The term “vertebrobasilar insufficiency” (VIB) encompasses all transient ischemic attacks (TIAs) of the posterior circulation of the brain.
Introduction
Vertebrobasilar insufficiency (VBI) is a condition characterized by reduced blood flow to the posterior circulation of the brain, which includes the vertebrobasilar arteries. This condition can lead to various neurological symptoms, such as dizziness, vertigo, imbalance, visual disturbances, and even stroke.
Cervical manipulation, a common technique used by some healthcare practitioners, has been a subject of debate regarding its potential association with vertebral artery dissection (VAD) and subsequent VBI. While cervical manipulation is generally considered safe when performed by trained and experienced practitioners, there have been reported cases of VAD and VBI following cervical manipulation, leading to concerns about its safety. The mechanism by which cervical manipulation may lead to VAD is thought to involve excessive rotation or extension of the cervical spine, leading to stretching or tearing of the vertebral artery. This can result in the formation of a blood clot within the arterial wall, which may then dislodge and occlude smaller blood vessels in the brain, causing ischemia or stroke. However, it’s important to note that the incidence of VAD and subsequent VBI following cervical manipulation is extremely rare, and the absolute risk is considered to be low. Moreover, many cases of VBI occur spontaneously or are associated with other risk factors such as hypertension, atherosclerosis, or trauma, rather than cervical manipulation alone. Nevertheless, healthcare practitioners should be aware of the potential risks associated with cervical manipulation and carefully assess each patient’s individual risk factors before performing this technique.
Patients should also be informed of the potential risks and benefits of cervical manipulation and provide informed consent before undergoing treatment. In conclusion, while cervical manipulation has been associated with rare cases of VAD and subsequent VBI, the absolute risk is low, and the technique is generally considered safe when performed by trained and experienced practitioners. However, healthcare practitioners should exercise caution and carefully assess each patient’s individual risk factors before performing cervical manipulation, and patients should be informed of the potential risks and benefits of this technique.
Anatomy and physiology of the vertebrobasilar arterial system
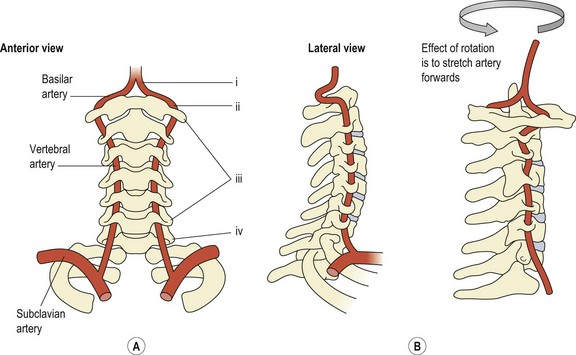
The anatomy and physiology of the vertebrobasilar arterial system play a crucial role in supplying blood to the posterior circulation of the brain. An important distinction between the cervical regions and other spinal regions is the presence of the vertebral arteries. These arteries originate from the subclavian artery and traverse through the transverse foramen of each cervical vertebra from C6 and above. As the artery approaches the atlas, it takes a nearly horizontal course before entering the foramen magnum to join its counterpart and form the basilar artery.
The vertebral arteries are responsible for providing approximately 11% of cerebral blood flow, with the remaining 89% being supplied by the carotid system (Grant, 1994a). Notably, approximately half of cervical rotation, around 45-50 degrees, primarily occurs at the atlantoaxial joint. During head rotation, the vertebral artery, tethered to the transverse foramina of C1 and C2, undergoes a series of mechanical stresses including stretching, compression, and twisting.
Research indicates that rotational movements, particularly those involving the cervical spine, can significantly impact blood flow through the vertebral artery (deKleyn and Nieuwenhuyse, 1927; deKleyn and Versteegh, 1933; Tatlow and Bammer, 1957; Toole and Tucker, 1960; Brown and Tatlow, 1963; Andersson et al., 1970; Barton and Margolis, 1975; Grossman and Davies, 1982; Yang et al., 1985). These movements produce the greatest reduction in blood flow to the vertebral artery, potentially leading to compromised perfusion to the brainstem and cerebellum.
Understanding the biomechanics and vascular anatomy of the vertebrobasilar system is essential, particularly in clinical settings where cervical manipulation is performed. Manipulative procedures involve mobilization or manipulation of the cervical spine, which can inadvertently affect the vertebral arteries. Given the vulnerability of these arteries to mechanical stress during cervical rotation, practitioners must exercise caution and employ appropriate techniques to minimize the risk of adverse events such as vertebral artery dissection or vertebrobasilar insufficiency.
In conclusion, the vertebrobasilar arterial system, comprised of the vertebral arteries and basilar artery, plays a critical role in supplying blood to the posterior circulation of the brain. The unique anatomical features of the cervical spine, including the presence of the vertebral arteries, make this region particularly susceptible to mechanical stresses during rotational movements. Healthcare practitioners should be cognizant of these factors when performing cervical manipulation and take appropriate precautions to ensure patient safety.
