Introduction
Pandemics, global epidemics, and plagues have left an indelible mark on human history, documented through historical records and personal writings since ancient times. These health tragedies, occurring at a rate of about three to four per century, have repeatedly devastated populations worldwide. Survivors have immortalized these deadly diseases by giving them names reflecting the most prominent symptoms, the place of their origin, or the reigning sovereign at the time.
Throughout history, notorious pandemics have made their mark, including the Black Death in the 14th century, the Spanish flu of 1918, and the HIV/AIDS pandemic that emerged in the last decades of the 20th century. Each of these crises caused socio-economic disruptions and left deep scars in collective memory.
The written testimonies of survivors, often poignant, narrate the horror and devastation left by these plagues. Diaries, letters, and narratives passed down from generation to generation are valuable sources for understanding the psychological and emotional impact of these events on individuals and communities.
History also reveals that these health crises have often been catalysts for social and medical changes. Significant advances in understanding diseases, hygiene practices, and healthcare systems have emerged in the wake of these painful episodes. The lessons learned from these pandemics have contributed to shaping public health policies and have raised awareness about the importance of prevention and preparedness in the face of global health threats.
The Thread of Time
Over the past 2,500 years, various names have been given to pandemics, such as the Peloponnesian War disease, the Antonine Plague, the Justinian Plague, the Black Death, the Red Death, cholera, and the Asian flu. The grim reality is that almost every generation has had the opportunity to add a new name to a growing list of deadly diseases. The early 20th century is no exception, and members of the young osteopathic profession faced their first direct encounter with a pandemic: a deadly influenza.
These historical pandemics, each with its distinctive name, reflect the enduring challenges humanity has faced in battling infectious diseases. From ancient times to the present, the cycle of pandemics has woven a tapestry of hardship, resilience, and scientific advancement. The osteopathic community, too, has navigated through these turbulent times, witnessing the impact of pandemics on public health and healthcare practices.
The smallpox pandemic
The smallpox pandemic, a devastating chapter in human history, unfolded over centuries, leaving a profound impact on societies around the globe. Caused by the variola virus, smallpox manifested as a highly contagious and often lethal disease, shaping the course of nations and influencing medical advancements. The first recorded instances of smallpox date back to ancient civilizations, with outbreaks occurring in Asia, Africa, and Europe. As trade and exploration expanded, so did the reach of this formidable disease, turning it into a global menace.
The true extent of the smallpox pandemic became evident during the Age of Exploration, when European colonizers inadvertently introduced the virus to previously unexposed populations in the Americas, leading to catastrophic consequences. Indigenous communities, lacking immunity to this new threat, faced unprecedented mortality rates, decimating their populations and altering the course of history.

Efforts to combat smallpox gained momentum in the 18th and 19th centuries with the introduction of variolation, a primitive form of vaccination involving the inoculation of individuals with small amounts of live virus to induce immunity. This method, though risky, marked a significant leap forward in the fight against the disease. However, it was the groundbreaking work of Edward Jenner in the late 18th century that laid the foundation for modern vaccination. Jenner’s discovery that cowpox exposure provided immunity to smallpox laid the groundwork for the development of the smallpox vaccine, a pivotal moment in medical history.
The eradication of smallpox stands as one of humanity’s greatest achievements, showcasing the power of international collaboration and the effectiveness of vaccination programs. In 1980, the World Health Assembly officially declared smallpox eradicated, making it the first and, so far, the only human disease to be eradicated globally. This monumental success not only spared countless lives but also paved the way for subsequent efforts to combat infectious diseases through vaccination.
