Overview of Elbow Dislocation
Elbow dislocation, a common traumatic injury, occurs when the forearm bones, the radius and ulna, move relative to the upper arm bone, the humerus. This painful condition often originates from trauma such as a fall on an outstretched arm or a direct impact on the elbow. When the bones that form the elbow joint are forced out of their normal position, it can lead to damage to the surrounding ligaments, nerves, and blood vessels.
The causes of elbow dislocation are often linked to accidents, falls or violent impacts. Athletes, in particular, are susceptible to this type of injury, especially in sports such as football, rugby or gymnastics. Symptoms of elbow dislocation include severe pain, immediate swelling, visible deformity of the joint, and an inability to move the elbow normally.
When an elbow dislocation is suspected, prompt medical evaluation is crucial to determine the extent of the damage and plan appropriate treatment. Healthcare professionals may perform x-ray examinations to confirm the dislocation and assess for any associated complications, such as a concomitant fracture. Prompt treatment of this injury helps minimize the risk of long-term complications and promotes more effective recovery.
First aid for an elbow dislocation can be administered at the scene of the accident before consulting a healthcare professional. It is imperative to maintain calm, immobilize the affected arm as much as possible, and apply ice to reduce swelling. Restraint with a splint can be beneficial to stabilize the joint and prevent involuntary movement. However, any attempt at reduction (returning the bones to their normal position) should be avoided without the assistance of a qualified healthcare professional, as incorrect handling can make the damage worse.
Medical treatment may involve reducing the dislocation, usually done by a doctor or orthopedist. In some complex cases, surgery may be necessary to restore the integrity of the joint. After reduction, a period of rest, immobilization and rehabilitation is essential to promote healing and restore normal function to the elbow. Physical therapy sessions aimed at strengthening surrounding muscles and improving range of motion may be prescribed.
It is crucial to emphasize that prevention remains an essential component of the management of elbow dislocations. Proper use of protective equipment in sporting activities, adoption of correct fall techniques, and caution during risky activities can help minimize the potential for traumatic elbow injuries.
Primary Causes
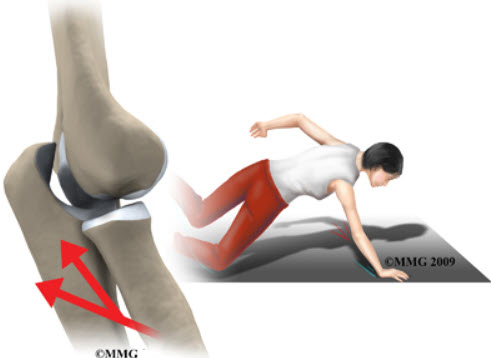
Elbow dislocation usually results from significant traumatic forces applied to the joint, causing the bones that compose it to move. A common cause of elbow dislocation is a fall on an outstretched arm. When a person falls, they instinctively tend to put their hands forward to absorb the shock, thus exposing the elbow to excessive stress. Similarly, a direct impact on the elbow, such as from a car accident or sports collision, can result in a force strong enough to dislodge the bones from their normal position.
Sports accidents represent another major source of elbow dislocations. Contact sports or those involving frequent falls, such as football, rugby, or gymnastics, increase the risk of severe joint trauma. During these activities, sudden movements, collisions with other players, or poorly controlled falls can lead to elbow dislocations.
Dislocations can also occur due to repetitive movements or excessive strain during certain activities. Workers involved in physically demanding tasks, such as heavy lifting or construction work, may be at increased risk of elbow dislocation due to repeated stress on the joint.
It is important to note that vulnerability to elbow dislocations may be influenced by pre-existing anatomical factors. Some people may have a more lax joint or ligament structure, increasing their susceptibility to traumatic injury.
Elbow dislocations are also more common in children and adolescents due to the still developing nature of their bones and ligaments. Young people’s elbows may be more easily dislodged due to the increased flexibility of their joint structures.
Finally, a history of elbow dislocations increases the risk of recurrence. Once the joint is displaced, surrounding ligamentous structures and tissues may be weakened, making the elbow more susceptible to subsequent dislocations, even with lesser forces.
Elbow dislocation can also be associated with fractures, creating more complex situations. Joint fractures can result from the same traumatic mechanism responsible for the dislocation, leading to significant impairment of joint stability.
- Falls: A direct fall onto the outstretched arm can exert enough force to dislodge the bones in the elbow joint.
- Sports Accidents: Contact sports or those involving the risk of falling, such as football, rugby, or gymnastics, can increase the risk of elbow dislocation.
- Traffic Accidents: Car accidents, falls from a bicycle, or other traffic accidents can generate significant force on the elbow, resulting in dislocation.
- Direct Impact: Direct impact to the elbow, such as from a collision with an object or hard surface, can cause dislocation.
