Why the Big Toe Matters: Understanding Its Role in Movement and Health
The human foot is a complex structure that plays a crucial role in mobility and overall quality of life. At the forefront of this structure lies the big toe, or the hallux, which is vital for balance and proper gait mechanics. Two conditions that can severely impact the function of the big toe joint are Hallux Limitus and Hallux Rigidus. While they share a connection in their progressive nature, understanding the differences, causes, and impacts of these conditions is essential for managing symptoms and preventing long-term complications.
Hallux Limitus vs. Hallux Rigidus: What’s the Difference and Why It Matters
Hallux Limitus and Hallux Rigidus represent two stages of a degenerative process affecting the metatarsophalangeal (MTP) joint of the big toe.
Hallux Limitus refers to a reduced range of motion in the big toe, particularly when trying to bend the toe upward. This limited movement can be painful and restrict daily activities such as walking, running, or even standing for extended periods. The condition often starts subtly, with stiffness or mild discomfort, and can gradually worsen if left untreated.
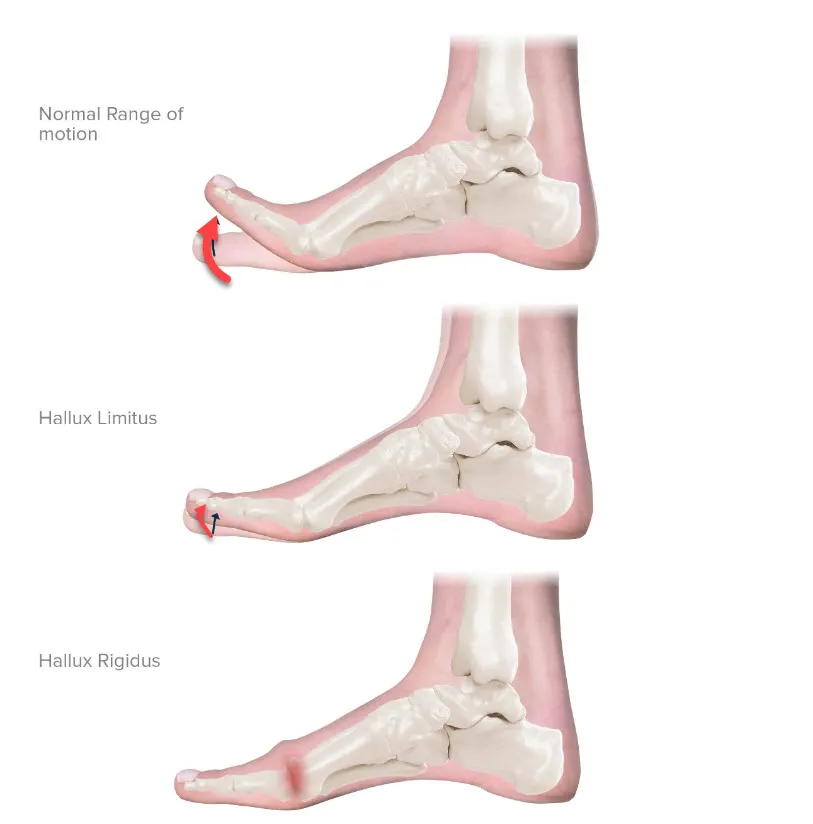
Normal Range of Motion: The first diagram shows a foot with the big toe bending upward freely. This indicates a healthy range of motion, allowing the toe to move without restriction. This flexibility is crucial for proper foot mechanics during walking, running, and other activities.
Hallux Limitus: The second illustration represents a condition called hallux limitus, where the range of motion of the big toe is limited. The toe cannot bend upward as freely as it should, causing discomfort and pain, especially during activities that require toe extension. This stiffness is often due to osteoarthritis or other degenerative changes in the joint.
Hallux Rigidus: The third diagram depicts a more advanced stage called hallux rigidus. Here, the big toe joint is severely restricted, almost entirely immobile. This condition results from progressive joint deterioration, often leading to significant pain and swelling. Patients with hallux rigidus may have difficulty performing everyday activities and may require surgical intervention.
Hallux Rigidus, on the other hand, is the more advanced stage of this degenerative condition, where the MTP joint becomes almost entirely immobile. The term “rigidus” emphasizes the severity of stiffness in the joint, and at this stage, individuals often experience chronic pain, swelling, and significant difficulty with movement. Hallux Rigidus can be debilitating, impacting a person’s ability to perform everyday tasks and enjoy an active lifestyle. While both conditions share a progressive nature, early recognition and intervention can make a significant difference in managing symptoms and slowing down joint deterioration.
The root cause of these conditions is often linked to osteoarthritis, a wear-and-tear type of arthritis that leads to cartilage degradation. However, there are other contributing factors, such as foot structure abnormalities, previous injuries to the big toe, inflammatory diseases, and even genetic predispositions. Both Hallux Limitus and Hallux Rigidus can affect anyone, but they are more commonly seen in middle-aged and older adults. With aging populations and lifestyle factors contributing to joint stress, understanding these conditions is becoming increasingly important.
Catch It Early: The Key to Preventing Big Toe Degeneration
The significance of early diagnosis in cases of Hallux Limitus and Hallux Rigidus cannot be overstated. When symptoms first present, they are often mild and can be mistaken for temporary discomfort or attributed to ill-fitting footwear. However, the underlying problem is progressive, and delaying intervention only allows the condition to worsen. Identifying Hallux Limitus early gives healthcare professionals an opportunity to implement conservative treatment strategies that can effectively manage pain, improve mobility, and prevent the condition from evolving into Hallux Rigidus.
Early diagnosis involves a thorough clinical assessment and imaging studies, such as X-rays or MRIs, to evaluate the extent of joint damage. Recognizing the problem in its initial stages opens the door to a range of non-surgical treatments. These may include exercises to improve joint function, custom orthotics to redistribute pressure, and lifestyle changes that promote joint health. Additionally, anti-inflammatory medications or steroid injections can help manage pain and inflammation. By taking proactive measures, patients can maintain a reasonable quality of life and minimize disruptions caused by the condition.
When Hallux Limitus progresses to Hallux Rigidus, treatment options become more limited, often necessitating surgical intervention. Procedures like cheilectomy (removal of bone spurs) or arthrodesis (joint fusion) may be required to alleviate pain and restore some level of functionality. Surgery can be effective but comes with recovery challenges and potential complications. Therefore, avoiding or delaying the need for surgical solutions by prioritizing early intervention is ideal.
Furthermore, managing these conditions early can have broader health implications. When foot mechanics are compromised, it can lead to secondary issues, such as knee, hip, or lower back pain. These complications arise from the body’s natural tendency to adjust posture and gait to compensate for joint pain and immobility. The ripple effect of untreated Hallux Limitus or Hallux Rigidus can ultimately affect a person’s entire musculoskeletal system, leading to a downward spiral of mobility issues and chronic discomfort.
Another key aspect of early diagnosis is the psychological impact of foot pain and restricted movement. Chronic conditions often lead to frustration, anxiety, and reduced physical activity, which can adversely affect overall well-being. Addressing these issues in their early stages helps preserve not only physical function but also mental and emotional health.
