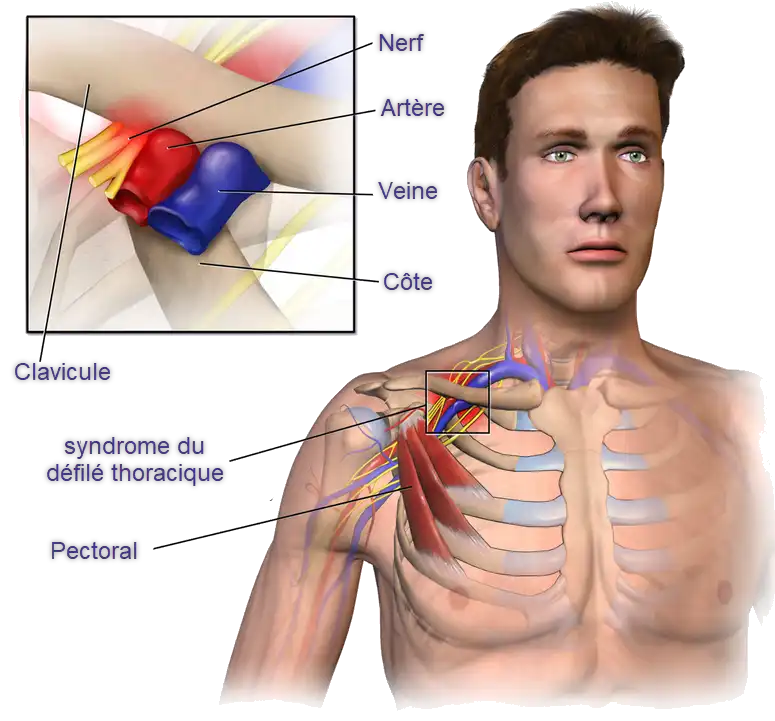
The brachial pluxus consists of nerve roots C5 to C8 and D1 and provides innervation to the entire upper limb. It travels with the subclavian artery between the anterior and medial scalenes (the intrascalene space). The subclavian vein becomes part of the neurovascular bundle as it passes under the clavicle (the costoclavicular space) and travels under the insertion of the pectoralis minor (the subpectoral space) before continuing the along the arm.
What are the types of compression?
- Neurogenic
- Venous
- Arterial
Approximately 95% of cases of thoracic outlet syndrome are neurogenic. Others are rare, but more serious when it affects a vein or artery.

