Introduction
Heel fat pad syndrome, also called heel atrophy syndrome, is characterized by thinning of the fat pad and muscle fibers that support and cushion the heel. This condition, although uncommon, can be particularly painful and impact the quality of life of individuals who suffer from it.
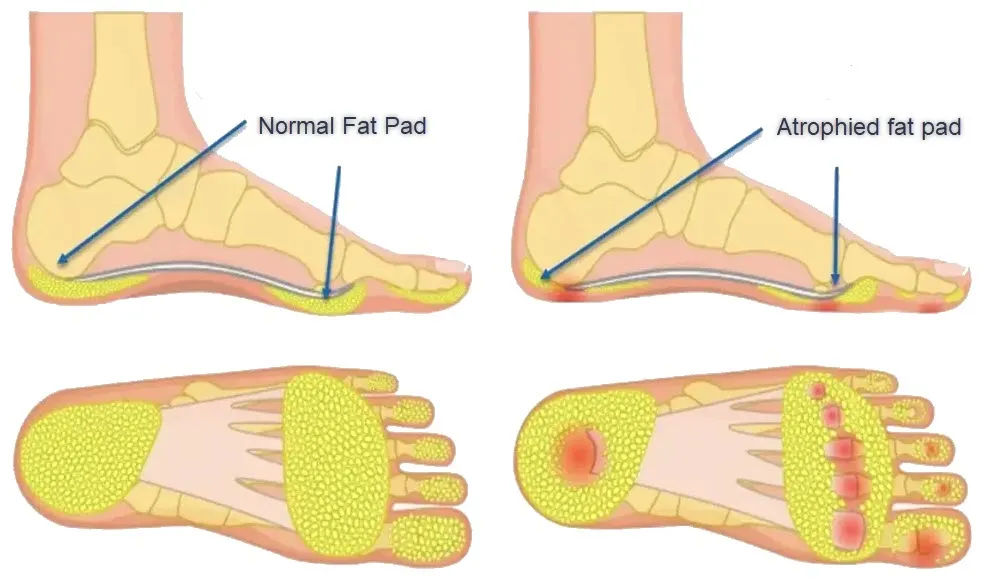
The heel fat pad, made up of adipose tissue and vascular structures, occupies a crucial place under the Achilles tendon at the heel. Its main function is to cushion the forces exerted on the heel during walking and physical activities. When this pad experiences thinning, it loses its ability to properly absorb shock, leading to increased pressure on the heel and surrounding structures.
Several factors can contribute to the development of heel fat pad syndrome. High-impact activities, such as running or other intensive sports, as well as prolonged standing and frequent walking, are common causes. Additionally, wearing the wrong shoes or not wearing the right shoes can make the situation worse. These factors induce excessive stress on the fat pad, leading to its progressive thinning.
Symptoms of SCAT typically include persistent pain in the heel, increased sensitivity when putting pressure on the affected area, and sometimes even local inflammation. The pain may be more pronounced when walking or engaging in physical activities, limiting mobility and engagement in daily activities.
