Introduction
Posterior cruciate ligament (PCL) rupture is a relatively less common injury than anterior cruciate ligament (ACL) rupture, but it can still cause significant symptoms and instability of the knee. The PCL is one of the primary stabilizers of the knee, helping to prevent the tibia from sliding backward relative to the femur.
PCL tears generally occur following direct or indirect trauma to the knee. Common causes include car accidents, falls on the knee, hard impact during contact sports, or excessive twisting of the knee. During these injuries, the knee can be pushed forward while the tibia remains immobile, causing excessive tension on the PCL and potentially leading to its partial or complete rupture.
Symptoms of a PCL rupture can vary depending on the severity of the injury, but they may include moderate to severe pain in the back of the knee, feeling weak or unsteady when walking or standing. physical activity, swelling and joint stiffness. In some cases, patients may also experience a feeling of giving way or instability in the knee, particularly when attempting to pivot or change direction abruptly.
The diagnosis of PCL rupture is usually confirmed by a combination of clinical examinations and medical imaging. Physical examination may reveal knee laxity during specific tests, such as the posterior drawer test. X-rays may be taken to assess for possible associated fractures, while magnetic resonance imaging (MRI) is often used to directly visualize the ligament and determine the extent of the injury.
Treatment of PCL ruptures depends on several factors, including the severity of the injury, the patient’s activity level, and the presence of associated injuries. In some cases, a conservative approach, including physical therapy to strengthen surrounding muscles and improve joint stability, may be sufficient to relieve symptoms and allow the patient to return to a functional activity level. However, in cases of severe ruptures or those associated with other injuries, surgery may be recommended to reconstruct or repair the ligament and restore stability to the knee.
Anatomy
The posterior cruciate ligament (PCL) is one of the two main cruciate ligaments of the knee, the other being the anterior cruciate ligament (ACL). Located within the knee joint, the PCL plays a critical role in stabilizing and maintaining the structural integrity of the joint.
Anatomically, the PCL is located at the back of the knee, inside the joint capsule. It extends obliquely from the posterior side of the femur (medial femoral condyle) towards the anterior side of the tibia (posterior intercondylar surface). This particular arrangement allows the LCP to control the movements of the tibia relative to the femur, in particular the backward movements of the tibia relative to the femur, called posterior translation movements.
The LCP is composed of bundles of strong and elastic collagen fibers, which give it both mechanical strength and a certain elasticity. These fibers are organized to form a sturdy structure capable of supporting significant loads and resisting tensile and compressive forces in different directions.
The primary function of the PCL is to stabilize the knee by preventing the tibia from sliding backward relative to the femur. It plays a crucial role in maintaining joint integrity and preventing knee instability during functional movements such as walking, running, jumping and spinning.
In addition to its stabilizing function, the PCL also participates in the transmission of forces between the femur and tibia during knee movements. It thus helps to effectively distribute joint stress and protect surrounding joint structures, such as the menisci and cartilaginous surfaces.
Degree of severity of posterior cruciate ligament rupture
Posterior cruciate ligament (PCL) ruptures can vary in severity depending on several factors, including the extent of the injury, the presence of concomitant injuries, symptoms experienced by the patient, and treatment goals. Classifications commonly used to assess the severity of PCL tears include anatomical and functional classifications.
- Anatomical classification:
- Grade I: Stretching or partial tear of the ligament with minor damage to its fibers.
- Grade II: Partial tear of the ligament with moderate to severe damage to the fibers, but the ligament remains structurally intact.
- Grade III: Complete rupture of the ligament, with complete separation of the fibers and loss of continuity of the ligament.
- Functional classification:
- Grade A: Normal knee stability with slight laxity (laxity) of the PCL, but the patient can still perform daily activities without significant symptoms.
- Grade B: Mild knee instability with more pronounced laxity of the PCL, leading to a feeling of sliding or imbalance during activities such as walking, going up or down stairs.
- Grade C: Severe knee instability with significant laxity of the PCL, making it difficult or impossible to perform simple activities and increasing the risk of falls or chronic instability.
In addition to these classifications, other factors can influence the severity of PCL rupture, such as the presence of associated injuries (e.g., meniscal injuries, bone fractures), the presence of symptoms such as pain, instability or joint blockage, and the patient’s treatment goals (e.g., return to a particular level of sporting activity
Mechanism of PCL injury
The posterior cruciate ligament (PCL) is one of the main ligaments stabilizing the knee. Its injury, although less common than that of the anterior cruciate ligament (ACL), can occur during violent trauma or during knee twisting mechanisms.