Causes
- Anatomical Anomalies:
- People who are born with anatomical abnormalities, such as an extra rib (cervical rib), abnormal muscle, or supernumerary ligament, may be predisposed to thoracic outlet syndrome.
- Trauma:
- Trauma, such as injuries or fractures to the neck or clavicle, can lead to anatomical changes that promote compression of nerve and vascular structures in the thoracic outlet.
- Muscle Hypertrophy:
- Hypertrophy of the scalene muscles, located in the neck, can lead to compression of nerves and blood vessels across the thoracic outlet.
- Repetitive Activities:
- Certain work or sporting activities that require repetitive movements of the arm and neck may contribute to the development of thoracic outlet syndrome.
- Inappropriate Rib Positioning:
- Inappropriate positioning of the ribs, often linked to postural disorders, can contribute to compression of structures at the thoracic outlet.
- Normal Anatomical Variations:
- Some people may have normal anatomic variations, such as a narrow thoracic outlet, that increase the risk of compression of neurovascular structures.
- Pregnancy :
- In some pregnant women, enlargement of blood vessels and compression from the growing uterus may contribute to thoracic outlet syndrome.
- Genetic Predisposition:
- Some individuals may have a genetic predisposition to develop anatomical abnormalities favoring thoracic outlet syndrome.
Symptoms
Thoracic outlet syndrome can present with a variety of symptoms that result from compression of neurovascular structures at the thoracic outlet. Symptoms can vary from person to person, and their intensity often depends on the severity of the compression. Here are some symptoms commonly associated with thoracic outlet syndrome:
- Pain and Discomfort:
- Pain in the neck, shoulder and arm, often on the side affected by the syndrome. The pain may be described as a burning, tingling, or electric shock sensation.
- Numbness and Tingling:
- Numbness or tingling in the arm, forearm, hand or fingers. It can be intermittent or constant.
- Muscular weakness :
- Muscle weakness in the arm, which may affect the ability to perform simple tasks or lift objects.
- Cold sensations:
- Feeling of cold in the hand and fingers, often associated with reduced blood circulation due to vascular compression.
- Skin Color Changes:
- Changes in skin color, such as cyanosis (blue discoloration) or paleness, due to impaired blood circulation.
- Swelling :
- Swelling of the hand and fingers, resulting from stagnation of blood and lymph.
- Headache :
- Headaches, which may be associated with muscle tension and changes in blood circulation.
- Pressure Sensitivity:
- Increased sensitivity to pressure in the neck and shoulder area.
- Loss of Coordination:
- Loss of coordination or difficulty making precise movements with the hand and fingers.
It is important to note that some symptoms of thoracic outlet syndrome may be exacerbated by specific activities, such as raising the arm or rotating the neck. Symptoms may also be intermittent, occurring during particular activities or specific body positions.
Osteopathic Treatment of Chest Distinction Syndrome
Osteopathic treatment of thoracic outlet syndrome aims to relieve pain, improve blood circulation and treat restrictions in the thoracic region. Osteopaths use a variety of gentle and specific manual techniques to restore balance and mobility to the affected area. Here are some commonly used approaches:
- Myofascial Release:
- Myofascial release techniques aim to release tension and adhesions in the muscles and fascia surrounding the thoracic outlet. This may help reduce compression of neurovascular structures.
- Stretching and Mobilization:
- Stretching and mobilization exercises may be prescribed to improve flexibility and mobility in the thoracic region. This helps reduce muscle tension and promote better posture.
- Release Techniques:
- Release techniques can be used to release muscle tension and trigger points in the scalene muscles and other muscles in the neck and shoulder area.
- Correction Posturale :
- The osteopath may recommend postural adjustments to avoid positions that exacerbate the symptoms of thoracic outlet syndrome. This may involve advice on sitting posture, standing posture and ergonomic adjustments.
- Functional rehabilitation :
- Functional rehabilitation exercises aim to strengthen the stabilizing muscles of the thoracic region, improve muscle coordination, and restore normal function of the arm and hand.
- Education and Advice:
- The osteopath provides educational advice on stress management, ergonomics, and self-management techniques to help the patient minimize the triggers of thoracic outlet syndrome.
Exercises and Rehabilitation for the Thoracic Parade
- Scalene Stretches:
- Position: Sitting or standing.
- Exercise: Gently tilt your head to one side while sliding your hand on the same side down your leg. Hold for 15-30 seconds. Repeat on the other side.
- Pectoral Stretches:
- Position: Standing in a corner of the room.
- Exercise: Place your forearms against the wall at a 90-degree angle to your arms. Take a step forward to stretch your chest. Hold for 15-30 seconds.
- Thoracic Mobilization:
- Position: Kneeling or sitting on a chair.
- Exercise: Place your hands behind your head, elbow open. Gently rotate your chest to one side. Return to center and repeat on the other side.
- Strengthening the Rhomboids:
- Position: Lying on your stomach on the ground.
- Exercise: Raise your torso and arms off the floor by squeezing your shoulder blades together. Hold for a few seconds and go back down. Repeat.
- Strengthening the Trapezoids:
- Position: Sitting or standing.
- Exercise: Raise your shoulders towards your ears, then bring them back as if you want to bring your shoulder blades together. Hold for a few seconds and release.
- Diaphragmatic Breathing Exercises:
- Position: Lying on your back.
- Exercise: Place one hand on your chest and the other on your abdomen. Breathe deeply through your nose, making sure that the hand on your abdomen rises more than the hand on your chest. Exhale slowly through your mouth.
- Strengthening the Abdominal Muscles:
- Position: Lying on your back.
- Exercise: Perform moderate abdominal exercises, such as leg raises or crunches, making sure to maintain a light abdominal contraction to stabilize the thoracic area.
- Postural Balancing Exercises:
- Position : Debout.
- Exercise: Practice single-leg balancing exercises, such as tree yoga, to improve stability and coordination.
Tips for Preventing Chest Distinction Syndrome
- Maintain Good Posture:
- Maintain an upright posture at all times. Make sure your shoulders are aligned with your hips, and your spine forms a straight line.
- Avoid Prolonged Positions:
- Avoid staying in the same position for long periods of time. If you work at a computer, take regular breaks to stretch and change positions.
- Ergonomics at Work:
- Adjust your workspace to promote healthy posture. The desk, chair and computer monitor should be at appropriate heights to avoid unnecessary strain.
- Perform Stretching Exercises:
- Incorporate stretching exercises into your daily routine to keep muscles and joints flexible. Focus particularly on the muscles of the neck, shoulders and thoracic region.
- Muscle Strengthening:
- Strengthen the stabilizing muscles of the thoracic region, such as the rhomboids and trapezius, to support healthy posture.
- Stress Management Techniques:
- Adopt stress management techniques, such as meditation, deep breathing, yoga, or progressive relaxation, to reduce tension in the neck and shoulder area.
- Avoid Repetitive Movements:
- Limit repetitive arm and neck movements that could contribute to compression of structures at the thoracic outlet.
- Maintain a Healthy Weight:
- Maintain a healthy body weight to reduce pressure on the spine and surrounding structures.
- Hydratation Adequate :
- Make sure you stay well hydrated. Adequate hydration promotes healthy intervertebral discs.
- Avoid Heavy Bags:
Osteopathic Case Studies and Successes
- Pain Relief Case:
- A patient presents with severe neck, shoulder, and arm pain associated with muscle weakness. After an osteopathic evaluation, the osteopath identifies joint and muscular restrictions at the thoracic outlet. By using myofascial release techniques and gentle joint manipulations, the osteopath manages to relieve tension, thereby improving mobility and reducing the patient’s pain.
- Mobility Improvement Case:
- An individual presents with significant stiffness in the neck and shoulders, accompanied by frequent numbness in the arm. The osteopath carries out a thorough assessment of posture and movement, identifying restrictions in the thoracic region. Through gentle manipulations and personalized stretching exercises, the patient gradually regains better mobility, thereby reducing stiffness and associated symptoms.
- Stress Management Case:
- A patient presents with symptoms of thoracic outlet syndrome exacerbated by daily stress. The osteopath incorporates relaxation techniques and stress management advice into the treatment plan. By teaching the patient deep breathing methods and relaxation exercises, the osteopath helps reduce muscle tension associated with stress, thus improving thoracic outlet symptoms.
- Postural Rehabilitation Cases:
- An individual has notable postural imbalances, contributing to the development of thoracic outlet syndrome. The osteopath works on postural reeducation by integrating specific exercises aimed at strengthening the stabilizing muscles of the thoracic region and promoting optimal posture. The patient also learns self-management techniques to maintain healthy posture on a daily basis.
- Cases of Improvement in Quality of Life:
- A patient suffers from persistent pain and functional limitations due to thoracic outlet syndrome. Thanks to a personalized osteopathic treatment plan, including gentle manipulations, rehabilitation exercises and prevention advice, the patient sees a significant improvement in their quality of life. Symptom management allows the patient to return to daily activities without excessive limitation.
Frequently asked questions
Q1: What is thoracic outlet syndrome (TDS)?
A: TDS is a condition where the nerves or blood vessels at the thoracic outlet are compressed. This can cause symptoms such as pain, numbness and weakness in the neck, shoulders and arms.
Q2: What are the symptoms of TDS?
A: Common symptoms include neck and shoulder pain, numbness or tingling in the arms, muscle weakness, and sometimes changes in skin color in the affected area.
Q3: How can osteopathy help in the treatment of TDS?
A: Osteopathy aims to improve mobility, release muscular tension and restore structural balance. Osteopaths use gentle manual techniques to relieve compression of nerves and blood vessels.
Q4: Are there any exercises I can do at home to relieve the symptoms of TDS?
A: Yes, gentle stretching and muscle strengthening exercises may be recommended. However, it is crucial to consult a healthcare professional before undertaking any exercise program.
Q5: How long does it typically take to feel improvements with osteopathic treatments for TDS?
A: The answer varies from person to person, but some patients experience relief after a few sessions. The frequency of treatments depends on the severity of the condition.
Q6: How can I prevent the development of TDS?
A: Maintaining good posture, avoiding prolonged positions, practicing muscle strengthening exercises, and managing stress can help prevent TDS.
Q7: When should I see an osteopath for SDT?
A: If you experience symptoms such as persistent pain, numbness or weakness in the neck, shoulders or arms, it is recommended that you see an osteopath for an evaluation.
Q8: Are there any possible complications related to SDT?
A: In some cases, untreated TDS can lead to complications such as muscle atrophy, deep vein thrombosis, or neurological disorders. It is essential to treat the condition appropriately.
Q9: Is osteopathy suitable for everyone with TDS?
A: Each case is unique. Before beginning any treatment, it is recommended to consult a healthcare professional to determine the best approach, taking into account the patient’s overall medical condition.
Q10: Are osteopathic treatments for SDT painful?
A: Osteopathic techniques are generally gentle. The osteopath works in collaboration with the patient to ensure that the treatment is comfortable and adapted to their tolerance.
Cervical rib syndrome
Cervical rib syndrome is a group of symptoms caused by a relatively rare congenital bone malformation condition. This syndrome is characterized by the presence of an additional cervical rib. This is a congenital anomaly found above the normal first rib. It is a congenital anomaly located above the normal first rib.
Anterior scalene syndrome
Scalene anterior syndrome is a defined clinical condition and the result of pressure placed on the parts that make up the brachial plexus and subclavian artery by the scalene anterior, scalene middle, scalene lesser muscles, and the first rib.
Travel, points out that the relaxation points in the main muscles involved, in particular the scalenes, contribute to muscular hypertrophy which is an important cause of compression of the brachial plexus (Travel/, Simons, 1983; Pecina et al., 1991).
Hyperabduction syndrome
Hyperabduction syndrome is characterized by pain extending down the arm, numbness, paresthesias and erythema, with weakness of the hands; it is due to abduction of the arm for a prolonged period (for example, during sleep or due to work activity) which stretches the axillary vessels and the nerves of the brachial plexus.
Costoclavicular syndrome
The mechanisms of neurovascular compression involve
- A downward movement of the clavicle against the first rib, which compromises the neurovascular plexus.
- The tense supraclavicular
- The first rib rises towards/against the clavicle.
- The clavicle lowers and the first rib rises.
Pectoralis minor syndrome
This syndrome is caused by the pectoralis minor being too tight. This muscle is often activated due to the rounded shoulder posture.
First thoracic rib syndrome
This syndrome is often present in those who have the first elevated dorsal rating.

