolic Syndrome: DISH has been associated with metabolic syndrome, which includes factors such as obesity, hypertension, hyperlipidemia, and insulin resistance.
- Male Sex: Men are at a higher risk of developing DISH, though the exact reason for this gender difference is unclear. Some researchers suggest hormonal influences, while others believe it may be related to lifestyle factors such as occupation and physical activity.
- Age: As mentioned earlier, age is one of the strongest risk factors for DISH. The prevalence rises sharply after the age of 50 and continues to increase with each decade of life.
5. Associated Conditions
DISH is often found in conjunction with other musculoskeletal conditions and systemic diseases. Some common conditions that are co-associated with DISH include:
- Osteoarthritis: While osteoarthritis and DISH are distinct conditions, they frequently coexist in older adults. Some studies suggest that individuals with DISH may be at an increased risk of developing osteoarthritis, particularly in the spine and peripheral joints.
- Spinal Stenosis: The ossification of ligaments seen in DISH can lead to spinal stenosis, a narrowing of the spinal canal, which may cause nerve compression and neurological symptoms.
- Enthesopathy: DISH frequently involves the entheses, the sites where tendons and ligaments attach to bones, resulting in enthesopathy (inflammation and ossification of the entheses).
- Hypertension and Cardiovascular Disease: Patients with DISH are more likely to have hypertension and other cardiovascular risk factors, potentially due to shared risk factors like obesity and metabolic syndrome.
6. Complications
Although DISH is often asymptomatic or mildly symptomatic, it can lead to a range of complications, particularly as the disease progresses:
- Spinal Rigidity: As the ligaments and tendons ossify, patients may experience limited spinal mobility and stiffness, especially in the thoracic and cervical regions of the spine.
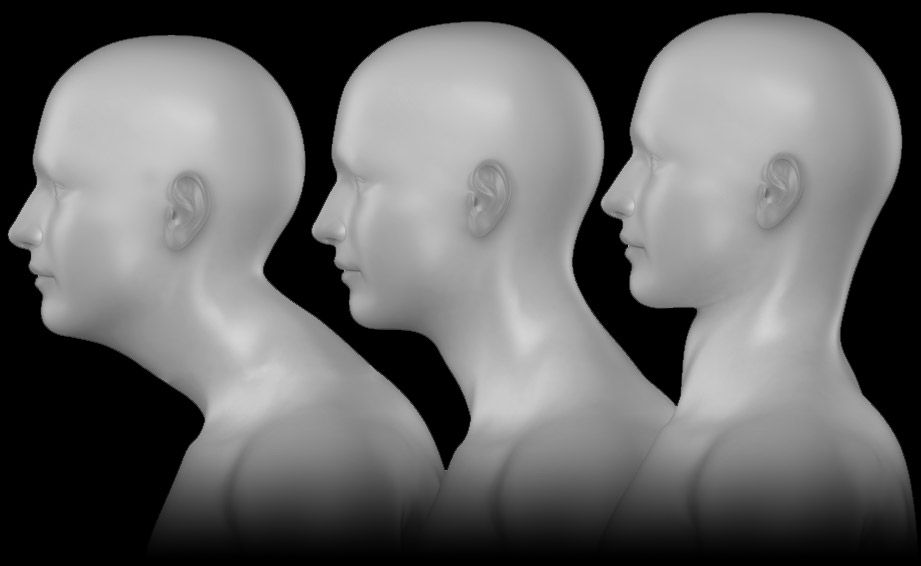
- Dysphagia: In advanced cases of cervical spine involvement, anterior ossification can cause dysphagia (difficulty swallowing) due to compression of the esophagus.
- Fractures: The presence of rigid, ossified ligaments can increase the risk of spinal fractures in individuals with DISH, particularly in the case of trauma, as the spine becomes less flexible.
Causes of DISH
The exact cause of diffuse idiopathic skeletal hyperostosis (DISH), also known as Forestier’s disease, is not fully understood. However, several factors can contribute to its development. Here are some considerations:
- Genetic factors: There is some genetic predisposition to diffuse idiopathic skeletal hyperostosis. Studies have suggested that genetic factors may play a role in susceptibility to this disease.
- Age: DISH tends to mainly affect older people. It is more common in individuals over 50 years old, and the prevalence increases with age.