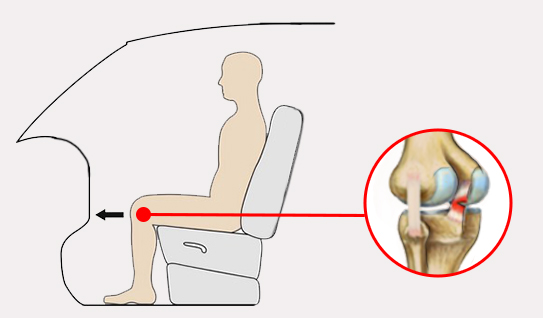
The most common mechanism of PCL injury is direct impact to the anterior aspect of the knee, often associated with a motor vehicle accident or contact sport. During these injuries, the tibia is pushed backwards in relation to the femur, thus putting the PCL under excessive tension. This can lead to partial or complete rupture of the ligament.
Another mechanism of PCL injury is forced hyperextension of the knee. This can happen when falling to the knee or landing from a jump. Excessive hyperextension of the knee can stretch or rupture the PCL, particularly if the ligamentous structures around the knee are already weakened.
PCL injuries can also occur gradually, often in athletes participating in sports that require high rotational movements of the knee, such as alpine skiing or American football. Repeated twisting movements can cause progressive wear of the ligament, eventually leading to injury.
Finally, PCL injuries may also be associated with tibial plateau fractures, particularly when the force of the trauma is great enough to simultaneously damage multiple structures around the knee.
- The injury typically occurs when force is placed on the anterior proximal tibia with a flexed knee.
- Hyperextension and rotational or varus/valgus stress mechanisms can also cause PCL tears.
Pathophysiology of posterior cruciate ligament rupture
The pathophysiology of posterior cruciate ligament (PCL) rupture is complex and can result from various traumatic mechanisms. Here are the main processes involved in LCP rupture:
- Direct trauma : Most PCL tears occur as a result of direct trauma to the knee, such as impact on the anterior aspect of the tibia when the knee is flexed. This type of trauma can occur in car accidents, falls or violent blows during contact sports. During this type of trauma, the force applied to the anterior surface of the tibia can cause excessive tension on the PCL, causing it to partially or completely rupture.
- Forced hyperextension : Forced hyperextension of the knee, which is when the knee is pushed beyond its normal extended position, can also lead to PCL rupture. This can occur during falls onto the knee or during landings from jumps, where the knee is subjected to a force of simultaneous compression and hyperextension. This overload can damage the LCP fibers and lead to rupture.
- Knee twisting : Twisting or rotating movements of the knee can also contribute to PCL rupture. When the knee is subjected to excessive twisting forces, the fibers of the PCL can be stretched beyond their resistance capacity, resulting in a partial or complete tear of the ligament.
- Combination of Forces : In many cases, PCL rupture results from a combination of traumatic forces, such as direct impact, forced hyperextension, and twisting of the knee. These combined forces can place excessive stress on the ligament, exceeding its capacity to withstand and leading to injury.
Once the PCL is ruptured, several pathological processes can occur, including local inflammation, degeneration of ligament fibers, and eventually joint laxity. These changes can lead to symptoms such as pain, knee instability, and decreased joint function.
Causes of posterior cruciate ligament rupture
Posterior cruciate ligament (PCL) rupture can be attributed to several traumatic factors and mechanisms. First of all, direct trauma represents one of the main causes of this injury. A direct impact on the anterior surface of the knee, often linked to car accidents, falls, or violent contact during sports, can cause overtension of the PCL and lead to its rupture. Likewise, forced hyperextension forces may play a crucial role in the occurrence of this injury. When the knee is pushed beyond its normal limit of extension, such as during a fall to the knee or a hard landing after a jump, it can damage the PCL and rupture it.
Twisting or rotating movements of the knee are also contributing factors to PCL rupture. When the knee experiences excessive twisting, especially when the foot is fixed to the ground and the body rotates around the knee joint, this can put stress on the ligament, causing it to partially or completely tear. Certain high-risk sports, such as American football, rugby, downhill skiing, ice hockey, and soccer, place athletes at increased risk of PCL rupture due to the nature of the movements performed and the potential for injury. direct trauma or twisting of the knee.