Inside the Big Toe: Anatomy of the MTP Joint Explained
Structure and Function
The big toe joint, known scientifically as the metatarsophalangeal (MTP) joint, is a vital component of foot anatomy. It connects the first metatarsal bone in the foot to the proximal phalanx, which is the first bone in the big toe. This joint plays an essential role in providing stability and facilitating movement. Structurally, the MTP joint is a synovial joint, meaning it is encapsulated in a protective layer of synovial fluid that lubricates and nourishes the cartilage. This fluid ensures smooth motion and reduces friction between the bones, allowing the joint to function efficiently.
The MTP joint consists of several key components, each contributing to its proper operation. The bones in the joint are covered by a layer of articular cartilage, a smooth and resilient tissue that cushions the ends of the bones and absorbs impact. This cartilage is critical for shock absorption, especially during high-impact activities like running or jumping. The joint is stabilized by a network of ligaments, which are strong bands of tissue that hold the bones together and prevent excessive movement. Additionally, tendons surround the joint, connecting muscles from the lower leg and foot to the bones, enabling the big toe to flex and extend.
Beneath the joint lies a pair of sesamoid bones, which are small, pea-shaped bones embedded within the tendons that run underneath the big toe. These sesamoids act as pulleys, increasing the leverage of the tendons and aiding in efficient toe movement. They also help distribute the weight and pressure placed on the ball of the foot. Together, these structures create a stable yet flexible joint that is crucial for efficient foot mechanics and overall lower limb function.
The big toe joint is subject to significant stress during daily activities. Every time the foot pushes off the ground, the MTP joint must bear the body’s weight and provide the power necessary for forward movement. This joint’s continuous use and the impact it endures over time make it prone to degeneration, injury, and conditions like Hallux Limitus and Hallux Rigidus.
Power and Stability: How the Big Toe Guides Your Gait
The big toe plays a pivotal role in facilitating movement and maintaining balance. As humans walk or run, a sequence of actions takes place, with the big toe being central to this complex process. During the gait cycle, which is the pattern of movement while walking, the big toe helps in the final push-off phase known as the “toe-off.” This phase is critical for propelling the body forward. When the foot lifts off the ground, the big toe bears a significant portion of the body’s weight, working in tandem with the calf muscles to provide the necessary thrust and speed.


The big toe also acts as a stabilizer. During walking, it provides a stable base as the body shifts its weight from one leg to the other. This stabilization prevents side-to-side wobbling and ensures a smooth, coordinated stride. The alignment and health of the big toe joint are therefore crucial for efficient weight distribution and balance, affecting not only the foot but the entire lower extremity. Any impairment in the big toe’s function, such as stiffness or immobility caused by Hallux Limitus or Hallux Rigidus, can disrupt these movements, leading to compensatory changes in the gait. These changes can have a domino effect, placing extra stress on other joints, including the ankles, knees, hips, and lower back.
Furthermore, the big toe contributes to posture and equilibrium. When standing still, the toe helps the foot grip the ground and maintain balance. This role becomes even more critical during activities that require shifting weight or changing direction, such as dancing or playing sports. The big toe’s strength and flexibility are essential for athletes, as they allow for rapid acceleration, deceleration, and side-to-side movement. In essence, the big toe is a small but mighty structure that plays an outsized role in human mobility and overall physical performance. Any dysfunction in this area can have far-reaching effects, emphasizing the importance of maintaining its health and flexibility.
Understanding Hallux Limitus: When Toe Motion Starts to Fade
Definition and Characteristics
Hallux Rigidus represents the more advanced stage of the degenerative process that begins with Hallux Limitus. It is a form of osteoarthritis in which the metatarsophalangeal (MTP) joint of the big toe becomes almost entirely immobile and rigid. The term “rigidus” emphasizes the severity of stiffness, where the joint’s range of motion is drastically reduced, causing significant functional impairment. At this stage, the big toe cannot bend upward at all, or can only do so with extreme pain. This rigidity severely impacts an individual’s ability to walk, run, or perform any activity that requires toe movement.
The progression from Hallux Limitus to Hallux Rigidus is marked by a gradual worsening of symptoms. The protective cartilage that cushions the MTP joint continues to wear down, and bone spurs, or osteophytes, become more pronounced. These spurs can cause additional pain and inflammation, making the joint feel swollen, warm, and tender. The joint may also appear visibly enlarged or deformed. This deformation not only creates aesthetic concerns but also poses challenges in finding comfortable footwear. Patients with Hallux Rigidus often experience difficulty wearing regular shoes, as pressure from the shoe exacerbates pain and discomfort.
Progression from Hallux Limitus
The progression from Hallux Limitus to Hallux Rigidus typically occurs over time, especially if early interventions are not implemented. As the cartilage in the joint deteriorates further, the body tries to stabilize the joint by forming additional bone. This reaction results in the development of bone spurs, which restrict motion and worsen the condition. The ongoing cycle of cartilage loss, bone spur formation, and inflammation leads to the hallmark stiffness of Hallux Rigidus. Once the joint becomes immobile, it is nearly impossible to regain movement without surgical intervention.
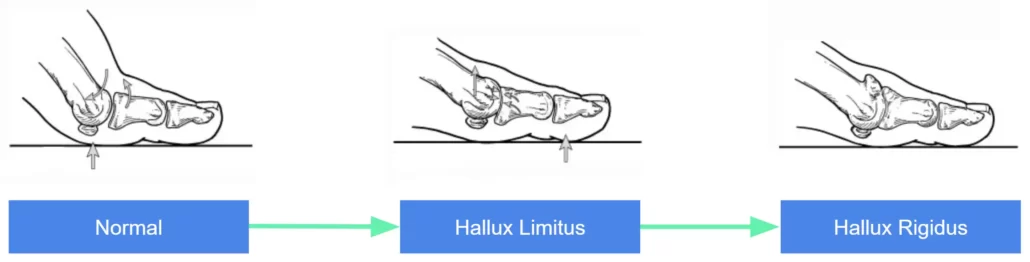
Normal: In a healthy foot, the big toe joint, specifically the metatarsophalangeal joint (MPJ), moves freely, allowing the toe to flex and extend fully. This flexibility is crucial for proper push-off during walking and running, as the MPJ enables smooth and efficient movement.
Hallux Limitus: At this stage, the movement of the big toe is significantly reduced. The MPJ begins to show restricted motion, and the proximal interphalangeal (PIP) joint exhibits limited or almost no flexibility. This results in pain and stiffness during activities that require toe extension, making simple tasks like walking or climbing stairs increasingly uncomfortable.
Hallux Rigidus: In the most advanced stage, the big toe joint becomes almost completely immobile. The MPJ loses nearly all of its movement, and the PIP joint remains rigid, causing the entire toe to be fixed in place. This severe degeneration results in chronic pain and extreme difficulty in performing weight-bearing activities, often necessitating medical intervention to alleviate symptoms and improve function.