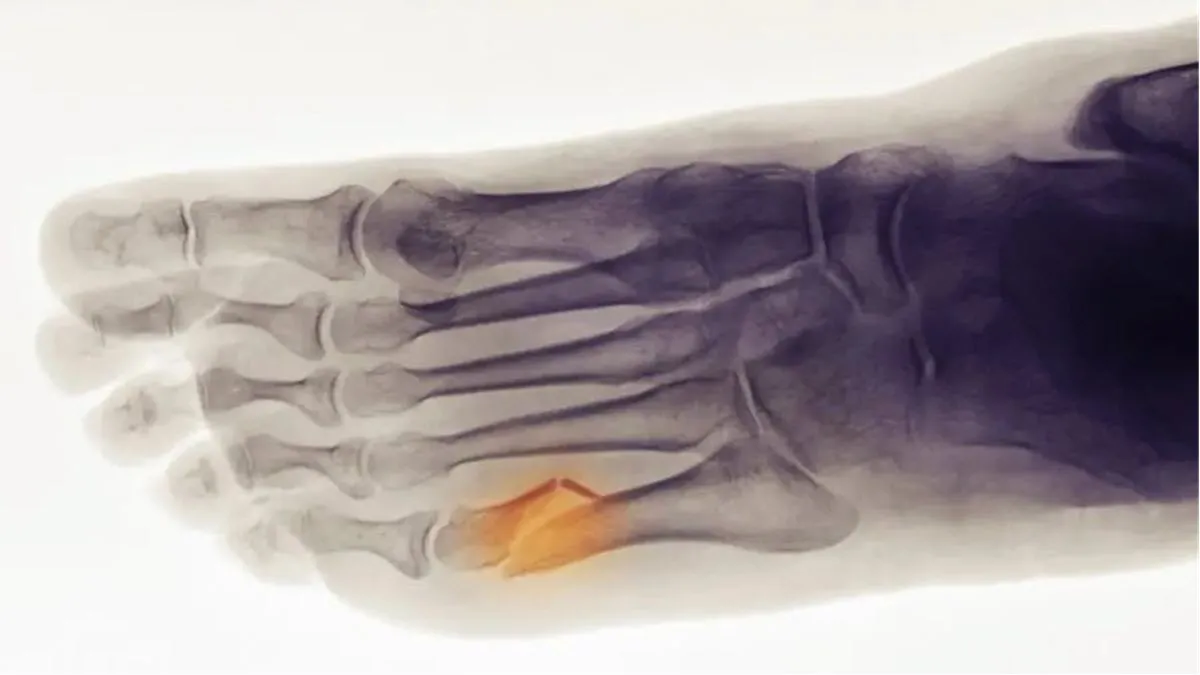
Diagnosis of heel fat pad syndrome is usually based on clinical examination, analysis of the patient’s medical history, and medical imaging tests such as ultrasound or MRI. Once the diagnosis is confirmed, treatment may include conservative approaches such as rest, modification of activities, use of appropriate footwear, and application of ice to reduce inflammation.
In certain cases that are more serious or resistant to conservative treatments, medical interventions may be considered. These may include corticosteroid injections to reduce inflammation, physical therapies to strengthen the surrounding muscles, or even surgery in the most extreme cases.
In conclusion, heel fat pad syndrome is a painful condition that can affect individuals’ quality of life by limiting their mobility and participation in physical activities. Early and appropriate management, based on a thorough understanding of the causes and symptoms, is essential to alleviate symptoms and promote effective recovery.
Anatomy of the Heel Fat Pad
- Adipose Tissue: The fat pad is primarily composed of adipose tissue, also called subcutaneous adipose tissue. This tissue is made up of fat cells (adipocytes) which store energy in the form of fat. The presence of this layer of fat provides a cushioning and protective function.
- Fascia: Fascia is fibrous connective tissue that surrounds and supports anatomical structures. At the heel fat pad, the plantar fascia associates with this region, contributing to stability and structural integrity.
- Blood Vessels: The fat pad is vascularized, which means that it is irrigated by blood vessels. Vascularization is crucial for tissue nutrition and cell regeneration. Blood vessels also contribute to the inflammatory response when injured.
- Fibrous Capsule: A fibrous capsule surrounds the fat pad, providing structural support. This capsule helps maintain the integrity of the region and protect the adipose tissue and surrounding structures.
Function of the Heel Fat Pad
The main function of the heel fat pad is to act as a natural shock absorber. It is composed of adipose tissue, which gives it shock absorption capacity. When walking, running, or other physical activities, the heel is subjected to significant forces with each impact on the ground. The fat pad absorbs these forces, relieving pressure on the bones, joints and soft tissues of the heel. This cushioning feature is essential for preventing injuries and ensuring comfortable walking.
In addition to its role as a shock absorber, the fat pad also contributes to the stability of the foot. It acts as structural support by maintaining the integrity of the arch and evenly distributing the load on the heel. This even distribution of forces is crucial to avoid excessive stress on certain parts of the foot, which could lead to biomechanical imbalances and musculoskeletal problems.
Furthermore, the heel fat pad plays a role in lubricating surrounding structures. Foot movements involve continuous sliding of tissues relative to each other. The fat pad, in addition to its cushioning properties, facilitates these movements by reducing friction between tendons, muscles and other surrounding tissues. This lubricating function contributes to the flexibility and mobility of the foot.
However, despite its robustness, the heel fat pad is not immune to various conditions. Conditions such as fat pad atrophy, where the amount of fatty tissue decreases, can compromise its cushioning and supporting functions, leading to heel pain and posture problems.