- Metabolic factors: Certain metabolic factors, such as diabetes, have been associated with an increased risk of developing diffuse idiopathic skeletal hyperostosis. This suggests a possible correlation with carbohydrate metabolism.
- Inflammation: Chronic inflammatory processes may play a role in excessive bone formation. Studies have shown elevated levels of inflammatory markers in some patients with DISH.
- Heredity: There are indications that the disease may be hereditary, meaning it may occur more frequently in people with a family history of the disease.
- Environmental factors: Certain environmental factors, such as diet and lifestyle, could also influence the development of DISH.
It is important to note that although these factors are associated with diffuse idiopathic skeletal hyperostosis, the disease can manifest variably from person to person, and there may be cases where no specific cause is present. is identified (hence the term “idiopathic”). Further research is needed to better understand the underlying mechanisms of this disease.
Symptoms of Diffuse Idiopathic Skeletal Hyperostosis
One of the most common symptoms seen in people with DISH is joint stiffness and pain. These symptoms usually affect the spine, particularly the cervical region, and can extend to other joints such as the shoulders, elbows, hips and knees. Morning stiffness is common and can contribute to decreased joint mobility.
Excessive ossification of ligaments and tendons can also lead to movement limitations, making daily activities more difficult for people with DISH. The formation of bony bridges between vertebrae, known as spondylophytes, can cause spinal fusion, which can have implications for posture and flexibility of the spine.
In some cases, DISH can cause swallowing disorders due to ossification of the pharyngeal ligaments. This can lead to a tight throat feeling and difficulty swallowing, which can impact nutrition and quality of life.
Palpable bony nodules, called exostoses, can sometimes form, particularly in the elbows and knees. These bony growths can be painful and contribute to limited joint mobility in these areas.
Pain associated with DISH can be chronic and have a significant impact on quality of life. Sufferers may experience constant fatigue due to the body’s ongoing efforts to manage excessive ossification and joint limitations.
It is important to note that the symptoms of DISH may progress gradually over time. Some individuals may remain asymptomatic for many years, while others may experience more rapid disease progression.
- Back Pain: Back pain is one of the most common symptoms. It can be intermittent or constant.
- Stiffness: Stiffness of the spine, particularly in the morning or after a period of inactivity, is commonly observed.
- Mobility Difficulties: People with DISH may have difficulty performing certain spinal movements due to ossification of ligaments and tendons.
- Spinal Deformity: In some advanced cases, DISH can cause deformity of the spine, with changes in posture.
- Dysphagia: Difficulty swallowing may occur if ossification affects structures near the throat.
- Neurological Complications: In more severe cases, excessive ossification can compress the spinal cord, leading to neurological symptoms such as numbness, tingling or weakness in the limbs.
Pathophysiology
Diffuse idiopathic skeletal hyperostosis (IDHS) is a complex pathology of the musculoskeletal system, characterized by excessive bone growth, particularly in ligaments and tendons. Although the pathophysiology of DISH is not completely understood, several mechanisms have been identified. Dysregulation of bone metabolism appears to play a major role, with inappropriate activation of osteoblasts leading to abnormal bone growth. At the same time, a chronic inflammatory response is observed in soft tissues and joints, promoting the proliferation of bone cells. Genetic factors are also involved, with genetic associations suggesting mutations that may influence the regulation of bone metabolism and the inflammatory response. Excessive ossification of ligaments and tendons, accompanied by osteophyte formation, contributes to characteristic symptoms such as joint stiffness and pain. Alterations in immune responses and environmental factors, such as trauma or infections, could also contribute to the pathophysiology of DISH. The progression of the disease varies from one individual to another, requiring multidisciplinary management focused on relieving symptoms, preserving joint function and improving quality of life. Although there is no cure, current therapeutic approaches, including anti-inflammatory medications and physiotherapy, aim to alleviate symptoms and minimize complications related to excessive ossification.
- Genetic Predisposition:
- Certain genetic factors may predispose a person to developing DISH, although the precise mechanisms are not clearly defined.
- Inflammation and Initial Injury:
- Chronic inflammation or repeated injury to ligaments and tendons can be initial triggers. This may be due to repetitive microtrauma, mechanical stress or inflammatory processes.