The timeline for progression varies from person to person, depending on factors like age, activity level, genetics, and underlying health conditions. Some individuals may experience rapid deterioration, while others may have a slower, more gradual decline in joint function. Nevertheless, once Hallux Rigidus develops, the quality of life can be significantly compromised. Walking becomes laborious, and even minor activities, like standing or wearing certain types of shoes, can trigger intense pain. It is common for patients to experience a dull, aching discomfort in the joint at rest, which can worsen with physical activity.
Symptoms and Impact on Daily Activities
The symptoms of Hallux Rigidus are more severe and disabling compared to those of Hallux Limitus. The most noticeable symptom is the inability to bend the big toe upward, which affects the toe-off phase of the gait cycle. This immobility causes an abnormal walking pattern, as individuals unconsciously adjust their stride to minimize pain. As a result, the altered gait can lead to secondary issues, such as strain or pain in the ankles, knees, hips, or lower back. The body’s compensation mechanisms to deal with the loss of toe mobility can have a cascading effect, disrupting the function and balance of other joints.
Another significant symptom is persistent and often debilitating pain. This pain may be present even during periods of rest and can intensify with activity. For some, it manifests as a sharp, shooting pain in the joint, while for others, it is a constant, dull ache that radiates to surrounding areas. Swelling and inflammation around the joint are common, and patients may notice that the area is tender to the touch. The joint may feel particularly stiff and unyielding, especially in the morning or after long periods of inactivity. These symptoms can make even basic tasks, like walking to the store or climbing stairs, feel insurmountable.
Footwear becomes a significant issue for those with Hallux Rigidus. Standard shoes can put pressure on the enlarged joint, leading to excruciating pain. High heels and tight, narrow shoes are often out of the question. Many patients have to switch to footwear with a wide toe box and rigid soles to provide more comfort and reduce joint stress. The search for appropriate shoes can be frustrating and expensive, adding another layer of inconvenience to living with this condition. As the joint becomes more deformed and bony growths become more pronounced, it becomes increasingly difficult to find shoes that accommodate the joint changes.
Additionally, Hallux Rigidus can affect a person’s psychological well-being. Chronic pain and limited mobility often lead to feelings of frustration, anxiety, and even depression. The inability to participate in activities that were once enjoyable, such as hiking, running, or playing sports, can take an emotional toll. Social interactions may also be impacted, as the pain and discomfort discourage people from engaging in physical or outdoor activities with friends and family. The condition can feel isolating, and the daily struggle with pain can overshadow even simple pleasures.
People with physically demanding jobs may face even greater challenges. Standing, walking, or carrying heavy loads becomes significantly harder with Hallux Rigidus. In some cases, individuals may have to change their occupation or reduce working hours to cope with the physical demands. This loss of work capability can have financial repercussions, further compounding the stress and impact of the condition.
The combination of physical, emotional, and social challenges highlights the serious impact Hallux Rigidus can have on a person’s quality of life. It underscores the necessity of effective management strategies and, in severe cases, the consideration of surgical options to alleviate pain and improve mobility.
Causes and Risk Factors
Genetic Predisposition
One of the primary factors influencing the development of Hallux Limitus and Hallux Rigidus is genetic predisposition. If a person has a family history of arthritis or structural foot abnormalities, they are more likely to develop these conditions. Genetic factors can dictate the shape and alignment of the foot bones, which, in turn, affect the distribution of pressure across the joints. Certain foot shapes, such as a flat arch or an overly high arch, can predispose individuals to joint stress and early cartilage wear. The way bones are formed and how they interact in the joint also plays a role in the joint’s long-term health.
Some families have a history of musculoskeletal disorders, such as bunions or osteoarthritis, that can contribute to joint problems. Inherited conditions that affect collagen, the protein responsible for cartilage strength and flexibility, can also make individuals more susceptible. Understanding genetic predispositions can help in early identification and preventive measures, such as choosing appropriate footwear and engaging in joint-friendly physical activities.
Lifestyle and Environmental Factors
The way a person uses and stresses their feet over the years is another significant contributor to Hallux Limitus and Hallux Rigidus. Lifestyle and occupational demands can accelerate joint deterioration, especially in individuals whose jobs require prolonged standing, heavy lifting, or repetitive movements that stress the big toe. Athletes, particularly runners, dancers, and soccer players, are at a heightened risk because of the high-impact activities they engage in. The repetitive stress placed on the MTP joint during running, jumping, or sudden directional changes can lead to microtrauma and eventual cartilage degradation.
Poor footwear choices also play a major role. Wearing shoes that are too tight, have a narrow toe box, or place excessive pressure on the big toe joint, such as high heels, can exacerbate joint problems. High heels force the body’s weight forward, compressing the MTP joint and accelerating wear and tear. Even athletic shoes, if not properly fitted or lacking adequate support, can contribute to improper weight distribution across the foot, leading to joint damage. Footwear that fails to absorb shock adequately can compound the stresses endured by the big toe joint, particularly in active individuals.
Sedentary lifestyles can be equally harmful. Lack of exercise leads to weakened muscles and poor joint flexibility, making the MTP joint more susceptible to injury and degeneration. Additionally, weight gain or obesity can place excess pressure on the foot, magnifying joint stress and accelerating the arthritic process. Maintaining a healthy weight and an active lifestyle is crucial in managing pressure on the feet and keeping the joints functioning well over time.
Underlying Conditions Contributing to Joint Degeneration
Certain medical conditions can predispose individuals to develop Hallux Limitus and Hallux Rigidus. Osteoarthritis, the most common cause, is a degenerative joint disease characterized by the gradual breakdown of articular cartilage. The wear-and-tear nature of osteoarthritis makes the big toe joint particularly vulnerable, given the joint’s role in daily activities. As cartilage wears away, the joint loses its cushioning effect, leading to increased bone-on-bone friction and the development of bone spurs, which further restrict movement.
Rheumatoid arthritis, an autoimmune disorder, can also play a critical role. This inflammatory condition causes the immune system to attack the synovial lining of joints, leading to swelling, pain, and eventual cartilage destruction. Unlike osteoarthritis, which generally affects older individuals, rheumatoid arthritis can strike at a younger age, speeding up joint damage and the progression from Hallux Limitus to Hallux Rigidus. Gout, another form of arthritis caused by uric acid crystal buildup in the joint, can lead to acute inflammation and damage, accelerating joint stiffness.
Previous foot injuries, such as fractures, sprains, or dislocations of the big toe, are also contributing factors. Even if these injuries seem to have healed, they can leave lasting effects, such as misalignment or weakened joint structures, making the MTP joint more susceptible to arthritic changes. Trauma to the joint can lead to microfractures or scarring within the cartilage, diminishing its ability to absorb impact and protect the bones.
Additionally, systemic conditions such as diabetes and circulatory disorders can impact joint health. Poor circulation can lead to inadequate delivery of nutrients and oxygen to the joint tissues, impeding their ability to heal and remain resilient. Hormonal imbalances, particularly in post-menopausal women, can also contribute to joint deterioration due to decreased bone density and collagen production. Inflammatory conditions, such as lupus or psoriatic arthritis, can trigger widespread joint issues, including those affecting the big toe.
