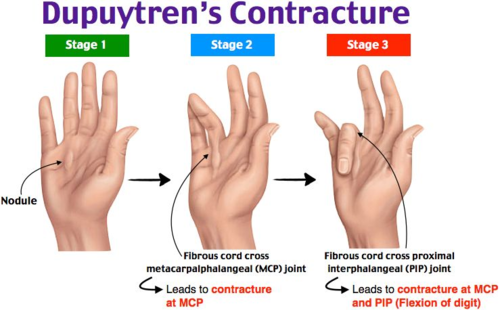
Dupuytren’s contracture is an abnormal thickening of the fascia of the palm of the hand at the base of the fingers. This thickened area may turn into a hard lump or a thick band. Over time, one or more fingers may bend (twitch) or deviate laterally or toward the palm.
Introduction
Dupuytren’s disease, also known as Dupuytren’s contracture, is a medical condition that affects the palm of the hand. This disease is characterized by the development of thick, fibrous scar tissue under the skin of the palm and fingers, leading to varying degrees of contractures.
The medical term “palmar fibromatosis” is also used to describe this condition, highlighting the fibrous nature of the tissue that forms. However, it is commonly called Dupuytren’s disease in honor of Guillaume Dupuytren, a 19th-century French surgeon who was the first to describe in detail the underlying mechanism of this condition.
Dupuytren’s disease usually occurs in middle- to older-aged people. It may have genetic implications, as it tends to occur more frequently in individuals with a family history of the condition. Men are also more likely to be affected than women.
The typical course of Dupuytren’s disease begins with the formation of small bumps or nodules under the skin of the palm. These nodules may be tender, but are usually not painful. Over time, scar tissue develops from these nodules, forming thick ropes that stretch down the length of the fingers. These cords can cause contractures, limiting finger mobility.
The fingers most affected are often the fourth and fifth fingers, although other fingers may also be affected. In severe cases, the fingers may gradually bend toward the palm, making full extension difficult or impossible.
Treatment for Dupuytren’s disease depends on the severity of the symptoms. In the early stages, when the nodules are small and finger mobility is not significantly affected, medical intervention may not be necessary. However, when the contracture becomes more severe, treatment options, including surgery, may be considered to release the strings and restore normal function to the fingers.
Medical research is advancing in the field of Dupuytren’s disease, seeking more effective and less invasive treatment approaches. People suspecting early signs of this condition should consult a healthcare professional for an accurate diagnosis and determine the most appropriate treatment plan. Early treatment can help alleviate symptoms and improve the quality of life of people with Dupuytren’s disease.

This condition is primarily a myofibroblastic disease that affects the palmar and digital fascia of the hand and results in contracture deformities. The most commonly affected fingers are the fourth (ring) and fifth (little finger). The disease first manifests itself in the palm of the hand as painless nodules that form along longitudinal lines of tension. The nodules transform into cords which generate deformations by contracture in the aponeurotic bands and tissues of the hand[1].
Causes of Dupuytren’s disease
The causes of Dupuytren’s disease are not completely understood, but several factors appear to contribute to its development.
Genetic predispositions play a significant role in the occurrence of Dupuytren’s disease. It has been observed that this condition tends to occur in individuals with a family history of the disease, suggesting a hereditary component. Some specific genes have been identified as potentially linked to genetic predisposition to Dupuytren’s disease, although genetics is not the only trigger.
Age and gender are also influential factors. Dupuytren’s disease tends to develop in middle- to older-aged people, usually after age 40. Additionally, men are more frequently affected than women. However, in affected women, the disease can be more severe.
Certain environmental and behavioral risk factors may also contribute to the development of Dupuytren’s disease. Smoking and excessive alcohol consumption have been linked to an increased risk of developing this condition. These habits can act as potential triggers by promoting inflammatory processes and alterations in connective tissues.
Medical factors, such as diabetes, have also been linked to an increased risk of Dupuytren’s disease. Although the precise nature of this association is not fully understood, it is suggested that metabolic changes associated with diabetes may contribute to excessive hand tissue fibrosis.
Dupuytren’s disease is more common in certain populations, particularly those of Northern European origin. There is a significant geographic incidence, and the prevalence of the disease varies across the world.
- Heredity: Genetics plays an important role in the development of Dupuytren’s disease. If members of your family have had the disease, you may be more likely to develop it.
- Ethnicity: Dupuytren’s disease is more common in people of European descent, particularly of Nordic ancestry.
- Sex and age: Men are more likely to develop the disease than women. Additionally, Dupuytren’s disease is more common in middle- to older-aged people, usually after the age of 40.