- Osteoblastic Response:
- In response to inflammation or injury, osteoblastic cells, responsible for bone formation, are activated. These cells begin to produce excess bone tissue along the ligaments and tendons, especially in the vertebrae.
- Formation of Osteophytes:
- Osteophytes, or bony growths, gradually form along the ligaments and tendons attached to the vertebrae. These osteophytes can fuse over time, resulting in continued ossification.
- Mineralization and Fusion of the Vertebrae:
- Osteophytes continue to grow and mineralize. Over time, this can cause adjacent vertebrae to fuse, limiting spinal mobility.
- Evolution Towards Spinal Ankylosis:
- Continued ossification and fusion of the vertebrae can lead to spinal ankylosis, where the vertebrae become attached to each other. This can lead to significant stiffness and loss of mobility in the spine.
- Symptoms and Complications:
- DISH may be asymptomatic in some individuals, but in others it can cause back pain, stiffness, and difficulty performing certain movements. In some cases, DISH may also be associated with complications such as swallowing problems or spinal cord compression.
It is important to note that DISH is often diagnosed in its late stages, when symptoms become apparent.
Recommendations
Although there is no specific treatment to cure DISH, some general recommendations can be followed to help manage symptoms and improve quality of life. However, this advice is not a substitute for personalized medical advice, and it is always best to consult a healthcare professional for recommendations specific to your situation. Here are some things to consider:
- Avoid prolonged positions: Avoid staying in the same position for long periods of time, especially if it involves sitting or standing without moving. It is important to take regular breaks to stretch and move the body.
- Maintain moderate physical activity: Regular physical activity can help maintain mobility and strengthen muscles. However, it is important to adopt exercises adapted to your condition. Consult a healthcare professional or physiotherapist for specific recommendations.
- Avoid excessive movements: Avoid excessive movements of the spine which could worsen bone formation. This may include extreme bending or twisting movements.
- Maintain a healthy weight: Maintaining a healthy body weight can help reduce the load on the spine and alleviate some symptoms.
- Eat a balanced diet: A balanced diet can help maintain overall health and support disease management. Consult a healthcare professional or nutritionist for personalized advice.
- Avoid incorrect postures: Adopt correct postures when walking, sitting and other daily activities to minimize pressure on the spine.
- Stress Management: Stress can sometimes worsen the symptoms of various musculoskeletal conditions. Stress management can be beneficial.
- Symptomatic treatment: Depending on the specific symptoms, your healthcare professional may recommend medications or other interventions to relieve pain or discomfort.
Possible complications
Diffuse idiopathic skeletal hyperostosis (DIHS) can cause various complications that significantly impact the daily life of affected individuals. Severe joint stiffness and decreased mobility are direct consequences of ossification of ligaments and tendons, often making daily activities difficult. Chronic pain, resulting from excessive bone growth, can be persistent and require constant management. Functional limitations related to ossification of joint structures can have a significant impact on the ability to perform daily tasks.
Structural deformities, such as spinal curvatures, can not only worsen symptoms but also have cosmetic implications. Respiratory disorders can occur when ossification affects the rib cage, leading to restriction of respiratory movements and, in severe cases, respiratory problems. Swallowing difficulties, caused by ossification of the pharyngeal ligaments, can impact diet and require nutritional adjustments.
Psychosocially, DISH can lead to complications such as anxiety, depression, and self-esteem issues due to its chronic and disabling nature. Additionally, nerve compression from excessive ossification can cause neurological symptoms, such as numbness and tingling. Management of DISH aims to alleviate these complications, involving a multidisciplinary approach with rheumatologists, physiotherapists, mental health professionals and other specialists to offer comprehensive support to those affected by this condition.
- Pain due to impingement on nerves or bony growths
- Acute monoarticular synovitis,
- Limitation of spinal range of motion
- Dysphagia
- Polyarticular pain
- Pain in the spine or extremities
- Increased risk of unstable spinal fractures.
Radiographic Signs
Radiographic signs of diffuse idiopathic skeletal hyperostosis (DIHS) play an essential role in the diagnosis of this rare condition of the musculoskeletal system. Medical imaging, such as radiography, can visualize characteristic changes in bones and periarticular structures, providing valuable clues to confirm the presence of DISH.
