Introduction
Psoriatic arthritis (PsA) is a type of inflammatory arthritis that commonly occurs in individuals with psoriasis, a skin disease characterized by the formation of red patches covered with silvery scales. About 5% of people with psoriasis later develop psoriatic arthritis. Psoriasis, an autoimmune disease, occurs when the immune system goes awry, causing the skin to “attack” and form these distinctive inflammatory plaques.
Psoriatic arthritis specifically targets the joints, particularly the hands, thus distinguishing itself from rheumatoid arthritis where mineralization is spared. Although the onset of skin lesions and arthritis is usually desynchronized and independent, 80 to 85% of affected individuals initially present with skin problems. This autoimmune condition affects both men and women, usually occurring between the ages of 20 and 50. Individuals with nail psoriasis are more predisposed to developing psoriatic arthritis.
The onset of psoriatic arthritis is often gradual, gradually spreading to other joints over a period of weeks to months. Although the exact cause of this condition remains unknown, genetics plays a major role in its triggering.
It is crucial to emphasize that psoriatic arthritis can have a significant impact on the quality of life of individuals, requiring appropriate medical management. Regular monitoring by healthcare professionals, such as rheumatologists, can help manage symptoms and minimize joint damage.
Causes of psoriatic arthritis
Psoriatic arthritis is a complex autoimmune disease characterized by joint inflammation and a skin condition called psoriasis. The exact causes of psoriatic arthritis are not fully understood, but several factors are known to contribute to the development of this condition.
First, there is a significant genetic component to psoriatic arthritis. Studies have shown that people who have family members with psoriasis or psoriatic arthritis have a higher risk of developing the disease themselves. Specific genetic variations, such as the HLA-B27 and HLA-Cw6 genes, have been linked to an increased risk of developing this condition.
Second, environmental factors can trigger or worsen psoriatic arthritis in genetically predisposed people. Potential triggers include infections, stress, joint injuries and certain medications. These environmental factors can trigger an abnormal immune response in predisposed individuals, leading to joint inflammation and exacerbation of psoriasis.
Third, the immune system plays a key role in the development of psoriatic arthritis. In this disease, the immune system mistakenly attacks healthy tissues in the body, causing chronic inflammation of the joints and skin. Immune cells, notably T lymphocytes and pro-inflammatory cytokines, are involved in this inflammatory process.
Finally, lifestyle risk factors, such as smoking, excessive alcohol consumption, and obesity, have been associated with an increased risk of developing psoriatic arthritis. These factors can worsen joint inflammation and increase the severity of symptoms in people with this condition.
- Genetic factors: There is a genetic predisposition to psoriatic arthritis. A family history of the disease increases the risk of developing it. Certain genes, such as HLA-B27, have been linked to an increased risk of psoriatic arthritis. Reference: Winchester, R., Minevich, G., Steshenko, V., Kirby, B., Kane, D., & Greenberg, DA (2012). HLA associations reveal genetic heterogeneity in psoriatic arthritis and in the psoriasis phenotype. Arthritis & Rheumatism, 64(4), 1134-1144.
- Immunological factors: An autoimmune reaction is involved in psoriatic arthritis, where the immune system mistakenly attacks healthy tissue, causing joint inflammation. T cells, a type of white blood cell, appear to play a key role in this abnormal immune response. Reference: Ritchlin, CT, & Colbert, RA (2017). Gladman D. Psoriatic Arthritis. New England Journal of Medicine, 376(10), 957-970.
- Predisposition to psoriasis: Most people with psoriatic arthritis have already been diagnosed with psoriasis, suggesting a correlation between the two conditions. Skin lesions of psoriasis often precede the appearance of joint symptoms. Reference: Polachek, A., Li, S., Polachek, IS, Chandran, V., Gladman, DD, & Eder, L. (2018). Psoriatic arthritis disease activity during pregnancy and the first-year postpartum. Seminars in Arthritis and Rheumatism, 47(2), 214-220.
- Environmental factors: Certain environmental triggers, such as infections, stress and physical trauma, can trigger the onset of psoriatic arthritis in genetically predisposed people. These factors can stimulate the immune response and trigger inflammation. Reference: Wilson, FC, Icen, M., Crowson, CS, McEvoy, MT, Gabriel, SE, & Kremers, HM (2009). Incidence and clinical predictors of psoriatic arthritis in patients with psoriasis: a population-based study. Arthritis & Rheumatism, 61(2), 233-239.