- Cushioning and Protection: The fat pad acts as a natural buffer, absorbing shock and reducing pressure on the heel. This helps cushion the forces generated during walking, running and other physical activities, providing protection to surrounding structures.
- Load Distribution: The fat pad contributes to the even distribution of loads on the heel, helping to prevent excessive pressure points. This balanced distribution is essential to maintain tissue integrity and avoid the development of lesions.
- Structural Support: In addition to its shock-absorbing role, the fat pad provides structural support to the heel. It contributes to the stability of the rearfoot and helps maintain the normal curvature of the plantar arch.
- Metabolic Role: Adipose tissue present in the footpad may also have metabolic implications. Adipose cells store energy in the form of fat, which can be mobilized in times of increased energy needs.
- Response to Mechanical Stress: The physiopathology of the fat pad also involves adaptation to mechanical stress. Changes in pressure or load can influence the size and density of adipose tissue to meet functional needs.
Causes of Heel Fat Pad Syndrome
One primary intrinsic factor contributing to this syndrome is the natural aging process. As individuals age, the plantar fat pad undergoes structural changes, losing its elasticity and thickness. This age-related degeneration is compounded by a reduction in vascularity and cellularity within the adipose tissue of the heel pad, diminishing its shock-absorbing capabilities. Systemic conditions, such as diabetes and rheumatoid arthritis, constitute additional intrinsic factors. These conditions not only accelerate the degenerative process but also compromise the overall health and integrity of the fat pad.
Extrinsic factors play a pivotal role in the development of heel fat pad syndrome, with mechanical stress being a primary culprit. Prolonged weight-bearing activities, especially on hard surfaces, subject the heel pad to repetitive microtrauma and compression, leading to collagen fiber breakdown within the fat pad. Inappropriate footwear choices exacerbate the impact, as shoes with inadequate cushioning or improper arch support contribute to accelerated degeneration. High-impact activities and occupations involving extended periods of standing or walking on hard surfaces further intensify the wear and tear on the plantar fat pad.
Biomechanical abnormalities and foot structure can also contribute to the development of heel fat pad syndrome. Conditions such as pes planus (flat feet) or pes cavus (high arches) alter the distribution of forces within the foot, placing additional stress on the heel pad. This altered biomechanics can accelerate the degeneration of the fat pad over time.
Moreover, obesity serves as a significant extrinsic factor, as excessive body weight places increased pressure on the heel during weight-bearing activities, accelerating the breakdown of the plantar fat pad. Inflammation is another key contributor, as chronic stress and microtrauma trigger an inflammatory response within the heel pad, exacerbating pain and swelling.
- Trauma and Injuries: Direct trauma to the heel, such as impact or blunt injuries, can damage the fat pad beneath the Achilles tendon, contributing to SCAT.
- Excessive Pressure on the Heel: Continuous or excessive pressure on the heel, often due to activities that frequently use this area, such as running or prolonged walking, can lead to irritation of the fat pad.
- Biomechanical Changes of the Foot: Changes in the biomechanics of the foot, such as excessive pronation or supination, can influence the distribution of forces on the heel. This can lead to compression and irritation of the fat pad.
- Ankle Instability: Ankle instability, often associated with recurrent sprains, can affect the way the foot absorbs shock while walking, increasing the risk of problems with the fat pad.
- Circulatory Problems: Circulatory problems in the foot can influence the health of tissues, including the fat pad. Impaired blood circulation can contribute to inflammation and tenderness in this area.
- Inappropriate Footwear: Wearing inappropriate shoes that do not provide adequate support or place excessive pressure on the heel can contribute to the development of SCAT.
- Obesity: Excess weight can increase the load on the heel during walking, creating increased pressure on the fat pad.
- Genetic Factors: Some people may have a genetic predisposition to develop problems with the fat pad of the heel.
Symptoms of Heel Fat Pad Syndrome
- Heel Pain: Heel pain is one of the most common symptoms of SCAT. The pain may be located under the heel, often on the back of the foot.
- Sensitivity to Touch: The affected area may become sensitive to touch. Light pressure or even the friction of shoes can trigger discomfort.
- Localized Swelling: Inflammation of the fat pad can lead to localized swelling around the heel. It can be visible and palpable.