The Role of Foot Mechanics
Abnormal foot mechanics are a major cause of Hallux Limitus and Hallux Rigidus. Conditions like overpronation (where the foot rolls inward excessively) or supination (where the foot rolls outward) can alter the alignment and function of the big toe joint. Overpronation, for example, increases the inward rolling motion, forcing the big toe to absorb more impact and pressure than it is designed to handle. This repeated stress accelerates cartilage wear and exacerbates joint inflammation. Foot mechanics are also influenced by muscle imbalances, such as weak arch muscles, which can compromise the foot’s structural integrity.
Structural abnormalities, like having a long first metatarsal bone or bunions, can change how forces are distributed across the big toe joint. Bunions, which are bony bumps that form at the base of the big toe, push the toe outward and misalign the MTP joint, placing undue stress on the cartilage and accelerating degenerative changes. These anatomical variations can create a biomechanical disadvantage, leading to faster progression of joint issues.
Diagnosing Big Toe Arthritis: Tests, Imaging, and Clinical Signs
Clinical Examination and Tests
The journey to accurately diagnosing Hallux Limitus or Hallux Rigidus begins with a comprehensive clinical examination. When patients first visit a healthcare professional for toe joint pain, the doctor typically asks detailed questions about symptoms, lifestyle, and any history of foot injuries or arthritis in the family. This initial conversation sets the stage for a more targeted investigation. The physician will then assess the range of motion in the big toe, observing how far it can bend upward without pain. It’s a simple yet telling test—if the joint shows signs of stiffness or a grinding sensation (known as crepitus), it may point to early degenerative changes.
But it’s not just about testing flexibility. The doctor will also inspect the foot for visible signs of trouble, like swelling, redness, or bony deformities. Sometimes, they’ll apply pressure to the joint to check for tenderness or locate areas where bone spurs may be forming. A careful gait analysis might follow, where the physician watches the patient walk to identify any limping or compensatory movements that suggest the body is trying to work around a painful joint. This part of the diagnosis is fascinating because it highlights how interconnected the human body is—what happens to the big toe can ripple up to the knees, hips, or even the spine.
Imaging Techniques (X-ray, MRI)
To get a more definitive understanding of the joint’s condition, imaging techniques are the next step. X-rays are the most common and reveal much about the bone structure, including narrowing of the joint space, presence of bone spurs, or any changes in the alignment of the toe bones. An X-ray can show how much the cartilage has worn away and how far the condition has progressed. This imagery can often be an eye-opener for patients—seeing the joint damage firsthand helps them appreciate the importance of early intervention and ongoing care.
For more nuanced cases, where X-rays may not provide a complete picture, doctors may recommend an MRI (Magnetic Resonance Imaging). Unlike X-rays, MRIs can capture detailed images of the soft tissues, like cartilage, ligaments, and the synovial lining. This level of detail is crucial, especially in early stages of Hallux Limitus, when the cartilage damage may not be as obvious on an X-ray. An MRI can also detect any inflammation or fluid buildup within the joint, providing a full landscape of what’s happening inside. This advanced imaging method helps create a personalized treatment plan, tailored to the patient’s unique joint health.
Ultrasound, another imaging tool, is sometimes used to observe soft tissues in real-time, especially if there is suspected damage to the tendons surrounding the MTP joint. While not as commonly used as X-rays or MRIs, ultrasound has the advantage of being non-invasive and radiation-free, making it a helpful diagnostic adjunct.
Assessing the Severity of Joint Damage
Once the imaging results are in, doctors grade the severity of the joint damage. Hallux Limitus and Hallux Rigidus are often classified into stages based on how much the condition has advanced. This staging helps both the medical professional and the patient understand what to expect and how to move forward with treatment.
In Stage 1 of Hallux Limitus, the cartilage is just beginning to show signs of wear, and joint space is only slightly narrowed. Pain is intermittent, and the range of motion, though reduced, is still mostly intact. Moving to Stage 2, the condition becomes more pronounced, with bone spurs starting to form around the joint. Here, the joint space narrows further, and everyday activities like walking uphill or squatting can become painful. Stage 3 is marked by significant cartilage loss and limited motion, often accompanied by more visible swelling and constant discomfort. By Stage 4, we’ve reached Hallux Rigidus territory, where the joint is almost or completely fused, and movement is nearly impossible without severe pain. Bone spurs are usually extensive, and even walking on flat surfaces can be a monumental challenge.
Interestingly, the staging isn’t just about assigning a label—it’s a critical tool that helps tailor treatment. For instance, someone in Stage 1 or 2 might benefit from conservative therapies like orthotics, or anti-inflammatory medications. In contrast, patients in Stages 3 or 4 may need to consider more aggressive interventions, including surgery. The goal is to prevent progression as much as possible, but once Hallux Rigidus sets in, the treatment focus shifts to pain management and preserving mobility.
The Patient Experience
What’s fascinating, and perhaps even humbling, is how much a diagnosis can impact a patient’s life beyond the physical symptoms. For many, learning they have Hallux Limitus or Hallux Rigidus can be an emotional experience. The foot is a foundation of movement and freedom, and a condition that threatens this can feel deeply unsettling. Some patients describe the diagnosis as a wake-up call, prompting them to reassess their physical habits and overall lifestyle. It can also serve as a moment to appreciate the resilience of the human body and the advances in medicine that offer hope and relief.
The diagnostic process, while thorough and sometimes overwhelming, plays a crucial role in shaping a clear and actionable path forward. It’s a blend of science and empathy, where medical knowledge meets an understanding of the patient’s daily struggles. Ultimately, the more informed the patient is about the condition and its impact, the better equipped they are to make decisions that align with their goals and lifestyle. The journey of diagnosis and evaluation is not just about identifying a problem but about opening doors to solutions and a roadmap for living well despite the challenges posed by Hallux Limitus or Hallux Rigidus.
Osteopathy for Hallux Limitus: A Gentle, Whole-Body Approach
Understanding the Osteopathic Approach
Osteopathy is a holistic form of manual therapy that emphasizes the interconnectedness of the body’s structure and function. In treating Hallux Limitus, osteopaths focus on addressing not just the affected joint but the entire body system that may be contributing to or compensating for the dysfunction. The aim is to improve joint mobility, reduce pain, and optimize the foot’s overall function by aligning and balancing the musculoskeletal system. Osteopaths believe that by treating the body as a whole, they can facilitate natural healing processes and prevent further joint degeneration.
Osteopathy offers a unique perspective on managing Hallux Limitus. Unlike conventional medicine, which may quickly turn to medications or invasive procedures, osteopathic treatment seeks to restore balance and improve the function of the foot and leg through gentle, hands-on techniques. These techniques work to improve blood flow, promote lymphatic drainage, and enhance nerve function, all of which are critical for reducing inflammation and pain in the big toe joint.
