Introduction
Sciatica, the nagging discomfort caused by compression of the sciatic nerve, can truly turn everyday life into a constant challenge. Limited mobility and persistent pain can quickly affect quality of life. In the face of this challenge, osteopathy is emerging as a powerful complementary approach, offering tangible hope for those who aspire to free their lives from the painful grip of sciatica.
The essence of osteopathy lies in a holistic approach, where the practitioner, armed with extensive knowledge of anatomy and physiology, uses precise and gentle manipulations to restore the musculoskeletal balance of the body. By focusing specifically on the areas impacted by sciatica, these practitioners aim to release muscle tension, improve blood circulation and reduce pressure on the sciatic nerve. Each osteopathy session is individually tailored, taking into account the particularities of each individual’s condition, thus creating a space conducive to relief.
Osteopathic sciatica relief is not limited to simply managing symptoms, but also explores the underlying causes of the condition. Osteopathic practitioners not only assess acute symptoms, but also examine postural habits, muscle imbalances, and other elements that may be contributing to the manifestation of sciatica. This preventative approach aims not only to relieve current pain but also to prevent recurrences, thus providing a complete and lasting solution.
Choosing osteopathy as a path to sciatica relief often represents much more than just pain relief. It is a redemption of freedom of movement, a rediscovery of flexibility and a rebirth of overall well-being. This therapeutic method offers a soothing power that transcends the simple resolution of symptoms to breathe new life into those who seek to find a lighter daily life, where comfort and mobility become the watchwords of a fulfilling existence.
How Sciatica Develops: Pathophysiology
The pathophysiology of sciatica can be understood through several key steps:
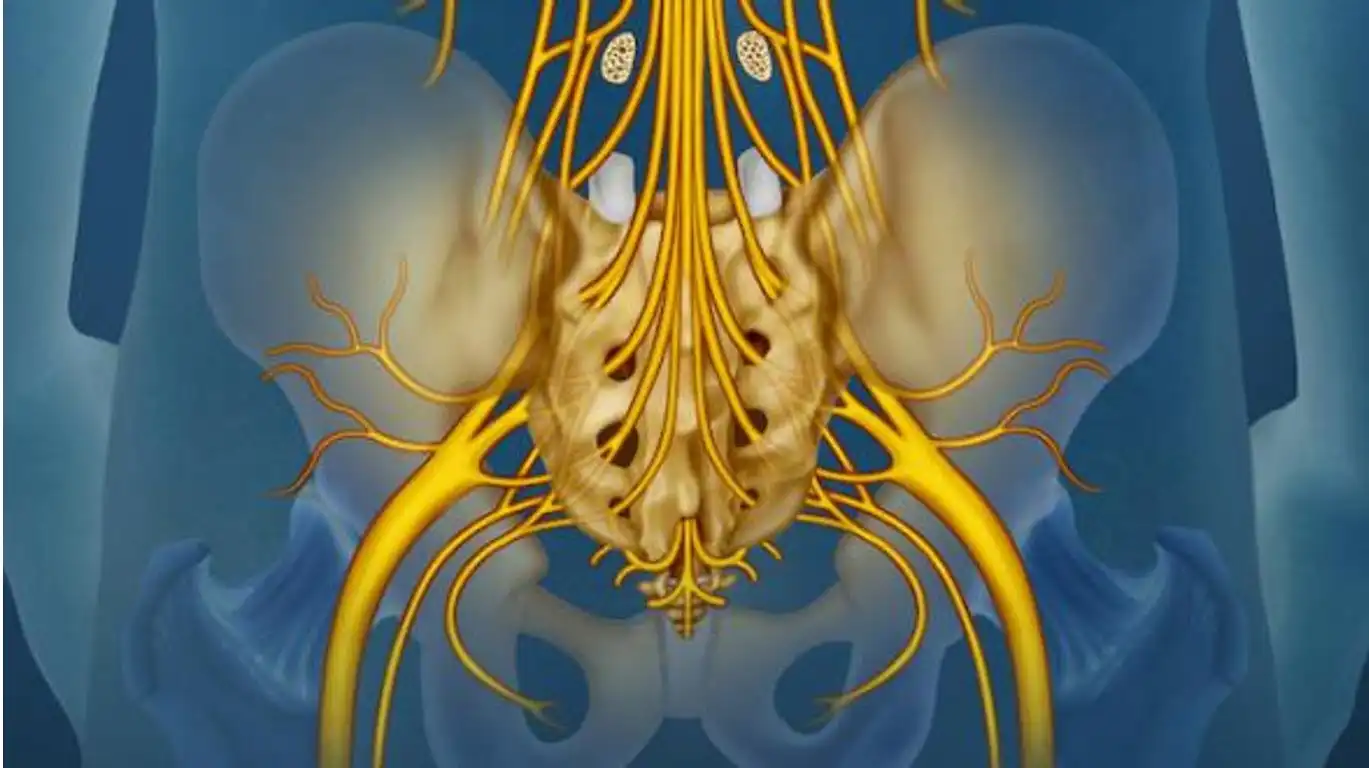
- Nerve Compression: The root cause of sciatica is compression of the sciatic nerve, usually in the lumbar spine. This compression can be due to several factors, including a herniated disc, spinal stenosis, spondylolisthesis, or muscle spasms. These conditions either put direct pressure on the nerve or create an inflammatory environment that can compress the nerve.