- Violent Trauma: Any violent trauma to the elbow can potentially cause dislocation, particularly if force is applied in an unusual direction.
Key Symptoms
Elbow dislocation manifests itself through a range of symptoms that signal significant disruption to the joint. One of the most obvious signs is severe pain in the elbow, usually occurring immediately after the trauma. This pain can be sharp and stabbing, making it difficult to move the joint. Individuals who have suffered an elbow dislocation frequently report a sensation of abnormal displacement of the bones, accentuated by a visible deformation of the joint. Loss of the normal shape of the elbow is often noticeable and can create an asymmetrical appearance.
Immediate swelling of the affected area is also a common symptom of elbow dislocation. This swelling results from inflammation of the surrounding soft tissues in response to the injury. The elbow area may become hot to the touch due to this inflammation, adding to the overall discomfort felt by the individual. Swelling can also contribute to further restricting the mobility of the joint.
Besides pain and swelling, an inability to move the elbow normally is a significant symptom of the dislocation. The joint, due to disruption of the surrounding bones and tissues, may lose its normal functionality. Attempts to flex or extend the elbow can be extremely painful and encounter resistance due to deviation of the anatomical structures.
A feeling of tingling, numbness, or weakness in the fingers may also accompany elbow dislocation. This may indicate damage to the peripheral nerves resulting from the trauma. Neighboring nerves may be compressed or stretched during the dislocation, causing abnormal sensations down the arm to the fingers.
Finally, elbow dislocation can lead to vascular complications, although less common. Damage to blood vessels near the joint can cause blood circulation problems. This may manifest as paleness or blueness of the skin around the elbow, signs indicating a disruption in blood supply.
It is crucial to note that the severity of symptoms can vary depending on the nature and severity of the dislocation. Simple dislocations, without associated fractures, may have less pronounced symptoms than complex dislocations involving extensive damage to surrounding structures.
When faced with suspicious symptoms of elbow dislocation, it is imperative to consult a healthcare professional quickly. A thorough medical evaluation, often supplemented by radiological examinations, is essential to confirm the diagnosis, assess the extent of damage and develop an appropriate treatment plan. Prompt management of elbow dislocation not only helps relieve immediate pain, but also minimizes potential long-term complications and promotes effective recovery of normal joint function.
- Acute Pain: Pain in the elbow is one of the most immediate symptoms. It is often acute and intense, especially at the time of injury.
- Swelling: The area around the elbow may have significant swelling due to tissue inflammation.
- Visible Deformity: In some cases, a deformity or abnormal appearance of the elbow may be visible, particularly if the dislocation is severe.
- Limitation of Mobility: The ability to bend or extend the elbow may be significantly reduced due to the injury. Mobility may be limited due to pain and muscle tension.
- Numbness or Tingling: Sensations of numbness or tingling may occur, particularly if nerve structures were affected during the dislocation.
- Sensitivity to Touch: The elbow area may be sensitive to touch, and even slight movements can trigger pain.
- Bruising: Bruising, commonly known as “bruises,” may appear around the elbow due to broken blood vessels.
Pathophysiology
The pathophysiology of elbow dislocation involves a complex disruption of the anatomical structures that make up this crucial joint. The elbow joint is made up of three main bones: the humerus, radius and ulna. These bones are held in place by a network of ligaments, tendons, muscles and cartilaginous structures, forming a functional joint unit. Elbow dislocation occurs when these structures are subjected to traumatic forces that exceed their ability to maintain stability.
One of the most common forms of dislocation is posterior elbow dislocation, where the lower end of the humerus is forced out of the joint posteriorly. This violent movement can damage the medial and lateral collateral ligaments, which are essential for stabilizing the elbow joint. Excessive force can also lead to associated fractures of the humerus, radius, or ulna bone.
Anterior dislocation of the elbow is less common but can also occur, resulting in the lower end of the humerus protruding forward. In this case, the posterior ligaments may be stretched or torn, causing damage to the opposite part of the joint.
When the elbow is dislocated, the ligaments that hold the bones in place are often stretched beyond their physiological limit. This creates significant joint instability, leading to immediate loss of normal joint function. Damaged ligaments may also bleed, contributing to the immediate swelling seen after the injury.
Surrounding soft tissues, such as tendons and muscles, can also be affected during an elbow dislocation. They can be stretched, torn, or pinched between displaced bony surfaces, causing additional pain and contributing to limited mobility.
The nerves that pass through the elbow area may be compressed or stretched during the dislocation, leading to neurological symptoms. This may appear as tingling, numbness or weakness in the fingers and hand. In severe cases, an elbow dislocation can cause more serious nerve damage, leading to permanent impairment of muscle sensation or function.
In terms of blood flow, elbow dislocation can also cause vascular damage, although this is less common. Blood vessels near the joint may become compressed or torn, causing circulation problems and symptoms such as pale or blue skin.