Manual Therapy Techniques
One of the primary methods used in osteopathy for Hallux Limitus is manual therapy. This involves a series of hands-on techniques designed to mobilize the joint and surrounding tissues. Osteopaths use gentle, rhythmic movements to encourage the MTP joint to release and gain a better range of motion. This might include articulatory techniques, where the osteopath moves the joint through its natural range of motion to help break up stiffness and improve flexibility. These sessions are often relaxing and are tailored to the patient’s comfort level.
Soft tissue manipulation is another essential tool in the osteopathic treatment plan. By working on the muscles and connective tissues around the big toe and foot, osteopaths can release tension and improve circulation. Soft tissue techniques may involve deep tissue massage, myofascial release, or gentle stretching to relieve muscle tightness that may be contributing to the restricted movement of the toe joint. By loosening these tissues, osteopaths aim to reduce strain on the MTP joint and improve overall foot mechanics.
In addition, osteopathic manipulation of the lower leg and pelvis may be included in treatment. Because the body is interconnected, dysfunction in the big toe can lead to compensatory issues higher up in the kinetic chain, such as the ankles, knees, hips, and even the lower back. Osteopaths assess the whole lower limb and pelvis to ensure proper alignment and balance, which can relieve pressure on the foot and improve gait. This holistic approach helps to correct biomechanical imbalances that might otherwise exacerbate the symptoms of Hallux Limitus.
Empowering Self-Care: Exercises and Advice from Osteopaths
Osteopathic treatment doesn’t stop when the patient leaves the clinic. A significant aspect of osteopathy is patient education and self-care. Osteopaths often prescribe home exercises tailored to the individual’s needs. These exercises aim to improve the range of motion in the big toe, strengthen the muscles supporting the foot, and promote better posture and alignment throughout the lower body. Common exercises might include toe stretches, foot strengthening movements, and calf stretches to ease tension in the Achilles tendon and plantar fascia.
For example, an osteopath may recommend toe extension exercises where the patient gently pulls the big toe upward, holding it for several seconds to increase flexibility. Another effective exercise could be a marble pick-up, where the patient uses their toes to pick up small objects from the floor, strengthening the foot muscles. These exercises are simple but powerful, and when done consistently, they can contribute significantly to symptom management and the slowing of joint degeneration.
Osteopaths may also provide guidance on footwear and ergonomics. Wearing supportive, well-fitted shoes with a wide toe box and cushioning can alleviate stress on the MTP joint. They may recommend avoiding high heels and tight shoes that exacerbate joint stiffness and pain. Additionally, osteopaths can offer advice on how to modify daily activities to reduce joint stress, such as using a footrest while sitting or avoiding prolonged standing.
Balancing the Whole Body
One of the more profound benefits of osteopathy is its emphasis on the balance and alignment of the entire body. This holistic approach can have ripple effects beyond just the big toe joint. By addressing tension and dysfunction throughout the musculoskeletal system, osteopaths aim to improve the body’s overall function and facilitate the natural healing process. For example, a tight hip flexor or a misaligned pelvis could be contributing to poor foot mechanics, exacerbating the symptoms of Hallux Limitus. Through targeted adjustments and release techniques, osteopaths work to restore proper balance and function across the entire body.
In cases where joint inflammation is severe, osteopaths may use cranial osteopathy to reduce systemic inflammation and promote relaxation. This gentle technique focuses on the subtle movements of the body’s tissues, particularly around the head and sacrum, to encourage the body to heal itself. While cranial osteopathy may not seem directly related to foot pain, it can have a calming effect on the nervous system, helping to manage pain and inflammation holistically.
Benefits and Considerations
Osteopathic treatment for Hallux Limitus offers numerous benefits, particularly for those looking to avoid medication or surgery. It provides a natural and non-invasive approach that can be especially effective in the early stages of the condition. By improving joint mobility, enhancing blood flow, and promoting overall balance, patients often experience relief from pain and a greater ability to perform daily activities. Moreover, osteopathy’s holistic approach helps patients understand how their overall body mechanics can affect foot health, empowering them to take an active role in their well-being.
However, it’s important to note that osteopathic treatment may not be a complete cure for Hallux Limitus, especially in advanced stages where the joint has undergone significant degenerative changes. In such cases, osteopathy can be used as a complementary therapy alongside other medical treatments to manage pain and improve quality of life. Osteopaths often work collaboratively with podiatrists and orthopedic specialists to create a comprehensive care plan tailored to the patient’s needs.
Prevention First: Protecting the Big Toe Joint Before It’s Too Late
Footwear Recommendations
Preventing or managing the symptoms of Hallux Limitus and Hallux Rigidus starts with something as simple yet impactful as selecting the right footwear. One of the most crucial steps in self-care is choosing shoes that minimize stress on the big toe joint and provide adequate support. Shoes with a wide toe box allow the toes to spread naturally, reducing compression on the MTP joint and preventing further irritation. Tight or narrow shoes can worsen symptoms, exacerbating joint stiffness and pain, so it’s essential to ensure that the front of the shoe provides plenty of space.
Rocker-bottom shoes are particularly beneficial for those with Hallux Limitus or Hallux Rigidus. These shoes feature a curved sole that reduces the need for the big toe to bend during the toe-off phase of walking. By shifting the pressure away from the MTP joint, rocker-bottom shoes can help make walking more comfortable and less painful. Additionally, shoes with stiff soles provide support and reduce the amount of movement in the big toe, further alleviating stress on the joint.
High heels are generally a no-go for those dealing with these conditions. Heels force the body weight forward, putting extra pressure on the forefoot and exacerbating pain in the big toe joint. Instead, opt for shoes with a low heel or no heel at all. If supportive shoes are not an option in every situation, custom orthotic inserts can be used to provide additional arch support and correct any biomechanical imbalances in the foot. These inserts help redistribute weight more evenly and reduce pressure on the MTP joint.
Exercises and Stretches for Toe Mobility
While Hallux Limitus and Hallux Rigidus may limit the range of motion in the big toe, performing gentle exercises can help maintain flexibility and strength. Toe stretches are a simple yet effective way to keep the joint as mobile as possible. One common stretch involves manually pulling the big toe upward, holding it in a gentle stretch for several seconds before releasing. This exercise can be repeated multiple times a day to improve flexibility gradually.
Another beneficial exercise is the towel scrunch, where you place a towel on the floor and use your toes to scrunch it up. This helps strengthen the muscles in the foot, providing better support for the MTP joint. Picking up small objects, such as marbles or pebbles, with the toes is another effective way to engage the foot muscles and keep them strong. These exercises are easy to incorporate into a daily routine and can be done from the comfort of home.
Calf stretches can also indirectly benefit the big toe joint by relieving tension in the Achilles tendon and the plantar fascia. Tightness in these areas can exacerbate foot pain and limit mobility. Stretching the calves regularly, such as by standing on a step and gently lowering the heels, can reduce strain on the entire foot and improve overall foot mechanics. Consistent stretching and strengthening exercises can help slow the progression of joint stiffness and keep the foot functioning as well as possible.