- Redness: If there is significant inflammation, the skin around the heel may turn red.
- Increased Pain During Activity: Pain may intensify during or after activities that put strain on the heel, such as walking, running, or wearing inappropriate shoes.
- Pain at Rest: In some cases, pain may persist even at rest, especially after periods of intense activity.
- Morning Stiffness: Some individuals may experience stiffness or discomfort in the heel in the morning upon waking. This stiffness may ease after a few steps.
- Difficulty Walking: Due to pain and discomfort, some people may have difficulty walking normally.
- Possible Difficulty Going Up or Down Stairs: Bending and extending movements of the foot, such as going up or down stairs, can be painful.
- Gait Modification: To avoid pain, people may modify their gait, which can lead to biomechanical changes and additional complications.
Pathophysiology of heel fat pad syndrome
Heel fat pad syndrome, also known as plantar fat pad atrophy or heel pad syndrome, involves the degeneration and thinning of the natural cushioning tissue beneath the heel. This critical structure, known as the plantar fat pad, serves as a shock absorber during weight-bearing activities and provides essential support to the foot. The pathophysiology of heel fat pad syndrome is multifaceted, often originating from a combination of intrinsic and extrinsic factors.
Intrinsic factors contributing to this syndrome include the natural aging process, where the plantar fat pad undergoes structural changes, losing its elasticity and thickness. As individuals age, the adipose tissue within the heel pad experiences a reduction in vascularity and cellularity, leading to diminished shock-absorbing capabilities. Additionally, systemic conditions such as diabetes and rheumatoid arthritis can exacerbate heel fat pad degeneration, as these conditions may compromise the overall health and integrity of the fat pad.
Extrinsic factors play a pivotal role in the pathophysiology of heel fat pad syndrome, with prolonged mechanical stress being a primary culprit. Excessive weight-bearing activities, particularly on hard surfaces, contribute to repetitive microtrauma and compression of the heel pad. This constant pressure can lead to the breakdown of collagen fibers within the fat pad, diminishing its ability to absorb and distribute the forces generated during walking or standing.
Footwear choices also influence the development of heel fat pad syndrome. Wearing shoes with inadequate cushioning or improper arch support can exacerbate the impact on the heel pad, accelerating its degeneration. High-impact activities and occupations that involve prolonged standing or walking on hard surfaces further contribute to the wear and tear of the plantar fat pad.
Inflammation is another aspect of the pathophysiology, as chronic stress and microtrauma can trigger an inflammatory response within the heel pad. Inflammatory mediators contribute to pain and swelling, amplifying the discomfort experienced by individuals with heel fat pad syndrome.
Heel fat pad syndrome, also known as heel fat pad syndrome, is a medical condition characterized by symptoms such as heel pain, increased sensitivity, inflammation, and possible loss of normal pad function. fatty tissue located at the back of the heel. Although this condition can have various causes, the general pathophysiology can be explored as follows:
- Inflammation: Heel fat pad syndrome may be associated with inflammation of the fatty tissue. Inflammatory factors can be triggered by injuries, repeated mechanical stress, infections or other stimuli.
- Degradation of Adipose Tissue: Degenerative processes or alterations in the composition of the adipose tissue of the pad can occur. This may include the breakdown of fat cells or changes in the distribution of adipocytes, which affects the ability of the pad to perform its normal functions.
- Vascular Alterations: Vascular problems, such as alterations in blood flow to the fat pad, may contribute to the development of the syndrome. Impaired blood circulation can compromise tissue health, leading to painful symptoms.
- Excessive Mechanical Stress: Excessive mechanical stress due to intense physical activities, inappropriate shoe wearing or other factors may contribute to the occurrence of the syndrome. The fat pad can be subjected to excessive forces, leading to microtrauma and inflammatory responses.
- Metabolic Conditions: Metabolic disorders, such as changes in lipid metabolism, can influence fat pad health. Abnormal lipid accumulation or changes in fat composition may contribute to pad dysfunction.
- Immune Response: In some cases, the immune system may be involved, triggering abnormal immune responses that contribute to inflammation and associated symptoms.