Furthermore, it is important to note that PCL rupture can also be associated with other knee injuries. Concomitant injuries, such as meniscal injuries, lateral ligament injuries, or bone fractures, may occur simultaneously with PCL rupture. These additional injuries may be the result of the same mechanism of trauma or be caused by joint laxity induced by PCL rupture. Outside of sporting activities, everyday accidents, such as falls on hard surfaces or household accidents, can also lead to PCL rupture if the knee is subjected to significant trauma.
- Direct Trauma: A direct impact to the front of the knee can exert enough force to stretch or tear the posterior cruciate ligament. This can happen in car accidents, falls on the extended knee, or sports collisions.
- Hyperextension of the Knee: Excessive hyperextension of the knee, occurring when the knee is forced to bend backward beyond its normal range of motion, can lead to a rupture of the posterior cruciate ligament.
- Impact During Flexion: Impact on the tibia when the knee is bent can also lead to PCL rupture. This can occur during falls onto a bent knee or other traumatic incidents.
- Incorrect Landing: In some sports, landing incorrectly after a jump can put excessive pressure on the posterior cruciate ligament, causing it to rupture. This can be seen in sports such as football, skiing, or basketball.
- Violent Knee Twisting: Sudden and violent twisting of the knee, especially when the foot is fixed to the ground and the body is moving, can lead to a tear of the posterior cruciate ligament.
- Sports Activities: Certain sports, such as American football, rugby, soccer, and sliding sports, carry an increased risk of posterior cruciate ligament injuries due to the nature of the movements and contacts involved.
- Work Accidents: Work accidents, particularly those involving falls or collisions, can also cause ruptures of the posterior cruciate ligament.
Symptoms of posterior cruciate ligament rupture
A ruptured posterior cruciate ligament (PCL) can cause a range of symptoms, often distinct and varied depending on the severity of the injury and associated lesions. Among these symptoms, knee pain is commonly reported. This can be felt at the back of the knee, but also in the anterior or lateral region. Its nature can vary, from sharp pain during certain activities to a dull, persistent sensation.
Another common symptom is knee swelling. This edema may result from fluid accumulation in the joint following the injury. The swelling may be localized to the back of the knee or spread to the entire joint, causing additional stiffness and discomfort with movement.
Knee instability is also a significant symptom of PCL rupture. This instability is often described as a feeling of “giving” or “sliding” in the knee, particularly when walking, running, or any movement that involves weight-bearing of the knee. Patients may experience a feeling of “giving” or “giving” of the knee, especially during sudden changes of direction or pivoting.
Decreased muscle strength around the knee is also seen in many patients with a PCL rupture. The quadriceps and hamstring muscles may be particularly affected, resulting in a reduced ability to support body weight or perform activities such as going up or down stairs.
Some patients also report a feeling of joint locking. This “stuck” or “stuck” feeling can occur when attempting to fully flex or extend the knee. It may result from the presence of torn fragments of tissue or cartilage in the joint, or be due to joint instability that interferes with normal movement of the knee.
Finally, in addition to physical symptoms, patients with a PCL rupture may also experience subjective sensations such as anxiety, frustration, or fear related to their injury. These feelings can be exacerbated by uncertainty about the severity of the injury and the length of recovery.
- Pain: Pain is one of the most common symptoms of a posterior cruciate ligament rupture. The pain may be felt at the back of the knee and may be worse when walking, bending, or extending the knee.
- Swelling: Significant swelling may develop around the knee due to inflammation caused by the ruptured posterior cruciate ligament.
- Knee Instability: Patients may feel a feeling of instability in the knee, especially when they try to put their weight on the affected leg or when they try to stand up.
- Difficulty Walking: Due to pain and instability, it may be difficult for sufferers to walk normally. Some patients may limp or have an altered gait.
- Limitation of Movement: The ability to fully bend or extend the knee may be compromised due to the injury.
- “Looping” or “Crackling” Sensation: Some patients report feeling a “give” or “crunch” sensation at the time of the incident that led to the rupture of the posterior cruciate ligament.
- Knee Stiffness: A feeling of stiffness may develop, making knee movements less fluid.
- Joint Effusion: A buildup of fluid in the knee joint, called a joint effusion, may occur, contributing to swelling.
- Hematoma: In some cases, a hematoma (collection of blood) may form around the knee due to the rupture of the posterior cruciate ligament.
Assessment of posterior cruciate ligament rupture
Evaluation of posterior cruciate ligament (PCL) rupture involves a series of steps to evaluate the patient’s symptoms, make an accurate diagnosis, and plan appropriate treatment. Here are the main elements of evaluating PCL rupture:
- History : The healthcare professional collects the patient’s medical history, including the circumstances of the injury, current symptoms, history of knee injuries, and physical activities performed. This information can help identify risk factors and guide the clinical examination.