- Smoking: Smoking has been associated with an increased risk of developing Dupuytren’s disease.
- Alcohol: Excessive alcohol consumption has also been identified as a potential risk factor.
- Diabetes: There are some associations between diabetes and Dupuytren’s disease, although the nature of this relationship is not completely understood.
- Environmental factors: Certain environmental factors, such as repeated hand injuries or constant vibration, have been studied as possible risk factors.
- Associated diseases: There are associations between Dupuytren’s disease and other medical conditions, such as Ledderhose disease (which affects the feet) and Peyronie’s disease (which affects the penis).
Although these factors are associated with increased risk, Dupuytren’s disease can also develop without any of these risk factors being present.
Symptoms of Dupuytren’s disease
The symptoms of Dupuytren’s disease are primarily characterized by a progressive contraction of the connective tissues of the palm of the hand, leading to changes in the position of the fingers, particularly the fourth and fifth fingers. The initial manifestation of Dupuytren’s disease often presents as nodules or small palpable masses in the palm, usually painless in the early stages.
As the disease progresses, these nodules may develop into thick fibrous cords, creating tension in the palm. One of the first noticeable signs is the progressive retraction of the fingers, mainly at the proximal joint and the distal phalanx. This contraction, known as Dupuytren’s contracture, can cause the fingers to permanently flex toward the palm, limiting joint mobility and making it difficult to fully extend the fingers.
Symptoms of Dupuytren’s disease can vary in severity and progression. Some individuals may experience only minor discomfort, while others may experience more significant functional limitations. The presence of nodules, although they are not always painful, can be the first indicator of the disease.
Progressive contracture of the fingers can make daily activities difficult. The inability to fully extend the fingers can affect grasping objects, manipulating small objects, and even performing simple gestures. In more advanced cases, this limitation of mobility can lead to significant deformation of the hand, impacting functionality and aesthetics.
Dupuytren’s disease can also manifest bilaterally, affecting both hands asymmetrically. Although symptoms may progress slowly over several years, it is essential to consult a healthcare professional at the first signs to obtain an accurate diagnosis and explore appropriate treatment options.
Complications related to Dupuytren’s disease may also include feelings of tightness, pain, or discomfort in the affected palm and fingers. The progression of the disease can vary between individuals, and some may never experience significant symptoms, while others may be more severely affected.
- Nodule formation: Dupuytren’s disease often begins with the formation of small nodules under the skin of the palm of the hand. These nodules may be tender to the touch.
- Cord retractions: Over time, nodules can develop into thick, fibrous cords. These cords can cause the fingers, usually the ring and little fingers, to contract and lead to loss of mobility.
- Finger deformity: Fibrous cords can cause the fingers to gradually flex toward the palm, creating a deformity known as Dupuytren’s contracture.
- Difficulty extending fingers: As the disease progresses, it may become difficult for the affected person to fully extend the affected fingers.
- Pain and tenderness: Some people with Dupuytren’s disease may experience pain or tenderness around the nodules or cords.
- Formation of cracks or folds: The skin above the nodules and cords may form cracks or folds.
Pathophysiology
The pathophysiology of Dupuytren’s disease, although complex, primarily involves changes in the connective tissues of the palm of the hand. The disease is characterized by excessive fibrosis, leading to the formation of nodules, thick cords, and ultimately contractures of the fingers. Several biological processes underlie these tissue alterations.
The first step in the pathophysiology of Dupuytren’s disease is the formation of nodules. These nodules are made up of cells called myofibroblasts, which are responsible for the excessive production of collagen and other components of the extracellular matrix. This excess deposition of collagen creates thick fibrous structures that are palpable in the palm of the hand.
As the disease progresses, these nodules evolve into fibrous cords. Myofibroblasts continue to proliferate and produce collagen, resulting in the formation of cords that gradually retract. These cords can pull on surrounding structures, causing permanent flexion of the fingers at the proximal joint and distal phalanx.
The precise mechanisms that trigger excessive fibrosis in Dupuytren’s disease are not fully understood, but genetic factors appear to play a major role. Studies have identified several genes associated with predisposition to Dupuytren’s disease, and a significant hereditary component has been observed. Genetic alterations can influence the response of connective cells to growth signals, thereby leading to abnormal collagen production.
In addition to genetic factors, environmental factors such as smoking and alcohol consumption have been associated with an increased risk of developing Dupuytren’s disease. These habits can create an inflammatory environment in the tissues, promoting excessive fibrosis.
Changes in local vasculature have also been suggested to contribute to the pathophysiology of Dupuytren’s disease. Impaired blood circulation can affect the delivery of nutrients and oxygen to tissues, contributing to fibrosis and nodule formation.