- Local Inflammation: Compression of the sciatic nerve triggers an inflammatory response. The surrounding tissues respond by releasing inflammatory mediators, resulting in swelling and irritation of the nerve. Inflammation contributes significantly to the pain and other symptoms associated with sciatica.
- Impaired Nerve Conduction: Compression of the sciatic nerve can disrupt the normal conduction of nerve impulses. This often results in symptoms such as shooting pain, tingling, burning sensations, and decreased sensation along the sciatic nerve.
- Muscle Responses: The presence of sciatica can induce muscle spasms in the surrounding areas. These spasms can worsen nerve compression and contribute to symptoms such as stiffness and loss of mobility.
- Reflex and Postural Responses: The pain associated with sciatica can trigger reflex responses, causing changes in posture and movement to relieve pressure on the nerve.
What Causes Sciatica?
Sciatica is a condition characterized by pain radiating along the path of the sciatic nerve, which extends from the lower back through the hips and buttocks and down each leg. This pain is often a symptom of an underlying issue that causes compression or irritation of the sciatic nerve. The most common cause of sciatica is a herniated disc, which occurs when the soft center of a spinal disc protrudes through a crack in the tougher exterior casing. This herniation can press on the nerve roots that form the sciatic nerve, leading to pain and discomfort. Another frequent cause is spinal stenosis, a narrowing of the spinal canal that puts pressure on the nerves. This condition often results from degenerative changes in the spine due to aging, which can lead to the thickening of ligaments, overgrowth of bone, and bulging of discs, all contributing to reduced space for the nerves. Degenerative disc disease, a condition where the discs between the vertebrae break down over time, can also contribute to sciatica by causing instability and inflammation in the spinal segments. Spondylolisthesis, a condition in which a vertebra slips out of place onto the bone below it, can also lead to sciatic nerve compression.
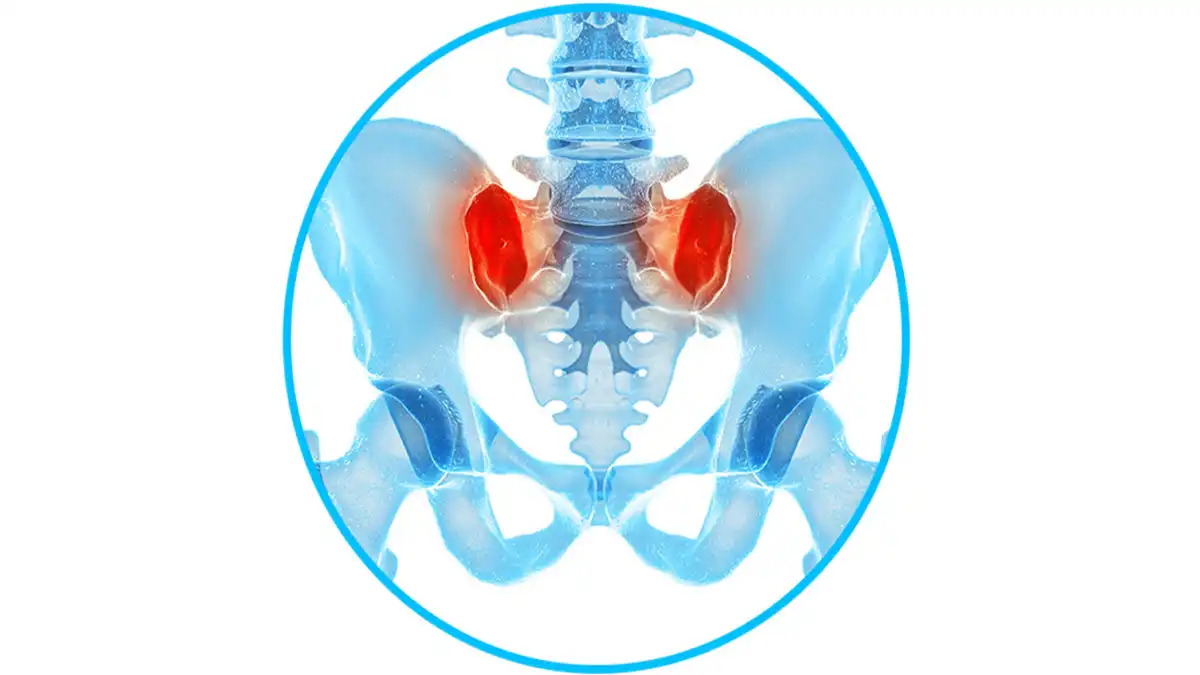
Additionally, sciatica may be caused by piriformis syndrome, where the piriformis muscle in the buttocks spasms or tightens, putting pressure on the sciatic nerve. This muscle is located near the sciatic nerve, and inflammation or injury can lead to nerve irritation. Another contributing factor can be traumatic injuries, such as fractures or falls, which might lead to direct pressure on the nerve. Less commonly, tumors or cysts in the lumbar region can compress the sciatic nerve, causing symptoms. In some cases, metabolic diseases such as diabetes can lead to diabetic neuropathy, which may involve the sciatic nerve, leading to symptoms similar to sciatica. Certain lifestyle factors can increase the risk of developing sciatica, including obesity, which puts additional stress on the spine, and sedentary habits, which can lead to weakened back muscles. Prolonged sitting, particularly with poor posture, may exacerbate sciatic