- Hormonal factors: Hormonal influences may also play a role, as some cases of psoriatic arthritis appear to be linked to hormonal changes, such as those occurring during pregnancy or menopause. Reference: Bremner, AP, Mason, K., & Pearce, MS (2013). A female preponderance in the incidence of psoriasis in Australasia and validation of an administrative case definition for population-based research. BMC Dermatology, 13(1), 10.
- Metabolic factors: Links between psoriatic arthritis and metabolism have been suggested, particularly with conditions such as obesity and metabolic syndrome. These factors may interact with genetic components to influence the risk of psoriatic arthritis. Reference: Haroon, M., Gallagher, P., Heffernan, E., FitzGerald, O., & Evaluation of an existing screening tool for psoriatic arthritis in people with psoriasis and the development of a new instrument: the Psoriasis Epidemiology Screening Tool ( PEST) questionnaire. Clinical and Experimental Rheumatology, 32(2), 141-145.
Immune cells attack healthy joint tissue, causing inflammation, swelling and pain. Science does not understand why the immune system becomes confused and attacks human cells. However, genetics contribute to its development. In fact, more than 40% of people affected have a family member with this disease.
Symptoms of psoriatic arthritis
Psoriatic arthritis is a form of inflammatory arthritis that affects people with psoriasis, a skin disease characterized by red, scaly patches. Symptoms of psoriatic arthritis vary from person to person, but they tend to affect the joints, skin, and sometimes other parts of the body. Understanding these symptoms is crucial to effectively diagnosing and managing the condition.
Joint pain is one of the most common symptoms of psoriatic arthritis. This pain may be localized in one or more joints and may be felt as a dull, stabbing, or burning pain. It can affect large joints such as the knees, hips or shoulders, as well as small joints in the hands and feet.
In addition to pain, people with psoriatic arthritis may experience joint stiffness, especially in the morning upon waking or after a prolonged period of rest. This stiffness can make movement difficult and uncomfortable, limiting mobility in the affected joints.
Joint inflammation is another characteristic symptom of psoriatic arthritis. Affected joints may become swollen, warm, and red, which can lead to loss of mobility and decreased joint function. This inflammation can also damage cartilage and bone over time, which can lead to long-term complications.
In many people with psoriatic arthritis, red, scaly patches appear on the skin, especially around affected joints. These patches can be accompanied by itching and skin irritation, which can worsen the discomfort and psychological impact of the disease.
Fatigue is a common symptom in people with psoriatic arthritis. This fatigue can be caused by chronic pain, inflammation, and difficulty with daily activities due to symptoms of the disease. It can have a significant impact on quality of life and the ability to lead a normal life.
In advanced cases of untreated psoriatic arthritis, joint deformities may develop. This can lead to impaired joint function and reduced quality of life. Additionally, some people with psoriatic arthritis may develop eye symptoms such as conjunctivitis or uveitis, requiring immediate medical attention.
Joint Symptoms
- Joint pain: Joint pain, often associated with a feeling of stiffness, is one of the most common symptoms of psoriatic arthritis. Pain can be felt in different joints of the body.
- Joint swelling: Affected joints may have visible swelling or feel swollen to the touch.
- Redness and warmth: Affected joints may become red and warm to the touch due to inflammation.
- Stiffness: Joint stiffness, especially in the morning or after periods of inactivity, is common in people with psoriatic arthritis.
- Loss of mobility: Over time, untreated joint inflammation can lead to loss of mobility and decreased joint function.
Skin Symptoms
- Psoriasis: Red, scaly patches on the skin, characteristic of psoriasis, are often seen in people with psoriatic arthritis. Psoriasis can appear before, during or after the onset of joint symptoms.
- Pustules on the palms and soles of the feet: Some individuals experience pus-filled pustules on the palms of the hands and soles of the feet, a specific symptom called pustular psoriasis.
General Symptoms
- Fatigue: People with psoriatic arthritis may experience significant fatigue, which may be related to the inflammation and stress associated with the disease.
- Tendonitis: Inflammation of the tendons (tendinitis) can occur, causing pain and loss of mobility in the affected area.