One of the distinctive radiographic signs of DISH is the presence of abnormal ossifications along the ligaments, tendons, and joint capsules. These calcium deposits, also called osteophytes, are clearly visible on x-rays, often as lines or bony growths. These osteophytes can be particularly pronounced in the spine, affecting the intervertebral joints and leading to progressive fusion of the vertebrae.
Another radiographic feature of DISH is the formation of bony bridges between the vertebrae, a phenomenon known as spondylophytes. These bony bridges result from the ossification of the anterior longitudinal ligaments, contributing to spinal stiffness and limited mobility. These changes can be clearly identified on spinal radiographs, highlighting the specificity of these alterations in the context of DISH .
X-rays can also reveal structural deformities in joints, such as abnormal curvatures of the spine or changes in posture. These structural alterations, combined with osteophytes and bony bridges, contribute to the overall diagnostic picture of DISH.
It is important to note that radiographic signs of DISH may change over time, reflecting disease progression. In early stages, changes may be less pronounced, sometimes requiring more sensitive imaging tests such as computed tomography (CT) or magnetic resonance imaging (MRI) for more detailed assessment.
- Excessive bone formation: One of the most characteristic radiographic signs of DISH is the presence of excessive bone formations along the spine, facet joints, and tendons. These bony growths can appear dense and rough on x-rays.
- Sacroiliitis: Some patients with DISH may have inflammation of the sacroiliac joints, which may also be visible on x-rays.
- Vertebral hyperostosis: The disease can cause partial or complete fusion of the joints between the vertebrae, which can be seen on x-rays.
- Ossification of ligaments: The ligaments surrounding the spine can undergo ossification, forming additional bony structures, often called “ligament ossification.”
- Spinal ankylosis: Some patients may experience spinal ankylosis, where the vertebrae partially or completely fuse together due to excessive bone formation.
- Thickening of the facet joints: X-rays may show thickening of the facet joints, which are the joints between the vertebrae.
- Preferential location: DISH often has a preferential location in the thoracic and lumbar region of the spine, but it can also affect other parts of the skeleton.

DISH typically affects the spine but can involve other parts of the skeleton. In this case, the abnormal bone growth causes narrowing of the space available for the esophagus, interfering with normal swallowing. Patients with DISH-related dysphagia may experience discomfort or pain while eating, or feel like food is stuck in their throat.
Treatment for dysphagia caused by DISH may involve dietary modifications or, in severe cases, surgical intervention to remove or reduce the bone growth impinging on the esophagus, providing relief and restoring swallowing function. Early diagnosis is crucial to managing symptoms effectively.

As the bone growth extends anteriorly, it can compress the esophagus, which is the tube responsible for moving food from the mouth to the stomach. This compression can obstruct the normal swallowing process, causing discomfort or difficulty when eating or drinking.
Dysphagia in patients with DISH, particularly when the cervical spine is involved, is a serious concern and may require intervention. Treatments may range from diet modifications to surgical removal of the ossified ligament to relieve esophageal compression and restore normal swallowing function. Early detection and treatment are crucial to prevent worsening of symptoms and complications.
References
- Mader R, Verlaan JJ, Buskila D. Diffuse idiopathic skeletal hyperostosis: clinical features and pathogenic mechanisms. Nat Rev Rheumatol. 2013 Dec;9(12):741-50. [ PubMed ]2.
- Belanger TA, Rowe DE. Diffuse idiopathic skeletal hyperostosis: musculoskeletal manifestations. J Am Acad Orthop Surg. 2001 Jul-Aug;9(4):258-67. [ PubMed ]3.
- Resnick D, Shaul SR, Robins JM. Diffuse idiopathic skeletal hyperostosis (DISH): Forestier’s disease with extraspinal manifestations. Radiology. 1975 Jun;115(3):513-24. [ PubMed ]4.
- FORESTIER J, ROTES-QUEROL J. Senile ankylosing hyperostosis of the spine. Ann Rheum Dis. 1950 Dec;9(4):321-30. [ PMC free article ] [ PubMed ]5.
- Vezyroglou G, Mitropoulos A, Antoniadis C. A metabolic syndrome in diffuse idiopathic skeletal hyperostosis. A controlled study. J Rheumatol. 1996 Apr;23(4):672-6. [ PubMed ]6.