pain. Moreover, occupational factors that require heavy lifting, twisting, or long periods of standing can also increase the risk of nerve damage or irritation leading to sciatica. Pregnancy can sometimes result in sciatica due to the combination of weight gain, altered center of gravity, and hormonal changes that can affect spinal stability. It’s important to recognize that while the pain of sciatica is the most obvious symptom, other accompanying symptoms may include numbness, tingling, or weakness in the affected leg or foot, and in severe cases, loss of bladder or bowel control, which requires immediate medical attention.
Here are some common causes of sciatica:
- Herniated disc: A herniated disc occurs when the jelly-like core inside an intervertebral disc protrudes through the outer wall of the disc, putting pressure on the sciatic nerve.
- Spinal stenosis: Spinal stenosis occurs when the spinal canal narrows, putting pressure on the spinal cord and nerves, including the sciatic nerve.
- Spondylolisthesis: This condition occurs when one vertebra slips forward relative to the adjacent vertebra, compressing the sciatic nerve.
- Piriformis syndrome: The sciatic nerve can pass through the piriformis muscle located in the buttock. If this muscle becomes tight or spasmodic, it can compress the nerve and cause sciatica symptoms.
- Tumors: Tumors located near the sciatic nerve or in the spinal canal can put pressure on the nerve and cause sciatica symptoms.
- Trauma: Injuries to the spine, such as fractures, can damage the sciatic nerve and lead to sciatica symptoms.
Understanding Sciatica Symptoms
Sciatica is characterized by a range of symptoms that result from irritation or compression of the sciatic nerve, which is the largest nerve in the human body. The hallmark symptom of sciatica is pain that radiates from the lower back down through the buttock and into one leg, following the path of the sciatic nerve. This pain can vary in intensity from a mild ache to a sharp, burning sensation or excruciating discomfort. Often, patients describe the pain as shooting or electric, which can be debilitating. The pain typically affects only one side of the body and can extend from the lower back to the back of the thigh and down the leg, sometimes reaching as far as the foot or toes. In addition to pain, sciatica is often accompanied by numbness or tingling in the leg or foot. This sensation, known as paresthesia, often occurs in the areas that experience pain and can lead to a “pins and needles” feeling. Some patients experience muscle weakness in the affected leg or foot, which can affect mobility and the ability to perform everyday activities such as walking, standing, or sitting for extended periods. This weakness can be subtle, with patients noticing that they have difficulty lifting the foot off the ground, a condition known as “foot drop.” The symptoms of sciatica are often exacerbated by prolonged sitting, standing, or movements that involve bending, twisting, or lifting. Coughing, sneezing, or sudden movements can also intensify the pain, as these actions increase pressure on the sciatic nerve.