It is important to note that the precise pathophysiology may vary from one individual to another, depending on factors specific to each case. The precise diagnosis and treatment plan are usually established after a thorough medical evaluation, possibly supported by medical imaging examinations and laboratory tests. Treatment may include measures to reduce inflammation, relieve pain, and treat the underlying cause of heel fat pad syndrome.
Prevention
- Choosing Appropriate Footwear:
- Opt for shoes with good heel support and adequate cushioning.
- Choose shoes that fit the shape of your feet properly, especially at the heel, to avoid excessive pressure on the fat pad.
- Bow Support:
- Use orthotic insoles or shoes with good arch support to evenly distribute pressure on the foot.
- Strengthening Exercises:
- Incorporate foot strengthening exercises into your routine, focusing on the calf and foot muscles.
- Regular stretching of the calf and leg muscles can also help maintain good foot mobility.
- Weight Control:
- Maintain a healthy body weight to reduce pressure on the feet, especially the heel fat pad.
- Morning Stretches:
- Practice gentle calf and foot stretches in the morning before putting your feet on the floor to help prevent stiffness.
- Gradual Shoe Changes:
- Avoid abruptly switching from one type of shoe to another. Gradual changes allow the foot to gradually adapt.
- Healthy Walking Habits:
- Adopt a regular walk with a natural gait.
- Avoid walking barefoot on hard surfaces to reduce stress on the fat pad.
Difference between heel fat pad syndrome and plantar fasciitis
Heel fat pad syndrome focuses on the fat pad, a structure located at the back of the heel, between the calcaneus and surrounding tissues. Its main role is to act as a natural shock absorber, absorbing shock during walking and running. Symptoms of this syndrome may include heel pain, fat pad inflammation, and posture problems. The causes are varied, from overuse to biomechanical abnormalities, and your expertise as an osteopath can help identify and treat these factors.
On the other hand, plantar fasciitis involves the inflammation of the plantar fascia, a thick band of connective tissue that connects the heel to the toes, supporting the arch of the foot. Common symptoms of plantar fasciitis include sharp pain in the heel, especially in the morning or after a period of inactivity. This condition is often associated with excessive tension on the plantar fascia, usually caused by prolonged activities, poor foot biomechanics, or wearing inappropriate shoes.
The fundamental difference therefore lies in the structures affected. Heel fat pad syndrome focuses on the fat pad at the back of the heel, while plantar fasciitis affects the plantar fascia under the arch of the foot. However, it is important to note that these conditions can sometimes coexist, as imbalances in one area of the foot can affect other structures.
Differential Diagnoses of Heel Fat Pad Syndrome
- Plantar Fasciitis: An inflammation of the plantar fascia, the thick band of tissue that connects the heel to the toes. The pain is usually felt under the heel.
- Heel Spur: An abnormal bone growth on the calcaneus (heel bone) that can cause heel pain.
- Achilles tendonitis: An inflammation of the Achilles tendon, which can cause heel pain and difficulty walking.
- Rheumatoid Arthritis: An autoimmune disease that can affect joints, including those in the foot, causing pain and inflammation.
- Osteoarthritis of the Foot: The breakdown of articular cartilage can cause heel pain and stiffness.
- Morton’s neuroma: Thickening of the tissue around the nerves in the front of the foot, causing pain and numbness.
- Posterior Compartment Syndrome: A condition where the muscles, blood vessels and nerves in the posterior compartment of the leg are compressed, leading to heel and calf pain.
- Heel Bursitis: Inflammation of the bursa, a fluid-filled sac between the tendons and bones, which can cause heel pain.
- Tarsal Neuralgia: Compression of the posterior tibial nerve, causing pain in the heel and ball of the foot.
- Bone Injuries: Fractures, cracks or other bone injuries that can cause heel pain.
Osteopathic Approach in the Management of SCAT
- Osteopathic Assessment : Osteopathy offers a holistic approach in the management of SCAT. During an initial assessment, the osteopathic practitioner carefully examines the biomechanics of the foot, posture, and evaluates heel and foot movements. Gentle manual techniques are often used to determine movement restrictions and structural imbalances.
- Biomechanical Rebalancing : Osteopathic treatment aims to restore the biomechanical balance of the foot by working on the joints, muscles, ligaments and fascia. Specific techniques can be applied to release tension in the heel area and restore joint mobility.