The pathophysiology of elbow dislocation highlights the complexity of the interactions between the different anatomical structures and the potentially serious consequences of their displacement. Early recognition of these injuries and prompt medical intervention are essential to minimize damage, restore joint stability, and promote optimal recovery. Treatment approaches may include reduction of dislocation, repair of damaged ligaments, and management of associated complications such as fractures, nerve or vascular injuries. By understanding the pathophysiology of elbow dislocation, healthcare professionals can develop treatment plans tailored to the specific severity of each case.
- Initial Trauma: Elbow dislocation is usually triggered by initial trauma, such as a fall on the outstretched arm, direct impact on the elbow, or violent trauma during sporting activities.
- Ligament Injuries: Traumatic force can lead to ligament injuries, including tearing of the ligaments surrounding the elbow joint. These ligaments, which hold bones in place, can be subjected to excessive stress, causing them to stretch, partially or completely tear.
- Displacement of Bones: Due to ligament damage, the bones of the elbow, including the ulna, radius and humerus, can be dislodged from their normal position. This leads to a dislocation where the joint surfaces are no longer aligned correctly.
- Nerve Compression: Elbow dislocation can compress nearby nerves, leading to symptoms such as numbness, tingling, or loss of sensation in the hand or fingers. Peripheral nerves, such as the ulnar nerve, may be particularly affected.
- Inflammatory Reaction: The trauma triggers a local inflammatory response. This leads to swelling, redness and increased pain around the elbow joint.
- Muscular Response: The muscles around the elbow joint may respond by reflexively contracting to protect the injured area. This can contribute to limited mobility and the appearance of muscle spasms.
- Additional Complications: In addition to dislocation, fractures of the forearm bones, damage to blood vessels, and injury to surrounding soft tissues can also occur, adding complications to the pathophysiology.
Differential diagnosis
The differential diagnosis of elbow dislocation involves the exclusion of other medical conditions that may present with similar symptoms. Here are some conditions that could be considered in the differential diagnosis:
- Elbow Fractures: Fractures of the bones of the forearm, such as the radius and ulna, can often be confused with an elbow dislocation, as they can also cause pain, swelling and limited mobility .
- Ligament Sprains: Sprains of the ligaments surrounding the elbow joint can cause symptoms similar to those of a dislocation. A radiographic evaluation can help distinguish between the two.
- Nerve Injury: Injuries to the peripheral nerves in the arm can sometimes cause loss of sensation or tingling, symptoms that can be confused with those of a dislocation.
- Elbow Bursitis: Inflammation of the synovial bursa located around the elbow joint can cause pain and swelling. Bursitis can present with symptoms similar to those of a dislocation.
- Elbow Arthritis: Inflammatory forms of arthritis, such as rheumatoid arthritis, can affect the elbow joint and cause pain, stiffness and swelling.
- Partial Dislocation: A partial dislocation, where the bones are not completely out of the joint, can be difficult to distinguish from a complete dislocation and may require extensive examinations.
- Muscle Bruising: Severe bruising of the muscles surrounding the elbow joint can also cause pain and swelling, mimicking the symptoms of a dislocation.
Diagnosis and treatment
Diagnosis of Elbow Dislocation:
Diagnosis of elbow dislocation is based on a thorough clinical evaluation, usually performed by a healthcare professional. Diagnostic steps may include:
- History: The doctor will collect information about the circumstances of the injury, the symptoms experienced, and the patient’s medical history.
- Physical Examination: The physical examination will allow the healthcare professional to assess the mobility of the elbow, look for signs of deformity, check sensitivity and detect possible skin lesions.
- Imaging: X-rays are usually taken to confirm the diagnosis and assess the severity of the dislocation. They allow the position of the bones to be visualized and any associated fractures to be detected.
Treatment of Elbow Dislocation:
Treatment of elbow dislocation aims to restore normal bone alignment, relieve pain, reduce inflammation, and promote functional recovery. Treatment approaches may include:
- Reduction: The first step is often to perform a reduction, where the healthcare professional uses maneuvers to return the bones to their normal position. This may sometimes require sedation or anesthesia.
- Immobilization: After reduction, the elbow may be immobilized using a splint or cast to allow healing. Immobilization can last several weeks.
- Medications: Pain relievers and anti-inflammatories may be prescribed to relieve pain and reduce inflammation.
- Rehabilitation: Once immobilization is lifted, rehabilitation is essential to restore strength, mobility and normal function of the elbow. Specific exercises may be prescribed.
- Surgery: In some cases, especially if there are complications such as severe fractures or soft tissue injuries, surgery may be necessary.
Radiographic signs
Radiographic signs of elbow dislocation can be clearly identified during a medical x-ray. The main features seen on x-ray images usually include:
- Displacement of Bones: X-ray may reveal abnormal displacement of the bones of the elbow joint from their normal position. This may include separation of the joint surfaces, indicating dislocation.