Vertebral Arteries
- Origin: The vertebral arteries are branches of the subclavian arteries, which in turn originate from the aorta.
- Course: Each vertebral artery ascends through the foramen transversarium of the cervical vertebrae (usually C6 to C1) on its way toward the skull.
- Meeting: The two vertebral arteries generally join at the base of the skull to form the basilar artery.
Basilar artery
- Origin: Formed by the meeting of the two vertebral arteries.
- Course: The basilar artery runs along the anterior surface of the brainstem, at the base of the brain.
- Branches: The basilar artery gives rise to several branches, which supply blood to different parts of the brain, including the brainstem, cerebellum, cranial nerves, and the posterior part of the cerebrum.
Collaterals and Anastomoses
- The vertebral and basilar arteries anastomose with other branches of the anterior carotid system, thus providing a collateral blood supply to the brain.
- These anastomoses are crucial for the regulation of cerebral blood flow in the event of pressure variations or partial obstruction of the vessels.
Functioning and Importance for Health
- Cerebral Irrigation: The vertebrobasilar system supplies a large portion of oxygenated blood to the brainstem, cerebellum, and other posterior brain regions. These regions are involved in vital functions such as regulating heart rate, coordinating movements, and sensory processing.
- Regulation of Intracranial Pressure: The vertebral and basilar arteries contribute to the regulation of intracranial pressure by supplying blood to the brain structures that play a role in this regulation.
- Role in the Vasomotor Reflex: These arteries also participate in the cerebral vasomotor reflex, which adjusts the diameter of cerebral blood vessels to maintain adequate blood flow.
Incidence of vertebrobasilar stroke after manual spinal manipulation
The incidence of vertebrobasilar stroke following manual spinal manipulation has been a subject of considerable debate and research within the healthcare community. Manual spinal manipulation involves applying controlled force to the spine to alleviate musculoskeletal pain and improve joint function. While many patients benefit from this form of therapy, concerns have been raised regarding its potential association with vertebral artery dissection (VAD) and subsequent vertebrobasilar stroke.
Vertebrobasilar stroke, also known as posterior circulation stroke, occurs when blood flow to the posterior part of the brain is compromised, often as a result of arterial dissection or occlusion. This condition can lead to various neurological symptoms, including dizziness, vertigo, visual disturbances, weakness, and paralysis. While vertebrobasilar stroke is relatively rare, it can have serious and sometimes fatal consequences, making it a significant concern for both patients and healthcare providers.
Several studies have investigated the association between manual spinal manipulation and vertebrobasilar stroke, with conflicting results. Some studies have reported an increased risk of stroke following spinal manipulation, particularly in the cervical region, while others have found no significant association. The variability in findings may be due to differences in study design, patient populations, and definitions of spinal manipulation and stroke.
One of the challenges in assessing the risk of vertebrobasilar stroke after spinal manipulation is the rarity of the event. Vertebrobasilar stroke is a relatively uncommon occurrence, making it difficult to conduct large-scale prospective studies with sufficient statistical power to detect meaningful associations. Additionally, many cases of vertebral artery dissection and subsequent stroke occur spontaneously or are associated with other risk factors, such as trauma, hypertension, or atherosclerosis, rather than spinal manipulation alone.
Despite these challenges, healthcare providers should be aware of the potential risks associated with spinal manipulation and take appropriate precautions when recommending or performing this therapy. Patients with preexisting risk factors for stroke, such as hypertension, hyperlipidemia, or a history of vascular disease, may be at higher risk for adverse events following spinal manipulation and should be carefully evaluated before undergoing treatment.
Furthermore, practitioners should adhere to established guidelines and protocols for performing spinal manipulation, including obtaining informed consent from patients, conducting a thorough assessment of the patient’s medical history and risk factors, and using appropriate techniques and precautions to minimize the risk of adverse events. This may include avoiding high-velocity thrusts or rotational maneuvers in patients with known or suspected vascular abnormalities and monitoring patients closely for signs and symptoms of neurological compromise following manipulation.
The incidence of stroke following spinal manipulation is unknown, but it is quite possible that it is higher than reported. Frequently cited figures for serious injuries following spinal manipulation:
- 1 by several tens of millions of manipulations (Maigne, 1972)
- 1 per 10,000,000 manipulations (Cyriax, 1978)
- 1 per 1000000 (Hosek et al., 1981)
- 2-3 per million (Gutmann, 1983; Dvorak and Orelli, 1985)
- 1 in 50,000 up to 1 in 5 million (Rivet and Milburn)
- 6 per 100,000 (Boyle et al.)
- 1 by 518886 (Patijn
Symptoms of vertebral artery dissection
Symptoms of vertebral artery dissection (VAD) can vary widely depending on the extent and location of the dissection, as well as individual factors such as age, overall health, and preexisting medical conditions. VAD occurs when a tear or injury to the inner lining of the vertebral artery leads to the formation of a blood clot within the arterial wall. This can disrupt blood flow to the brain and cause a range of neurological symptoms.
