Introduction
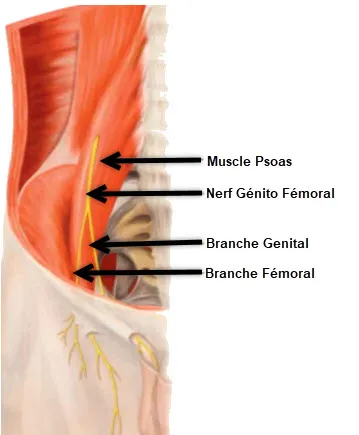
Genitofemoral neuralgia is a medical condition characterized by pain along the path of the genitofemoral nerve. This nerve, originating from the L1 and L2 nerve roots of the spinal cord, innervating the genital region and the anterior surface of the thigh, can be subject to irritation or compression, thus leading to the manifestation of painful symptoms.
Symptoms of genitofemoral neuralgia are often described as sharp pain, burning, tingling, or electric shock sensations along the path of the nerve. The pain may radiate from the genital area to the front of the thigh, causing significant discomfort for affected individuals.
The causes of genitofemoral neuralgia can be varied. Nerve compression can result from anatomical disorders such as inguinal hernias, trauma, or even surgical procedures in the pelvic region. Inflammatory or infectious conditions can also contribute to the development of this neuralgia.
The impact of genito-femoral neuralgia on patients’ quality of life is often underestimated. Severe pain can interfere with daily activities, personal relationships, and even sleep. Due to the specific location of the genitofemoral nerve, the condition can also cause particular emotional and psychological challenges.
The diagnosis of genito-femoral neuralgia is based on clinical assessment of symptoms, possibly supplemented by medical imaging examinations such as MRIs or CT scans to identify the source of the nerve irritation. It is crucial to rule out other possible causes of pain in the pelvic area before confirming the diagnosis.
Management of genitofemoral neuralgia may involve a multidisciplinary approach. Treatment options may include analgesic medications to relieve pain, osteopathic interventions to improve mobility and reduce nerve compression, and more invasive approaches such as nerve blocks or electrical stimulation.
It is essential to take a holistic approach to managing genitofemoral neuralgia. Pain management, physical rehabilitation, and psychological support can play a crucial role in improving the quality of life of those affected. Regular follow-up with healthcare professionals allows the treatment plan to be adjusted based on the patient’s individual response.
So, genito-femoral neuralgia is a condition that can have a significant impact on the daily lives of people who suffer from it. Understanding the symptoms, possible causes and available treatment options is essential to providing effective support to individuals affected by this neuralgia. An integrated approach, involving different medical disciplines, can help alleviate pain and improve patients’ overall quality of life.
Symptoms
Symptoms of genitofemoral neuralgia can vary from person to person, but they are usually related to irritation or compression of the genitofemoral nerve. Common manifestations of this condition include:
- Pain along the nerve: Pain is the main symptom of genitofemoral neuralgia. It can manifest as sharp pain, burning, tingling, or sensations of electric shock along the path of the genitofemoral nerve.
- Radiation to the genital area and thigh: The pain may radiate from the genital area to the front of the thigh. This creates an extended area of tenderness along the affected nerve.
- Discomfort in the pelvic region: Patients may experience discomfort in the pelvic region, and this sensation may be exacerbated by certain body movements or positions.
- Increased sensitivity: Increased sensitivity may be present along the course of the genitofemoral nerve. Tight clothing or physical contact can make the pain worse.
- Impaired quality of life: Due to the specific location of the genitofemoral nerve, neuralgia can impact daily life, including physical activities, intimate relationships, and even sleep.
- Numbness: Some individuals with genitofemoral neuralgia may experience sensations of numbness along the path of the nerve, in addition to pain and tingling sensations.
- Muscle weakness: Prolonged compression of the genitofemoral nerve can lead to muscle weakness in the thigh or pelvic region.
- Sensitivity disorders: Alterations in sensitivity, such as decreased tactile sensation or changes in temperature perception, may also be observed.
- Autonomic reactions: Some patients may experience autonomic reactions, such as changes in sweating or changes in skin color in the affected area.
- Worsened by certain movements: Symptoms of genitofemoral neuralgia may worsen with certain specific body movements, physical activities, or even prolonged sitting.
- Impact on sexual quality of life: Due to the innervation of the genital region by the genitofemoral nerve, this condition can also influence the sexual quality of life of affected individuals.