- Mader R, Novofastovski I, Schwartz N, Rosner E. Serum adiponectin levels in patients with diffuse idiopathic skeletal hyperostosis (DISH). Clin Rheumatol. 2018 Oct;37(10):2839-2845. [ PubMed ]7.
- Mader R, Novofestovski I, Adawi M, Lavi I. Metabolic syndrome and cardiovascular risk in patients with diffuse idiopathic skeletal hyperostosis. Semin Arthritis Rheum. 2009 Apr;38(5):361-5. [ PubMed ]8.
- Pariente-Rodrigo E, Sgaramella GA, Olmos-Martínez JM, Pini-Valdivieso SF, Landeras-Alvaro R, Hernández-Hernández JL. Relationship between diffuse idiopathic skeletal hyperostosis, abdominal aortic calcification and associated metabolic disorders: Data from the Camargo Cohort. Med Clin (Barc). 2017 Sep 08;149(5):196-202. [ PubMed ]9.
- Orden AO, David JM, Díaz RP, Nardi NN, Ejarque AC, Yöchler AB. Association of diffuse idiopathic skeletal hyperostosis and aortic valve sclerosis. Medicine (B Aires). 2014;74(3):205-9. [ PubMed ]10.
- Cassim B, Mody GM, Rubin DL. The prevalence of diffuse idiopathic skeletal hyperostosis in African blacks. Br J Rheumatol. 1990 Apr;29(2):131-2. [ PubMed ]11.
- Boachie-Adjei O, Bullough PG. Incidence of ankylosing hyperostosis of the spine (Forestier’s disease) at autopsy. Spine (Phila Pa 1976). 1987 Oct;12(8):739-43. [ PubMed ]12.
- Mata S, Wolfe F, Joseph L, Esdaile JM. Absence of an association of rheumatoid arthritis and diffuse idiopathic skeletal hyperostosis: a case-control study. J Rheumatol. 1995 Nov;22(11):2062-4. [ PubMed ]13.
- Mata S, Chhem RK, Fortin PR, Joseph L, Esdaile JM. Comprehensive radiographic evaluation of diffuse idiopathic skeletal hyperostosis: development and interpreter reliability of a scoring system. Semin Arthritis Rheum. 1998 Oct;28(2):88-96. [ PubMed ]14.
- Weinfeld RM, Olson PN, Maki DD, Griffiths HJ. The prevalence of diffuse idiopathic skeletal hyperostosis (DISH) in two large American Midwest metropolitan hospital populations. Skeletal Radiol. 1997 Apr;26(4):222-5. [ PubMed ]15.
- Meyer PR. Diffuse idiopathic skeletal hyperostosis in the cervical spine. Clin Orthop Relat Res. 1999 Feb;(359):49-57. [ PubMed ]16.
- Hirasawa A, Wakao N, Kamiya M, Takeuchi M, Kawanami K, Murotani K, Matsuo T, Deie M. The prevalence of diffuse idiopathic skeletal hyperostosis in Japan – the first report of measurement by CT and review of the literature. J Orthop Sci. 2016 May;21(3):287-90. [ PubMed ]17.
- Bakker JT, Kuperus JS, Kuijf HJ, Oner FC, de Jong PA, Verlaan JJ. Morphological characteristics of diffuse idiopathic skeletal hyperostosis in the cervical spine. PLoS One. 2017;12(11):e0188414. [ PMC free article ] [ PubMed ]18.
- Carile L, Verdone F, Aiello A, Buongusto G. Diffuse idiopathic skeletal hyperostosis and situs viscerum inversus. J Rheumatol. 1989 Aug;16(8):1120-2. [ PubMed ]19.
- Holgate RL, Steyn M. Diffuse idiopathic skeletal hyperostosis: Diagnostic, clinical, and paleopathological considerations. Clin Anat. 2016 Oct;29(7):870-7. [ PubMed ]20.
- Shamrock AG, Donnally III CJ, Varacallo M. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Aug 7, 2023. Lumbar Spondylolysis and Spondylolisthesis. [ PubMed ]21.
- Donnaly III CJ, Hanna A, Varacallo M. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Aug 4, 2023. Lumbar Degenerative Disk Disease. [ PubMed ]22.
- Akhondi H, Varacallo M. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Aug 4, 2023. Rheumatoid Arthritis and Ankylosing Spondylitis. [ PubMed ]23.