- Clinical examination : The clinical examination of the knee includes an assessment of pain, swelling, range of motion, joint stability and muscle strength. Specific tests, such as the Godfrey test and the pivot-shift test, can be used to assess knee stability and identify a possible PCL rupture.
- Imaging tests : Imaging tests, such as magnetic resonance imaging (MRI) or computed tomography (CT), can be used to confirm the diagnosis of PCL rupture and assess the extent of associated lesions, such as concomitant meniscal or ligamentous lesions.
- Functional assessment : The functional assessment of the knee assesses the impact of the injury on the patient’s daily activities, such as walking, going up and down stairs, as well as participating in sports activities. This assessment can help plan rehabilitation and return to normal activities.
- Assessment of associated injuries : In addition to the PCL rupture, it is important to assess for associated injuries, such as meniscal injuries, concomitant ligament injuries, or bone fractures. This assessment can influence the choice of treatment and the approach to rehabilitation.
Posterior drawer test
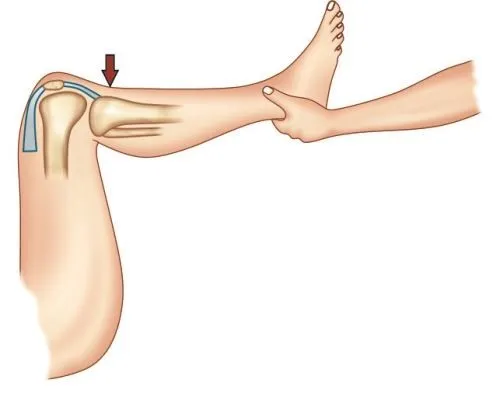
The posterior drawer test is a clinical examination procedure used to assess the integrity of the posterior cruciate ligament (PCL) of the knee. Here is how it is generally done:
- Patient Position: The patient lies supine on an examination table, with knees flexed approximately 90 degrees and feet flat on the surface.
- Practitioner position: The practitioner stands on the side of the knee to be tested. One hand is placed on the patient’s shin, just below the knee, while the other hand is placed on the femur, at thigh level.
- Execution of the test: The practitioner exerts a backward force on the patient’s tibia while holding the femur still. This force is applied in such a way as to push the tibia backwards in relation to the femur.
- Translation Assessment: During force application, the practitioner assesses the amount of translation or movement of the tibia relative to the femur. Excessive translation, relative to the healthy or normal side, may indicate PCL rupture.
- Comparison with the healthy side: The test is generally performed on both knees to allow comparison with the healthy side. A significant difference in posterior drawer translation between the two sides may indicate an abnormality in the knee being tested.

Godfrey test
The Godfrey test, also known as the “Godfrey drop test,” is a clinical examination used to assess laxity of the posterior cruciate ligament (PCL) of the knee. Here is how it is generally done:
- Patient position: The patient lies on an examination table with legs extended and relaxed.
- Practitioner position: The practitioner stands on the side of the knee to be tested.
- Performing the test: The practitioner flexes the patient’s knee to approximately 90 degrees, placing one hand under the patient’s shin to support the lower extremity. The other hand is placed on the patient’s foot.
- Assessment of the position of the tibia: The practitioner observes the position of the tibia in relation to the femur. Normally, the tibia is aligned with the femur when flexed 90 degrees.
- Observation of the fall of the tibia: By gently releasing the hand which supports the patient’s foot, the practitioner observes if there is a posterior fall of the tibia in relation to the femur. An excessive drop may indicate PCL laxity.
- Comparison with the healthy side: The test is generally performed on both knees to allow comparison with the healthy side. A significant difference in tibial drop between the two sides may indicate an abnormality in the knee being tested.
Differential diagnosis
The differential diagnosis of posterior cruciate ligament (PCL) rupture is essential to correctly identify the source of the patient’s symptoms and plan appropriate treatment. Conditions that may present with symptoms similar to PCL rupture include damage to other knee structures, such as the lateral ligaments (lateral collateral ligament), anterior cruciate ligaments (ACL), menisci, and as bone fractures and muscle injuries.
One of the main conditions to rule out is anterior cruciate ligament (ACL) rupture, which can also lead to knee instability and symptoms similar to those of PCL rupture. However, mechanisms of injury and specific clinical tests can help distinguish these two injuries. For example, a positive Lachman or pivot-shift test is often associated with an ACL tear, while a positive Godfrey test may indicate a PCL tear.