Assessment
- To develop an effective treatment plan to treat thoracic outlet syndrome, it is essential to accurately identify the location of the compression.
- Several orthopedic tests are used.
- These tests reduce the space for potential compression sites and then cause an increase in symptoms or a decrease in the radial pulse at the wrist.
- In some cases, the neurovascular bundle is compressed in several places. This situation is called “ double crush syndrome ”.
The cervical rib
- Some people have an extra rib at level C7.
- This results in symptoms of thoraco-brachial outlet syndrome in about half of people (Mumenthaler, Schliack, 1991).
- The transverse process is often as wide as T1 and the cervical rib then extends beyond the transverse process of C7.
- It usually comes just behind the lateral border of the anterior scalene muscle tendon, often over the prominence of the first rib.
- This narrows the interscalene triangle, causing the vascular bundle to be more or less taut on the cervical rib under tension.
- This contributes to bundle compression, with symptoms varying depending on the amount of compression.
- This rib is identified by radiography and palpation, at the level of the clavicle, as a bulge in the space between the anterior and middle scalenes.

Anterior scalene syndrome
The intrascalene triangle lies in front of the anterior scalene muscle. This attaches proximally to the anterior transverse processes of cervical vertebrae three through six and distally to the scalene tubercle on the medial border of the first rib. Posteriorly, it consists of the middle scalene muscle which attaches proximally to the posterior transverse process of C2 to C7 and distally to the first rib. The brachial pluxus and the subclavian artery pass through this space. The subclavian vein passes anterior to the scalene anterior muscle and is not affected by compression. Narrowing of the triangle by changes in muscles or ribs, or by space-occupying structures, often results in symptoms of brachial plexus and subclavian artery compression (Szabq 1989).

- Scalene trigger points will cause pain in the lower lateral part of the neck radiating to the lateral shoulder and arm (over the biceps and triceps), the upper part of the chest as well as the medial scapular border.
- Trigger points are activated by the
- Lifting and transporting heavy loads
- Excessive use of respiratory muscles
- Paradoxical breathing
- Extreme cough
- Bronchitis
- Pneumonia
- Asthma
- Emphysema
- The specific causes of anterior scalene syndrome are
- Hypertonicity of the anterior or middle scalene
- Anterior or middle scalene trigger points
- Anatomical abnormalities such
- Cervical rib
- C7 wide transverse process
- Extra wide anterior scalene insertion

Syndrome costoclaviculaire
- Costoclavicular syndrome differs from anterior scalene syndrome in that vascular compression plays a greater role (Pecina et al., 1991; Turner et al., 1990).
- The neurovascular bundle, including both the artery and vein of the axillary-subclavian anterior scalene muscle, passes through a space created by the clavicle anteriorly and the first rib posteriorly.
- The size of the space is variable, depending on the position of the shoulder or anatomical abnormalities.
- Abduction of the arm, retraction of the scapula, and elevation of the first rib on inspiration (especially with apical breathing) will cause the space to narrow.
- The subclavius inserts on the underside of the lateral clavicle and on the first medial rib and its costal cartilage.
- The hypertonic subclavius muscle contributes to compression and leads to fixation of the clavicle.
- Additionally, weakness of the trapezius and levator scapula, muscles that suspend the shoulder, causes the shoulder to sag, with the clavicle resting on the first rib (Szabo, 1989).
- Subclavian trigger points refer to the lateral arm, bypassing the elbow and wrist, then continuing along the dorsal and palmar lateral sides of the hand as well as into the thumb, index, and middle fingers.

Cause
- Fracture (especially if it has been poorly fixed)
- Marked bone callus,
- Dropped shoulders
- Chronic respiratory pathologies
- Emphysema
- arthrosis
- Carrying a heavy or hard object on the shoulder
- Hypertrophy and trigger points of the subclavian muscle.
Pectoralis minor syndrome
- The subpectoral space is formed by the clavicle and the pectoralis minor muscle at its insertion at the level of the coracoid process (the distal attachment is made up of the third, fourth and fifth ribs near the costal cartilages).
- At this level, the brachial plexus continues to travel with the axillary artery and vein; when the subclavian artery and vein enter the axillary fossa, their names change to axillary artery and vein.

- The neurovascular bundle enters the axilla under the pectoralis minor muscle.
- When the arm is in maximum extension and abduction (180 degrees), the bundle is stretched and compressed between the pectoralis minor tendon and the coracoid process as well as between the clavicle and the first rib (Figure 68.4).
- The trigger points of the pectoralis minor, referring the pain mainly to the
- Anterior deltoid muscle
- Pectoral region
- Subclavicular region
- Some pain may extend down the medial side of the arm, into the palm and third to fifth fingers
- Symptoms
- Numbness and tingling in the fingers and progresses to the hand.
- If venous damage
- Ischemia and edema of the hand.
- Symptoms similar to Raynaud’s disease may appear in more than a third of people with pectoralis minor syndrome (Pecina et al., 1991)
- Causes
- Arm raised above the head for an extended period during specific activities.
- Paint a ceiling
- Play an instrument like a violin or flute.
- Arm raised above the head for an extended period during specific activities.