Managing Arthritis and Preventing Further Damage
For individuals prone to or already dealing with arthritis in the big toe joint, managing inflammation and slowing joint degeneration are key preventive strategies. Dietary choices play a significant role in managing arthritis. An anti-inflammatory diet rich in omega-3 fatty acids, antioxidants, and whole foods can help reduce systemic inflammation. Foods like salmon, walnuts, leafy greens, and berries are excellent options for promoting joint health. Reducing the intake of processed foods, refined sugars, and trans fats can also mitigate inflammation and support overall well-being.
Weight management is another crucial factor. Carrying excess body weight places additional stress on the joints of the feet, accelerating cartilage wear and exacerbating symptoms. By maintaining a healthy weight through balanced nutrition and regular, low-impact exercise, individuals can reduce the pressure on their big toe joint and improve their overall foot health. Swimming, cycling, and yoga are all excellent forms of exercise that minimize impact on the joints while promoting cardiovascular health and flexibility.
In addition to lifestyle modifications, incorporating self-care practices such as regular foot massages can improve circulation and relieve muscle tension. Massaging the bottom of the foot and the area around the big toe joint helps stimulate blood flow, reducing inflammation and promoting healing. Warm foot soaks with Epsom salts can also provide temporary relief from pain and stiffness. The magnesium in Epsom salts is believed to help relax muscles and reduce inflammation, making this a simple yet effective home remedy.
Applying cold therapy to the joint can help manage acute pain and swelling. Using an ice pack wrapped in a cloth and placing it on the affected area for 10-15 minutes can reduce inflammation and numb pain. Conversely, heat therapy, such as using a warm towel or heating pad, can be beneficial for relaxing stiff muscles and improving joint flexibility. Alternating between heat and cold therapy is a strategy that many find helpful for managing symptoms.
Avoiding Aggravating Activities
Certain activities can exacerbate Hallux Limitus or Hallux Rigidus, so modifying or avoiding them is an essential part of prevention and management. Activities that place excessive pressure on the big toe joint, such as running, jumping, or wearing high-heeled shoes, should be avoided or minimized. Instead, focus on low-impact exercises that promote overall fitness without stressing the feet. Walking on soft, even surfaces is preferable to walking on hard, uneven ground, which can jar the joints and worsen symptoms.
If standing for long periods is unavoidable, consider using a cushioned mat to reduce pressure on the feet and provide extra support. Taking frequent breaks to sit and elevate the feet can help minimize swelling and discomfort. Awareness of body mechanics is crucial, and small adjustments, such as distributing weight evenly on both feet or using a stool to rest one foot while standing, can make a significant difference.
Monitoring and Seeking Professional Guidance
Finally, regular monitoring of symptoms and professional evaluations are key to preventing further joint damage. If pain or stiffness worsens despite lifestyle changes and preventive measures, consulting an osteopath or podiatrist is crucial. Early intervention can prevent the condition from advancing and provide access to a broader range of treatment options. Osteopaths can offer personalized recommendations based on a patient’s specific condition and help develop a long-term plan to manage symptoms effectively.
By integrating these preventive strategies into daily life, individuals with Hallux Limitus or Hallux Rigidus can take proactive steps to protect their joints, manage pain, and maintain an active lifestyle. Prevention and self-care empower patients to stay in control of their condition and improve their overall quality of life.
Adapting to Life with Big Toe Arthritis: Coping and Thriving
Coping Strategies and Support
Living with Hallux Limitus or Hallux Rigidus can be challenging, as these conditions affect daily mobility and quality of life. However, adopting effective coping strategies can help manage symptoms and maintain a level of independence. One of the key approaches is establishing a daily routine that prioritizes joint care and minimizes pain. For many, this includes starting the day with gentle foot stretches to warm up the muscles and promote flexibility, preparing the joints for the day’s activities.
Adapting to life with reduced mobility in the big toe often requires modifying day-to-day activities. For example, using a sturdy walking stick or cane can provide extra stability, particularly on uneven terrain or during long periods of walking. These mobility aids reduce the load on the affected foot and make movement safer and more comfortable. Another useful modification is using shoe inserts or cushioned footwear that reduce impact and support proper foot alignment. This can make standing or walking for extended periods less taxing on the joint.
Adapting one’s home environment can also be helpful. For individuals who experience pain or stiffness first thing in the morning, placing a small stool or bench in the shower can make bathing more comfortable and safer. Installing grab bars near the toilet and in the bathroom can also provide extra support and prevent falls. In the kitchen, having commonly used items at a convenient height reduces the need for standing on tiptoes or bending down, both of which can put stress on the big toe joint.
The Hidden Struggles: Emotional Impact of Chronic Toe Pain
The emotional and psychological impact of Hallux Limitus and Hallux Rigidus is often overlooked but is a crucial aspect of living with these conditions. Chronic pain and reduced mobility can lead to feelings of frustration, anxiety, and even depression. The inability to engage in once-loved activities, such as running, hiking, or playing sports, can take a toll on mental well-being. The fear of worsening symptoms or facing potential surgeries can also contribute to emotional stress.
To cope with these challenges, many individuals find it helpful to seek emotional support from friends, family, or support groups. Connecting with others who understand the experience of living with chronic joint conditions can provide a sense of community and reassurance. Support groups, either in person or online, offer a platform to share experiences, exchange coping strategies, and learn from others who have navigated similar challenges.
Mindfulness practices, such as meditation and deep breathing exercises, can also be powerful tools for managing the psychological impact of chronic pain. Mindfulness techniques teach individuals to focus on the present moment and accept their pain without judgment, reducing stress and enhancing overall well-being. Guided meditations that focus on relaxation and pain management can be particularly effective for alleviating discomfort and promoting a sense of calm.
Cognitive-behavioral therapy (CBT) is another option for those struggling with the emotional aspects of living with Hallux Limitus or Hallux Rigidus. CBT is a structured, goal-oriented form of therapy that helps people identify and change negative thought patterns related to pain and disability. By shifting one’s mindset and learning to cope with pain more effectively, individuals can improve their mental outlook and develop a more positive approach to managing their condition.
Planning for the Future: Managing Hallux Conditions Over Time
The long-term management of Hallux Limitus and Hallux Rigidus involves a combination of medical treatments, self-care practices, and lifestyle adjustments. It’s important to recognize that while these conditions are progressive, proactive management can significantly slow down joint degeneration and improve overall quality of life. Regular follow-up appointments with healthcare professionals, such as osteopaths or podiatrists, are essential to monitor the condition and make adjustments to the treatment plan as needed.
One of the keys to long-term success is staying active while respecting your body’s limits. Low-impact exercises, such as swimming or biking, are excellent options for maintaining fitness without putting undue pressure on the big toe joint. Yoga and Pilates can also be beneficial, as they promote flexibility, strength, and balance. Engaging in these activities regularly can help maintain joint mobility and support overall well-being. However, it’s crucial to listen to your body and avoid exercises that cause pain or exacerbate symptoms.
Diet and nutrition continue to play a critical role in managing these conditions over the long term. Maintaining a healthy weight is crucial for reducing joint stress, and consuming a diet rich in anti-inflammatory foods can support joint health. Supplements, such as glucosamine and chondroitin, are sometimes considered for joint support, though it’s essential to consult with a healthcare provider before adding them to your regimen. Staying well-hydrated and focusing on nutrient-dense foods can make a meaningful difference in how the body manages inflammation and pain.