Meniscal injuries, especially posterior meniscus tears, can also present with symptoms similar to PCL tears, such as pain, swelling, and instability of the knee. Magnetic resonance imaging (MRI) may be necessary to differentiate these lesions and assess their extent.
Bone fractures around the knee, especially those involving the posterior tibial plateau, may also be associated with symptoms similar to PCL rupture. An X-ray or computed tomography (CT) scan may be necessary to identify these fractures and assess their severity.
Additionally, muscle injuries, such as hamstring muscle tears, may also present with symptoms similar to PCL tears, such as pain and decreased muscle strength. A thorough clinical examination and, sometimes, medical imaging tests, may be necessary to differentiate these lesions.
Finally, other less common conditions, such as peripheral nerve damage or vascular injuries, may also present with symptoms similar to PCL rupture and should be considered in the differential diagnosis.
Conclusion
In conclusion, posterior cruciate ligament (PCL) rupture is a less common injury than anterior cruciate ligament (ACL) rupture, but it can still result in significant symptoms and knee instability. This injury usually occurs following direct or indirect trauma to the knee, such as car accidents, falls on the knee, or excessive twisting movements. Symptoms of a PCL tear include pain in the back of the knee, a feeling of weakness or instability, swelling, and joint stiffness.
The diagnosis of PCL rupture is confirmed by a combination of clinical examinations and medical imaging, such as the posterior drawer test and MRI. Treatment depends on the severity of the injury and may include a conservative approach with physical therapy or surgery to reconstruct or repair the ligament.
It is essential to differentiate PCL rupture from other knee injuries, such as lateral ligament or meniscal injuries, in order to make an accurate diagnosis and plan appropriate treatment. A thorough clinical examination and imaging tests are necessary for this. In summary, effective management of PCL rupture requires careful assessment and an individualized approach for each patient.
References
- Freychet B, Desai VS, Sanders TL, Kennedy NI, Krych AJ, Stuart MJ, Levy BA. All-inside Posterior Cruciate Ligament Reconstruction: Surgical Technique and Outcome. Clin Sports Med. 2019 Apr;38(2):285-295. [ PubMed ]2.
- Hopper GP, Heusdens CHW, Dossche L, Mackay GM. Posterior Cruciate Ligament Repair With Suture Tape Augmentation. Arthrosc Tech. 2019 Jan;8(1):e7-e10. [ PMC free article ] [ PubMed ]3.
- Strauss MJ, Varatojo R, Boutefnouchet T, Condello V, Samuelsson K, Gelber PE, Adravanti P, Laver L, Dimmen S, Eriksson K, Verdonk P, Spalding T. The use of allograft tissue in posterior cruciate, collateral and multi-ligament knee reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019 Jun;27(6):1791-1809. [ PubMed ]4.
- Bernhardson AS, DePhillipo NN, Daney BT, Kennedy MI, Aman ZS, LaPrade RF. Posterior Tibial Slope and Risk of Posterior Cruciate Ligament Injury. Am J Sports Med. 2019 Feb;47(2):312-317. [ PubMed ]5.
- Tadlock BA, Pierpoint LA, Covassin T, Caswell SV, Lincoln AE, Kerr ZY. Epidemiology of knee internal disturbance injuries in United States high school girls’ lacrosse, 2008/09-2016/17 academic years. Res Sports Med. 2019 Oct-Dec;27(4):497-508. [ PubMed ]6.
- Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C, LaPrade RF. Posterior Cruciate Ligament: Current Concepts Review. Arch Bone Jt Surg. 2018 Jan;6(1):8-18. [ PMC free article ] [ PubMed ]7.
- Fanelli GC. Knee Dislocation and Multiple Ligament Injuries of the Knee. Sports Med Arthrosc Rev. 2018 Dec;26(4):150-152. [ PubMed ]8.
- Logterman SL, Wydra FB, Frank RM. Posterior Cruciate Ligament: Anatomy and Biomechanics. Curr Rev Musculoskelet Med. 2018 Sep;11(3):510-514. [ PMC free article ] [ PubMed ]9.
- Lee BK, Nam SW. Rupture of posterior cruciate ligament: diagnosis and treatment principles. Knee Surg Relat Res. 2011 Sep;23(3):135-41. [ PMC free article ] [ PubMed ]10.