Symptoms can sometimes resemble angina
The pain of dorsal outlet syndrome is often confused with that of angina pectoris (discomfort felt in the dorsal region caused by insufficient oxygen to the heart). However, the back pain does not appear when walking, but increases when the arm is raised.
X-ray
- An x-ray of the apical region of the rib cage may be necessary to rule out the possibility of an additional cervical rib. One person in 200 has an additional cervical rib.

The suprapleural membrane, or Sibson’s fascia, is a structure separable from the endothoracic fascia, ribs and parietal pleura. The top of the parietal pleura forms a dome that rises above the first rib anteriorly, so that the lung actually grows into the cervical region. The outer surface of this parietal pleural dome is attached to the suprapleural membrane, making the mechanics of the lung and pleura inseparable from those of the thoracic inlet. The suspensory ligament of the pleural dome consists of bands or fibers that pass from the suprapleural membrane to the first rib, the transverse processes, and the bodies of the lower cervical vertebrae.

In this way, the mechanics of the lung and pleura are also closely linked to those of the lower cervical spine. Indeed, any mediastinal tension can pass through the suspensory ligament of the pleural dome, to the suspensory ligament of the pleural dome, thus connecting the cervical mechanics to those of the internal thorax.
This may be of particular interest in cases of whiplash or thoracic trauma, where internal mediastinal tissue tension manifests as cervicobrachial pain and neurovascular presentations.
Adson maneuver

One of the most common TOS tests
- The examiner locates the pulse.
- He turns his head towards the affected shoulder/test side.
- Then, he asks the patient to bring the head into extension while the therapist externally rotates and extends the patient’s arm.
- The patient is asked to breathe deeply and maintain breathing.
Positive test: Disappearance of pulse.
General rebound procedure
The goal is to find a tissue barrier (by a gentle direct test). Once the direction of greatest resistance is found, this becomes the direction of application of the recoil technique:
- This technique uses breathing and the elastic rebound of tissues.
- To implement the elastic recoil component, move the fabric within the identified barrier (greatest resistance) to the limit of the fabric’s “softness”.
- Maintain this contact with the barrier while the patient breathes in and out.
- At the appropriate time, release the tissue barrier and the tissue will move back in the direction opposite to the resistance.
Thoraco-brachial outlet rebound procedure

- Both hands will create the tissue barrier by moving in opposite directions.
- When the tissues are released, it is important to ensure that the patient’s head or face will not be accidentally struck.
- The occipital hand should not exert pressure on the ear or mandible, nor on the side of the throat.
- It should engage the occiput and use it to pull the cervical spine longitudinally.
- A slight rotation of the head may be necessary, but too much rotation is contraindicated.
- Place a small pillow on the opposite side of the patient’s head to limit this if necessary.
- The contact of the other hand will indirectly engage the suspensory ligament of the pleural dome by engaging the first rib, which will put tension on the pleural dome then the suspensory ligament.
- By avoiding contact with the clavicle, we direct the technique towards the thoracic inlet rather than towards the shoulder girdle.
Therapeutic approach
- After a complete orthopedic examination, perform a postural assessment.
- Release contracted painful tissues with PRT before using direct manipulation techniques.
- Consider first rib mobilization if other indirect tissue manipulations have failed.
- Consider ordering an x-ray if you suspect an extra rib.
- Evaluate work-related ergonomics as a potential causal factor.
- Ask the patient to take stress reduction measures to reduce the things that trigger somatic stress.
- Consider the use of neural silk once painful contracted tissues are released.
- Myofascial massage of the cervical and shoulder musculature can complement PRT as long as it does not cause reflex muscle spasm.
- Strengthening the shoulder girdle, upper limbs and cervical muscles must focus on acquiring postural endurance.
Recommendation
- Proper posture
- Correction of rounded shoulders
- Maintain a healthy weight
- Perform strengthening exercises
- Avoid lifting heavy objects
- Avoid carrying heavy bags on your shoulders
- Avoid doing repetitive movements
- Stop smoking to reduce coughing
- Avoid lying on the injured side
- Do not lift heavy loads
Muscle to treat
- Anterior and middle scalenes
- Pectoralis minor
- Sub-keyboard
- Sternocleidomastoïde
- Shoulder lifter
- The acromioclavicular joint
- Upper trapezius
- Serrated front
- Rhomboids
References
- Park JY, Oh KS, Yoo HY, Lee JG. Case report: Thoracic outlet syndrome in an elite archer in full-draw position. Clin Orthop Relat Res. 2013 Sep;471(9):3056-60. [PMC free article] [PubMed]
- Levine NA, Rigby BR. Thoracic Outlet Syndrome: Biomechanical and Exercise Considerations. Healthcare (Basel). 2018 Jun 19;6(2) [PMC free article] [PubMed]
- Jones MR, Prabhakar A, Viswanath O, Urits I, Green JB, Kendrick JB, Brunk AJ, Eng MR, Orhurhu V, Cornett EM, Kaye AD. Thoracic Outlet Syndrome: A Comprehensive Review of Pathophysiology, Diagnosis, and Treatment. Pain Ther. 2019 Jun;8(1):5-18. [PMC free article] [PubMed]
- Hussain MA, Aljabri B, Al-Omran M. Vascular Thoracic Outlet Syndrome. Semin Thorac Cardiovasc Surg. 2016 Spring;28(1):151-7. [PubMed]
- Stewman C, Vitanzo PC, Harwood MI. Neurologic thoracic outlet syndrome: summarizing a complex history and evolution. Curr Sports Med Rep. 2014 Mar-Apr;13(2):100-6. [PubMed]
- Grunebach H, Arnold MW, Lum YW. Thoracic outlet syndrome. Vasc Med. 2015 Oct;20(5):493-5. [PubMed]
- Povlsen S, Povlsen B. Diagnosing Thoracic Outlet Syndrome: Current Approaches and Future Directions. Diagnostics (Basel). 2018 Mar 20;8(1) [PMC free article] [PubMed]
- Kuhn JE, Lebus V GF, Bible JE. Thoracic outlet syndrome. J Am Acad Orthop Surg. 2015 Apr;23(4):222-32. [PubMed]
- Raptis CA, Sridhar S, Thompson RW, Fowler KJ, Bhalla S. Imaging of the Patient with Thoracic Outlet Syndrome. Radiographics. 2016 Jul-Aug;36(4):984-1000. [PubMed]
- Freischlag J, Orion K. Understanding thoracic outlet syndrome. Scientifica (Cairo). 2014;2014:248163. [PMC free article] [PubMed]
- Yunce M, Sharma A, Braunstein E, Streiff MB, Lum YW. A case report on 2 unique presentations of upper extremity deep vein thrombosis. Medicine (Baltimore). 2018 Mar;97(11):e9944. [PMC free article] [PubMed]
- Peek J, Vos CG, Ünlü Ç, van de Pavoordt HDWM, van den Akker PJ, de Vries JPM. Outcome of Surgical Treatment for ThoracicOutletSyndrome: Systematic Review and Meta-Analysis. Ann Vasc Surg. 2017 Apr;40:303-326. [PubMed]
Anatomy
The brachial pluxus consists of nerve roots C5 to C8 and D1 and provides innervation to the entire upper limb. It travels with the subclavian artery between the anterior and medial scalenes (the intrascalene space). The subclavian vein becomes part of the neurovascular bundle as it passes under the clavicle (the costoclavicular space) and travels under the insertion of the pectoralis minor (the subpectoral space) before continuing the along the arm.
What are the types of compression?
- Neurogenic
- Venous
- Arterial
Approximately 95% of cases of thoracic outlet syndrome are neurogenic. Others are rare, but more serious when it affects a vein or artery.