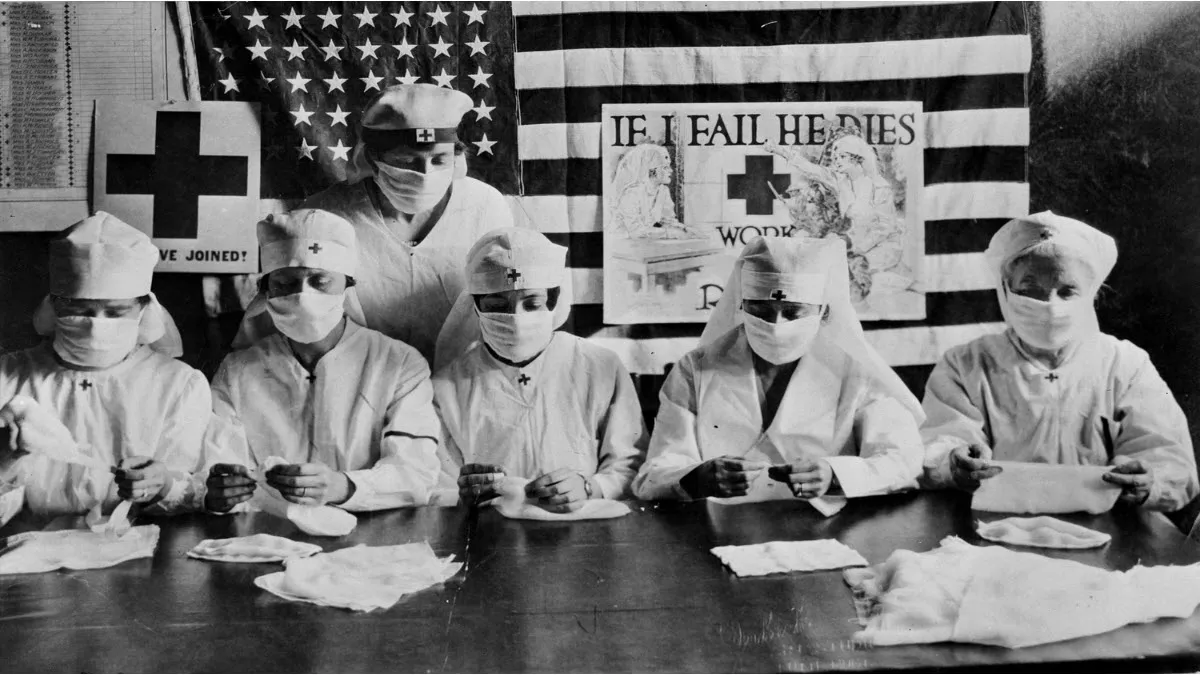
Montreal’s Crucible: The Anti-Vaccination Uprising of 1885 After Smallpox’s Devastation
In the aftermath of a devastating smallpox epidemic in 1885, Montreal found itself grappling not only with the lingering effects of the deadly disease but also with a rising tide of anti-vaccination sentiment. The French-Canadian adversaries of vaccination, fueled by a combination of fear, misinformation, and distrust in medical interventions, launched a riot that targeted City Hall in Montreal, marking a tumultuous chapter in the city’s history.
The smallpox epidemic that preceded the anti-vaccination riot had left a profound impact on Montreal, with the disease claiming numerous lives and instilling widespread fear within the community. As public health authorities sought to implement vaccination campaigns to curb the spread of smallpox, a vocal faction of French-Canadian residents resisted, viewing vaccination with suspicion and skepticism.
Amidst this backdrop, tensions escalated, culminating in a violent clash outside City Hall. The anti-vaccination riot, fueled by a deep-seated distrust of medical authorities and fueled by rumors of adverse effects associated with vaccination, saw a fervent mob descending upon the seat of municipal governance. The rioters, predominantly French-Canadian, expressed their opposition to vaccination mandates and perceived government intrusion into personal health decisions.
The attack on City Hall unfolded as a chaotic and tumultuous event, with protestors wielding signs and banners denouncing vaccination. The atmosphere was charged with emotion as the crowd vented its frustration and anger at perceived infringements on personal liberties. The riot underscored the challenges faced by public health officials in convincing a skeptical population of the benefits of vaccination, even in the face of a recent and devastating epidemic.
In the aftermath of the anti-vaccination riot, Montreal became a focal point for discussions on public health, individual rights, and the role of government in disease prevention. The incident prompted authorities to reevaluate their communication strategies, recognizing the importance of addressing public concerns and dispelling myths surrounding vaccination. Over time, as the scientific understanding of vaccines improved and their efficacy became more evident, anti-vaccination sentiments gradually waned.
The anti-vaccination riot of 1885 in Montreal remains a historical testament to the complex interplay between public health initiatives, cultural beliefs, and civic unrest. It serves as a reminder of the challenges faced by communities in embracing medical advancements and highlights the importance of effective communication in fostering trust and cooperation during times of public health crises.
The Spanish Flu of 1918
The 1918 Spanish flu remains one of the deadliest pandemics in history, killing at least 40 million people from 1917 to 1919, according to the most modest estimates. Recent research suggests that figure may be closer to 100 million. The first names given to this flu were varied: the Purple Plague, Purulent Bronchitis, Three-Day Fever, Influenza, Flanders Fever, Blitzkatarrh, Sand Fever, and of course the “Spanish Flu,” which wrongly identified Spain as the origin of the virus.