- Wang D, Weiss LJ, Abrams M, Barnes RP, Warren RF, Rodeo SA, Taylor SA. Athletes With Musculoskeletal Injuries Identified at the NFL Scouting Combine and Prediction of Outcomes in the NFL: A Systematic Review. Orthop J Sports Med. 2018 Dec;6(12):2325967118813083. [ PMC free article ] [ PubMed ]11.
- Petrillo S, Volpi P, Papalia R, Maffulli N, Denaro V. Management of combined injuries of the posterior cruciate ligament and posterolateral corner of the knee: a systematic review. Br Med Bull. 2017 Sep 01;123(1):47-57. [ PubMed ]12.
- Beaufils P, Becker R, Kopf S, Matthieu O, Pujol N. The knee meniscus: management of traumatic tears and degenerative lesions. EFORT Open Rev. 2017 May;2(5):195-203. [ PMC free article ] [ PubMed ]13.
- Mariani PP, Margheritini F, Christel P, Bellelli A. Evaluation of posterior cruciate ligament healing: a study using magnetic resonance imaging and stress radiography. Arthroscopy. 2005 Nov;21(11):1354-61. [ PubMed ]14.
- Wang D, Graziano J, Williams RJ, Jones KJ. Nonoperative Treatment of PCL Injuries: Goals of Rehabilitation and the Natural History of Conservative Care. Curr Rev Musculoskelet Med. 2018 Jun;11(2):290-297. [ PMC free article ] [ PubMed ]15.
- Bedi A, Musahl V, Cowan JB. Management of Posterior Cruciate Ligament Injuries: An Evidence-Based Review. J Am Acad Orthop Surg. 2016 May;24(5):277-89. [ PubMed ]16.
- Jacobi M, Reischl N, Wahl P, Gautier E, Jakob RP. Acute isolated injury of the posterior cruciate ligament treated by a dynamic anterior drawer brace: a preliminary report. J Bone Joint Surg Br. 2010 Oct;92(10):1381-4. [ PubMed ]17.
- Chandrasekaran S, Ma D, Scarvell JM, Woods KR, Smith PN. A review of the anatomical, biomechanical and kinematic findings of posterior cruciate ligament injury with respect to non-operative management. Knee. 2012 Dec;19(6):738-45. [ PubMed ]18.
- Shelbourne KD, Clark M, Gray T. Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am J Sports Med. 2013 Jul;41(7):1526-33. [ PubMed ]19.
- Shelbourne KD, Muthukaruppan Y. Subjective results of nonoperatively treated, acute, isolated posterior cruciate ligament injuries. Arthroscopy. 2005 Apr;21(4):457-61. [ PubMed ]20.
- Montgomery SR, Johnson JS, McAllister DR, Petrigliano FA. Surgical management of PCL injuries: indications, techniques, and outcomes. Curr Rev Musculoskelet Med. 2013 Jun;6(2):115-23. [ PMC free article ] [ PubMed ]21.
- Jansson KS, Costello KE, O’Brien L, Wijdicks CA, Laprade RF. A historical perspective of PCL bracing. Knee Surg Sports Traumatol Arthrosc. 2013 May;21(5):1064-70. [ PubMed ]22.
- Meleiro SA, Mendes VT, Kaleka CC, Cury RP., Brazilian Society of Orthopedics and Traumatology. Treatment of isolated lesions of the posterior cruciate ligament. Rev Assoc Med Bras (1992). 2015 Mar-Apr;61(2):102-7. [ PubMed ]23.
- Pierce CM, O’Brien L, Griffin LW, Laprade RF. Posterior cruciate ligament tears: functional and postoperative rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2013 May;21(5):1071-84. [ PubMed ]24.
- Wang CJ, Chan YS, Weng LH, Yuan LJ, Chen HS. Comparison of autogenous and allogenous posterior cruciate ligament reconstructions of the knee. Injury. 2004 Dec;35(12):1279-85. [ PubMed ]25.
- Breed A, Friends AA. PCL reconstruction. In vitro biomechanical comparison of ‘isometric’ versus single and double-bundled ‘anatomic’ grafts. J Bone Joint Surg Br. 1998 Jan;80(1):173-9. [ PubMed ]26.
- Wijdicks CA, Kennedy NI, Goldsmith MT, Devitt BM, Michalski MP, Årøen A, Engebretsen L, LaPrade RF. Kinematic analysis of the posterior cruciate ligament, part 2: a comparison of anatomic single- versus double-bundle reconstruction. Am J Sports Med. 2013 Dec;41(12):2839-48. [ PubMed ]



