- Utsinger PD. Diffuse idiopathic skeletal hyperostosis. Clin Rheum Dis. 1985 Aug;11(2):325-51. [ PubMed ]24.
- Mader R, Buskila D, Verlaan JJ, Atzeni F, Olivieri I, Pappone N, Di Girolamo C, Sarzi-Puttini P. Developing new classification criteria for diffuse idiopathic skeletal hyperostosis: back to square one. Rheumatology (Oxford). 2013 Feb;52(2):326-30. [ PubMed ]25.
- Durback MA, Edelstein G, Schumacher HR. Abnormalities of the sacroiliac joints in diffuse idiopathic skeletal hyperostosis: demonstration by computed tomography. J Rheumatol. 1988 Oct;15(10):1506-11. [ PubMed ]26.
- Kritzer RO, Rose JE. Diffuse idiopathic skeletal hyperostosis presenting with thoracic outlet syndrome and dysphagia. Neurosurgery. 1988 Jun;22(6 Pt 1):1071-4. [ PubMed ]27.
- Palmer JH, Ball DR. Awake tracheal intubation with the intubating laryngeal mask in a patient with diffuse idiopathic skeletal hyperostosis. Anaesthesia. 2000 Jan;55(1):70-4. [ PubMed ]28.
- Vazan M, Ryang YM, Barz M, Török E, Gempt J, Meyer B. Ankylosing Spinal Disease-Diagnosis and Treatment of Spine Fractures. World Neurosurg. 2019 Mar;123:e162-e170. [ PubMed ]29.
- Garber EK, Silver S. Pedal manifestations of DISH. Foot Ankle. 1982 Jul-Aug;3(1):12-6. [ PubMed ]30.
- Haller J, Resnick D, Miller CW, Schils JP, Kerr R, Bielecki D, Sartoris DJ, Gundry CR. Diffuse idiopathic skeletal hyperostosis: diagnostic significance of radiographic abnormalities of the pelvis. Radiology. 1989 Sep;172(3):835-9. [ PubMed ]31.
- Sohn S, Chung CK, Han I, Park SB, Kim H. Increased Bone Mineral Density in Cervical or Thoracic Diffuse Idiopathic Skeletal Hyperostosis (DISH): A Case-Control Study. J Clin Densitom. 2018 Jan-Mar;21(1):68-74. [ PubMed ]32.
- Varacallo M, Davis DD, Pizzutillo P. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Aug 28, 2023. Osteoporosis in Spinal Cord Injuries. [ PubMed ]33.
- Varacallo MA, Fox EJ. Osteoporosis and its complications. Med Clin North Am. 2014 Jul;98(4):817-31, xii-xiii. [ PubMed ]34.
- Porter JL, Varacallo M. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Aug 4, 2023. Osteoporosis. [ PubMed ]35.
- Varacallo M, Seaman TJ, Jandu JS, Pizzutillo P. StatPearls [Internet]. Stat Pearls Publishing; Treasure Island (FL): Aug 4, 2023. Osteopenia. [ PubMed ]36.
- Varacallo MA, Fox EJ, Paul EM, Hassenbein SE, Warlow PM. Patients’ response toward an automated orthopedic osteoporosis intervention program. Geriatr Orthop Surg Rehabil. 2013 Sep;4(3):89-98. [ PMC free article ] [ PubMed ]37.
- Königshausen M, Dudda M, Merle C, Schildhauer TA, Fehmer T. Thoracic vertebral body fracture after total hip replacement in diffuse idiopathic skeletal hyperostosis. Orthopedics. 2012 Jun;35(6):e1000-4. [ PubMed ]38.
- Mata S, Hill RO, Joseph L, Kaplan P, Dussault R, Watts CS, Fitzcharles MA, Shiroky JB, Fortin PR, Esdaile JM. Chest radiographs as a screening test for diffuse idiopathic skeletal hyperostosis. J Rheumatol. 1993 Nov;20(11):1905-10. [ PubMed ]39.
- Lee S, Coel M, Ko J, Edwards J. Diffuse idiopathic skeletal hyperostosis can resemble metastases on bone scan. Clin Nucl Med. 1993 Sep;18(9):791-2. [ PubMed ]