Dupuytren’s disease can sometimes be associated with other medical conditions such as diabetes. Although the exact nature of this association is not completely understood, diabetes-related metabolic changes could influence the development of fibrosis.
- Formation of Palmar Nodules:
- Dupuytren’s disease usually begins with the formation of palpable nodules under the skin of the palm of the hand. These nodules are often painless at first.
- Activated Myofibroblasts:
- These nodules are composed of cells called myofibroblasts, which are activated in an abnormal way. Myofibroblasts are responsible for the contraction of connective tissue.
- Excessive Collagen Production:
- Activated myofibroblasts excessively produce collagen fibers, a structural protein found in connective tissue. This overproduction of collagen leads to the formation of thick cords in the palm of the hand.
- Thick Ropes and Finger Retraction:
- Over time, thick ropes of connective tissue develop from the nodules, causing the fingers to retract. This gradual retraction can lead to loss of mobility and deformity of the fingers.
- Heredity and Genetic Factors:
- Dupuytren’s disease often has a genetic component. Hereditary factors may predispose some people to developing this condition, although other factors, such as age, male gender, smoking, alcoholism, and diabetes, may also play a role.
- Fibroblast Proliferation:
- Fibroblasts, which are cells responsible for collagen production, proliferate abnormally in Dupuytren’s disease. This contributes to the buildup of connective tissue and the formation of thick cords.
- Impairment of the Palmar Fascia:
- Dupuytren’s disease primarily affects the palmar fascia, a layer of connective tissue under the skin of the palm of the hand. Contracture often occurs in the flexor tendons of the fingers, causing permanent flexion.
- Progressive Evolution:
- Dupuytren’s disease has a progressive course, with contracture that can develop slowly over several years. It can affect one or more fingers and, in some cases, both hands.
- Treatment:
- Treatment for Dupuytren’s disease depends on the severity of the symptoms. It may include regular monitoring, physiotherapy, injection of medication (collagenase) to dissolve the cords, or in more advanced cases, surgery to release the tendons and improve mobility of the fingers.
Risk factors
Risk factors associated with Dupuytren’s disease play a crucial role in understanding the predisposition and likelihood of development of this condition affecting the connective tissues of the hand. These factors can be divided into several categories, providing insight into genetic, demographic, lifestyle, and medical influences.
At the heart of risk factors is genetic predisposition. Dupuytren’s disease has a strong hereditary component, with family history significantly increasing the risk of developing this condition. Studies have identified specific genes linked to genetic susceptibility to the disease, highlighting the importance of genetic influences in its occurrence.
Age and gender also emerge as determining elements. Dupuytren’s disease has a higher prevalence in middle- to older-aged individuals, usually after age 40. Additionally, men are more commonly affected than women, although severity may vary by gender.
Demographic characteristics, such as ethnicity, also play a role in risk factors. Dupuytren’s disease shows differences in prevalence between ethnic groups, being more common in people of Northern European descent.
Lifestyle habits, particularly smoking and excessive alcohol consumption, are emerging as modifiable factors associated with increased risk of Dupuytren’s disease. These behaviors can contribute to inflammatory processes and alterations in connective tissues, exacerbating the development of the disease.
Certain medical conditions, such as diabetes, are also linked to increased risk. The precise mechanisms of this association require further exploration, but underlying metabolic changes may play a role in disease progression.
Finally, occupational factors and repeated hand trauma may be elements of risk, although the exact nature of this relationship is not always clear.
- Age: Dupuytren’s disease is more common in middle-aged and older people. It generally occurs after the age of 50.
- Heredity: There is a genetic component to Dupuytren’s disease. If family members have been affected, the risk may be higher.
- Gender: Men tend to develop Dupuytren’s disease more frequently than women.
- Ethnic origin: Dupuytren’s disease is more common in people of European origin, particularly those of Nordic origin.
- Genetic factors: Certain genes have been associated with an increased risk of developing Dupuytren’s disease.
- Smoking and alcohol: There are possible links between smoking, excessive alcohol consumption and the development of Dupuytren’s disease.
- Diabetes: It has been suggested that diabetes may be a risk factor, although the relationship is not completely understood.
A Day in the Life of Someone Suffering from Dupuytren’s Disease
6:30 AM: Waking Up to a Constant Reminder
Maria, a 55-year-old retired piano teacher, begins her day with a familiar challenge. She suffers from Dupuytren’s disease, a condition that causes the fingers, especially the ring and little fingers, to curl inward due to thickening of the palmar fascia. As she wakes up, she instinctively stretches her hands, feeling the tension and stiffness in her right palm. The once-fluid movements of her fingers now feel constrained and rigid, serving as a constant reminder of her condition. Maria massages her hands with a warm cloth to ease the stiffness, starting her day with the care her hands need.