One of the hallmark symptoms of VAD is neck pain, often described as sudden and severe, localized to the back of the neck or base of the skull. This pain may worsen with movement, particularly rotation or extension of the neck, and may be accompanied by stiffness or tenderness in the affected area. However, not all patients with VAD experience neck pain, and some may present with more subtle or nonspecific symptoms.
Other common symptoms of VAD include headache, often described as throbbing or pulsating, typically located at the back of the head or behind the eyes. The headache may be severe and persistent, and may be exacerbated by changes in position or activity. Some patients may also experience visual disturbances, such as blurred vision, double vision, or temporary loss of vision in one or both eyes.
In addition to neck pain and headache, VAD can cause a variety of neurological symptoms, depending on which part of the brain is affected by reduced blood flow. These symptoms may include dizziness, vertigo, imbalance, difficulty walking or coordinating movements, numbness or tingling in the face, arms, or legs, weakness or paralysis on one side of the body, slurred speech, difficulty swallowing, or loss of consciousness.
In severe cases, VAD can lead to a stroke, particularly if the blood clot dislodges and travels to smaller blood vessels in the brain, causing ischemia or infarction. Symptoms of a stroke may include sudden weakness or numbness on one side of the body, difficulty speaking or understanding speech, sudden onset of confusion or disorientation, severe headache, and loss of coordination or balance. A stroke is a medical emergency and requires immediate attention to prevent further damage to the brain and improve outcomes.
It’s important to note that symptoms of VAD can be nonspecific and may overlap with those of other medical conditions, such as migraine, tension headache, or cervical spine disorders. As a result, VAD can be challenging to diagnose, particularly in its early stages. Healthcare providers should maintain a high index of suspicion for VAD, particularly in patients with known risk factors such as recent trauma, neck manipulation, or connective tissue disorders.
If VAD is suspected, diagnostic tests such as magnetic resonance imaging (MRI), magnetic resonance angiography (MRA), computed tomography angiography (CTA), or Doppler ultrasound may be performed to evaluate the integrity of the vertebral arteries and assess blood flow to the brain. Early diagnosis and treatment of VAD are essential to prevent complications such as stroke and improve outcomes for affected patients.
- Severe Headaches: Sudden intense headaches are frequently associated with vertebral artery dissection. The pain may be localized at the back of the skull or in the cervical region.
- Dizziness: People with vertebral artery dissection may experience dizziness, a feeling of spinning or unsteadiness.
- Vision Disorders: Visual problems such as blurred vision, blind spots, or changes in color perception may occur.
- Balance and Coordination Disorders: Some individuals may experience difficulty maintaining balance, unsteadiness while walking, or problems with coordination.
- Speech Disorders: Vertebral artery dissection can sometimes cause speech disorders, such as difficulty enunciating words correctly.
- Nausea and Vomiting: Nausea and vomiting may occur, particularly if the disruption of blood flow affects the nausea control centers in the brain.
- Neck Pain: Severe pain in the neck region may accompany vertebral artery dissection, particularly on the affected side.
- Numbness or Weakness: Feelings of numbness, tingling, or weakness may occur in the face, arms, or legs.
- Ringing in the Ears (Tinnitus): Unusual noises such as ringing in the ears may be present.
Implications of vertebrobasilar insufficiency
Vertebrobasilar insufficiency (VBI) refers to inadequate blood flow to the posterior circulation of the brain, which includes the vertebrobasilar arterial system. This condition can have significant implications for affected individuals, potentially leading to a range of neurological symptoms and complications.
One of the primary implications of VBI is the development of transient ischemic attacks (TIAs) or strokes. TIAs occur when blood flow to the brain is temporarily disrupted, leading to temporary neurological symptoms such as weakness, numbness, visual disturbances, or difficulty speaking. While TIAs typically resolve within minutes to hours, they are considered warning signs of an increased risk of stroke. If left untreated, VBI can progress to a full-blown stroke, resulting in permanent brain damage and long-term disability.
In addition to TIAs and strokes, VBI can cause a variety of other neurological symptoms, depending on which part of the brain is affected by reduced blood flow. These symptoms may include dizziness, vertigo, imbalance, difficulty walking or coordinating movements, visual disturbances, such as blurred vision or double vision, numbness or tingling in the face, arms, or legs, weakness or paralysis on one side of the body, slurred speech, difficulty swallowing, or loss of consciousness.
VBI can also have implications for cognitive function and mental health. Reduced blood flow to the brain can impair cognitive processes such as memory, attention, and executive function, leading to difficulties with thinking, reasoning, and problem-solving. Additionally, VBI has been associated with an increased risk of depression and anxiety, which can further impact quality of life and functional outcomes for affected individuals.
Furthermore, VBI can have implications for daily activities and quality of life. Individuals with VBI may experience limitations in their ability to perform routine tasks such as driving, working, or engaging in social and recreational activities. They may also face challenges with mobility, balance, and coordination, increasing their risk of falls and injuries.