Causes
- Anatomical Anomalies:
- People who are born with anatomical abnormalities, such as an extra rib (cervical rib), abnormal muscle, or supernumerary ligament, may be predisposed to thoracic outlet syndrome.
- Trauma:
- Trauma, such as injuries or fractures to the neck or clavicle, can lead to anatomical changes that promote compression of nerve and vascular structures in the thoracic outlet.
- Muscle Hypertrophy:
- Hypertrophy of the scalene muscles, located in the neck, can lead to compression of nerves and blood vessels across the thoracic outlet.
- Repetitive Activities:
- Certain work or sporting activities that require repetitive movements of the arm and neck may contribute to the development of thoracic outlet syndrome.
- Inappropriate Rib Positioning:
- Inappropriate positioning of the ribs, often linked to postural disorders, can contribute to compression of structures at the thoracic outlet.
- Normal Anatomical Variations:
- Some people may have normal anatomic variations, such as a narrow thoracic outlet, that increase the risk of compression of neurovascular structures.
- Pregnancy :
- In some pregnant women, enlargement of blood vessels and compression from the growing uterus may contribute to thoracic outlet syndrome.
- Genetic Predisposition:
- Some individuals may have a genetic predisposition to develop anatomical abnormalities favoring thoracic outlet syndrome.
Symptoms
Thoracic outlet syndrome can present with a variety of symptoms that result from compression of neurovascular structures at the thoracic outlet. Symptoms can vary from person to person, and their intensity often depends on the severity of the compression. Here are some symptoms commonly associated with thoracic outlet syndrome:
- Pain and Discomfort:
- Pain in the neck, shoulder and arm, often on the side affected by the syndrome. The pain may be described as a burning, tingling, or electric shock sensation.
- Numbness and Tingling:
- Numbness or tingling in the arm, forearm, hand or fingers. It can be intermittent or constant.
- Muscular weakness :
- Muscle weakness in the arm, which may affect the ability to perform simple tasks or lift objects.
- Cold sensations:
- Feeling of cold in the hand and fingers, often associated with reduced blood circulation due to vascular compression.
- Skin Color Changes:
- Changes in skin color, such as cyanosis (blue discoloration) or paleness, due to impaired blood circulation.
- Swelling :
- Swelling of the hand and fingers, resulting from stagnation of blood and lymph.
- Headache :
- Headaches, which may be associated with muscle tension and changes in blood circulation.
- Pressure Sensitivity:
- Increased sensitivity to pressure in the neck and shoulder area.
- Loss of Coordination:
- Loss of coordination or difficulty making precise movements with the hand and fingers.
It is important to note that some symptoms of thoracic outlet syndrome may be exacerbated by specific activities, such as raising the arm or rotating the neck. Symptoms may also be intermittent, occurring during particular activities or specific body positions.
Osteopathic Treatment of Chest Distinction Syndrome
Osteopathic treatment of thoracic outlet syndrome aims to relieve pain, improve blood circulation and treat restrictions in the thoracic region. Osteopaths use a variety of gentle and specific manual techniques to restore balance and mobility to the affected area. Here are some commonly used approaches:
- Myofascial Release:
- Myofascial release techniques aim to release tension and adhesions in the muscles and fascia surrounding the thoracic outlet. This may help reduce compression of neurovascular structures.
- Stretching and Mobilization:
- Stretching and mobilization exercises may be prescribed to improve flexibility and mobility in the thoracic region. This helps reduce muscle tension and promote better posture.
- Release Techniques:
- Release techniques can be used to release muscle tension and trigger points in the scalene muscles and other muscles in the neck and shoulder area.
- Correction Posturale :
- The osteopath may recommend postural adjustments to avoid positions that exacerbate the symptoms of thoracic outlet syndrome. This may involve advice on sitting posture, standing posture and ergonomic adjustments.
- Functional rehabilitation :
- Functional rehabilitation exercises aim to strengthen the stabilizing muscles of the thoracic region, improve muscle coordination, and restore normal function of the arm and hand.
- Education and Advice:
- The osteopath provides educational advice on stress management, ergonomics, and self-management techniques to help the patient minimize the triggers of thoracic outlet syndrome.
Exercises and Rehabilitation for the Thoracic Parade
- Scalene Stretches:
- Position: Sitting or standing.
- Exercise: Gently tilt your head to one side while sliding your hand on the same side down your leg. Hold for 15-30 seconds. Repeat on the other side.
- Pectoral Stretches:
- Position: Standing in a corner of the room.
- Exercise: Place your forearms against the wall at a 90-degree angle to your arms. Take a step forward to stretch your chest. Hold for 15-30 seconds.
- Thoracic Mobilization:
- Position: Kneeling or sitting on a chair.
- Exercise: Place your hands behind your head, elbow open. Gently rotate your chest to one side. Return to center and repeat on the other side.
- Strengthening the Rhomboids:
- Position: Lying on your stomach on the ground.
- Exercise: Raise your torso and arms off the floor by squeezing your shoulder blades together. Hold for a few seconds and go back down. Repeat.
- Strengthening the Trapezoids:
- Position: Sitting or standing.
- Exercise: Raise your shoulders towards your ears, then bring them back as if you want to bring your shoulder blades together. Hold for a few seconds and release.
- Diaphragmatic Breathing Exercises:
- Position: Lying on your back.
- Exercise: Place one hand on your chest and the other on your abdomen. Breathe deeply through your nose, making sure that the hand on your abdomen rises more than the hand on your chest. Exhale slowly through your mouth.
- Strengthening the Abdominal Muscles:
- Position: Lying on your back.
- Exercise: Perform moderate abdominal exercises, such as leg raises or crunches, making sure to maintain a light abdominal contraction to stabilize the thoracic area.
- Postural Balancing Exercises:
- Position : Debout.
- Exercise: Practice single-leg balancing exercises, such as tree yoga, to improve stability and coordination.
Tips for Preventing Chest Distinction Syndrome
- Maintain Good Posture:
- Maintain an upright posture at all times. Make sure your shoulders are aligned with your hips, and your spine forms a straight line.
- Avoid Prolonged Positions:
- Avoid staying in the same position for long periods of time. If you work at a computer, take regular breaks to stretch and change positions.
- Ergonomics at Work:
- Adjust your workspace to promote healthy posture. The desk, chair and computer monitor should be at appropriate heights to avoid unnecessary strain.
- Perform Stretching Exercises:
- Incorporate stretching exercises into your daily routine to keep muscles and joints flexible. Focus particularly on the muscles of the neck, shoulders and thoracic region.
- Muscle Strengthening:
- Strengthen the stabilizing muscles of the thoracic region, such as the rhomboids and trapezius, to support healthy posture.
- Stress Management Techniques:
- Adopt stress management techniques, such as meditation, deep breathing, yoga, or progressive relaxation, to reduce tension in the neck and shoulder area.
- Avoid Repetitive Movements:
- Limit repetitive arm and neck movements that could contribute to compression of structures at the thoracic outlet.
- Maintain a Healthy Weight:
- Maintain a healthy body weight to reduce pressure on the spine and surrounding structures.
- Hydratation Adequate :
- Make sure you stay well hydrated. Adequate hydration promotes healthy intervertebral discs.
- Avoid Heavy Bags:
Osteopathic Case Studies and Successes
- Pain Relief Case:
- A patient presents with severe neck, shoulder, and arm pain associated with muscle weakness. After an osteopathic evaluation, the osteopath identifies joint and muscular restrictions at the thoracic outlet. By using myofascial release techniques and gentle joint manipulations, the osteopath manages to relieve tension, thereby improving mobility and reducing the patient’s pain.
- Mobility Improvement Case:
- An individual presents with significant stiffness in the neck and shoulders, accompanied by frequent numbness in the arm. The osteopath carries out a thorough assessment of posture and movement, identifying restrictions in the thoracic region. Through gentle manipulations and personalized stretching exercises, the patient gradually regains better mobility, thereby reducing stiffness and associated symptoms.
- Stress Management Case:
- A patient presents with symptoms of thoracic outlet syndrome exacerbated by daily stress. The osteopath incorporates relaxation techniques and stress management advice into the treatment plan. By teaching the patient deep breathing methods and relaxation exercises, the osteopath helps reduce muscle tension associated with stress, thus improving thoracic outlet symptoms.
- Postural Rehabilitation Cases:
- An individual has notable postural imbalances, contributing to the development of thoracic outlet syndrome. The osteopath works on postural reeducation by integrating specific exercises aimed at strengthening the stabilizing muscles of the thoracic region and promoting optimal posture. The patient also learns self-management techniques to maintain healthy posture on a daily basis.
- Cases of Improvement in Quality of Life:
- A patient suffers from persistent pain and functional limitations due to thoracic outlet syndrome. Thanks to a personalized osteopathic treatment plan, including gentle manipulations, rehabilitation exercises and prevention advice, the patient sees a significant improvement in their quality of life. Symptom management allows the patient to return to daily activities without excessive limitation.
Frequently asked questions
Q1: What is thoracic outlet syndrome (TDS)?
A: TDS is a condition where the nerves or blood vessels at the thoracic outlet are compressed. This can cause symptoms such as pain, numbness and weakness in the neck, shoulders and arms.
Q2: What are the symptoms of TDS?
A: Common symptoms include neck and shoulder pain, numbness or tingling in the arms, muscle weakness, and sometimes changes in skin color in the affected area.
Q3: How can osteopathy help in the treatment of TDS?
A: Osteopathy aims to improve mobility, release muscular tension and restore structural balance. Osteopaths use gentle manual techniques to relieve compression of nerves and blood vessels.
Q4: Are there any exercises I can do at home to relieve the symptoms of TDS?
A: Yes, gentle stretching and muscle strengthening exercises may be recommended. However, it is crucial to consult a healthcare professional before undertaking any exercise program.
Q5: How long does it typically take to feel improvements with osteopathic treatments for TDS?
A: The answer varies from person to person, but some patients experience relief after a few sessions. The frequency of treatments depends on the severity of the condition.
Q6: How can I prevent the development of TDS?
A: Maintaining good posture, avoiding prolonged positions, practicing muscle strengthening exercises, and managing stress can help prevent TDS.
Q7: When should I see an osteopath for SDT?
A: If you experience symptoms such as persistent pain, numbness or weakness in the neck, shoulders or arms, it is recommended that you see an osteopath for an evaluation.
Q8: Are there any possible complications related to SDT?
A: In some cases, untreated TDS can lead to complications such as muscle atrophy, deep vein thrombosis, or neurological disorders. It is essential to treat the condition appropriately.
Q9: Is osteopathy suitable for everyone with TDS?
A: Each case is unique. Before beginning any treatment, it is recommended to consult a healthcare professional to determine the best approach, taking into account the patient’s overall medical condition.
Q10: Are osteopathic treatments for SDT painful?
A: Osteopathic techniques are generally gentle. The osteopath works in collaboration with the patient to ensure that the treatment is comfortable and adapted to their tolerance.
Cervical rib syndrome
Cervical rib syndrome is a group of symptoms caused by a relatively rare congenital bone malformation condition. This syndrome is characterized by the presence of an additional cervical rib. This is a congenital anomaly found above the normal first rib. It is a congenital anomaly located above the normal first rib.
Anterior scalene syndrome
Scalene anterior syndrome is a defined clinical condition and the result of pressure placed on the parts that make up the brachial plexus and subclavian artery by the scalene anterior, scalene middle, scalene lesser muscles, and the first rib.
Travel, points out that the relaxation points in the main muscles involved, in particular the scalenes, contribute to muscular hypertrophy which is an important cause of compression of the brachial plexus (Travel/, Simons, 1983; Pecina et al., 1991).
Hyperabduction syndrome
Hyperabduction syndrome is characterized by pain extending down the arm, numbness, paresthesias and erythema, with weakness of the hands; it is due to abduction of the arm for a prolonged period (for example, during sleep or due to work activity) which stretches the axillary vessels and the nerves of the brachial plexus.
Costoclavicular syndrome
The mechanisms of neurovascular compression involve
- A downward movement of the clavicle against the first rib, which compromises the neurovascular plexus.
- The tense supraclavicular
- The first rib rises towards/against the clavicle.
- The clavicle lowers and the first rib rises.
Pectoralis minor syndrome
This syndrome is caused by the pectoralis minor being too tight. This muscle is often activated due to the rounded shoulder posture.
First thoracic rib syndrome
This syndrome is often present in those who have the first elevated dorsal rating.