7:00 AM: Morning Routine with Modifications
Getting ready in the morning has become a meticulous process for Maria. Brushing her teeth, washing her face, and styling her hair take longer than they used to. Her fingers don’t move as they once did, requiring her to use adaptive tools to maintain her independence. Her toothbrush has a thicker handle, and the hairbrush is modified to fit comfortably in her hand. These adjustments, though small, are vital for her to navigate her daily routine independently.
8:00 AM: Breakfast Challenges
Preparing breakfast is another task that demands creativity and patience. Maria uses specialized kitchen tools, like easy-grip utensils and jar openers, to help her prepare meals without straining her hands. Cutting fruits, pouring milk, or even making coffee requires extra attention and care. Despite the difficulties, Maria takes pride in maintaining her autonomy, finding innovative solutions to complete everyday tasks.
9:00 AM: Coping with Work and Hobbies
Maria no longer teaches piano full-time due to her condition, but she still tutors a few students privately. Teaching piano with Dupuytren’s disease is challenging, but Maria finds joy in sharing her passion for music. She demonstrates techniques using modified finger positions and encourages her students with her determination. Maria’s approach to teaching has changed, focusing more on theory and ear training, but her love for music remains unwavering.
12:00 PM: Lunch and Hand Exercises
Lunch is a time for Maria to rest and perform her hand exercises. Her therapist has given her a series of exercises to help maintain her finger mobility and slow the progression of her condition. These exercises include gentle stretching, squeezing a soft ball, and using a therapy putty to strengthen her hands. Maria also applies a moisturizing cream to her hands to keep the skin supple, which helps ease some of the tightness she experiences.
2:00 PM: Social Engagements
In the afternoon, Maria often meets friends for a social gathering or engages in community activities. Socializing is essential for Maria’s mental well-being, providing a sense of connection and belonging. However, activities like holding a cup or shaking hands remind her of her limitations. Despite this, Maria remains upbeat and focuses on the joy of interaction, using humor to navigate any awkward situations that arise from her condition.
5:00 PM: Evening Reflection and Adaptation
As the day winds down, Maria spends time reflecting on her day. She journals about her experiences and challenges, finding solace in expressing her thoughts and emotions. Writing has become therapeutic, allowing her to document her journey with Dupuytren’s disease. She often uses voice-to-text software for longer entries, reducing the strain on her hands.
7:00 PM: Dinner and Relaxation
Preparing dinner is a slower process, similar to breakfast and lunch. Maria takes her time, mindful of her limitations, and enjoys the satisfaction of a meal well-prepared. In the evening, she practices relaxation techniques such as deep breathing and meditation, focusing on mental well-being to cope with the frustrations of her physical condition. Maria understands the importance of a positive mindset in managing her disease.
9:00 PM: Preparing for Bed
Before heading to bed, Maria performs her nighttime hand routine. She gently stretches her fingers and applies a soothing balm to keep them flexible. As she settles into bed, she places a soft splint on her hand to keep her fingers in a more extended position overnight. This routine is crucial in managing the progression of her condition and ensuring a more restful sleep.
10:00 PM: Ending the Day with Hope
Maria ends her day with hope and resilience. She knows that living with Dupuytren’s disease requires adaptability and perseverance, but she remains determined to live life on her terms. Each day presents its challenges, but Maria is committed to finding joy and fulfillment, embracing life with strength and courage. Her journey with Dupuytren’s disease is a testament to her resilience, and she looks forward to new beginnings each morning.
Diagnosis and treatment of Dupuytren’s disease
The diagnosis of Dupuytren’s disease is generally based on a clinical examination performed by a healthcare professional, such as a hand surgeon or rheumatologist. Characteristic symptoms include the formation of nodules under the skin of the palm of the hand and progressive contraction of the fingers, especially the fourth (ring) and fifth (little) fingers. Imaging tests such as ultrasound can sometimes be used to assess the extent of the disease.
Regarding the treatment of Dupuytren’s disease, several approaches can be considered, depending on the severity of the symptoms and the associated functional impairment. The main treatment options include:
- Observation: In the early stages of the disease, when the symptoms are mild, the doctor can simply monitor the progress of the disease without initiating immediate treatment.
- Drug therapy: Certain medications, such as collagenase, may be injected into the affected area to weaken scar tissue and make contractions easier to break.
- Physical therapy: Physiotherapy and osteopathy sessions may be recommended to maintain finger mobility and prevent serious deformities.