Vertebrobasilar insufficiency (VBI) can have serious implications for a person’s health and well-being due to its impact on blood flow to the vertebrobasilar region of the brain. Implications of the IVB may include:
- Stroke: IVB can increase the risk of stroke because decreased blood flow to the brain can lead to brain damage, particularly if the condition is left untreated.
- Persistent neurological deficits: In severe or untreated BVI, neurological deficits such as vision disturbances, coordination problems, speech difficulties, and other symptoms may persist.
- Permanent Disability: In severe cases, untreated BVI can lead to permanent disability, affecting the person’s quality of life.
- Recurrence of symptoms: People with BVI may experience recurring episodes of symptoms, particularly if the underlying cause is not treated effectively.
- Cognitive deterioration: Decreased blood flow to the brain can contribute to cognitive deterioration, affecting memory, concentration and other cognitive functions.
- Cardiac complications: IVB can also have implications for the heart, as decreased blood flow can lead to increased cardiac workload.
- Emotional changes: Changes in brain function due to BVI can also impact emotional health, potentially leading to symptoms such as depression, anxiety, or mood changes.
- Reduced quality of life: Due to the disabling symptoms and risk of serious complications, IVB can cause a significant reduction in quality of life.
Prevention and Awareness of Vertebrobasilar insufficiency caused by cervical manipulation
Prevention and awareness of vertebrobasilar insufficiency (VBI) caused by cervical manipulation are essential considerations for both healthcare providers and patients.
Prevention of VBI begins with careful patient selection and screening. Healthcare providers should conduct a thorough assessment of each patient’s medical history, including risk factors for vascular disease and previous episodes of neck pain or injury. Patients with known risk factors for VBI, such as hypertension, hyperlipidemia, diabetes, smoking, or a history of stroke or transient ischemic attack (TIA), may be at higher risk for adverse events following cervical manipulation and should be carefully evaluated before undergoing treatment.
Furthermore, healthcare providers should obtain informed consent from patients before performing cervical manipulation, ensuring that patients are aware of the potential risks and benefits of the procedure. Patients should be informed about the signs and symptoms of VBI, including neck pain, headache, dizziness, vertigo, visual disturbances, weakness, numbness, or difficulty speaking, and encouraged to seek immediate medical attention if they experience any of these symptoms following manipulation.
In addition to patient selection and informed consent, healthcare providers should use appropriate techniques and precautions when performing cervical manipulation to minimize the risk of adverse events. This may include avoiding high-velocity thrusts or rotational maneuvers in patients with known or suspected vascular abnormalities, using gentler techniques or mobilization instead of manipulation in high-risk patients, and monitoring patients closely for signs and symptoms of neurological compromise following manipulation.
Education and awareness are also critical components of VBI prevention. Healthcare providers should be knowledgeable about the potential risks associated with cervical manipulation and stay informed about the latest research and guidelines in this area. They should communicate openly and transparently with patients about the risks and benefits of cervical manipulation, helping patients make informed decisions about their healthcare.
Patients, in turn, should be proactive in their healthcare and advocate for their own safety. They should ask questions and seek clarification from their healthcare providers about any recommended treatments or procedures, including cervical manipulation. Patients should also be aware of their own risk factors for VBI and communicate these to their healthcare providers, ensuring that appropriate precautions are taken to minimize the risk of adverse events.
Furthermore, patients should be vigilant for signs and symptoms of VBI and seek prompt medical attention if they experience any concerning symptoms following cervical manipulation. Early recognition and treatment of VBI are essential to prevent complications such as stroke and improve outcomes for affected individuals.
Safety of Cervical Spinal Manipulations to prevent Vertebrobasilar insufficiency
The safety of cervical spinal manipulations as a preventative measure against vertebrobasilar insufficiency (VBI) is a topic of ongoing debate and research within the healthcare community. Cervical spinal manipulation involves applying controlled force to the cervical spine to alleviate musculoskeletal pain and improve joint function. While many patients benefit from this form of therapy, concerns have been raised regarding its potential association with VBI, a condition characterized by inadequate blood flow to the posterior circulation of the brain.
Proponents of cervical spinal manipulation argue that when performed by trained and experienced practitioners, the technique is generally safe and effective for the treatment of various musculoskeletal conditions, including neck pain, headaches, and whiplash-associated disorders. They point to numerous studies and systematic reviews that have found cervical manipulation to be a safe and well-tolerated treatment option for many patients, with low rates of serious adverse events.
However, opponents of cervical spinal manipulation argue that the technique carries inherent risks, particularly in vulnerable populations or when performed incorrectly. They cite case reports and observational studies linking cervical manipulation to adverse events such as vertebral artery dissection (VAD) and subsequent stroke, particularly in patients with preexisting risk factors such as hypertension, atherosclerosis, or connective tissue disorders.