- Affected nails: Changes in the nails, such as discoloration, thickening, streaking, or separation of the nail from the nail bed (pitting), may occur.
- Edema of fingers or toes: Some people develop swelling of the fingers or toes, called dactylitis, giving these limbs a “sausage” appearance.
- Red, painful eyes: In rare cases, inflammation can affect the eyes, causing a condition called uveitis.
Pathophysiology of joint psoriasis
The pathophysiology of joint psoriasis, also known as psoriatic arthritis, is complex and involves an interaction between genetic, immune and environmental factors. Understanding the underlying mechanisms of this condition is crucial to developing effective and targeted treatments.
At the genetic level, studies have identified several genes associated with joint psoriasis, including genetic variants involved in immune response and inflammation. Among these genes are genes involved in the regulation of the immune system and pro-inflammatory cytokines.
Immunologically, joint psoriasis is considered an autoimmune disease, in which the immune system mistakenly attacks healthy tissues in the body. In joint psoriasis, this autoimmune response results in chronic inflammation of the joints, similar to that seen in other forms of inflammatory arthritis such as rheumatoid arthritis.
A key feature of joint psoriasis is the presence of inflammatory immune cells, such as T lymphocytes and dendritic cells, in affected joints. These cells release pro-inflammatory cytokines, such as TNF-alpha, IL-17, and IL-23, which contribute to inflammation and joint tissue destruction.
The interaction between genetic and environmental factors also plays an important role in triggering and worsening joint psoriasis. Factors such as stress, infections, joint trauma and certain medications can trigger disease flares in genetically predisposed people.
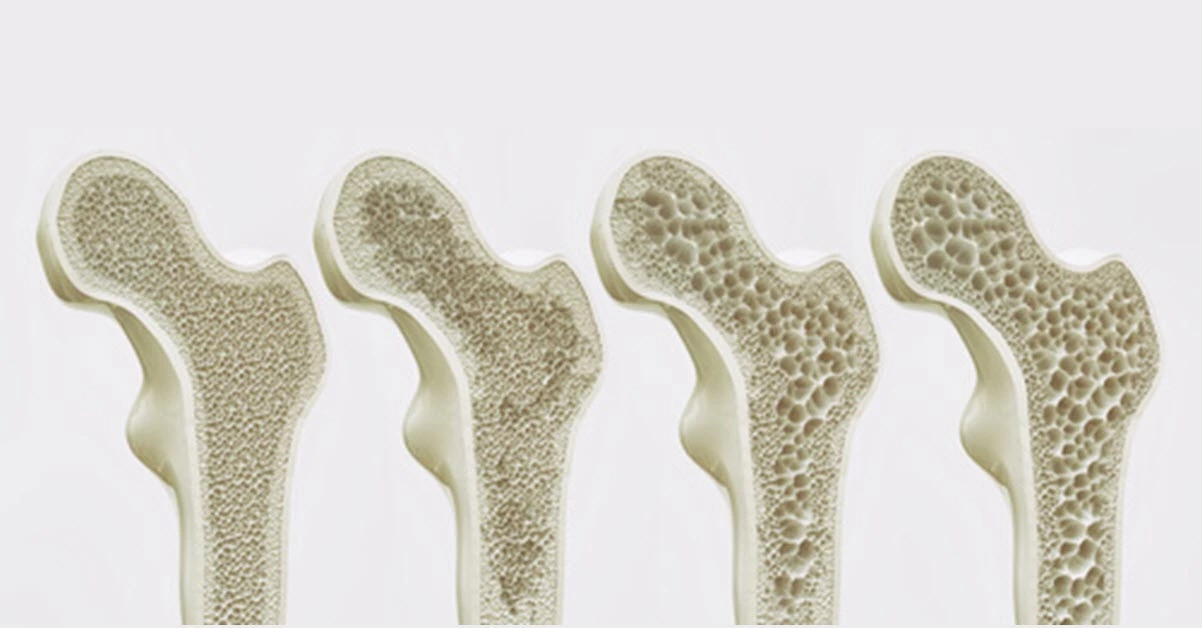
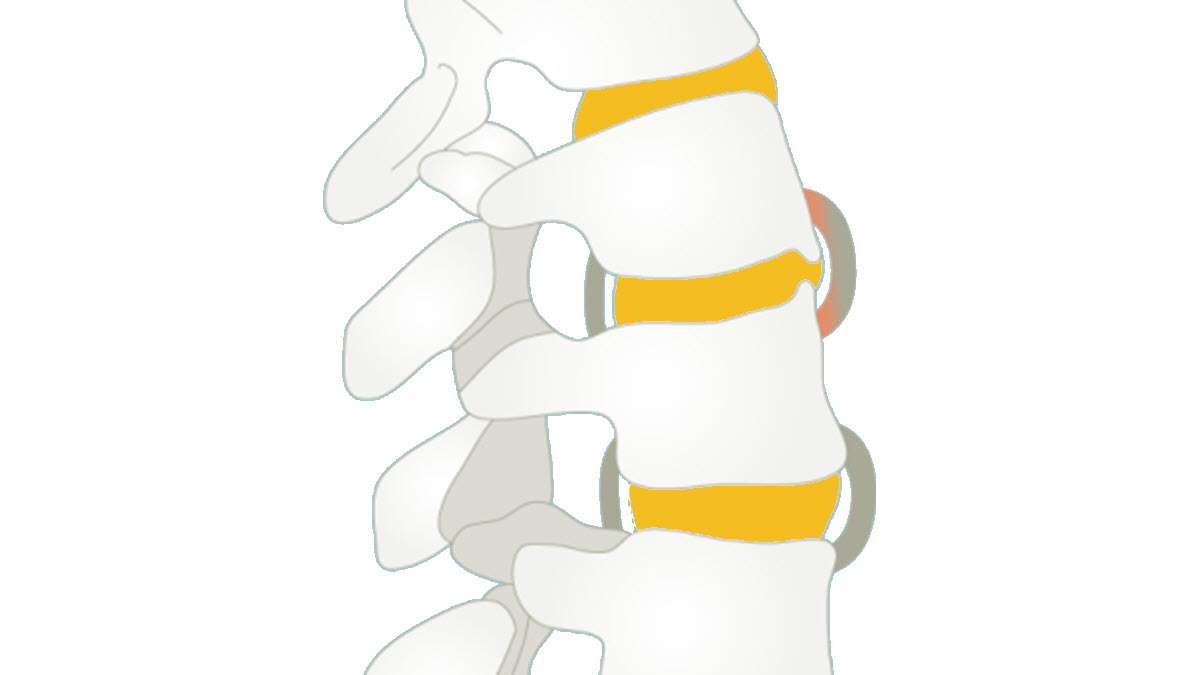