- Orthotics: Using splints or orthotics can help maintain normal finger position and prevent further deformity.
- Surgery: In cases of severe finger contraction and significant impact on function, surgery may be considered. The procedure usually involves incision and excision of contracted scar tissue.
- Laser therapy: Laser therapy techniques have been explored to treat Dupuytren’s disease, but their effectiveness is still being evaluated.
It is important to note that Dupuytren’s disease can be recurrent, and treatments may not prevent the nodules or contractions from reappearing. The choice of treatment depends on many factors, including severity of symptoms, impact on hand functionality, and patient preference. It is recommended to discuss with a healthcare professional to determine the best treatment approach for each specific case.
Conclusion
Dupuytren’s disease, a progressive condition primarily affecting the connective tissues of the hand, highlights the complex interplay of genetic, environmental, and lifestyle factors. Despite its sometimes subtle onset, Dupuytren’s disease can significantly impact hand function, emphasizing the importance of early diagnosis and personalized treatment strategies. The disease’s pathophysiology involves excessive fibrosis leading to nodule and cord formation, which gradually retract the fingers and limit mobility. With its higher prevalence in individuals of Northern European descent, particularly men over the age of 40, Dupuytren’s disease demonstrates a marked hereditary component.
While the exact mechanisms behind Dupuytren’s disease remain incompletely understood, ongoing research continues to uncover genetic predispositions and the role of modifiable risk factors such as smoking and alcohol consumption. Advances in treatment, including less invasive options like collagenase injections and laser therapy, offer hope for more effective management of the condition. However, it is crucial for individuals, particularly those with a family history, to seek early consultation with healthcare professionals to monitor and address the disease’s progression.
Ultimately, managing Dupuytren’s disease requires a comprehensive approach, combining patient education, lifestyle modifications, and appropriate therapeutic interventions to maintain hand function and improve quality of life. By understanding the multifaceted nature of this condition, patients and healthcare providers can work together to mitigate its impact and explore the most suitable treatment pathways tailored to individual needs.
References
- Hindocha S. Risk Factors, Disease Associations, and Dupuytren Diathesis. Hand Clin. 2018 Aug;34(3):307-314. [ PubMed ]
- Ross DC. Epidemiology of Dupuytren’s disease. Hand Clin. 1999 Feb;15(1):53-62, vi. [ PubMed ]
- Benson LS, Williams CS, Kahle M. Dupuytren’s contracture. J Am Acad Orthop Surg. 1998 Jan-Feb;6(1):24-35. [ PubMed ]
- Larsen S, Krogsgaard DG, Aagaard Larsen L, Iachina M, Skytthe A, Frederiksen H. Genetic and environmental influences in Dupuytren’s disease: a study of 30,330 Danish twin pairs. J Hand Surg Eur Vol. 2015 Feb;40(2):171-6. [ PMC free article ] [ PubMed ]
- Hettiaratchy S, Tonkin MA, Edmunds IA. Spiraling of the neurovascular bundle in Dupuytren’s disease. J Hand Surg Eur Vol. 2010 Feb;35(2):103-8. [ PubMed ]
- Dolmans GH, Werker PM, Hennies HC, Furniss D, Festen EA, Franke L, Becker K, van der Vlies P, Wolffenbuttel BH, Tinschert S, Toliat MR, Nothnagel M, Franke A, Klopp N, Wichmann HE, Nürnberg P, Giele H, Ophoff RA, Wijmenga C., Dutch Dupuytren Study Group. German Dupuytren Study Group. LifeLines Cohort Study. BSSH-GODD Consortium. Wnt signaling and Dupuytren’s disease. N Engl J Med. 2011 Jul 28;365(4):307-17. [ PubMed ]
- Layton T, Nanchahal J. Recent advances in the understanding of Dupuytren’s disease. F1000Res. 2019;8 [ PMC free article ] [ PubMed ]
- Melling M, Karimian-Teherani D, Mostler S, Behnam M, Sobal G, Menzel EJ. Changes of biochemical and biomechanical properties in Dupuytren disease. Arch Pathol Lab Med. 2000 Sep;124(9):1275-81. [ PubMed ]
- Verjee LS, Midwood K, Davidson D, Essex D, Sandison A, Nanchahal J. Myofibroblast distribution in Dupuytren’s cords: correlation with digital contracture. J Hand Surg Am. 2009 Dec;34(10):1785-94. [ PubMed ]
- McCarty S, Syed F, Bayat A. Role of the HLA System in the Pathogenesis of Dupuytren’s Disease. Hand (NY). 2010 Sep;5(3):241-50. [ PMC free article ] [ PubMed ]