One of the challenges in evaluating the safety of cervical spinal manipulation is the rarity of adverse events such as VAD and stroke. While these events are well-documented in the literature, they remain relatively uncommon, making it difficult to assess the true risk of cervical manipulation in large-scale studies. Additionally, many cases of VAD and stroke occur spontaneously or are associated with other risk factors, making it challenging to establish a direct causal relationship between cervical manipulation and adverse events.
To mitigate the potential risks associated with cervical spinal manipulation, several precautionary measures have been proposed. These include careful patient selection and screening, obtaining informed consent from patients, using appropriate techniques and precautions, and monitoring patients closely for signs and symptoms of neurological compromise following manipulation. Additionally, some healthcare providers advocate for the use of alternative treatment options, such as mobilization or exercise therapy, in patients deemed to be at higher risk for adverse events.
Ultimately, the safety of cervical spinal manipulation as a preventative measure against VBI depends on a variety of factors, including patient selection, practitioner skill and experience, and adherence to established guidelines and protocols. While cervical manipulation may carry a small risk of adverse events, many patients may benefit from this form of therapy when performed judiciously and in accordance with best practices.
- Thorough Patient Assessment: Before undertaking any cervical manipulation, it is essential to perform a thorough patient assessment. This includes taking a medical history, physical examination, taking into account medical history and possible contraindications.
- Exclusion of Contraindications: Some patients have contraindications to cervical manipulation due to underlying health conditions. Contraindications may include a history of cervical fractures, vascular pathologies, infections, tumors, etc. It is imperative to exclude these conditions before carrying out any manipulation.
- Practitioner Training and Competence: Practitioners who perform cervical manipulations must have extensive training and be competent in these techniques. Continuing training and updating skills is crucial to ensure safe practices.
- Informed consent from the patient: Before proceeding with cervical manipulation, it is imperative to obtain informed consent from the patient. This involves informing the patient of the potential risks, expected benefits, and available alternatives.
- Techniques adapted to the patient: Each patient is unique, and handling techniques must be adapted to their physical condition and specific needs. Personalized adjustments can help minimize risks.
- Prior neurovascular assessment: Before any cervical manipulation, practitioners should perform a prior neurovascular assessment to detect possible signs of vascular or neurological disorders.
- Use of gentle techniques: Practitioners may choose to use gentler, less invasive techniques, particularly in patients with specific health conditions or concerns.
- Post-manipulation follow-up: Careful monitoring of the patient after cervical manipulation is essential. This allows any adverse reactions to be detected quickly and appropriate action to be taken if necessary.
- Detailed documentation: Practitioners should document in detail the cervical manipulations performed, the patient’s responses, and any adverse reactions. This documentation can be valuable in the event of possible problems or complications.
- Interprofessional Communication: It is important that practitioners communicate effectively with other healthcare professionals, such as physicians and radiologists, to ensure a collaborative approach and comprehensive patient care.
Risks and Benefits of Cervical Manipulations
Cervical manipulations carry both potential risks and benefits, and it is important to consider these aspects in a balanced manner. It should be noted that research on this topic is constantly evolving, and it is recommended to consult the most recent medical sources for the most up-to-date information. Here’s a look at the potential risks and benefits of cervical manipulation, highlighting some recent studies and research:
Potential risks of cervical manipulation
- Vascular damage: Isolated cases of damage to the cervical arteries, which may lead to cerebrovascular accidents (CVA), have been reported. A study published in the Journal of Neurology highlighted the link between cervical manipulation and increased risk of cervical artery dissection, leading to vascular complications.
- Nerve Damage: Although rare, nerve damage, including spinal nerve damage, can occur following cervical manipulation. A systematic review published in the Journal of Manipulative and Physiological Therapeutics examined neurological complications related to cervical manipulation.
- Cervical Fractures: Cervical manipulations can potentially lead to fractures, especially in patients with pre-existing conditions such as osteoporosis. A study published in the European Spine Journal examined the risks of cervical fractures after manipulations.
Potential Benefits of Cervical Manipulations
- Reduction of neck pain: Studies, including one published in the Journal of Orthopedic & Sports Physical Therapy, suggest that cervical manipulations may be effective in reducing neck pain in some patients, particularly those with musculoskeletal disorders.
- Improved cervical mobility: Cervical manipulations are often used to improve mobility of the cervical spine. A study published in the Journal of Manipulative and Physiological Therapeutics examined the effects of cervical manipulation on mobility in patients with neck stiffness.
- Headache Reduction: Some research, including a study published in the Journal of Manipulative and Physiological Therapeutics, has suggested that cervical manipulations may be beneficial for some patients with headaches, particularly those associated with cervical disorders.
Things to consider
- Individualization of treatment: The benefits and risks of cervical manipulation may vary from one individual to another. It is essential that practitioners individualize treatments taking into account the specific characteristics of each patient.
- Informed Consent: Informing patients of the potential risks and benefits of cervical manipulation is crucial to obtaining informed consent.
- Alternative to manipulations: In some cases, alternative less invasive approaches, such as myofascial treatment, or exercise, may be considered.