- Associated Fractures: Elbow dislocations can often be accompanied by fractures, particularly when the force of impact is significant. Fractures of the forearm bones, such as the radius and ulna, may also be visible on x-rays.
- Abnormal Alignment: X-rays may show abnormal alignment of the bones of the forearm in relation to the upper arm. Incorrect alignment is a clear sign of dislocation.
- Assessment of Joints: X-rays help assess the condition of joint surfaces, ligaments and surrounding structures. Signs of ligament damage, such as bone avulsions, may be detected.
- Vascular Assessment: In some severe cases of dislocation, vascular damage may occur. X-rays can help evaluate the integrity of the blood vessels around the elbow joint.
Conclusion
In conclusion, elbow dislocation is an injury that requires immediate attention and proper care. Evaluation by a healthcare professional, usually followed by manipulations to return the bones to their correct position, is often essential for optimal recovery. Rehabilitation and physical therapy can also play a crucial role in restoring elbow mobility and strength after a dislocation. It is imperative to follow medical advice, adhere to the recommended treatment plan, and take the time necessary to allow for complete recovery.
References
- Taylor F, Sims M, Theis JC, Herbison GP. Interventions for treating acute elbow dislocations in adults. Cochrane Database Syst Rev. 2012 Apr 18;2012(4):CD007908. [PMC free article] [PubMed]2.
- Stoneback JW, Owens BD, Sykes J, Athwal GS, Pointer L, Wolf JM. Incidence of elbow dislocations in the United States population. J Bone Joint Surg Am. 2012 Feb 01;94(3):240-5. [PubMed]3.
- Mathew PK, Athwal GS, King GJ. Terrible triad injury of the elbow: current concepts. J Am Acad Orthop Surg. 2009 Mar;17(3):137-51. [PubMed]4.
- Gottschalk HP, Eisner E, Hosalkar HS. Medial epicondyle fractures in the pediatric population. J Am Acad Orthop Surg. 2012 Apr;20(4):223-32. [PubMed]5.
- Card RK, Lowe JB. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 24, 2023. Anatomy, Shoulder and Upper Limb, Elbow Joint. [PubMed]6.
- Glover NM, Black AC, Murphy PB. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Nov 5, 2023. Anatomy, Shoulder and Upper Limb, Radial Nerve. [PubMed]7.
- Wheeler R, DeCastro A. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): May 1, 2023. Posterior Interosseous Nerve Syndrome. [PubMed]8.
- Murphy KA, Morrisonponce D. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Aug 20, 2023. Anatomy, Shoulder and Upper Limb, Median Nerve. [PubMed]9.
- Akhondi H, Varacallo M. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Aug 4, 2023. Anterior Interosseous Syndrome. [PubMed]10.
- Lleva JMC, Munakomi S, Chang KV. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Aug 13, 2023. Ulnar Neuropathy. [PubMed]11.
- Morrey BF. Acute and Chronic Instability of the Elbow. J Am Acad Orthop Surg. 1996 May;4(3):117-128. [PubMed]12.
- O’Driscoll SW. How Do Elbows Dislocate?: Commentary on an article by Marc Schnetzke, MD, et al.: « Determination of Elbow Laxity in a Sequential Soft-Tissue Injury Model. A Cadaveric Study ». J Bone Joint Surg Am. 2018 Apr 04;100(7):e46. [PubMed]13.
- Kuhn MA, Ross G. Acute elbow dislocations. Orthop Clin North Am. 2008 Apr;39(2):155-61, v. [PubMed]14.
- Saouti R, Albassir A, Berger JP, Fatemi F, Willems S. Anterior elbow dislocation with recurrent instability. Acta Orthop Belg. 2003 Apr;69(2):197-200. [PubMed]15.
- Cohen MS, Hastings H. Acute elbow dislocation: evaluation and management. J Am Acad Orthop Surg. 1998 Jan-Feb;6(1):15-23. [PubMed]16.
- Donohue KW, Mehlhoff TL. Chronic Elbow Dislocation: Evaluation and Management. J Am Acad Orthop Surg. 2016 Jul;24(7):413-23. [PubMed]17.
- Martin BD, Johansen JA, Edwards SG. Complications related to simple dislocations of the elbow. Hand Clin. 2008 Feb;24(1):9-25. [PubMed]18.
- Paydar-Darian N, Goldman MP, Michelson KA, Button KC, Hewett EK, Macnow TE, Miller AF, Musisca MA, Hudgins JD, Eisenberg MA. Improving Efficiency and Communication around Sedated Fracture Reductions in a Pediatric Emergency Department. Pediatr Qual Saf. 2019 Jan-Feb;4(1):e135. [PMC free article] [PubMed]




