Assessment
- To develop an effective treatment plan to treat thoracic outlet syndrome, it is essential to accurately identify the location of the compression.
- Several orthopedic tests are used.
- These tests reduce the space for potential compression sites and then cause an increase in symptoms or a decrease in the radial pulse at the wrist.
- In some cases, the neurovascular bundle is compressed in several places. This situation is called “ double crush syndrome ”.
The cervical rib
- Some people have an extra rib at level C7.
- This results in symptoms of thoraco-brachial outlet syndrome in about half of people (Mumenthaler, Schliack, 1991).
- The transverse process is often as wide as T1 and the cervical rib then extends beyond the transverse process of C7.
- It usually comes just behind the lateral border of the anterior scalene muscle tendon, often over the prominence of the first rib.
- This narrows the interscalene triangle, causing the vascular bundle to be more or less taut on the cervical rib under tension.
- This contributes to bundle compression, with symptoms varying depending on the amount of compression.
- This rib is identified by radiography and palpation, at the level of the clavicle, as a bulge in the space between the anterior and middle scalenes.

Anterior scalene syndrome
The intrascalene triangle lies in front of the anterior scalene muscle. This attaches proximally to the anterior transverse processes of cervical vertebrae three through six and distally to the scalene tubercle on the medial border of the first rib. Posteriorly, it consists of the middle scalene muscle which attaches proximally to the posterior transverse process of C2 to C7 and distally to the first rib. The brachial pluxus and the subclavian artery pass through this space. The subclavian vein passes anterior to the scalene anterior muscle and is not affected by compression. Narrowing of the triangle by changes in muscles or ribs, or by space-occupying structures, often results in symptoms of brachial plexus and subclavian artery compression (Szabq 1989).

- Scalene trigger points will cause pain in the lower lateral part of the neck radiating to the lateral shoulder and arm (over the biceps and triceps), the upper part of the chest as well as the medial scapular border.
- Trigger points are activated by the
- Lifting and transporting heavy loads
- Excessive use of respiratory muscles
- Paradoxical breathing
- Extreme cough
- Bronchitis
- Pneumonia
- Asthma
- Emphysema
- The specific causes of anterior scalene syndrome are
- Hypertonicity of the anterior or middle scalene
- Anterior or middle scalene trigger points
- Anatomical abnormalities such
- Cervical rib
- C7 wide transverse process
- Extra wide anterior scalene insertion

Syndrome costoclaviculaire
- Costoclavicular syndrome differs from anterior scalene syndrome in that vascular compression plays a greater role (Pecina et al., 1991; Turner et al., 1990).
- The neurovascular bundle, including both the artery and vein of the axillary-subclavian anterior scalene muscle, passes through a space created by the clavicle anteriorly and the first rib posteriorly.
- The size of the space is variable, depending on the position of the shoulder or anatomical abnormalities.
- Abduction of the arm, retraction of the scapula, and elevation of the first rib on inspiration (especially with apical breathing) will cause the space to narrow.
- The subclavius inserts on the underside of the lateral clavicle and on the first medial rib and its costal cartilage.
- The hypertonic subclavius muscle contributes to compression and leads to fixation of the clavicle.
- Additionally, weakness of the trapezius and levator scapula, muscles that suspend the shoulder, causes the shoulder to sag, with the clavicle resting on the first rib (Szabo, 1989).
- Subclavian trigger points refer to the lateral arm, bypassing the elbow and wrist, then continuing along the dorsal and palmar lateral sides of the hand as well as into the thumb, index, and middle fingers.

Cause
- Fracture (especially if it has been poorly fixed)
- Marked bone callus,
- Dropped shoulders
- Chronic respiratory pathologies
- Emphysema
- arthrosis
- Carrying a heavy or hard object on the shoulder
- Hypertrophy and trigger points of the subclavian muscle.
Pectoralis minor syndrome
- The subpectoral space is formed by the clavicle and the pectoralis minor muscle at its insertion at the level of the coracoid process (the distal attachment is made up of the third, fourth and fifth ribs near the costal cartilages).
- At this level, the brachial plexus continues to travel with the axillary artery and vein; when the subclavian artery and vein enter the axillary fossa, their names change to axillary artery and vein.

- The neurovascular bundle enters the axilla under the pectoralis minor muscle.
- When the arm is in maximum extension and abduction (180 degrees), the bundle is stretched and compressed between the pectoralis minor tendon and the coracoid process as well as between the clavicle and the first rib (Figure 68.4).
- The trigger points of the pectoralis minor, referring the pain mainly to the
- Anterior deltoid muscle
- Pectoral region
- Subclavicular region
- Some pain may extend down the medial side of the arm, into the palm and third to fifth fingers
- Symptoms
- Numbness and tingling in the fingers and progresses to the hand.
- If venous damage
- Ischemia and edema of the hand.
- Symptoms similar to Raynaud’s disease may appear in more than a third of people with pectoralis minor syndrome (Pecina et al., 1991)
- Causes
- Arm raised above the head for an extended period during specific activities.
- Paint a ceiling
- Play an instrument like a violin or flute.
- Arm raised above the head for an extended period during specific activities.

Symptoms can sometimes resemble angina
The pain of dorsal outlet syndrome is often confused with that of angina pectoris (discomfort felt in the dorsal region caused by insufficient oxygen to the heart). However, the back pain does not appear when walking, but increases when the arm is raised.
X-ray
- An x-ray of the apical region of the rib cage may be necessary to rule out the possibility of an additional cervical rib. One person in 200 has an additional cervical rib.