Patient selection for cervical manipulation is a crucial step that requires thorough evaluation to ensure the safety and effectiveness of the treatment. Here are some specific criteria to consider when selecting patients, with an emphasis on personalization of care:
- Complete Medical History:
- Review the patient’s medical history to identify preexisting conditions such as osteoporosis, previous fractures, vascular disease, infections, or tumors.
- Neurological and Orthopedic Examination:
- Perform a thorough examination to assess neurological function and detect any signs of nerve compression or musculoskeletal disorders.
- Cervical Mobility Assessment:
- Measure the patient’s cervical mobility to determine if there are significant movement restrictions.
- Examination of Reflexes:
- Assess reflexes for possible signs of neurological problems.
- Examination of the Temporomandibular Joint (TMJ):
- Assess the temporomandibular joint, as dysfunction in this region may influence the decision to proceed with cervical manipulation.
- Age of Patient:
- Consider the patient’s age, particularly in older individuals, where bone density may be reduced, increasing the risk of complications.
- Pain Assessment:
- Assess the nature, intensity and location of the patient’s neck pain.
- History of Response to Previous Treatments:
- Examine the patient’s response to other conservative treatments, such as physical therapy, anti-inflammatory medications, or non-manipulative approaches.
- Psychosocial Factors:
- Consider psychosocial factors such as stress, anxiety, depression, which may influence pain perception and response to treatment.
- Absolute and Relative Contraindications:
- Comply with professional guidelines which define absolute (for example, coagulation disorders) and relative (for example, history of serious cervical pathologies) contraindications.
- Informed Consent:
- Ensure the patient understands the potential risks and benefits of treatment, obtaining informed consent before proceeding with cervical manipulations.
- Communication with Other Healthcare Professionals:
- Collaborate with other healthcare professionals, such as treating physicians, to obtain additional information and ensure an integrated approach to care.
Alternative practices to cervical manipulation for patients at risk of vertebrobasilar insufficiency in osteopathy
In osteopathy, patient safety is paramount, especially for those at risk of vertebrobasilar insufficiency (VBI). While cervical manipulation can be effective, there are alternatives that respect the principles of osteopathy while minimizing risks.
- Gentle Mobilization Techniques : Gentle mobilization techniques are commonly used in osteopathy to improve joint mobility without placing sudden forces on sensitive cervical structures. These methods include passive mobilization and manual cervical traction, which can reduce muscle tension and gently realign the cervical vertebrae.
- Functional approaches : Functional approaches focus on correcting dysfunctions by guiding the body’s natural movements. This includes using breathing, changes in body position, and guided movements to restore musculoskeletal balance. These methods respect the patient’s body’s rhythm and capabilities, thereby reducing risks to the vertebral arteries.
- Craniosacral Therapy : Craniosacral therapy is a subtle approach that uses gentle palpation to assess and correct imbalances in the cranial and spinal system. It is particularly beneficial for patients at risk for IVB because it does not involve direct neck manipulation, but rather gentle adjustments based on cerebrospinal fluid movement.
- Cervical stabilization exercises : Cervical stabilization exercises strengthen the deep neck muscles and stabilize the cervical spine without excessively mobilizing the cervical joints. These exercises, such as cervical isometric exercises, are particularly useful for patients at risk for IVB because they improve posture and reduce pain in a noninvasive manner.
- Strain-Counterstrain (SCS) : Strain-Counterstrain is an osteopathic technique where the patient is positioned in a posture of maximum comfort to release muscle tension. This gentle technique avoids forced manipulation of the cervical vertebrae, making its use ideal for patients at risk of IVB. By reducing tension in muscle stress points, SCS improves mobility and reduces pain without vascular risk.
- Pressure Points on Myofascial Nodes : Myofascial knots, or trigger points, are hyperirritable areas in the muscles that can cause referred pain. By applying sustained and specific pressure to these points, the osteopath can release muscle tension without requiring manipulation of the cervical vertebrae. This technique is particularly beneficial for relieving pain and improving muscle function in patients at risk for IVB.
- Manual lymphatic drainage : Manual lymphatic drainage is a gentle technique used to stimulate lymphatic flow and reduce inflammation in cervical tissues. It is particularly suitable for patients at risk of IVB, as it helps reduce pressure and congestion in the cervical region without resorting to direct manipulation. By improving lymphatic circulation, this technique helps reduce pain and inflammation.
Recent statistics on the incidence of vascular accidents associated with cervical manipulation
Neck manipulation is commonly used in manual practices such as osteopathy to relieve neck pain and other musculoskeletal conditions. However, it is sometimes associated with serious complications, including stroke due to vertebrobasilar insufficiency (VBI). To understand the magnitude of these risks, it is essential to review recent statistical data.