- Pain and Inflammation Management : Osteopathic techniques can also help alleviate the pain and inflammation associated with SCAT. The osteopath may use methods such as manual therapy, joint mobilization, and advice on self-management of pain.
- Integration with Other Approaches : In addition to osteopathic treatment, a comprehensive approach may involve collaboration with other healthcare professionals, such as physiotherapists, podiatrists and exercise specialists. Personalized recommendations can be provided for specific strengthening exercises and shoe changes.
Home Exercises
The following exercises can be performed at home to strengthen the heel region, improve foot stability, and promote healing from heel adipose syndrome. Before you begin, be sure to consult your healthcare professional to ensure these exercises are appropriate for your specific condition.
- Calf Stretch:
- Standing facing a wall, place your hands against it.
- Take a large step back with the affected leg while slightly bending the front knee.
- Keep the heel of the back leg on the floor and stretch the calf by pushing the hips forward.
- Hold the position for 20 to 30 seconds and repeat several times.
- Lateral Leg Raises:
- Lie on your side with the affected leg up.
- Lift the leg straight up, keeping the foot aligned with the rest of the leg.
- Hold the position at the top for a few seconds, then slowly lower back down.
- Perform 2 to 3 sets of 15 repetitions.
- Toe Puppet:
- Sitting in a chair, place a towel under the arch of your foot.
- Use your toes to pull the towel toward you while keeping your heel on the floor.
- Hold the contraction for a few seconds, then release.
- Repeat this movement for 2 to 3 minutes.
- Ball Roll Underfoot:
- Sit in a chair with your feet flat on the floor.
- Place a tennis ball under the arch of the affected leg.
- Gently roll the ball under your foot, focusing on tense areas.
- Do this for 5 minutes every day.
- Achilles Stretch on Steps:
- Stand on the edge of a stair step with your heels sticking out slightly.
- Let the heels gently drop below step level to stretch the calf and Achilles muscles.
- Hold the position for 20 to 30 seconds and repeat several times.
- Writing the Alphabet with the Feet:
- Sit or lie down and draw the alphabet in the air with the affected foot.
- Do this slowly and precisely to engage different muscles in the foot.
- Repeat the process twice in each direction.
These exercises aim to strengthen muscles, improve flexibility and support healing from heel adipose syndrome. It is important to perform them regularly, but gently, avoiding excessive pain. If pain persists or worsens, consult your healthcare professional.
Conclusion
In conclusion, heel fat pad syndrome, or Hoffa syndrome, represents a relatively rare but significant condition, resulting in the thinning of the fat pad and muscle fibers that play a crucial role in cushioning the heel. Factors such as high-impact activities, prolonged standing, wearing inappropriate shoes, and even no shoes can contribute to the development of this painful condition.
Symptoms, including persistent heel pain and increased sensitivity, can have a noticeable impact on quality of life, limiting mobility and participation in daily activities. The diagnosis, based on clinical examination and medical imaging investigations, helps guide treatment.
Management of heel fat pad syndrome often relies on conservative approaches such as rest, activity modification, use of appropriate footwear, and anti-inflammatory treatments. However, in more severe cases, medical interventions, including corticosteroid injections or surgical procedures, may be considered.
It is crucial to emphasize the importance of early intervention to alleviate symptoms and prevent possible complications. Patients should consult a healthcare professional as soon as symptoms appear to receive an accurate diagnosis and appropriate treatment plan.
In summary, a thorough understanding of this condition and a well-tailored therapeutic approach are essential to help affected individuals regain optimal quality of life by restoring heel fat pad function and reducing associated pain.
References
- Borja MJ, Jose J, Vecchione D, Clifford PD, Lesniak BP. Prefemoral fat pad impingement syndrome: identification and diagnosis. Am J Orthop (Belle Mead NJ). 2013 Jan;42(1):E9-11. [PubMed]2.
- Biedert RM, Sanchis-Alfonso V. Sources of anterior knee pain. Clin Sports Med. 2002 Jul;21(3):335-47, vii. [PubMed]3.
- Radu A, Discepola F, Volesky M, Munk PL, Le H. Posterior Hoffa’s fat pad impingement secondary to a thickened infrapatellar plica: a case report and review of the literature. J Radiol Case Rep. 2015 Mar;9(3):20-6. [PMC free article] [PubMed]4.