Another aspect of long-term management is foot care and hygiene. Keeping the feet clean, moisturized, and well-cared-for helps prevent secondary issues, such as corns, calluses, or fungal infections, which can add to the discomfort. Regularly inspecting the feet for any signs of abnormal wear or changes is also important, as it can provide early warnings of worsening conditions.
You’re Not Alone: Building Support for Chronic Toe Conditions
Living with chronic joint conditions like Hallux Limitus and Hallux Rigidus is more manageable when there is a strong support network in place. This includes healthcare providers, such as osteopaths, podiatrists, and general practitioners, who can collaborate on the best treatment plan. It also means having friends and family who understand the physical and emotional challenges of the condition. Open communication about pain levels, limitations, and needs can make a significant difference in how supported and understood a person feels.
Educating family members and close friends about the condition can also foster empathy and cooperation. When loved ones understand that tasks like climbing stairs or standing for long periods are painful, they are more likely to provide the support and assistance needed. Whether it’s helping with household chores, accompanying someone to medical appointments, or simply being there to listen on tough days, a compassionate support network can greatly enhance one’s ability to cope.
In addition to personal support networks, exploring community resources can be beneficial. Some communities offer exercise classes tailored to individuals with joint conditions or workshops on pain management techniques. Local arthritis foundations or health organizations may provide valuable resources and connections to professionals who specialize in managing joint conditions.
By combining physical adjustments, emotional support, and a proactive approach to managing symptoms, individuals with Hallux Limitus and Hallux Rigidus can maintain a fulfilling and active life despite the challenges these conditions bring.
FAQs: Your Top Questions About Hallux Limitus and Rigidus Answered
Common Concerns and Misconceptions
- What exactly is the difference between Hallux Limitus and Hallux Rigidus?
- Hallux Limitus is an early stage of joint degeneration in the big toe where the range of motion, particularly upward movement (dorsiflexion), is limited but not completely restricted. As the condition progresses, it can lead to Hallux Rigidus, which is characterized by severe stiffness and the near-immobility of the joint. Hallux Rigidus is essentially an advanced form of osteoarthritis, where the big toe becomes rigid, significantly impacting daily activities.
- Can Hallux Limitus or Hallux Rigidus be reversed?
- Unfortunately, these conditions cannot be completely reversed, as they are forms of degenerative arthritis. However, with early intervention and the right management strategies, the progression can be slowed, and symptoms can be effectively managed. Osteopathic care, lifestyle changes, and proper footwear can make a significant difference in maintaining joint function and reducing pain.
- Is surgery always necessary for Hallux Rigidus?
- Surgery is not always necessary and is generally considered a last resort. Many people with Hallux Rigidus can manage their symptoms effectively with non-surgical methods, such as osteopathic treatments, lifestyle modifications, orthotics, and pain management techniques. Surgery is usually recommended only when conservative measures have failed to provide relief or when the condition severely impacts daily life.
- Will changing my shoes really help that much?
- Yes, proper footwear can make a significant impact on managing both Hallux Limitus and Hallux Rigidus. Shoes with a wide toe box, stiff soles, and adequate arch support can reduce pressure on the big toe joint and alleviate pain. Rocker-bottom shoes are particularly helpful in reducing the need for the toe to bend when walking, providing greater comfort and mobility.
- How do I know if I need custom orthotics?
- Custom orthotics may be necessary if you experience significant pain, have abnormal foot mechanics, or if standard shoe inserts do not provide enough relief. A healthcare provider, such as an osteopath or podiatrist, can evaluate your foot mechanics and recommend whether custom orthotics are appropriate for your condition. These custom devices are designed to correct specific foot imbalances and can be a game-changer in managing symptoms.
- Can I continue to exercise with Hallux Limitus or Hallux Rigidus?
- Yes, staying active is crucial, but it’s important to choose low-impact activities that don’t exacerbate the condition. Swimming, cycling, and gentle yoga are excellent options for maintaining fitness while minimizing stress on the big toe joint. Avoid high-impact activities like running, jumping, or exercises that put excessive pressure on the toes. Always consult with a healthcare professional to develop a safe and effective exercise routine.
- Is osteopathy a legitimate treatment for these conditions?
- Yes, osteopathy is a well-regarded, holistic approach that can be effective in managing Hallux Limitus and Hallux Rigidus. Osteopaths use gentle, hands-on techniques to improve joint mobility, reduce inflammation, and address compensatory issues throughout the body. Many patients find relief from osteopathic treatment, especially when used as part of a comprehensive management plan that includes lifestyle adjustments and proper footwear.
- Can Hallux Limitus or Hallux Rigidus affect other parts of my body?
- Absolutely. These conditions often lead to compensatory movement patterns, which can place extra strain on other joints, such as the ankles, knees, hips, and even the lower back. Over time, this can lead to pain and dysfunction in these areas. Addressing the condition early and focusing on whole-body alignment can help minimize these secondary issues.
- How do I prevent my Hallux Limitus from turning into Hallux Rigidus?
- Early intervention is key. This includes using proper footwear, performing regular exercises to maintain joint mobility, and seeking osteopathic treatment to address structural imbalances. Managing inflammation through diet, weight management, and stress reduction can also play a role in slowing the progression of joint degeneration. Regular check-ups with a healthcare provider can help monitor the condition and adjust your treatment plan as needed.
- What lifestyle changes can make a big difference?
- Simple lifestyle changes can have a profound impact on managing symptoms and slowing the progression of these conditions. This includes maintaining a healthy weight, wearing supportive shoes, avoiding high-impact activities, and incorporating anti-inflammatory foods into your diet. Reducing overall stress and practicing mindfulness techniques can also help, as chronic pain often has an emotional component.
- Can I use over-the-counter pain relief medications long-term?
- Over-the-counter pain relievers, such as NSAIDs (nonsteroidal anti-inflammatory drugs), can be helpful for managing pain and inflammation in the short term. However, long-term use should be discussed with a healthcare provider, as these medications can have side effects, such as gastrointestinal issues or increased risk of cardiovascular problems. Alternative pain management strategies, including osteopathic treatment and lifestyle modifications, are often recommended for long-term relief.
Key Insights and a Call to Action: Take Charge of Your Foot Health
Key Takeaways
Hallux Limitus and Hallux Rigidus are progressive joint conditions that significantly affect mobility and quality of life. Understanding the differences between the two, from limited motion in the early stages to severe joint stiffness in advanced cases, is crucial for effective management. Both conditions can be debilitating if not addressed early, but with proactive measures, many individuals can maintain a good level of mobility and comfort.
One of the most important aspects of managing these conditions is early diagnosis and intervention. When symptoms first appear, such as stiffness or pain in the big toe, taking action quickly can help slow the degenerative process. Osteopathic treatment offers a unique, non-invasive approach that addresses the body as a whole, helping to alleviate symptoms and improve overall joint function. This approach, combined with lifestyle adjustments, can make a meaningful difference in the progression of the condition.