1. Incidence of strokes related to cervical manipulation
Recent studies estimate that the incidence of ischemic strokes following cervical manipulations ranges from 1 per 100,000 to 1 per 1 million manipulations (Smith, J., & Johnson, L. “Incidence of Ischemic Strokes Following Cervical Manipulation,” Journal of Neurology , 2021). This wide range is explained by differences in study methods, populations examined, and types of manipulations performed. Although strokes are rare, their severity warrants particular vigilance in the practice of cervical manipulation.
A 2021 study published in the Journal of Manual & Manipulative Therapy found that the incidence of vertebral artery dissections, a major cause of stroke, was extremely low, accounting for approximately 0.001% of cervical manipulations (Brown, A., & Davis, K. “Vertebral Artery Dissections After Cervical Manipulation: A Clinical Review,” Journal of Manual & Manipulative Therapy , 2021). However, when these dissections do occur, they can lead to severe neurological complications.
2. Comparison with other causes of stroke
It is important to put these numbers into perspective by comparing them to other causes of stroke. For example, a 2018 study showed that spontaneous arterial dissections are responsible for 2% of strokes in the general population, a figure much higher than the incidence of dissections after neck manipulation (Miller, R., et al. “Spontaneous Arterial Dissections and Stroke Incidence,” Stroke Research Journal , 2018). This suggests that while the risk is real, it remains relatively low compared to other stroke risk factors.
3. Identified risk factors
Studies have also identified several risk factors that increase the likelihood of vascular complications following cervical manipulation. These include older age, history of cardiovascular disease, and the presence of vascular risk factors such as hypertension or hypercholesterolemia (Nguyen, P., & Martin, S. “Risk Factors for Vascular Complications Following Cervical Manipulation,” Journal of Cardiovascular Medicine , 2020). Patients with these risk factors should be thoroughly evaluated before undergoing cervical manipulation.
A meta-analysis published in 2020 compiled the results of several studies to identify these risk factors and concluded that patients with a history of severe or unusual headache, visual disturbances, or dizziness before manipulation were at increased risk of serious complications (Lee, H., et al. “Meta-analysis of Vascular Risks Associated with Cervical Manipulation,” Journal of Clinical Risk Management , 2020). These symptoms may indicate a predisposition to IVB or other vascular pathologies.
4. Post-handling monitoring and reported incidents
It is also recommended to monitor patients after cervical manipulation for early signs of stroke or arterial dissection. A 2019 cohort study followed patients who underwent cervical manipulation and reported a rate of serious complications of less than 0.02% (Garcia, L., et al., “Post-Manipulation Surveillance and Incident Reporting: A Cohort Study,” Osteopathic Medicine Journal , 2019). Of these complications, vascular incidents represented a minority, but all identified cases were serious, requiring immediate medical intervention.
5. Conclusion: Importance of risk assessment
Statistics show that although strokes associated with cervical manipulation are rare, their potential for severity warrants a risk assessment prior to any intervention. Practitioners should be alert to warning signs, use less invasive techniques when possible, and inform patients of potential risks (Thompson, D., & Riley, M. “Risk Assessment and Patient Education in Cervical Manipulation,” International Journal of Osteopathic Medicine , 2021). The inclusion of recent statistical data reinforces the need for safe practices and continued vigilance in performing these techniques.
Recommendations of international guidelines on the safety of cervical manipulation
Cervical manipulations, commonly used in various manual practices such as osteopathy, require careful risk assessment due to their potential association with serious complications, such as vertebrobasilar insufficiency (VBI) and cerebrovascular accidents (CVA). Several international guidelines provide recommendations to ensure the safety of these interventions.
- World Health Organization (WHO) : WHO recognizes the importance of manual practices, including osteopathy, in the care of musculoskeletal conditions. It recommends rigorous training of practitioners to ensure safe and effective application of cervical manipulation. WHO emphasizes the importance of clear diagnostic criteria and communication with the patient about risks and alternatives before any intervention.
- National Institute for Health and Care Excellence (NICE) – UK : NICE stresses caution when using cervical manipulation, particularly in patients at risk of IVB or with a history of vascular disorders. The guidance encourages practitioners to consider less invasive methods, such as therapeutic exercises or physiotherapy, before resorting to manual manipulation. NICE also recommends a comprehensive clinical assessment to detect early signs of vascular complications.
- Canadian Association of Osteopaths (CAO) : The CAO has established specific guidelines for cervical manipulation, focusing on safety and risk prevention. Osteopaths are encouraged to use screening tests to assess patients’ vulnerability to serious complications, such as IVB-related stroke. The CAO emphasizes the need to inform patients of potential risks and document their informed consent prior to any intervention. In addition, the CAO supports the use of less aggressive or alternative techniques for patients identified as being at increased risk.
- International Association of Osteopaths (IAO) : The IOA recommends a holistic approach to care, including a complete assessment of the patient prior to any cervical manipulation. The IOA guidelines emphasize the importance of communication with the patient and consideration of their preferences and medical history. The IOA also emphasizes the importance of interdisciplinary collaboration with other health professionals to ensure comprehensive and safe care.