The Spanish Flu, a dark chapter in global pandemic history, has its roots in the tumult of the First World War. The origin of this pandemic can be explored through several crucial elements that shaped its emergence and spread.
1. Wartime Information Censorship: During World War I, information censorship was commonplace in countries involved in the conflict. Governments sought to tightly control the narrative to preserve public morals, avoid panic, and protect war interests. This censorship had significant implications, as it hindered the dissemination of vital information, including that related to the emergence of diseases.
2. Spain’s Role as a Neutral Witness: Spain, remaining neutral during the war, played a crucial role as an impartial witness to the ravages of the disease. Exempt from the censorship constraints that hampered other nations, Spain openly reported the devastating effects of a newly identified disease on its territory. This transparency was double-edged, because it made Spain the first country identified as the center of the pandemic.
3. Unfair Stigmatization of Spain: With approximately 8 million Spaniards affected, the country was wrongly designated as the source of the pandemic, leading to the name “Spanish Flu”. Spanish authorities, although they were the first to report the disease, never admitted responsibility for its origin. Ironically, they accused France of being the origin of the “killer flu”, creating an unfair stigma.
4. Subsequent Research and Links to France: Subsequent investigations have shed light on possible links between the Spanish Flu and viral evolution in Etaples, France. The conditions of war, with large concentrations of troops, created an environment conducive to the mutation and spread of the virus. Thus, France has been suggested as a likely location for the emergence of this pandemic.
5. Complexity of Viral Origins: It is essential to highlight the complexity surrounding the viral origins of the Spanish Flu. Factors related to war, censorship, troop movements and harsh sanitary conditions have all contributed to the rapid spread of this disease, leaving its exact origin subject to debate among researchers.
In summary, the Spanish Flu has its roots in a complex combination of factors linked to war, censorship, the neutrality of Spain and precarious health conditions. His story is a reminder of the challenges inherent in understanding pandemics and highlights the importance of a holistic approach in analyzing historical events of this magnitude.
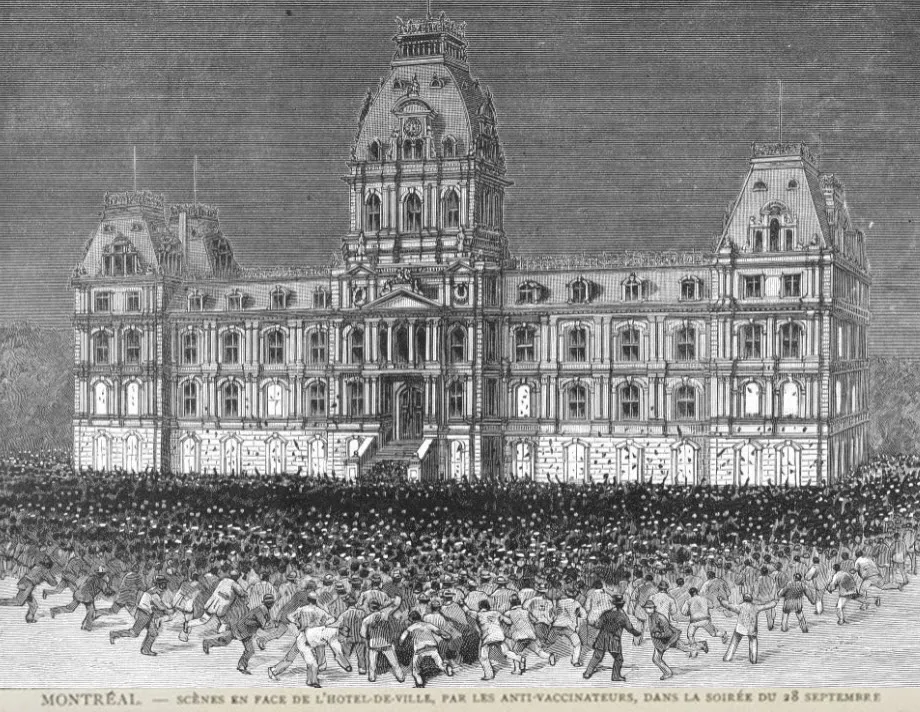
Étaples and Viral Evolution
Étaples, located on the northern coast of France, played a significant role in the viral evolution that led to the dreaded 1918 influenza strain, known as the Spanish Flu. This vast military camp, housing around 100,000 soldiers, was much more than just a gathering place. It was almost a city in its own right, with constant movement of sick and injured troops, creating a fertile ground for viruses to evolve.