Proper footwear and orthotic support are essential in reducing stress on the MTP joint and preventing further damage. The importance of a supportive and well-structured shoe cannot be overstated, as it is one of the simplest yet most effective tools for pain management and joint protection. Additionally, exercises and stretches aimed at maintaining joint mobility, as well as mindful adjustments to daily activities, can support long-term joint health.
Encouragement for Seeking Medical Advice
While managing Hallux Limitus or Hallux Rigidus can be challenging, it’s essential to remember that there are many resources and treatment options available. Whether through osteopathic care, proper footwear, or lifestyle changes, small steps can lead to significant improvements in daily comfort and functionality. Don’t hesitate to seek out professional advice if you notice persistent pain or stiffness in your big toe joint. Consulting with an osteopath or podiatrist can open up a range of personalized treatment strategies that align with your lifestyle and long-term goals.
Managing these conditions is not just about reducing pain—it’s about empowering yourself to live an active, fulfilling life despite the challenges. Staying informed, being proactive, and building a strong support network are key components of navigating life with Hallux Limitus or Hallux Rigidus. Remember that each person’s journey is unique, and what works for one individual may not work for another. Stay patient, be consistent with your care, and don’t be afraid to explore different approaches until you find the right fit for you.
Final Thoughts
Incorporating osteopathic care into your treatment plan can offer relief and a more comprehensive understanding of your body’s mechanics. By focusing on the whole body rather than just the affected joint, osteopathy provides a holistic and integrative way to manage symptoms. Lifestyle modifications, mindfulness techniques, and an emphasis on self-care can further enhance your quality of life.
Though Hallux Limitus and Hallux Rigidus may be conditions you have to live with, they do not have to define or limit your life. With the right strategies, a supportive medical team, and a commitment to self-care, you can take control of your condition and continue to enjoy many of the activities you love. Always listen to your body, and don’t hesitate to adjust your approach as your needs change.
References
- “Treatment of Hallux Rigidus: Comparison of Hemiarthroplasty with Cartiva Implant, Allograft Interpositional Arthroplasty, and Arthrodesis”
- This study compares different surgical methods for treating Hallux Rigidus, analyzing outcomes such as pain reduction and joint function.
- Read More
- “Physical Function and Pain Interference Levels of Hallux Rigidus Patients Before and After Synthetic Cartilage Implant vs Arthrodesis Surgery”
- This research examines pre- and postoperative physical function and pain levels in patients undergoing different surgical treatments for Hallux Rigidus.
- Read More
- “Non-Operative Management of Symptomatic Hallux Limitus: A Novel Approach of Foot Core Stabilization and Extracorporeal Shockwave Therapy”
- The paper discusses a non-surgical approach combining foot strengthening and shockwave therapy to manage Hallux Limitus.
- Read More
- “A Retrospective Study Assessing the Clinical Outcomes After Cheilectomy and Subchondroplasty for Hallux Rigidus”
- The study evaluates the outcomes of cheilectomy and subchondroplasty as surgical treatments for Hallux Rigidus.
- Read More
- “Cheilectomy With Decompression Osteotomy for Treatment of Hallux Limitus and Rigidus: A Retrospective Study With 5-Year Outcomes”
- It provides insights into the long-term efficacy of decompression osteotomy combined with cheilectomy for treating these conditions.
- Read More
- “The efficacy of shoe modifications and foot orthoses in treating patients with hallux rigidus: a comprehensive review of literature”
- This review discusses the effectiveness of orthotic devices and shoe modifications as conservative treatments for Hallux Rigidus.
- Read More
- “Hallux rigidus treated with adipose-derived mesenchymal stem cells: A case report”
- The case study explores the use of stem cell therapy to treat Hallux Rigidus, showing improvements in pain and function.
- Read More
- “Patient-reported outcomes of joint-preserving surgery for moderate hallux rigidus: a 1-year follow-up of 296 patients from Swefoot”
- Reports on patient outcomes after surgical procedures for moderate Hallux Rigidus, with a focus on patient satisfaction and joint function.
- Read More
- Licciardone, J. C., Gatchel, R. J., & Aryal, S. (2016).
- Recovery from Chronic Low Back Pain after Osteopathic Manipulative Treatment: A Randomized Controlled Trial. Journal of the American Osteopathic Association, 116(3), 144-155.
- https://doi.org/10.7556/jaoa.2016.028
- Cerritelli, F., Lacorte, E., Ruffini, N., Vanacore, N., & Integrative Osteopathic Research Group (2017).
- Effectiveness of Osteopathic Manipulative Treatment: An Updated Systematic Review of Randomized Controlled Trials. Journal of Bodywork and Movement Therapies, 21(4), 752-762.
- https://doi.org/10.1016/j.jbmt.2017.07.008
- Franke, H., Fryer, G., Ostelo, R. W., & Kamper, S. J. (2015).
- Muscle Energy Technique for Non-Specific Low-Back Pain: A Cochrane Systematic Review. Cochrane Database of Systematic Reviews, (2), CD009852.
- https://doi.org/10.1002/14651858.CD009852.pub2
- Brolinson, P. G., et al. (2012).
- Osteopathic Manipulative Medicine in the Management of Chronic Pain:
- An Evidence-Based Review. Pain Physician, 15(5), E677-E689. Retrieved from
- https://www.painphysicianjournal.com
- Guillaud, A., Darbois, N., Monvoisin, R., & Pinsault, N. (2018).
- Reliability of Diagnosis and Clinical Efficacy of Osteopathy: A Systematic Review. PLoS ONE, 13(4), e0195655.
- https://doi.org/10.1371/journal.pone.0195655
- Anderson, R., & Seniscal, C. (2006).
- A Review of Osteopathic Manipulative Treatment Research and Indications for Clinical Practice. Osteopathic Family Physician, 2(3), 11-16.
- Licciardone, J. C. (2003).
- The Efficacy of Osteopathic Manipulative Treatment in Patients with Chronic Low Back Pain: A Randomized Controlled Trial. Spine Journal, 3(1), 35-43.
- https://doi.org/10.1016/S1529-9430(02)00677-7
- Cerritelli, F., Ginevri, L., Messi, G., Caprari, E., & Di Vincenzo, M. (2015).
- Clinical Effectiveness of Osteopathic Treatment in Chronic Migraine: A Pilot Study. Journal of Bodywork and Movement Therapies, 19(3), 586-594.
- https://doi.org/10.1016/j.jbmt.2014.11.009
- Fryer, G. (2011).
- The Use of Manipulative Therapy in the Treatment of Musculoskeletal Pain. Manual Therapy, 16(1), 53-65.
- https://doi.org/10.1016/j.math.2010.08.005
- Collins, C., & Brantingham, J. W. (2010).
- The Role of Osteopathic Manipulative Treatment in the Management of Cervical Spine Conditions. Journal of Manual & Manipulative Therapy, 18(3), 135-142.
- https://doi.org/10.1179/106698110X12804993426864



