At the joint level, joint psoriasis causes inflammation of the synovial membrane, which lines the inside of the joints. This chronic inflammation leads to hypertrophy of the synovial membrane, the formation of pannus (inflammatory tissue invading the joint tissues) and the progressive destruction of cartilage and bone.
In addition, joint psoriasis is associated with extra-articular manifestations, such as cutaneous manifestations, ocular involvement and cardiovascular comorbidities. These manifestations demonstrate the systemic nature of the disease and highlight the importance of a holistic approach in its management.
- Dysregulated immune response: The pathophysiology begins with dysregulation of the immune system. Immune cells, particularly T lymphocytes, are inappropriately activated, causing an exaggerated immune response.
- Skin inflammation: In the case of psoriasis, this heightened immune response initially targets the skin. Activated T cells enter the skin and trigger inflammation. This leads to the rapid proliferation of skin cells, forming the characteristic erythematous plaques with scales seen in psoriasis.
- Cytokine production: Immune cells release cytokines, signaling proteins that play an essential role in cellular communication. In psoriasis, pro-inflammatory cytokines such as TNF-alpha (tumor necrosis factor alpha) and interleukin-17 (IL-17) are overproduced.
- Impact on joints: In the case of psoriatic arthritis, this inflammation is not limited to the skin. The same pro-inflammatory cytokines circulate in the blood and can reach joints, triggering inflammation in those areas.
- Attack on joints: Immune cells and pro-inflammatory cytokines then attack joint tissues, particularly the synovial membranes that surround the joints. This causes synovial inflammation, characteristic of inflammatory rheumatic diseases.
- Proliferation of synovial tissue: In response to this persistent inflammation, the synovial tissue inside the joints undergoes excessive proliferation. This can lead to the formation of pannus, an inflammatory tissue that can damage surrounding cartilage and bone.