Many individuals with sciatica report that their symptoms worsen at night, potentially disrupting sleep and affecting overall quality of life. In some cases, the pain may be alleviated by changing positions, such as lying down with the knees elevated or using a firm mattress that supports the spine’s natural alignment. Although sciatica typically presents with a combination of pain, numbness, and weakness, the exact symptoms can vary widely depending on the underlying cause and the specific nerve roots affected. For instance, if the sciatic nerve’s upper part is compressed, the pain may be more pronounced in the buttocks and thigh, while compression lower along the nerve can result in symptoms concentrated in the calf and foot. In severe cases, sciatica may lead to more serious neurological symptoms, such as a loss of bladder or bowel control, which could indicate a condition called cauda equina syndrome. This rare but serious complication requires immediate medical attention. It is important to seek a proper diagnosis and treatment plan if sciatica symptoms persist or worsen, as early intervention can help prevent chronic pain and potential complications. Treatment options typically include physical therapy, medications to manage pain and inflammation, and, in some cases, surgical interventions to address the underlying cause of nerve compression. Understanding the symptoms of sciatica can aid in seeking timely medical advice and implementing effective management strategies to alleviate discomfort and improve daily function.
Symptoms of sciatica can vary from person to person, but they are usually associated with irritation or compression of the sciatic nerve. Common symptoms of sciatica include:
- Radicular pain: Pain is the main symptom of sciatica. It can be intense and throbbing, following the path of the sciatic nerve. The pain can start in the lower back, pass through the buttocks and go down the leg, sometimes to the foot.
- Tingling and numbness: Some people may experience tingling or numbness along the path of the sciatic nerve. This may occur in the buttock, leg, or foot.
- Muscle weakness: Compression of the nerve can cause muscle weakness in the affected leg. This can make it difficult to perform certain activities, such as getting up from a chair or climbing stairs.
- Pain worse when sitting: Pain may be worse when sitting, especially for prolonged periods.
- Coughing or sneezing that makes pain worse: Pain may be worse with coughing, sneezing, or physical exertion.
- Loss of bladder or bowel control (rare): In rare cases of severe sciatic nerve compression, there may be loss of bladder or bowel control, which requires immediate medical attention.
It is important to note that sciatica is not a disease in itself, but rather a symptom of other health problems, such as a herniated disc, spinal stenosis, or other conditions that affect the sciatic nerve.
Risk factors of sciatica
Certain factors can increase the risk of developing sciatica. These risk factors may include:
- Age: Sciatica is most common in people between the ages of 30 and 50, as the aging process can lead to degeneration of the intervertebral discs and other changes in the spine.
- Obesity: Being overweight or obese can put increased pressure on the spine, increasing the risk of sciatic nerve compression.
- Sedentary Lifestyle: A sedentary lifestyle can contribute to the development of sciatica. Inactivity weakens the back muscles and can lead to spinal health problems.
- Physical work: Certain jobs requiring repetitive movements, frequent lifting, or awkward positions can increase the risk of sciatica.
- Diabetes: People with diabetes have an increased risk of peripheral neuropathy, which can also affect the sciatic nerve.
- Smoking: Smoking can cause decreased blood flow to the spine, which can contribute to disc problems and increase the risk of sciatica.
- Genetic factors: Some individuals may have a genetic predisposition to developing spinal problems, increasing their susceptibility to sciatica.
It is important to note that even in the absence of these risk factors, a person can develop sciatica due to a specific injury or condition. Managing modifiable risk factors, such as maintaining a healthy weight and adopting an active lifestyle, can help prevent or alleviate sciatica symptoms.
How Sciatica is Diagnosed
Medical History
- Symptoms Assessment:
- Patients are asked to describe their symptoms, including the location, nature (sharp, dull, burning), and severity of the pain. Sciatica typically presents as pain that radiates from the lower back down to the leg and can be accompanied by numbness, tingling, or weakness.