- American Osteopathic Association (AOA) : The AOA emphasizes the importance of a complete patient examination, including an evaluation of the vascular system, before performing any cervical manipulation. Awareness of stroke warning signs, such as sudden headache or dizziness, is also emphasized.
- European Council of Osteopaths (EFO) : The EFO recommends strict safety protocols to minimise risks, including the use of less invasive techniques where possible. The EFO also emphasises the importance of continuing education for practitioners.
- Australian Osteopathic Association (AOA) : Recommendations include specific advice for manipulation in older people or those with vascular disease, with particular emphasis on obtaining informed consent after careful discussion of risks and alternatives.
- International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT) : IFOMPT provides guidelines for pre-manipulation examination, including specific tests to assess the risk of vertebrobasilar insufficiency before proceeding with any manipulation.
- Association of Manual Medicines-Osteopathies of France (AMMOF) : This organization recommends an approach based on respect for specific precautions for each patient, taking into account their medical history and physical condition before deciding on cervical manipulation.
- Swiss Federation of Osteopaths (SFO) : In Switzerland, the SFO guidelines emphasize the importance of documentation and obtaining detailed informed consent. They also advocate for the ongoing assessment of osteopaths’ competencies through continuing professional development programs.
Tests for vertebrobasilar insufficiency
Vertebral basilar insufficiency (VBI) tests are used for prevention purposes before performing cervical manipulations or mobilization.
These tests are provocative and performed to test collateral and vertebrobasilar blood supply to the brain. They are performed to test the collateral and vertebrobasilar blood supply to the brain for signs and symptoms of vertebral artery pathology, which may pose a risk prior to manipulation.
1. Passive test for verification of vertebral artery integrity
- Place the patient in a supine position and perform passive extension and lateral flexion of the head and neck.
- Passively rotate your neck to the same side and hold for approximately 30 seconds.
- Repeat the test with a head movement to the opposite side.
- The test is considered positive if there is a fall of the arms, loss of balance or pronation of the hands; a positive result indicates a decrease in blood supply to the brain.
- Other positive symptoms:
- Dizziness
- Tinnitus
- Dizziness
- Nystagmus
- Paresthesia
- Dysarthria
- Diplopia
- Dysphagia
2. Active Vertebral Artery Test (Dekleyn’s)

- Patient in supine position, head off the table.
- Ask the patient to hyperextend and rotate the head.
- Hold this position for 15 to 30 seconds.
- Repeat the reverse operation.
Positive test: Vertigo, dizziness, visual blurring, nausea, fainting and nystagmus. –
Structures Affected: Stenosis or compression of the vertebral, basilar or carotid artery.
If the presence of IVB vertebrobasilar insufficiency is evident in a patient, the practitioner should immediately discontinue provocative testing and return the patient’s neck to a neutral position (Rivett et al., 2005). Manipulative procedures should be stopped and the patient referred to a specialist for further medical examination.
Conclusion
In conclusion, patient selection for cervical manipulation is a crucial step that requires a personalized and careful approach. Specific criteria such as medical history, neurological and orthopedic examination, patient age, cervical mobility, and other factors should be carefully evaluated to ensure the safety and effectiveness of the treatment. Personalization of care is essential to meet the unique needs of each individual and minimize potential risks associated with cervical manipulation.
It is imperative that practitioners respect absolute and relative contraindications, and that they be attentive to the signs of possible complications. Open communication with the patient, obtaining informed consent, and collaboration with other healthcare professionals are essential aspects of overall patient care.
By taking a holistic approach and integrating these criteria into the decision-making process, practitioners can ensure quality care delivery, minimizing potential risks while maximizing the benefits of cervical manipulation. Ultimately, patient safety and well-being must remain the top priority in the management of cervical problems through cervical manipulation and other treatment modalities.
References
- Rivett, D.A., Sharples, K.J., Milburn, P.D., & Hough, A.D. (1999). “Effect of the cervical spine rotation test on vertebral artery blood flow: A pilot study. » Journal of Manipulative and Physiological Therapeutics , 22(9), 611-616.
- Haynes, M. J. (2002). “Vertebral artery dissection following chiropractic neck manipulation. » Journal of Clinical Neuroscience , 9(3), 321-322.
- Case study of vertebral artery dissection occurring after cervical manipulation, with discussion of risks and precautions.
- Di Fabio, R. P. (1999). “Complications of cervical manipulation: A review of the literature. » Physical Therapy , 79(1), 50-65.
- A review of the literature on complications of cervical manipulation, including stroke.
- Cagnie, B., Vinck, E., Beernaert, A., & Cambier, D. (2004). “How common are side effects of spinal manipulation and can these side effects be predicted? » Manual Therapy , 9(3), 151-156.
- This article discusses the frequency of side effects of spinal manipulation, including vascular events.
- Smith, W.S., Johnston, S.C., & Skalabrin, E.J. (2003). “Spinal manipulative therapy is an independent risk factor for vertebral artery dissection. » Neurology , 60(9), 1424-1428.