The suprapleural membrane, or Sibson’s fascia, is a structure separable from the endothoracic fascia, ribs and parietal pleura. The top of the parietal pleura forms a dome that rises above the first rib anteriorly, so that the lung actually grows into the cervical region. The outer surface of this parietal pleural dome is attached to the suprapleural membrane, making the mechanics of the lung and pleura inseparable from those of the thoracic inlet. The suspensory ligament of the pleural dome consists of bands or fibers that pass from the suprapleural membrane to the first rib, the transverse processes, and the bodies of the lower cervical vertebrae.

In this way, the mechanics of the lung and pleura are also closely linked to those of the lower cervical spine. Indeed, any mediastinal tension can pass through the suspensory ligament of the pleural dome, to the suspensory ligament of the pleural dome, thus connecting the cervical mechanics to those of the internal thorax.
This may be of particular interest in cases of whiplash or thoracic trauma, where internal mediastinal tissue tension manifests as cervicobrachial pain and neurovascular presentations.
Adson maneuver

One of the most common TOS tests
- The examiner locates the pulse.
- He turns his head towards the affected shoulder/test side.
- Then, he asks the patient to bring the head into extension while the therapist externally rotates and extends the patient’s arm.
- The patient is asked to breathe deeply and maintain breathing.
Positive test: Disappearance of pulse.
General rebound procedure
The goal is to find a tissue barrier (by a gentle direct test). Once the direction of greatest resistance is found, this becomes the direction of application of the recoil technique:
- This technique uses breathing and the elastic rebound of tissues.
- To implement the elastic recoil component, move the fabric within the identified barrier (greatest resistance) to the limit of the fabric’s “softness”.
- Maintain this contact with the barrier while the patient breathes in and out.
- At the appropriate time, release the tissue barrier and the tissue will move back in the direction opposite to the resistance.
Thoraco-brachial outlet rebound procedure

- Both hands will create the tissue barrier by moving in opposite directions.
- When the tissues are released, it is important to ensure that the patient’s head or face will not be accidentally struck.
- The occipital hand should not exert pressure on the ear or mandible, nor on the side of the throat.
- It should engage the occiput and use it to pull the cervical spine longitudinally.
- A slight rotation of the head may be necessary, but too much rotation is contraindicated.
- Place a small pillow on the opposite side of the patient’s head to limit this if necessary.
- The contact of the other hand will indirectly engage the suspensory ligament of the pleural dome by engaging the first rib, which will put tension on the pleural dome then the suspensory ligament.
- By avoiding contact with the clavicle, we direct the technique towards the thoracic inlet rather than towards the shoulder girdle.
Therapeutic approach
- After a complete orthopedic examination, perform a postural assessment.
- Release contracted painful tissues with PRT before using direct manipulation techniques.
- Consider first rib mobilization if other indirect tissue manipulations have failed.
- Consider ordering an x-ray if you suspect an extra rib.
- Evaluate work-related ergonomics as a potential causal factor.
- Ask the patient to take stress reduction measures to reduce the things that trigger somatic stress.
- Consider the use of neural silk once painful contracted tissues are released.
- Myofascial massage of the cervical and shoulder musculature can complement PRT as long as it does not cause reflex muscle spasm.
- Strengthening the shoulder girdle, upper limbs and cervical muscles must focus on acquiring postural endurance.
Recommendation
- Proper posture
- Correction of rounded shoulders
- Maintain a healthy weight
- Perform strengthening exercises
- Avoid lifting heavy objects
- Avoid carrying heavy bags on your shoulders
- Avoid doing repetitive movements
- Stop smoking to reduce coughing
- Avoid lying on the injured side
- Do not lift heavy loads
Muscle to treat
- Anterior and middle scalenes
- Pectoralis minor
- Sub-keyboard
- Sternocleidomastoïde
- Shoulder lifter
- The acromioclavicular joint
- Upper trapezius
- Serrated front
- Rhomboids
References
- Park JY, Oh KS, Yoo HY, Lee JG. Case report: Thoracic outlet syndrome in an elite archer in full-draw position. Clin Orthop Relat Res. 2013 Sep;471(9):3056-60. [PMC free article] [PubMed]
- Levine NA, Rigby BR. Thoracic Outlet Syndrome: Biomechanical and Exercise Considerations. Healthcare (Basel). 2018 Jun 19;6(2) [PMC free article] [PubMed]
- Jones MR, Prabhakar A, Viswanath O, Urits I, Green JB, Kendrick JB, Brunk AJ, Eng MR, Orhurhu V, Cornett EM, Kaye AD. Thoracic Outlet Syndrome: A Comprehensive Review of Pathophysiology, Diagnosis, and Treatment. Pain Ther. 2019 Jun;8(1):5-18. [PMC free article] [PubMed]
- Hussain MA, Aljabri B, Al-Omran M. Vascular Thoracic Outlet Syndrome. Semin Thorac Cardiovasc Surg. 2016 Spring;28(1):151-7. [PubMed]
- Stewman C, Vitanzo PC, Harwood MI. Neurologic thoracic outlet syndrome: summarizing a complex history and evolution. Curr Sports Med Rep. 2014 Mar-Apr;13(2):100-6. [PubMed]
- Grunebach H, Arnold MW, Lum YW. Thoracic outlet syndrome. Vasc Med. 2015 Oct;20(5):493-5. [PubMed]
- Povlsen S, Povlsen B. Diagnosing Thoracic Outlet Syndrome: Current Approaches and Future Directions. Diagnostics (Basel). 2018 Mar 20;8(1) [PMC free article] [PubMed]
- Kuhn JE, Lebus V GF, Bible JE. Thoracic outlet syndrome. J Am Acad Orthop Surg. 2015 Apr;23(4):222-32. [PubMed]
- Raptis CA, Sridhar S, Thompson RW, Fowler KJ, Bhalla S. Imaging of the Patient with Thoracic Outlet Syndrome. Radiographics. 2016 Jul-Aug;36(4):984-1000. [PubMed]
- Freischlag J, Orion K. Understanding thoracic outlet syndrome. Scientifica (Cairo). 2014;2014:248163. [PMC free article] [PubMed]
- Yunce M, Sharma A, Braunstein E, Streiff MB, Lum YW. A case report on 2 unique presentations of upper extremity deep vein thrombosis. Medicine (Baltimore). 2018 Mar;97(11):e9944. [PMC free article] [PubMed]
- Peek J, Vos CG, Ünlü Ç, van de Pavoordt HDWM, van den Akker PJ, de Vries JPM. Outcome of Surgical Treatment for ThoracicOutletSyndrome: Systematic Review and Meta-Analysis. Ann Vasc Surg. 2017 Apr;40:303-326. [PubMed]