1. Size of the Military Town: Etaples, with its massive population of 100,000 soldiers, formed a large-scale military town. Crowded conditions, continuous troop movements, and densely occupied infrastructure have created an environment conducive to the rapid transmission of pathogens, thereby promoting viral evolution.
2. Constant Movements of Sick and Wounded Soldiers: The nature of the First World War resulted in a constant flow of sick and wounded soldiers to Etaples. Precarious medical conditions and poor hygiene measures facilitated the spread of diseases among the military population, creating a context conducive to the evolution of viruses.
3. Viral Exchanges with Animals from Local Markets: Interactions between soldiers stationed in Etaples and animals from local French markets were important vectors of viral exchanges. These animals were often used for various logistical services and were in close contact with soldiers. These interactions contributed to the transmission of viruses between species, thereby facilitating viral evolution.
4. Professor John Oxford and the Research: The work of Professor John Oxford has shed particular light on the role of Etaples in the evolution of the 1918 flu. His research indicates that this military camp was a major focus of evolution viral, with emerging virus strains that later contributed to the formation of the strain responsible for the Spanish Flu.
5. Major Focus of Viral Evolution: Etaples, due to its nature as a crowded military town and the various factors at play, is considered a major focus of viral evolution during the First World War. The conditions prevailing in this camp favored the transformation of viruses, leading to the emergence of potentially more virulent strains.
The Spanish Flu: A Deadly Turning Point
The Spanish flu, which occurred between 1918 and 1919, remains one of the deadliest pandemics in human history, having affected millions of people around the world. This scourge stood out for its devastating attack, targeting healthy adults, unlike the usual patterns where the elderly and young children are the most vulnerable.
Initially, the Spanish flu manifested itself insidiously, starting as a regular flu with symptoms such as sore throat, chills and fever. However, it quickly took a deadly turn by violently targeting the lungs. Patients often faced complete respiratory failure within hours, a tragic outcome underscored by autopsies revealing hard, red lungs submerged in fluid.
The anatomy of the victims provided alarming clues. The pulmonary alveoli, normally filled with vital air, were invaded by a devastating liquid, causing affected individuals to drown. The appearance of mahogany spots on the face signaled the severity of the disease, creating a poignant contrast with later cyanosis, giving patients a characteristic blue-black hue.
What made the Spanish flu particularly fearsome was its ability to wreak havoc among the young, healthy population. Medical experts at the time were baffled by this unusual feature, breaking with established epidemiological patterns. The consequences of this pandemic have been felt globally, affecting not only public health but also the social and economic order of many nations.
Subsequent research has attempted to demystify the origins of this deadly flu, often pointing to conditions conducive to viral evolution. Overcrowded military camps, such as Etaples in France, have been identified as potential hotbeds for the emergence of the 1918 viral strain. Thus, the Spanish flu remains a dark chapter in medical history, highlighting the vulnerability of the humanity in the face of devastating pandemics.
Osteopathic Reaction to the Spanish Flu
During the devastating Spanish Flu pandemic between 1918 and 1919, osteopaths adopted alternative approaches in hopes of treating patients affected by this deadly disease. Faced with the absence of conventional remedies, some practitioners sought solutions in osteopathic methods, believing that these interventions could offer relief and even stop the progression of the flu.
Osteopathy during the Spanish Flu was characterized by extensive use of manipulations aimed at relaxing the muscles along the spine. Osteopaths believed that muscle relaxation could help alleviate symptoms, particularly respiratory problems which were a critical aspect of the Spanish flu. Osteopathic manipulations were designed to promote greater mobility of the ribs and respiratory muscles, providing potential relief to patients struggling with respiratory failure.
Some osteopaths of the time put forward the idea that osteopathy could intervene at an early stage of the disease, thus stopping its progression. They argued that strengthening the musculoskeletal system through osteopathy could help the body better resist and overcome viral infection. According to this perspective, patients treated with osteopathic methods could have escaped a severe deterioration in their health and recovered without the serious after-effects often associated with the Spanish flu.
However, it is important to note that these osteopathic approaches were controversial and largely unrecognized in conventional medical circles of the time. While some osteopaths reported successes, other skeptics pointed out the lack of solid scientific evidence supporting these alternative practices.
Overall, the osteopathic response to the Spanish flu represents a fascinating example of efforts to combat a devastating pandemic with unconventional medical approaches. Although these methods were not widely adopted or recognized at the time, they reflect the diversity of medical responses to a major health crisis.