- Joint destruction: Chronic inflammation and proliferation of synovial tissue can lead to progressive joint breakdown, causing irreversible damage, joint deformation and loss of function.
Triggers of psoriatic arthritis
- Infections: Infections, especially streptococcal infections, can trigger an inflammatory response in people who are genetically predisposed to psoriatic arthritis. Upper respiratory infections are often associated with these triggers. Reference: Albanesi, C., Madonna, S., Gisondi, P., & Girolomoni, G. (2018). The Interplay Between Keratinocytes and Immune Cells in the Pathogenesis of Psoriasis. Frontiers in Immunology, 9, 1549.
- Physical Trauma: Physical trauma, such as joint injuries or surgeries, can trigger joint inflammation in some people with a genetic predisposition to psoriatic arthritis. Reference: Queiro-Silva, R., Alperi, M., & López-Larrea, C. (2016). Non-psoriatic spondyloarthritis. Best Practice & Research Clinical Rheumatology, 30(4), 673-688.
- Stress: Emotional stress can act as a potential trigger for psoriatic arthritis. Stressful situations can trigger disease flares or worsen symptoms in some people. Reference: Evers, AW, Verhoeven, EW, Kraaimaat, FW, de Jong, EM, de Brouwer, SJ, Schalkwijk, J., … & van de Kerkhof, PC (2010). How stress gets under the skin: cortisol and stress reactivity in psoriasis. British Journal of Dermatology, 163(5), 986-991.
- Medications: Certain medications, such as beta-adrenergic blockers used to treat high blood pressure, may act as potential triggers for psoriatic arthritis in some people. Reference: Fjellner, B., Hagermark, O., & Hagermark, A. (1985). Substance P antagonists inhibit the release of IL-1 from immunocompetent cells. British Journal of Dermatology, 112(6), 651-656.
- Smoking: Smoking is associated with an increased risk of developing psoriatic arthritis, and it can also worsen symptoms in those who already have it. Reference: Di Lernia, V., & Ricci, C. (2007). Does cigarette smoking protect against psoriasis? Annals of the Rheumatic Diseases, 66(6), 859-860.
- Hormones: Hormonal changes, such as those occurring during pregnancy or menopause, may influence the onset or worsening of psoriatic arthritis in some women. Reference: Cutolo, M., Sulli, A., Pizzorni, C., Accardo, S., & Nailfold capillaroscopy. Best Practice & Research Clinical Rheumatology, 17(6), 979-1006.
Radiological signs of psoriatic arthritis
- Soft tissue swelling – may be due to joint, tendon or soft tissue swelling and dactylitis.
- Erosions – usually well defined and located in a periarticular location (similar to RA) but are more likely to be asymmetric.
- Proliferative new bone formation – characteristic and often coexisting with erosive changes, sometimes giving an ill-defined spiculated appearance at the joint margin.
- Narrowing of the joint space – may develop as the disease progresses.
- Periostitis – inflammation of the periosteal surface, particularly at the shaft, may be visible as increased radiographic density adjacent to the bone surface.
- Sacroiliitis – erosions and new bone formation can occur in the sacroiliac joints, producing irregular margins and sclerosis. irregularities and sclerosis, making these joints difficult to clearly delineate on the x-ray.
- Spondylitis – this can manifest as bony overgrowth (syndesmophytes) throughout the spine. between the vertebrae is less common.
- Bone proliferation at the level of the entheseal attachments – for example at the level of the insertions of the Achilles tendon and the plantar aponeurosis on the limestone. and the plantar aponeurosis at the level of the calcaneus, as well as at enthesis sites around the pelvis.
- Pencil-shaped deformity, osteolysis and ankylosis – Progressive destruction of bone and osteolysis, particularly in the fingertip joints, can lead to bone deformity. especially in the end joints of the fingers, can result in a pointed appearance of the end of the phalanx and a pronounced curved appearance due to the formation of new bones. a pronounced curved appearance caused by the formation of new bone at the base of the adjacent phalanx, giving a “pencil in a cup” appearance.