- Eymard F, Chevalier X. Inflammation of the infrapatellar fat pad. Joint Bone Spine. 2016 Jul;83(4):389-93. [PubMed]5.
- Kennedy JC, Alexander IJ, Hayes KC. Nerve supply of the human knee and its functional importance. Am J Sports Med. 1982 Nov-Dec;10(6):329-35. [PubMed]6.
- Brooker B, Morris H, Brukner P, Mazen F, Bunn J. The macroscopic arthroscopic anatomy of the infrapatellar fat pad. Arthroscopy. 2009 Aug;25(8):839-45. [PubMed]7.
- Gallagher J, Tierney P, Murray P, O’Brien M. The infrapatellar fat pad: anatomy and clinical correlations. Knee Surg Sports Traumatol Arthrosc. 2005 May;13(4):268-72. [PubMed]8.
- Grando H, Chang EY, Chen KC, Chung CB. MR imaging of extrasynovial inflammation and impingement about the knee. Magn Reson Imaging Clin N Am. 2014 Nov;22(4):725-41. [PubMed]9.
- Pharis H, Kong A, Robbins M, Waranch C, Wissman R. Friction Syndromes of the Knee. J Knee Surg. 2022 Apr;35(5):491-497. [PubMed]10.
- Bohnsack M, Meier F, Walter GF, Hurschler C, Schmolke S, Wirth CJ, Rühmann O. Distribution of substance-P nerves inside the infrapatellar fat pad and the adjacent synovial tissue: a neurohistological approach to anterior knee pain syndrome. Arch Orthop Trauma Surg. 2005 Nov;125(9):592-7. [PubMed]11.
- Kim SJ, Kim JY, Lee JW. Pathologic infrapatellar plica. Arthroscopy. 2002 May-Jun;18(5):E25. [PubMed]12.
- Ushiyama T, Chano T, Inoue K, Matsusue Y. Cytokine production in the infrapatellar fat pad: another source of cytokines in knee synovial fluids. Ann Rheum Dis. 2003 Feb;62(2):108-12. [PMC free article] [PubMed]13.
- Rooney A, Wahba AJ, Smith TO, Donell ST. The surgical treatment of anterior knee pain due to infrapatellar fat pad pathology: A systematic review. Orthop Traumatol Surg Res. 2015 Jun;101(4):469-75. [PubMed]14.
- Ogilvie-Harris DJ, Giddens J. Hoffa’s disease: arthroscopic resection of the infrapatellar fat pad. Arthroscopy. 1994 Apr;10(2):184-7. [PubMed]15.
- Steadman JR, Dragoo JL, Hines SL, Briggs KK. Arthroscopic release for symptomatic scarring of the anterior interval of the knee. Am J Sports Med. 2008 Sep;36(9):1763-9. [PubMed]16.
- Paulos LE, Wnorowski DC, Greenwald AE. Infrapatellar contracture syndrome. Diagnosis, treatment, and long-term followup. Am J Sports Med. 1994 Jul-Aug;22(4):440-9. [PubMed]17.
- Krebs VE, Parker RD. Arthroscopic resection of an extrasynovial ossifying chondroma of the infrapatellar fat pad: end-stage Hoffa’s disease? Arthroscopy. 1994 Jun;10(3):301-4. [PubMed]18.
- Hardy P, Muller GP, Got C, Lortat-Jacob A, Benoit J. Glomus tumor of the fat pad. Arthroscopy. 1998 Apr;14(3):325-8. [PubMed]19.
- Draghi F, Ferrozzi G, Urciuoli L, Bortolotto C, Bianchi S. Hoffa’s fat pad abnormalities, knee pain and magnetic resonance imaging in daily practice. Insights Imaging. 2016 Jun;7(3):373-83. [PMC free article] [PubMed]20.
- Vahlensieck M, Linneborn G, Schild H, Schmidt HM. Hoffa’s recess: incidence, morphology and differential diagnosis of the globular-shaped cleft in the infrapatellar fat pad of the knee on MRI and cadaver dissections. Eur Radiol. 2002 Jan;12(1):90-3. [PubMed]21.
- Ioan-Facsinay A, Kloppenburg M. An emerging player in knee osteoarthritis: the infrapatellar fat pad. Arthritis Res Ther. 2013;15(6):225. [PMC free article] [PubMed]