- Onset and Duration:
- The doctor may inquire about when the pain started, its duration, and any activities or positions that worsen or relieve it.
- Previous Injuries or Conditions:
- Any history of back injuries, herniated discs, or conditions like arthritis is considered.
2. Physical Examination
- Range of Motion Tests:
- The patient may be asked to perform certain movements to see if they exacerbate or alleviate the pain, such as bending forward, backward, or to the sides.
- Neurological Examination:
- The doctor will test reflexes, muscle strength, and sensory perception in the legs to check for signs of nerve compression.
- Lasègue sign:
- Maneuver:
- Patient in supine position
- Thigh bent at 90° and knee bent at 90°
- Progressive extension of the knee while keeping the hip flexed
- Thigh pain radiating down the leg = +v
- Maneuver:

- Extended leg raise test:
- To perform the test, the patient lies supine on the bench. Holding onto the affected side, you will grasp the patient’s leg so that the knee is fully extended during the test. Then, slowly raise the leg to induce hip flexion while maintaining full knee extension and carefully observe the patient’s response.
- Interpretation: If the patient experiences sciatic pain, and more specifically pain radiating down the leg (radiculopathy), when the straightened leg is at an angle between 30 and 70 degrees, then the test is positive and a herniated disc is a possible cause of the pain. A negative test suggests a likely different cause for the back pain.

- Rollover test:
- Extending the leg while sitting causes the back to extend or roll backwards due to tension on the sciatic nerve.

3. Diagnostic Imaging Tests
While a physical examination and medical history can often lead to a presumptive diagnosis, imaging tests help confirm the diagnosis and determine the underlying cause.
- X-rays:
- These can show bone spurs or arthritis affecting the spine but may not reveal herniated discs or nerve damage.
- Magnetic Resonance Imaging (MRI):
- An MRI provides detailed images of soft tissues, including herniated discs and nerve roots, and is the most common imaging test used to diagnose sciatica.
- Computed Tomography (CT) Scan:
- A CT scan, sometimes combined with a myelogram (where a dye is injected into the spinal canal), can provide detailed cross-sectional images of the spinal structures.
- Electromyography (EMG):
- EMG measures the electrical activity in muscles and can help identify nerve compression or damage.
4. Differential Diagnosis
- Ruling Out Other Conditions:
- Conditions such as piriformis syndrome, hip bursitis, or spinal stenosis may mimic sciatica symptoms. The doctor may use specific tests to rule out these conditions.
- History of Diseases:
- Conditions like diabetes, which can cause neuropathy, should be considered in the differential diagnosis.
References
- Lagerbäck T, Fritzell P, Hägg O, Nordvall D, Lønne G, Solberg TK, Andersen MØ, Eiskjær S, Gehrchen M, Jacobs WC, van Hooff ML, Gerdhem P. Effectiveness of surgery for sciatica with disc herniation is not substantially affected by differences in surgical incidences among three countries: results from the Danish, Swedish and Norwegian spine registries. Eur Spine J. 2019 Nov;28(11):2562-2571. [PubMed]
- Alrwaily M, Almutiri M, Schneider M. Assessment of variability in traction interventions for patients with low back pain: a systematic review. Chiropr Man Therap. 2018;26:35. [PMC free article] [PubMed]
- Hong X, Shi R, Wang YT, Liu L, Bao JP, Wu XT. Lumbar disc herniation treated by microendoscopic discectomy : Prognostic predictors of long-term postoperative outcome. Orthopade. 2018 Dec;47(12):993-1002. [PubMed]
- Flug JA, Burge A, Melisaratos D, Miller TT, Carrino JA. Post-operative extra-spinal etiologies of sciatic nerve impingement. Skeletal Radiol. 2018 Jul;47(7):913-921. [PubMed]
- Hicks BL, Lam JC, Varacallo M. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Feb 12, 2022. Piriformis Syndrome. [PubMed]
- Delgado-López PD, Rodríguez-Salazar A, Martín-Alonso J, Martín-Velasco V. [Lumbar disc herniation: Natural history, role of physical examination, timing of surgery, treatment options and conflicts of interests]. Neurocirugia (Astur). 2017 May – Jun;28(3):124-134. [PubMed]