Conclusion
Psoriatic arthritis is a chronic inflammatory condition that affects both the skin and joints, significantly impacting the quality of life for patients. Osteopathic care offers a complementary approach by improving the mobility of affected structures, reducing pain, and enhancing joint function. By tailoring treatment to the individual needs of each patient, osteopathy can play a valuable role in the overall management of the condition, particularly by addressing mobility, stress, and circulation. A multidisciplinary approach, combining conventional medical treatments with osteopathic interventions, is often recommended to achieve the best long-term outcomes.
It is crucial to consult a healthcare professional for an accurate diagnosis and appropriate management to slow the progression of the disease and improve quality of life.
References
- Karmacharya P, Chakradhar R, Ogdie A. The epidemiology of psoriatic arthritis : A literature review. Best Pract Res Clin Rheumatol. 2021 Jun;35(2):101692. [ PubMed ]
- Eder L, Haddad A, Rosen CF, Lee KA, Chandran V, Cook R, Gladman DD. The Incidence and Risk Factors for Psoriatic Arthritis in Patients With Psoriasis: A Prospective Cohort Study. Arthritis Rheumatol. 2016 Apr;68(4):915-23. [ PubMed ]
- FitzGerald O, Haroon M, Giles JT, Winchester R. Concepts of pathogenesis in psoriatic arthritis : genotype determines clinical phenotype. Arthritis Res Ther. 2015 May 07;17:115. [ PMC free article ] [ PubMed ]
- Wake up JD. The genetic basis of spondyloarthritis. Ann Rheum Dis. 2011 Mar;70 Suppl 1:i44-50. [ PubMed ]
- Gladman DD, Anhorn KA, Schachter RK, Mervart H. HLA antigens in psoriatic arthritis . J Rheumatol. 1986 Jun;13(3):586-92. [ PubMed ]6.O’Rielly DD, Rahman P. Clinical and molecular significance of genetic loci associated with psoriatic arthritis . Best Pract Res Clin Rheumatol. 2021 Jun;35(2):101691. [ PubMed ]
- Nair RP, Stuart PE, Nistor I, Hiremagalore R, Chia NVC, Jenisch S, Weichenthal M, Abecasis GR, Lim HW, Christophers E, Voorhees JJ, Elder JT. Sequence and haplotype analysis supports HLA-C as the psoriasis susceptibility 1 gene. Am J Hum Genet. 2006 May;78(5):827-851. [ PMC free article ] [ PubMed ]
- Cafaro G, McInnes IB. Psoriatic arthritis : tissue-directed inflammation? Clin Rheumatol. 2018 Apr;37(4):859-868. [ PubMed ]
- Feld J, Chandran V, Haroon N, Inman R, Gladman D. Axial disease in psoriatic arthritis and ankylosing spondylitis: a critical comparison. Nat Rev Rheumatol. 2018 Jun;14(6):363-371. [ PubMed ]
- Feld J, Ye JY, Chandran V, Inman RD, Haroon N, Cook R, Gladman DD. Is axial psoriatic arthritis distinct from ankylosing spondylitis with and without concomitant psoriasis? Rheumatology (Oxford). 2020 Jun 01;59(6):1340-1346. [ PubMed ]
- Thorleifsdottir RH, Sigurdardottir SL, Sigurgeirsson B, Olafsson JH, Sigurdsson MI, Petersen H, Arnadottir S, Gudjonsson JE, Johnston A, Valdimarsson H. Improvement of psoriasis after tonsillectomy is associated with a decrease in the frequency of circulating T cells that recognize streptococcal determinants and homologous skin determinants. J Immunol. 2012 May 15;188(10):5160-5. [ PubMed ]
- Thrastardottir T, Love TJ. Infections and the risk of psoriatic arthritis among psoriasis patients: a systematic review. Rheumatol Int. 2018 Aug;38(8):1385-1397. [ PubMed ]
- Pattison E, Harrison BJ, Griffiths CE, Silman AJ, Bruce IN. Environmental risk factors for the development of psoriatic arthritis : results from a case-control study. Ann Rheum Dis. 2008 May;67(5):672-6. [ PubMed ]
- Eder L, Law T, Chandran V, Shanmugarajah S, Shen H, Rosen CF, Cook RJ, Gladman DD. Association between environmental factors and onset of psoriatic arthritis in patients with psoriasis. Arthritis Care Res (Hoboken). 2011 Aug;63(8):1091-7. [ PubMed ]