Response from Kirksville Osteopaths
Response from Kirksville Osteopaths to the Spanish Flu
In Kirksville, Dr. George Still, vice president of the American School of Osteopathy (ASO), became actively involved in the fight against the Spanish Flu, providing a distinctive osteopathic perspective. He has been critical of the treatment choices of allopaths, highlighting the mixed results of their excessive use of aspirin.
Unlike the allopathic approach, which often focused on medications like aspirin, osteopathy advocated a mechanical approach to treatment. Dr. George Still and other Kirksville osteopaths argued that osteopathic manipulations could play a crucial role in relieving Spanish flu symptoms and contributing to faster recovery of patients.
Osteopathy, with its emphasis on musculoskeletal manipulation, aimed to restore mechanical balance to the body. Dr. Still firmly believed that this approach could help the immune system fight the viral infection while relieving the physical symptoms associated with the Spanish flu, such as respiratory problems.
Overall, the response of Kirksville osteopaths to the Spanish Flu highlights the emergence of osteopathy as a perceived alternative to traditional allopathic methods. Their emphasis on the effectiveness of the mechanical approach in treating the Spanish flu reflects the medical debates and divergent treatment choices that characterized this period of health crisis.
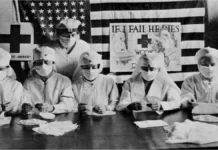
Red Cross Contagious Hospital
Red Cross Contagious Hospital in Kirksville
In Kirksville, a Red Cross contagious hospital was erected to meet the needs of patients affected by the Spanish flu. This hospital facility was the result of a community effort, with the active participation of local businesses and professionals who generously donated their time and materials to quickly equip the facilities.
Medical students, local residents and area businesses joined forces to support the initiative. The particularity of this hospital was its ability to accommodate patients from both schools of medicine, namely doctors of osteopathy (DO) and doctors of traditional medicine (MD). Each could send patients to be treated according to the methods specific to their respective school.
The Red Cross Contagious Hospital was operational for a month, during which it treated a total of 36 patients. Of these, 19 had symptoms of pneumonia, while 17 had Spanish flu. This interdisciplinary collaboration made it possible to provide appropriate care to patients, while demonstrating the unity of the community in the face of this health crisis.

Worldwide Osteopathic Success Stories
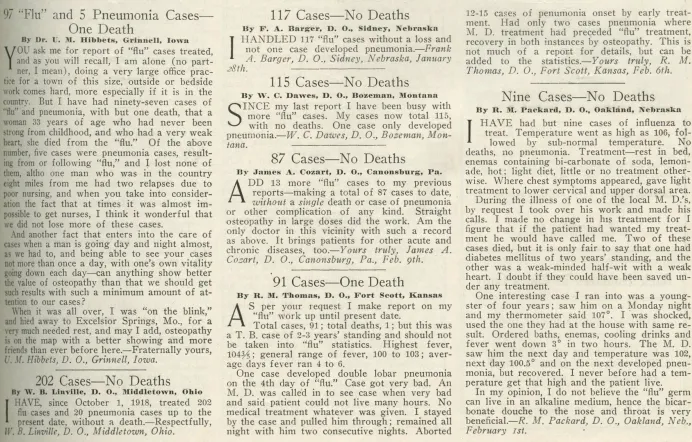
Osteopaths around the world have begun reporting success in treating the Spanish flu. A survey conducted by the American Ostheopathic Association (AOA) revealed significant results. Of a total of 110,122 flu cases treated by doctors of osteopathy (DOs), only 257 died, which equates to a mortality rate of only a quarter of one percent. In comparison, allopathic statistics showed a 40 times higher mortality rate.
This data has had a major impact on the credibility of the osteopathic profession. They have conclusively demonstrated the effectiveness of osteopathic approaches in the management of this pandemic. Attention to osteopathic manipulations and alternative methods has been justified by these impressive results, thereby strengthening confidence in this medical discipline on a global scale.
The Current Challenge
Today, with history as our guide, we are overdue for another pandemic. International travel facilitated by airplanes provides rapid access to every corner of the world. This may facilitate the transmission of future pandemics, similar to the Spanish flu spread by soldiers in World War I. One likely candidate is a strain of avian flu called H5N1, first identified in humans in Hong Kong in 1997.
Conclusion
The 1918 Spanish Flu remains a dark chapter in history, but it also showed how different medical approaches were implemented to combat a global pandemic. Osteopaths, by adopting alternative methods, have contributed to the management of this health crisis. Lessons from this pandemic continue to guide preparation for current and future public health challenges.