Genitofemoral neuralgia, although it can affect both sexes, can present with different manifestations in men and women. Symptoms reported by men who suffer from this condition frequently include localized pain in the groin and testicles, creating a deep and often persistent aching sensation.
For men, the location of pain in the groin area can be particularly debilitating, affecting not only their daily physical comfort, but also their daily activities and general well-being. The pain may manifest as burning sensations, tingling sensations, or even a dull, constant ache.
On the other hand, in women with genitofemoral neuralgia, symptoms are often reported in specific areas of the genital tract. The pain is most commonly felt in the clitoris and labia majora. This specific location of pain can cause additional difficulties, particularly regarding sexuality and general physical comfort.
When genitofemoral neuralgia affects the clitoris and labia majora in women, it can directly influence the sensory response during sexual activities, thus leading to complications in the intimate sphere. Pain can also interfere with women’s emotional and psychological well-being, adding a complex dimension to the management of this condition.
These differences in symptom localization between men and women highlight the complexity of genitofemoral neuralgia and the importance of an individualized approach in the diagnosis and management of this condition. Healthcare professionals must take these variations into account to provide personalized treatment, tailored to the specific physiology of each patient.
In addition to differences in the location of symptoms, the severity of genitofemoral neuralgia can also vary greatly from person to person. Some individuals may experience intermittent, manageable pain, while others may experience persistent, disabling pain requiring more intensive medical management.
Recognition of these gender differences in manifestation highlights the importance of open communication between patients and healthcare professionals. This allows not only an accurate assessment of symptoms, but also treatment planning tailored to the individual needs of each person affected by genitofemoral neuralgia.
Causes
The causes of genitofemoral neuralgia are usually related to irritation or compression of the genitofemoral nerve. Several factors can contribute to the development of this condition, including:
- Inguinal hernias: An inguinal hernia, which occurs when some of the abdominal contents pass through a weak point in the muscular wall of the groin, can put pressure on the genitofemoral nerve, causing irritation.
- Trauma: Direct trauma, such as injuries or accidents, can damage the genitofemoral nerve and lead to inflammation or compression.
- Pelvic Surgery: Surgical procedures in the pelvic region, especially those involving the inguinal canal, can result in irritation of the genitofemoral nerve.
- Infections: Infections, such as post-surgical infections or pelvic infections, can contribute to inflammation of the genitofemoral nerve.
- Muscle Compression: Certain muscles in the pelvic region can put excessive pressure on the genitofemoral nerve due to muscle spasms or excessive tension.
- Anatomical abnormalities: Congenital or acquired anatomical abnormalities, such as variations in nerve path or spinal abnormalities, may increase the risk of genitofemoral neuralgia.
- Tumors: Although rarer, the presence of tumors in the pelvic region can put pressure on the genitofemoral nerve, causing symptoms.
- Compression during pregnancy: In pregnant women, the growing uterus can sometimes put pressure on the genitofemoral nerve, causing temporary symptoms.
Pathophysiology
The pathophysiology of genitofemoral neuralgia primarily involves irritation or compression of the genitofemoral nerve, a mixed nerve arising from the L1 and L2 nerve roots of the spinal cord. This nerve innervates the genital region and the anterior surface of the thigh. When subjected to excessive pressure, inflammation or trauma, it can result in characteristic painful symptoms.
Here are the general stages of the pathophysiology of genito-femoral neuralgia:
- Nerve irritation or compression: Genitofemoral neuralgia often results from irritation or compression of the genitofemoral nerve. This compression can be caused by several factors, such as inguinal hernias, trauma, surgeries, infections, or other medical conditions.
- Local inflammation: Irritation of the genitofemoral nerve can trigger a local inflammatory reaction. Inflammation contributes to the release of pro-inflammatory chemicals, which makes painful symptoms worse.
- Impaired nerve conduction: Irritation of the nerve can impair normal nerve conduction. This can cause the nerve to become more sensitive, causing abnormal sensations such as pain, tingling, and numbness.
- Central Nervous System Response: Pain signals from the genitofemoral nerve can be interpreted and amplified by the central nervous system. This contributes to the perception of pain and can lead to an amplified response to normal stimuli.
- Adaptive Responses: In response to pain, the body may develop adaptive responses, such as changes in posture or changes in gait pattern. These adjustments can, in turn, lead to musculoskeletal imbalances and worsen symptoms.
It is important to note that genitofemoral neuralgia can have variable manifestations from person to person depending on the underlying cause, the